ABSTRACT
Background: Despite growing support for the distinction between posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) as separate diagnoses within the ICD-11 psychiatric taxonomy, the prevalence and treatment implications of CPTSD among current and ex-serving military members have not been established.
Objective: The study aims were to a) establish the prevalence of provisional ICD-11 CPTSD diagnosis relative to PTSD in an Australian sample of treatment-seeking current and ex-serving military members, and b) examine the implications of CPTSD diagnosis for intake profile and treatment response.
Methods: The study analysed data collected routinely from Australian-accredited treatment programmes for military-related PTSD. Participants were 480 current and ex-serving military members in this programmes who received a provisional ICD-11 diagnosis of PTSD or CPTSD at intake using proxy measures. Measures of PTSD symptoms, disturbances in self-organisation, psychological distress, mental health and social relationships were considered at treatment intake, discharge, and 3-month follow-up.
Results: Among participants with a provisional ICD-11 diagnosis, 78.2% were classified as having CPTSD, while 21.8% were classified as having PTSD. When compared to ICD-11 PTSD, participants with CPTSD reported greater symptom severity and psychological distress at intake, and lower scores on relationship and mental health dimensions of the quality of life measure. These relative differences persisted at each post-treatment assessment. Decreases in PTSD symptoms between intake and discharge were similar across PTSD (dRM = −0.81) and CPTSD (dRM = −0.76) groups, and there were no significant post-treatment differences between groups when controlling for initial scores.
Conclusions: CPTSD is common among treatment-seeking current and ex-serving military members, and is associated with initially higher levels of psychiatric severity, which persist over time. Participants with CPTSD were equally responsive to PTSD treatment; however, the tendency for those with CPTSD to remain highly symptomatic post-treatment suggests additional treatment components should be considered.
HIGHLIGHTS
• ICD-11 complex PTSD (CPTSD) is more prevalent than PTSD in current and ex-serving military members seeking treatment for PTSD.
• Responses to programmatic trauma-focused treatment were similar across the two provisional diagnoses.
• Participants with CPTSD maintained higher symptom severity overall post-treatment than those with PTSD, and further research is needed to establish what supplementary treatment might be appropriate.
• CPTSD is more prevalent than PTSD in treatment-seeking current and ex-serving military members. Participants with CPTSD were equally responsive as those with PTSD to trauma-focused treatment, though those with CPTSD maintained higher symptom severity pre- and post-treatment.
Antecedentes: A pesar del creciente apoyo para la distinción entre trastorno de estrés postraumático (TEPT) y trastorno de estrés postraumático complejo (TEPTC) como diagnósticos separados dentro de la taxonomía psiquiátrica de la CIE-11, la prevalencia y las implicaciones en el tratamiento del TEPTC dentro de miembros militares activos o en retiro no han sido establecidas.
Objetivo: Los objetivos del estudio fueron a) establecer la prevalencia de TEPTC provisional según CIE-11 en relación al TEPT en una muestra australiana de miembros militares activos o en retiro en busca de tratamiento, y b) examinar las implicaciones del diagnóstico de TEPTC para el perfil de ingreso y respuesta a tratamiento.
Método: El estudio analizó datos recolectados de forma rutinaria por programas de tratamiento australianos acreditados para TEPT relacionado a militares. Los participantes fueron 480 miembros activos o en retiro ingresados a este programa bajo el diagnóstico provisional de TEPT o TEPTC según CIE-11 a través de indicadores indirectos. Al ingreso, egreso y a los 3 meses de seguimiento, se consideraron mediciones de los síntomas de TEPT, alteraciones en la organización del Yo, estrés psicológico, salud mental y relaciones sociales.
Resultados: Dentro de los participantes con un diagnóstico provisional según CIE-11, el 78,2% fue clasificado como portador de TEPTC, mientras que un 21,8% fue clasificado como portador de TEPT. Al ser comparados con TEPT según CIE-11, los participantes con TEPTC reportaron al ingreso una mayor severidad en la sintomatología y en el estrés psicológico, y menores puntajes en las dimensiones de medida de calidad de vida de salud mental y relaciones sociales. Estas diferencias relativas persistieron en cada seguimiento posterior al tratamiento. Las disminuciones en los síntomas de TEPT entre el ingreso y el egreso fueron similares entre los grupos con TEPT (dRM = -0.81) y TEPTC (dRM = -0.76), y no hubo diferencias significativas post-tratamiento entre los grupos al controlarlos según los puntajes iniciales.
Conclusiones: El TEPTC es común dentro de miembros militares activos o en retiro en busca de tratamiento, y está asociado a mayores niveles de severidad psiquiátrica inicial, la cual persiste a lo largo del tiempo. Los participantes con TEPTC respondieron igualmente al tratamiento del TEPT; sin embargo, la tendencia de aquéllos con TEPTC de permanecer altamente sintomáticos tras el tratamiento sugiere componentes de tratamiento adicionales que deberían ser considerados.
背景: 尽管在ICD-11精神病学分类法中作为独立诊断的创伤后应激障碍 (PTSD) 和复杂性PTSD (CPTSD) 之间的区别得到越来越多的支持, 但现役和退役军人中CPTSD的流行率和治疗意义尚未得到证实。
目的: 本研究旨在:a) 在澳大利亚寻求治疗的现役和退役军人样本中, 确定相对于PTSD的ICD-11 CPTSD临时诊断的流行率, 以及b) 考查CPTSD诊断对治疗摄入的剖面和治疗反应的意义。
方法: 本研究分析了从澳大利亚认可的军事相关PTSD治疗计划中定期收集的数据。参与者为480名在此计划中通过代理测量得到ICD-11 PTSD或CPTSD临时诊断的现役和退役军人。考虑了治疗期间, 出院时和3个月的随访时的PTSD症状, 自我组织障碍, 心理困扰, 心理健康和社会关系的测量。
结果: 在具有ICD-11临时诊断的参与者中, 有78.2%归类为CPTSD组, 而21.8%;归类为PTSD组。相较于ICD-11 PTSD组, CPTSD组的参与者在治疗摄入时报告了更高的症状严重程度和心理困扰, 和更低的生活质量测量的关系和心理健康维度得分。这些相对差异在每次治疗后评估中均持续存在。治疗和出院时PTSD组 (dRM = −0.81) 和CPTSD组 (dRM = −0.76) PTSD症状的减少相似, 并且在控制初始得分时治疗后无显著组间差异。
结论: 在寻求治疗的现役和退役军人中CPTSD很常见, 并且与初始更高的精神病严重程度有关, 并随着时间的流逝而持续。 患有CPTSD的参与者对PTSD的治疗反应相同。但是, 对于CPTSD患者, 在治疗后仍保持高度症状的趋势表明, 应考虑使用额外治疗方法。
1. Introduction
The 11th edition of the International Classification of Diseases and Related Health Problems (ICD; World Health Organisation, Citation2018) has introduced significant changes under the umbrella of ‘disorders specifically associated with stress’. Alongside the previously established diagnosis of posttraumatic stress disorder (PTSD), the new ICD-11 taxonomy has proposed a ‘sibling’ diagnosis with a related but distinct symptom profile: complex PTSD (CPTSD). This addition was based on mounting evidence, extending on the work of Herman (Citation1992) and earlier researchers (De Wind, Citation1972; Horowitz, Citation1974; Marmar, Citation1991; Niederland, Citation1964), highlighting the impact of prolonged and/or repetitive interpersonal traumatic stress on self-organisation independently of PTSD symptomatology.
According to the ICD-11, the CPTSD diagnostic concept retains the core symptom clusters of PTSD including: (1) re-experiencing the traumatic event in the form of flashbacks or nightmares; (2) avoidance of internal and external trauma reminders related to the event; and (3) persistent-heightened sense of current threat, indicated by hypervigilance or increased startle response (World Health Organisation, Citation2018). However, CPTSD is also characterised by additional symptoms relating to ‘disturbances in self-organisation’ (DSO), which comprise three clusters relating to negative self-concept (e.g. feelings like failure or worthlessness), affective dysregulation (e.g. heightened or lowered emotional reactivity), and disturbances in relationships (e.g. difficulties in establishing or sustaining interpersonal connections, or avoidance of relationships; Maercker et al., Citation2013). In order to meet a CPTSD diagnosis, each of the PTSD diagnostic criteria must be met, as well as at least one symptom from each of the three DSO clusters (Cloitre, Garvert, Brewin, Bryant, & Maercker, Citation2013). Notably, those with a CPTSD diagnosis are not considered to have a PTSD diagnosis, such that a PTSD diagnosis and a CPTSD diagnosis are mutually exclusive.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, Citation2013) has taken a different approach than ICD-11 to address clinical complexity in PTSD conditions. Rather than introducing a new diagnosis, the DSM-5 expanded the prior DSM-IV PTSD diagnostic criteria to include ‘negative alterations in cognitions and mood’, which overlaps significantly with complex PTSD-associated negative self-concept, affective dysregulation, and difficulties in relationships. In addition, the expanded DSM-5 criteria include a specifier for a dissociative subtype, with dissociation more commonly associated with complex presentations. As such, these two nosological systems differ regarding whether or not complex PTSD constitutes a distinct diagnostic category. The ICD-11 PTSD diagnosis has aimed to be more specific in identifying PTSD, with relevant studies also demonstrating that ICD-11 PTSD prevalence estimates are lower than those derived from the DSM-5 (Wisco et al., Citation2016).
There is considerable empirical support for distinct profiles of ICD-11 PTSD and CPTSD symptomatology, suggesting that CPTSD is a useful addition to this psychiatric taxonomy. Given that the ICD-11 took a restricted approach to the PTSD diagnosis by only including core intrusion, avoidance, and arousal symptoms that are specific to PTSD and not shared by other disorders (Brewin et al., Citation2017), the CPTSD diagnosis provides a way of distinguishing those with more complex presentations. CPTSD has been differentiated from PTSD in a broad range of trauma-exposed samples, including victims of childhood interpersonal trauma (e.g. repeated childhood physical or sexual abuse (Cloitre, Garvert, Weiss, Carlson, & Bryant, Citation2014) or maltreatment within institutional settings (Knefel, Garvert, Cloitre, & Lueger-Schuster, Citation2015), as well as adults exposed to terrorism (Cloitre et al., Citation2013), prisoners of war (Palic et al., Citation2016; Zerach, Shevlin, Cloitre, & Solomon, Citation2019), refugees (Hyland et al., Citation2018; Nickerson et al., Citation2016; Palic et al., Citation2016) and homeless populations (Armstrong, Phillips, Alkemade, & Louise O’Donnell, Citation2020). However, empirical research into how the CPTSD concept might apply to military populations is both scarce and inconsistent. While Palic et al. (Citation2016), Folke, Nielsen, Andersen, Karatzias, and Karstoft (Citation2019), and Mordeno, Nalipay, and Mordeno (Citation2019) have identified distinct CPTSD symptom profiles in military samples, Wolf et al. (Citation2015) question the validity of the CPTSD diagnosis, arguing that PTSD and CPTSD are not distinct. The degree to which the CPTSD diagnosis has utility in the context of military-related trauma thus requires further exploration.
Research into the prevalence of CPTSD as defined by ICD-11 criteria is now emerging. Early estimates of ICD-11 CPTSD in general population samples have suggested rates ranging from 0.5% to 2.6%, relative to 2.3% to 9.0% for ICD-11 PTSD (Ben‐Ezra et al., Citation2018; Hyland et al., Citation2017; Maercker, Hecker, Augsburger, & Kliem, Citation2018; Wolf et al., Citation2015). Sample-based estimates for specific subpopulations have also indicated rates of ICD-11 CPTSD ranging from 13% to 20.7% among victims of single event physical and sexual assault, respectively (Elklit, Hyland, & Shevlin, Citation2014), 21.4% among survivors of childhood institutional abuse (Knefel & Lueger-Schuster, Citation2013), 32.8% among refugees (Nickerson et al., Citation2016), and 42.8% among survivors of childhood sexual abuse (Hyland et al., Citation2017). In the first studies of CPTSD in veterans, Wolf et al. (Citation2015) found a CPTSD prevalence rate of 13% and PTSD prevalence rate of 21.4% in an internet-based sample of trauma-exposed military veterans from the U.S., while Mordeno et al. (Citation2019) found prevalence rates of 16.4% CPTSD and 36.7% PTSD in Filipino combat-exposed soldiers. Conversely, in a latent profile analysis of a sample of treatment-seeking Danish military veterans, Folke et al. (Citation2019) found that 14.1% scored highly on only PTSD symptoms, whereas 17.3% scored highly on PTSD as well as DSO symptoms. Furthermore, a recent study found that 80.63% of treatment-seeking Croatian military veterans with a prior PTSD diagnosis met criteria for a provisional CPTSD diagnosis (Letica-Crepulja et al., Citation2020). It should be noted that with the exception of Letica-Crepulja et al. (Citation2020), these papers used proxy measures of ICD-11 PTSD and DSO symptoms – i.e. items taken from other measures that map onto ICD-11 symptoms – rather than ICD-11-based clinician-administered measure. Nonetheless, these high prevalence rates of CPTSD amongst veterans, and their variability relative to PTSD rates, suggest that it is important to continue investigations into the clinical utility of the ICD-11 CPTSD diagnosis in this population.
In order to determine the utility of the CPTSD diagnosis among current and ex-serving military members, the potential implications of the CPTSD classification for treatment response should be investigated. There has been vigorous debate as to whether individuals with CPTSD are likely to benefit from modified forms of current evidence-based PTSD treatments; specifically, whether those with CPTSD require interventions that directly address problems in emotion regulation, negative self-concept and disturbances in relationships (Cloitre, Citation2015; De Jongh et al., Citation2016; Karatzias & Cloitre, Citation2019). The recommendation for additional CPTSD-specific intervention is predicated on the idea that standard trauma-focused treatment may be less effective for those with CPTSD – however, others have argued that there is insufficient evidence to support this (De Jongh et al., Citation2016). While treatment guidelines support the efficacy of trauma-focused interventions for PTSD more broadly (Hamblen et al., Citation2019; International Society of Traumatic Stress Studies, Citation2018b; National Institute for Health and Care Excellence, Citation2018; Phoenix Australia Centre for Posttraumatic Mental Health, Citation2013), there are limited data available regarding their efficacy specifically for treating CPTSD. However, one meta-analysis of 51 PTSD treatment trials found beneficial effects of trauma-focused treatments, such as cognitive behavioural therapy (CBT), exposure alone (EA) and eye movement desensitisation and reprocessing (EMDR), in reducing PTSD symptoms in those likely to have clinically significant baseline levels of one or more DSO symptom cluster; albeit with smaller effects than non-specific interventions (Karatzias et al., Citation2019). This review also indicated that standard CBT and EA reduced the distinctive CPTSD symptoms, specifically negative self-concept and relationship disturbances. There was, however, insufficient evidence regarding the treatments’ impacts on emotion dysregulation. Such studies suggest that standard trauma-focused interventions may be effective not only for patients with PTSD, but also for those with CPTSD. In Australia, standard trauma-related interventions focussed on PTSD, not CPTSD, are commonly provided to treatment-seeking current and ex-serving military members – however, it remains unclear to what extent this standard treatment might also benefit those with CPTSD.
1.1. Aims
This study involved the investigation of treatment outcome data collected routinely from Australian current and ex-serving military members seeking PTSD treatment, and was intended to address the following aims:
Aim I: Establish the relative rates and socio-demographic, service-related and pension-related characteristics of ICD-11 PTSD and CPTSD presentations in a sample of current and ex-serving military members seeking treatment for PTSD; and
Aim II: Examine the extent to which a provisional CPTSD diagnosis is associated with distinct treatment intake profiles and treatment response patterns in a national accredited PTSD treatment programmes for current and ex-serving military members with PTSD.
2. Method
2.1. Participants and procedure
Participants comprised current and ex-serving members of the Australian Defence Force (ADF) who participated in one of 14 accredited PTSD treatment programmes across Australia that were funded by the Australian Government Department of Veterans’ Affairs (DVA) between 2014 and 2019. Participants are referred to the programmes by their GPs, treating psychiatrists or psychologists, and ex-serving members typically have not responded to prior treatment and/or have long chronicity of disorder. In order to be eligible for treatment, participants were required to meet diagnostic criteria for military-related PTSD on the Clinician Administered PTSD Scale for DSM-5 (Weathers et al., Citation2018). Routine treatment in these accredited PTSD treatment programmes followed national DVA accreditation standards for group and individual intervention components (Department of Veterans’ Affairs, Citation2015). The individual components specified in these standards include engagement work, evidence-based trauma-focussed therapy and relapse prevention. The group components include psychoeducation and symptom management, including for comorbid problems such as anxiety, anger, depression, sleep and substance use issues. Programmes incorporated 20–30 treatment days with each cohort of 5–10 participants receiving a combination of individual and group therapy. Participants were excluded from the programmes if they were currently psychotic, actively suicidal, had acute substance use disorders or were currently experiencing major life crises. As part of the programmes quality assurance processes, all participants completed a battery of standardised questionnaires at treatment intake, and again at treatment discharge and 3 months post-treatment follow-up. The Australian Government Departments of Defence and Veterans’ Affairs Human Research Ethics Committee approved the administration of these questionnaires and secondary analyses of these for research purposes.
As the present study aimed to investigate the prevalence and treatment implications of the ICD-11 CPTSD concept in a military sample, eligibility for inclusion of a participant’s data in the analysis required a provisional ICD-11 diagnosis of either PTSD or CPTSD. presents the total number of current and ex-serving members of the ADF who had commenced the programmes with a DSM-5 PTSD diagnosis (n = 780), those excluded from the original data source, and the final number of participants included in this study (n = 458).
2.2. Measures
2.2.1. Sociodemographic variables
A variety of sociodemographic information was collected at treatment intake, including participant age, gender, marital status, employment status, service status, and pension status, and whether participants were applying for a pension or a pension increase.
2.2.2. PTSD symptoms
PTSD symptom severity was measured using the PTSD Checklist (PCL-5), which is a 20-item self-report scale that measures DSM-5 PTSD symptoms in the past month (Blevins, Weathers, Davis, Witte, & Domino, Citation2015). Items ask respondents to rate the degree to which they were bothered by symptoms using 5-point scales ranging from ‘not at all’ (0) to ‘extremely’ (4). The PCL-5 has demonstrated good internal consistency, convergent and discriminant validity, and strong structural validity based on confirmatory factor analysis (Blevins et al., Citation2015). Participants were asked to answer PCL-5 items with reference to their most traumatic military experience.
A provisional diagnosis of ICD-11 PTSD was made if participants reported a score of 2 (‘moderately’) or higher on at least one of the two items measuring re-experiencing (PCL-5 item 2 and 3), avoidance (PCL-5 item 6 and 7), and sense of threat (PCL-5 items 17 and 18), and did not exhibit significant DSO features (see below). This subset of PCL-5 items was used to make a provisional ICD-11 PTSD diagnosis as they best relate to the core ICD-11 PTSD criteria, i.e. re-experiencing, avoidance and heightened sense of threat (see Barbano et al., Citation2019; Cloitre et al., Citation2018).
2.2.3. Disturbance in Self-Organisation (DSO)
DSO symptoms were measured using a preliminary version of the DSO subscale of the International Trauma Questionnaire (ITQ; Cloitre et al., Citation2018). This preliminary version (Cloitre, Roberts, Bisson, & Brewin, Citation2014) was provided by the ITQ authors in advance of its publication, and the final published version of the scale is a subset of the DSO items provided in the draft measure – only the items included in the final measure were included for analysis in this study. This subscale measure comprises six items, with two items each measuring affective dysregulation, negative self-concept and disturbances in relationships, as well as three linked items addressing functional impairment. See for a full list of scale items. Item responses are scored on a 5-point scale ranging from ‘not at all’ (0) to ‘extremely’ (4), and preliminary research indicates the 6-item scale has good structural validity and favourable psychometric properties (Cloitre et al., Citation2018; Shevlin et al., Citation2018). There is early evidence for the validity of the ITQ and its ability to distinguish between PTSD and CPTSD within veteran populations (Murphy et al., Citation2020). It should be noted that the PTSD items of the ITQ were not provided in advance – as such, the relevant items on the PCL-5 were used to measure PTSD symptoms instead.
Table 1. ITQ (Cloitre et al., Citation2018) items used to measure DSO symptoms
A provisional diagnosis of CPTSD was made if participants met criteria for ICD-11 PTSD using the subset of PCL-5 items and also met criteria for DSO symptom clusters according to the subscale measure of the ITQ. Consistent with the approach used in the ITQ validation study (Cloitre et al., Citation2018), a positive DSO screen required that participants report scores of 2 (‘moderately’) or higher on at least one of the two items assessing each DSO symptom feature (affective dysregulation, negative self-concept, disturbances in relationships), and at least one of the three items assessing functional impairment. Supplementary analyses investigating the impact of treatment specifically on DSO symptoms used the sum of each individual’s scores across all six DSO-related items, where potential scores could range from 0 to 24.
2.2.4. Psychological distress
The Kessler Psychological Distress Scale (K10; Kessler et al., Citation2002) comprises 10 items assessing general psychological distress, which are scored on a 5-point scale ranging from ‘None of the time’ (1) to ‘All of the time’ (5). Items are summed to produce a total score, where the maximum score of 50 indicates severe distress and the minimum of 10 indicates no distress. The K10 has shown high levels of internal consistency and concurrent validity (Hides et al., Citation2007), and internal reliability in this sample was calculated at intake as α = .90.
2.2.5. Quality of life
Quality of life was assessed using the ‘Relationships’ and ‘Mental Health’ subscales of the Assessment of Quality of Life Questionnaire – 4D (AQOL-4D; Hawthorne, Richardson, & Osborne, Citation1999), which consist of 3 items each. These subscales were chosen for this study as they were expected to be most sensitive to symptom change, whereas the ‘Senses’ and ‘Independent Living’ subscales were not included as they were not considered conceptually relevant, and no changes were expected as a result of treatment or PTSD symptom exacerbation. Each item is scored on a scale ranging from 1 to either 4 or 5, and a total score for each scale is produced from summing item scores within that domain. Higher scores on the AQOL signify poorer quality of life. The AQOL-4D has excellent psychometric properties and high levels of construct validity (Hawthorne, Richardson, & Day, Citation2001). Mean inter-item correlations were used to index item homogeneity for these subscales since Cronbach’s alpha is biased with small numbers of items. Values above .20 indicate acceptable levels of homogeneity (Briggs & Cheek, Citation1986). Both the Mental Health (Mean r = .35) and Relationships (Mean r = .21) subscales displayed acceptable properties in this sample at treatment intake.
2.2.6. Anxiety and depressive symptoms
The Hospital Depression and Anxiety Scale (HADS; Zigmond & Snaith, Citation1983) comprises 14 items, which form two subscales of seven items each, assessing anxiety and depressive symptoms, respectively. For each question, participants indicate the reply that is closest to how they have felt in the past week. Items are rated on a scale from 0 to 3, and form a score of 0–21 for each subscale. The HADS has demonstrated high concurrent validity and internal reliability (Bjelland, Dahl, Haug, & Neckelmann, Citation2002). Internal reliability was calculated as α = .80 for the anxiety subscale and α = .74 for the depression subscale.
2.3. Data analysis
Data-file preparation and preliminary analyses were conducted using SPSS Version 25, while subsequent analyses used Program R 3.5.1 and MPlus Version 8. Preliminary analyses involved screening for out of range values and description of missing data. This included examination of any systematic patterns of missing data over time, through a series of logistic regression analyses which quantified associations with loss to follow-up and treatment intake measures of age, ex-serving (versus currently serving), marital and employment status, as well as PTSD symptom severity.
Descriptive statistics (frequencies and proportions) were initially produced for purposes of addressing Aim I, while χ2 tests were used to explore associations with CPTSD and various socio-demographic and service-related characteristics. In order to examine Aim II, participants who received a classification of CPTSD were considered relative to participants with a provisional diagnosis of ICD-11 PTSD. For these groups, descriptive statistics (Means and SDs) were produced at treatment intake, treatment discharge and 3-month post-treatment follow-up, across primary outcome measures including the PCL-5, K10, and the Relationships and Mental Health subscales of the AQOL-4D, and secondary outcome measure, the HADS (depression and anxiety subscales). Inferential tests of between-group differences were conducted at each time point, and comprised independent group t-tests. A series of repeated measures effect size estimates (dRM) with 95% Confidence Intervals (CIs) were then used to quantify the overall magnitude of change for each group over time, and also to inform between-group comparisons in the magnitude of change. These effect size estimates were analogous to Cohen’s d statistic, but were based on formulae for the single-group pre-test-post-test design which standardises the sample mean change by variability in change scores (as opposed to the pooled between-group variability) (Morris & DeShon, Citation2002). These were produced in Program R using the Package ‘effsize’ (Torchiano, Citation2016).
The aforementioned analyses all used pairwise deletion of missing data from loss to follow-up, and further analyses were then conducted using Multiple Imputation (MI) of missing values (across k = 20 data sets). The latter were conducted in MPlus version 8, which was also used to specify a series of linear regression models with imputed datasets in which outcome measures at discharge and 3-month post-treatment were considered as endogenous variables in separate analyses. These were estimated using robust Maximum Likelihood (MLR) estimation, and also specified exogenous variables including intake measures of the outcome variable, and a binary variable indicating CPTSD status. These analyses thus compared CPTSD with ICD-11 PTSD on each outcome measure (i.e. PCL-5, K10, and Relationships and Mental Health subscales of the AQOL-4D), and were equivalent to Analysis of Covariance (ANCOVA) models controlling for scores at intake.
Finally, there were a series of supplementary analyses conducted in order to examine the nature and extent of change in DSO symptoms among participants with CPTSD. For purposes of these exploratory analyses, a summed scale score based on the six DSO items were derived at each time-point, and were treated as an indicator of DSO symptom severity. Descriptive statistics and repeated measures effect size estimates (dRM) were then produced for this measure in order to quantify the magnitude of change in DSO symptoms for the CPTSD group over time.
3. Results
3.1. Missing data analyses
A series of logistic regression analyses were conducted to examine bivariate associations between loss to follow-up and treatment intake measures of age, ex-service (versus currently serving), marital and employment status, as well as PTSD symptom severity. These indicated no significant (p < .05) differences between participants who completed and were lost to follow-up at treatment discharge. However, higher PTSD scores at treatment intake were associated with an increased likelihood of being lost to follow-up at 3 months post-treatment (OR = 1.02), while older age was associated with a decreased likelihood of loss to follow-up at 3 months (OR = .97). These point estimates for the OR were small in magnitude and thus suggested that any potential biases from systematic patterns of missing data were modest.
3.2. Descriptive analyses
Within the current sample of participants with a provisional ICD-11 diagnosis, 21.8% (n = 100) were classified as having ICD-PTSD, and 78.2% (n = 358) were classified as CPTSD. presents descriptive and χ2 analyses of associations with provisional CPTSD (versus ICD-PTSD) across a range of sociodemographic and service-related characteristics. As can be seen, there were no significant differences across participants with CPTSD versus ICD-PTSD according to gender, employment and service status, or any pension-related characteristic. However, there was a significant association observed with marital status, indicating that participants with CPTSD were less likely to be in a marital/de facto relationship (Partnered: 66.5%) when compared to participants with ICD-PTSD (77.0%). Participants with a provisional CPTSD diagnosis also had more severe anxiety and depressive symptoms, as measured by the HADS at intake, when compared to those with ICD-PTSD.
Table 2. Sociodemographics of ICD-PTSD and CPTSD subgroups in a treatment-seeking sample of current and ex-serving military members (n = 458)
3.3. Implications of CPTSD for treatment outcomes
shows descriptive statistics across all outcome measures for participants with ICD-11 CPTSD versus PTSD. At treatment intake, participants with CPTSD, relative to ICD-PTSD, exhibited significantly higher levels of PTSD symptom severity (as measured by the PCL-5), depressive and anxious symptom severity (as measured by the HADS), psychological distress (as measured by the K10), and lower quality of life (as measured by the Relationships and Mental Health subscales of the AQOL-4D). Furthermore, the CPTSD group continued to report higher PTSD severity, depressive and anxious symptom severity, and psychological distress, and lower levels of quality of life, at both treatment discharge and 3-month follow-up. also presents estimates of repeated measure effect size (dRM), along with 95% CIs, which quantify the magnitude of change for both the CPTSD and ICD-PTSD groups over time. As can be seen, the CPTSD group reported levels of change over time across outcomes that were broadly comparable to changes for participants with ICD-PTSD. By way of illustration, the point estimate for dRM indicated substantial reductions in PCL-5 scores for the CPTSD group between intake and discharge (dRM = −0.76), which were similar to changes observed for participants with ICD-PTSD (dRM = −0.81). Both groups then indicated no discernible change between treatment discharge and 3-month follow-up. These approximately parallel changes were notwithstanding that the CPTSD group had significantly higher scores initially, and thus also had higher scores at each post-treatment assessment (i.e. discharge and 3 months follow up; see ). A similar pattern of change was observed for secondary outcome measures of anxiety and depression symptoms; point estimates for DRM indicated reductions in HADS scores for the CPTSD group between intake and discharge (dRM-depression = −0.63, dRM-anxiety = −0.65) which paralleled changes observed for participants in the ICD-PTSD group (dRM-depression = −0.54, dRM-anxiety = −0.52). No discernible change between treatment discharge and 3 months follow-up were observed for either group. Changes in psychological distress between intake and discharge were also comparable across CPTSD (dRM = −0.64) and ICD-PTSD groups (dRM = −0.44), while there were low levels of change across time for both groups when defined by AQOL-4D subscales. Results from follow-up regression analyses (see ) also indicated no significant effects, and thus no discernible differences in treatment response between the ICD-PTSD and CPTSD groups across the primary outcome measures when adjusting for higher levels of intake severity associated with CPTSD.
Figure 2. Course of symptom severity at intake, discharge and 3 months post-treatment for (A). PCL-5 score severity for ICD-11 PTSD and CPTSD groups and (B). Average total DSO score severity for CPTSD group
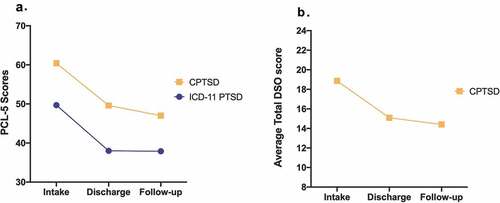
Table 3. Outcome measures for ICD-PTSD and CPTSD groups across intake, discharge and 3-month follow-up
Table 4. Treatment effects for ICD-PTSD and CPTSD groups across primary outcome measures when adjusting for scores at treatment intake
Using the criteria for provisional diagnosis defined in the ITQ validation study (Cloitre et al., Citation2018), we also examined loss of diagnosis between intake and discharge. Amongst those with a provisional ICD-11 CPTSD diagnosis at intake (n = 358), 50.6% (n = 181) retained this diagnosis at discharge, 12% (n = 43) moved to a provisional PTSD diagnosis at discharge, while 37.4% (n = 134) did not report either diagnoses. Comparatively, amongst participants with a provisional ICD-PTSD diagnosis at intake (n = 100), 27% (n = 27) retained this provisional diagnosis at discharge, while 16% (n = 16) moved to a provisional diagnosis of CPTSD, and 57% (n = 57) did not report either diagnosis.
Finally, a supplementary series of analyses were conducted to examine the nature of change in DSO symptoms for participants classified in terms of CPTSD. A summed scale score based on the six DSO items (where potential scores could range between 0 and 24) was derived and treated as an indicator of DSO symptom severity at intake (M = 18.9, SD = 3.4), treatment discharge (M = 15.1, SD = 5.8) and 3-month post-treatment follow-up (M = 14.4, SD = 6.1). Repeated measures effect size estimates were produced and indicated moderate-large reductions in DSO symptom severity from intake to discharge (dRM = −0.70, 95% CI = −0.87 to −0.54), which were maintained with no additional changes from discharge to 3-month follow-up (dRM = −0.07, 95% CI = −0.26 to 0.11).
4. Discussion
The aim of this study was to investigate the relative rates and treatment implications of a CPTSD diagnosis in a treatment-seeking sample of Australian current and ex-serving military members with a provisional ICD-11 PTSD or CPTSD diagnosis. The results indicated that over 75% of this sample met provisional criteria for CPTSD, demonstrating not only a high rate of CPTSD, but also that CPTSD is a more common disorder than ICD-11 PTSD among this group of current and ex-serving military members seeking PTSD treatment.
The findings of this study are in contrast to those of Wolf et al. (Citation2015), who found that ICD-11 PTSD was more prevalent in veterans than CPTSD. This discrepancy may be due to differences across target populations for each of these studies, with Wolf et al.’s sample being non-treatment-seeking veterans, unlike those in the present study. However, the current results are consistent with Letica-Crepulja et al. (Citation2020)’s findings that around 80% of treatment-seeking military veterans met criteria for a probable diagnosis of CPTSD, as well as Folke et al. (Citation2019)’s latent profile analysis which found that treatment-seeking veterans were more often in the CPTSD symptom class than the PTSD symptom class. It may be that while PTSD is comparatively more prevalent among the general population of veterans, the symptom composition that characterise CPTSD may drive treatment-seeking and may thus be the predominant diagnosis for veterans who present to trauma-related clinical services. This is consistent with evidence from other trauma-exposed populations which also suggests higher CPTSD rates among clinical samples when compared to community samples (Brewin et al., Citation2017).
The results also indicated that participants with CPTSD, when compared to ICD-11 PTSD, reported higher PTSD symptom severity, psychological distress, and anxiety and depressive symptoms, as well as lower levels of relationship and mental health dimensions of quality of life, and these relative differences persisted at each post-treatment assessment. Such findings suggest that in this clinical context, the CPTSD diagnosis is capturing participants with both more severe symptoms, as well as more severe impacts in other areas of life (e.g. relationships), associated with DSO symptoms (Karatzias et al., Citation2017).
The current study also found that participant responses to Australian DVA-funded accredited PTSD treatment programmes did not differ significantly between participants who had a provisional diagnosis of ICD-11 PTSD and those who had CPTSD. Rather, participants in both diagnostic categories showed significant and large reductions in PTSD symptomatology and general psychological distress from intake to discharge. Although participants in the CPTSD group displayed higher psychiatric severity across all measures at both intake and discharge, relative to ICD-11 PTSD, there were no discernible differences in the rate of change across time in PTSD severity, quality of life, or general psychological distress, when controlling for initial differences at treatment intake. That is, both the PTSD and CPTSD groups had similar symptom trajectories in response to treatment. Further, the rate at which participants lost their provisional intake diagnoses at discharge was comparable for the CPTSD and PTSD groups. This suggests that while participants with CPTSD had more severe symptomatology overall, they were still able to engage and respond to the standard PTSD treatment. This is consistent with findings from a recent meta-analysis which also suggested standard evidence-based trauma-focussed therapies for PTSD are likely to also be useful for those with CPTSD (Karatzias et al., Citation2019). Interestingly, in the current study, there was a moderate reduction in DSO symptoms from intake to discharge for those in the CPTSD group. While the programmes did not address DSO symptoms directly, these symptoms appear to have been at least partially addressed indirectly through the individual and group-based symptom management and skills training for comorbid issues such as anxiety, anger and depression. It remains unclear whether or not the addition of intervention components that directly target DSO symptoms, such as emotion regulation, negative self-concept and relationship disturbances, would further reduce post-treatment levels of PTSD symptom severity, psychological distress and quality of life beyond the improvements seen with the current standard accredited PTSD treatment programmes.
It is noteworthy that by focusing on only participants who had a provisional ICD-11 PTSD or CPTSD diagnosis, there were high numbers of participants in the accredited PTSD treatment programmes who were excluded from analysis – 63.6% of participants who had a DSM-5 PTSD diagnosis received a provisional ICD-11 PTSD or CPTSD diagnosis and were thus included in the current analyses. This suggests that the ICD-11 taxonomy captured a narrower group of participants than the DSM-5 PTSD diagnosis, which is in line with previous studies that have demonstrated that ICD-11-based PTSD prevalence estimates are significantly lower than those derived from the DSM-5 (Wisco et al., Citation2016). This may mean that trauma-impacted people who might benefit from trauma-focussed therapy may be restricted from accessing appropriate trauma-focussed care and treatment if an ICD-11 diagnosis of PTSD or CPTSD is part of the eligibility criteria.
The findings of this study should be considered in the context of various limitations. First, the data were collected as part of routine quality assurance processes for accredited PTSD treatment programmes, and there was no control condition. Given the lack of a control condition, these results do not preclude the possibility that observed symptom improvements were a reflection of natural fluctuations in the course of chronic PTSD. Second, while eligibility for the programmes was determined by a DSM-5 PTSD diagnosis as measured by the Clinician Administered PTSD Scale for DSM-5 (Weathers et al., Citation2018), the PCL-5 (Blevins et al., Citation2015) was used to determine a provisional diagnosis of ICD-11 PTSD or CPTSD. Although items used as a proxy mapped onto the ICD-11 symptoms, it is possible that the available items did not fully capture the ICD-11 diagnostic construct, and the use of different measures may contribute to the notable drop in numbers from those eligible for the accredited PTSD treatment programmes to those eligible for this study. Third, although statistical models made use of all available data using multiple imputation, this technique provides unbiased estimates when data are missing at random (MAR), and there is no way to test whether this assumption holds in the current data. Fourth, while the Australian PTSD treatment programmes are independently assessed against accreditation standards that specify the components of treatment, these standards are broad so some heterogeneity in programmes content and delivery must be acknowledged.
Future research is required to help maximise treatment outcomes for current and ex-serving military members with CPTSD. The current study points to the high levels of clinical complexity of current and ex-serving military members presenting to standard PTSD programmes in Australia, and while participants respond to treatment with significant reductions in symptoms, those with CPTSD remain highly symptomatic. It is therefore essential to continue exploring how to enhance treatment outcomes in current and ex-serving military members with CPTSD and maximise their end-state functioning. The ISTSS Guidelines Position Paper on CPTSD in Adults presents a number of future research directions to help identify optimal treatments for CPTSD (International Society of Traumatic Stress Studies, Citation2018a). These include (i) comparing standard treatments with protocols that add components targeting DSO symptoms, (ii) testing the order in which multi-component interventions are delivered, and (iii) examining the benefits of delivering multi-component treatments in flexible ways that target the most salient symptoms for a specific patient. Further research into these areas will ultimately assist current and ex-serving military personnel in their recovery from trauma.
Copyright notice
© Commonwealth of Australia 2021
This Work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be reproduced by any process without prior written permission from the Commonwealth. Requests and enquiries concerning reproduction and rights should be directed in the first instance to [the publisher]; or to the Department of Veterans’ Affairs.
Ethical approval
Ethical approval for this study was granted by the Departments of Defence and Veterans’ Affairs Human Research Ethics Committee (DDVA HREC; Protocol Number: 828-16).
Acknowledgments
This Work has been produced with the assistance of funding provided by the Department of Veterans’ Affairs. However, the views expressed in this version of the Work do not necessarily represent the views of the Minister for Veterans’ Affairs or the Department of Veterans’ Affairs. The Commonwealth does not give any warranty nor accept any liability in relation to the contents of this Work.
Data Availability Statement
The data are not publicly available due to privacy or ethical restrictions of data owned by the Australian Government Department of Veterans’ Affairs.
Disclosure statement
The authors have no competing interests to declare in relation to this article.
Additional information
Funding
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC, USA: American Psychiatric Pub.
- Armstrong, R., Phillips, L., Alkemade, N., & Louise O’Donnell, M. (2020). Using latent class analysis to support the ICD-11 complex posttraumatic stress disorder diagnosis in a sample of homeless adults. Journal of Traumatic Stress, 33(5), 677–13. doi:10.1002/jts.22554
- Barbano, A. C., van der Mei, W. F., Bryant, R. A., Delahanty, D. L., deRoon-Cassini, T. A., Matsuoka, Y. J., … Schnyder, U. (2019). Clinical implications of the proposed ICD-11 PTSD diagnostic criteria. Psychological Medicine, 49(3), 483–490.
- Ben‐Ezra, M., Karatzias, T., Hyland, P., Brewin, C. R., Cloitre, M., Bisson, J. I., … Shevlin, M. (2018). Posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) as per ICD‐11 proposals: A population study in Israel. Depression and Anxiety, 35(3), 264–274.
- Bjelland, I., Dahl, A. A., Haug, T. T., & Neckelmann, D. (2002). The validity of the hospital anxiety and depression scale: An updated literature review. Journal of Psychosomatic Research, 52(2), 69–77.
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM‐5 (PCL‐5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498.
- Brewin, C. R., Cloitre, M., Hyland, P., Shevlin, M., Maercker, A., Bryant, R. A., … Rousseau, C. (2017). A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clinical Psychology Review, 58, 1–15.
- Briggs, S. R., & Cheek, J. M. (1986). The role of factor analysis in the development and evaluation of personality scales. Journal of Personality, 54(1), 106–148.
- Cloitre, M. (2015). The “one size fits all” approach to trauma treatment: Should we be satisfied? European Journal of Psychotraumatology, 6(1), 27344.
- Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4(1), 20706.
- Cloitre, M., Garvert, D. W., Weiss, B., Carlson, E. B., & Bryant, R. A. (2014). Distinguishing PTSD, complex PTSD, and borderline personality disorder: A latent class analysis. European Journal of Psychotraumatology, 5(1), 25097.
- Cloitre, M., Roberts, N. P., Bisson, J. I., & Brewin, C. R. (2014). ICD-11 trauma questionnaire. Unpublished Measure.
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The International Trauma Questionnaire: Development of a self‐report measure of ICD‐11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546.
- De Jongh, A., Resick, P. A., Zoellner, L. A., Van Minnen, A., Lee, C. W., Monson, C. M., … Feeny, N. (2016). Critical analysis of the current treatment guidelines for complex PTSD in adults. Depression and Anxiety, 33(5), 359–369.
- De Wind, E. (1972). Persecution, aggression and therapy. International Journal of Psycho-Analysis, 53, 173–177.
- Department of Veterans’ Affairs. (2015). National accreditation standards for trauma recovery programmes - posttraumatic stress disorder. Day programmes. Version 1.0. Canberra, Australia: Author.
- Elklit, A., Hyland, P., & Shevlin, M. (2014). Evidence of symptom profiles consistent with posttraumatic stress disorder and complex posttraumatic stress disorder in different trauma samples. European Journal of Psychotraumatology, 5(1), 24221. doi:10.3402/ejpt.v5.24221
- Folke, S., Nielsen, A. B., Andersen, S. B., Karatzias, T., & Karstoft, K.-I. (2019). ICD-11 PTSD and complex PTSD in treatment-seeking Danish veterans: A latent profile analysis. European Journal of Psychotraumatology, 10(1), 1686806.
- Hamblen, J. L., Norman, S. B., Sonis, J. H., Phelps, A. J., Bisson, J. I., Nunes, V. D., … Schnurr, P. P. (2019). A guide to guidelines for the treatment of posttraumatic stress disorder in adults: An update. Psychotherapy, 56(3), 359.
- Hawthorne, G., Richardson, J., & Day, N. A. (2001). A comparison of the Assessment of Quality of Life (AQoL) with four other generic utility instruments. Annals of Medicine, 33(5), 358–370. doi:10.3109/07853890109002090
- Hawthorne, G., Richardson, J., & Osborne, R. (1999). The Assessment of Quality of Life (AQoL) instrument: A psychometric measure of Health-Related Quality of Life. Quality of Life Research, 8(3), 209–224. doi:10.1023/a:1008815005736
- Herman, J. L. (1992). Trauma and recovery: The aftermath of violence–from domestic abuse to political terror. New York, NY: Basic Books.
- Hides, L., Lubman, D. I., Devlin, H., Cotton, S., Aitken, C., Gibbie, T., & Hellard, M. (2007). Reliability and validity of the Kessler 10 and Patient Health Questionnaire among injecting drug users. Australian & New Zealand Journal of Psychiatry, 41(2), 166–168.
- Horowitz, M. (1974). Stress response syndromes: Character style and dynamic psychotherapy. Archives of General Psychiatry, 31(6), 768–781.
- Hyland, P., Ceannt, R., Daccache, F., Daher, R. A., Sleiman, J., Gilmore, B., … Vallières, F. (2018). Are posttraumatic stress disorder (PTSD) and complex-PTSD distinguishable within a treatment-seeking sample of Syrian refugees living in Lebanon? Global Mental Health, 5. doi:10.1017/gmh.2018.2
- Hyland, P., Murphy, J., Shevlin, M., Vallieres, F., McElroy, E., Elklit, A., … Cloitre, M. (2017). Variation in post-traumatic response: The role of trauma type in predicting ICD-11 PTSD and CPTSD symptoms. Social Psychiatry and Psychiatric Epidemiology, 52(7), 727–736.
- Hyland, P., Shevlin, M., Elklit, A., Murphy, J., Vallières, F., Garvert, D. W., & Cloitre, M. (2017). An assessment of the construct validity of the ICD-11 proposal for complex posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 9(1), 1–9. doi:10.1037/tra0000114
- International Society of Traumatic Stress Studies. (2018a). ISTSS guidelines position paper on complex PTSD in adults. Retrieved from http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-andTreatment-Guidelines/ISTSS_CPTSD-Position-Paper-(Adults)_FNL.pdf.aspx
- International Society of Traumatic Stress Studies. (2018b). ISTSS PTSD prevention and treatment guidelines: Methodology and recommendations. Illinois, USA: Author.
- Karatzias, T., & Cloitre, M. (2019). Treating adults with complex posttraumatic stress disorder using a modular approach to treatment: Rationale, evidence, and directions for future research. Journal of Traumatic Stress, 32(6), 870–876. doi:10.1002/jts.22457
- Karatzias, T., Murphy, P., Cloitre, M., Bisson, J., Roberts, N., Shevlin, M., … Hutton, P. (2019). Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychological Medicine, 49(11), 1761–1775. doi:10.1017/S0033291719000436
- Karatzias, T., Shevlin, M., Fyvie, C., Hyland, P., Efthymiadou, E., Wilson, D., … Cloitre, M. (2017). Evidence of distinct profiles of posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD) based on the new ICD-11 trauma questionnaire (ICD-TQ). Journal of Affective Disorders, 207, 181–187.
- Kessler, R. C., Andrews, G., Colpe, L. J., Hiripi, E., Mroczek, D. K., Normand, S.-L., … Zaslavsky, A. M. (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32(6), 959–976.
- Knefel, M., Garvert, D. W., Cloitre, M., & Lueger-Schuster, B. (2015). Update to an evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse by Knefel & Lueger-Schuster (2013): A latent profile analysis. European Journal of Psychotraumatology, 6(1), 25290.
- Knefel, M., & Lueger-Schuster, B. (2013). An evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse. European Journal of Psychotraumatology, 4(1), 22608. doi:10.3402/ejpt.v4i0.22608
- Letica-Crepulja, M., Stevanović, A., Protuđer, M., Grahovac Juretić, T., Rebić, J., & Frančišković, T. (2020). Complex PTSD among treatment-seeking veterans with PTSD. European Journal of Psychotraumatology, 11(1), 1716593.
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., van Ommeren, M., Jones, L. M., … Rousseau, C. (2013). Diagnosis and classification of disorders specifically associated with stress: Proposals for ICD‐11. World Psychiatry, 12(3), 198–206.
- Maercker, A., Hecker, T., Augsburger, M., & Kliem, S. (2018). ICD-11 prevalence rates of posttraumatic stress disorder and complex posttraumatic stress disorder in a German nationwide sample. The Journal Of Nervous And Mental Disease, 206(4), 270–276.
- Marmar, C. R. (1991). Brief dynamic psychotherapy of post-traumatic stress disorder. Psychiatric Annals, 21(7), 405–414.
- Mordeno, I. G., Nalipay, M. J. N., & Mordeno, E. R. (2019). The factor structure of complex PTSD in combat-exposed Filipino soldiers. Psychiatry Research, 278, 65–69. doi:10.1016/j.psychres.2019.05.035
- Morris, S. B., & DeShon, R. P. (2002). Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychological Methods, 7(1), 105.
- Murphy, D., Shevlin, M., Pearson, E., Greenberg, N., Wessely, S., Busuttil, W., & Karatzias, T. (2020). A validation study of the International Trauma Questionnaire to assess post-traumatic stress disorder in treatment-seeking veterans. The British Journal of Psychiatry, 216(3), 132–137.
- National Institute for Health and Care Excellence. (2018). Guideline for post-traumatic stress disorder. London, UK: Author.
- Nickerson, A., Cloitre, M., Bryant, R. A., Schnyder, U., Morina, N., & Schick, M. (2016). The factor structure of complex posttraumatic stress disorder in traumatized refugees. European Journal of Psychotraumatology, 7(1), 33253.
- Niederland, W. G. (1964). Psychiatric disorders among persecution victims: A contribution to the understanding of concentration camp pathology and its after-effects. The Journal Of Nervous And Mental Disease, 139(5), 458–474.
- Palic, S., Zerach, G., Shevlin, M., Zeligman, Z., Elklit, A., & Solomon, Z. (2016). Evidence of complex posttraumatic stress disorder (CPTSD) across populations with prolonged trauma of varying interpersonal intensity and ages of exposure. Psychiatry Research, 246, 692–699.
- Phoenix Australia Centre for Posttraumatic Mental Health. (2013). Australian guidelines for the treatment of acute stress disorder and posttraumatic stress disorder. Melbourne, Australia: Author.
- Shevlin, M., Hyland, P., Roberts, N. P., Bisson, J. I., Brewin, C. R., & Cloitre, M. (2018). A psychometric assessment of Disturbances in Self-Organization symptom indicators for ICD-11 Complex PTSD using the International Trauma Questionnaire. European Journal of Psychotraumatology, 9(1), 1419749.
- Torchiano, M. (2016). Effsize: Efficient effect size computation. R package version 0.6.1. Retrieved from http://CRAN.R-project.org/package=effsize2016
- Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., … Marx, B. P. (2018). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395. doi:10.1037/pas0000486
- Wisco, B. E., Miller, M. W., Wolf, E. J., Kilpatrick, D., Resnick, H. S., Badour, C. L., … Friedman, M. J. (2016). The impact of proposed changes to ICD-11 on estimates of PTSD prevalence and comorbidity. Psychiatry Research, 240, 226–233.
- Wolf, E. J., Miller, M. W., Kilpatrick, D., Resnick, H. S., Badour, C. L., Marx, B. P., … Friedman, M. J. (2015). ICD-11 Complex PTSD in US National and Veteran Samples: Prevalence and Structural Associations with PTSD. Clinical Psychological Science: A Journal of the Association for Psychological Science, 3(2), 215–229. doi:10.1177/2167702614545480
- World Health Organisation. (2018). International statistical classification of diseases and related health problems (11th Revision). Retrieved from https://icd.who.int/
- Zerach, G., Shevlin, M., Cloitre, M., & Solomon, Z. (2019). Complex posttraumatic stress disorder (CPTSD) following captivity: A 24-year longitudinal study. European Journal of Psychotraumatology, 10(1), 1616488. doi:10.1080/20008198.2019.1616488
- Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370.