ABSTRACT
Background: The inclusion of complex post-traumatic stress disorder (CPTSD) in ICD-11 represents a turning point for the field of traumatic stress, with accumulative evidence of this disorder in refugees and displaced populations.
Objective: The objectives of this systematic review are to examine, in refugee and displaced populations: 1) the prevalence of CPTSD; 2) factors contributing to CPTSD; and 3) and associations between CPTSD and other common mental disorders including: PTSD, depression, anxiety and somatisation.
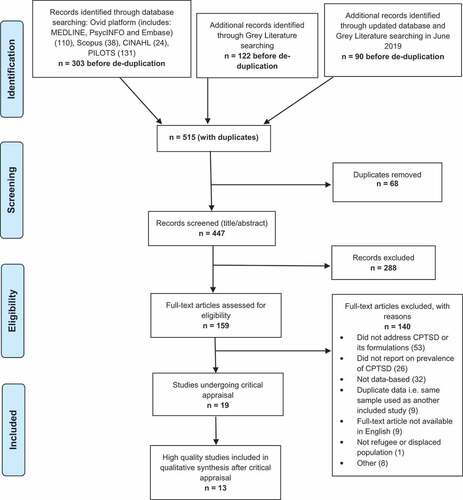
Method: We followed the Joanna Briggs Institute Methodology for Systematic Reviews. Papers published in English language were included, with date of publication between 1987 and June 2019. We searched six relevant databases: MEDLINE, PsycINFO, Embase, Scopus, CINAHL, and PILOTS, and the grey literature. We included observational studies with prevalence data on CPTSD.
Results: 19 articles met all inclusion criteria. Quality assessment was performed on each included study using the Joanna Briggs Institute Critical Appraisal Checklist for Studies Reporting Prevalence Data. Based on this, 13 moderate and high-quality studies were included in our narrative synthesis. The included studies reported prevalence of CPTSD in refugees and displaced populations ranging from 2% to 86%.
Conclusions: Reasons for the wide variation in prevalence may include contextual and geographical differences, the influence of post-migration difficulties, and sample population characteristics such as treatment seeking versus general population. We found higher prevalence rates (range: 16–82%) in more studies with treatment seeking samples, followed by convenience and snowball samples (40–51%), and lower rates in more studies utilising random sampling techniques (2–86%). Consistent with the broader literature, the studies in our review supported an association for complex post-traumatic stress disorder with prolonged, repeated trauma, and post-migration living difficulties, with the latter association being specific to refugee and displaced populations. Further research on this construct in this population group, including effective treatments, is required.
HIGHLIGHTS
• Complex traumatic stress disorder in refugees and forcibly displaced populations.
Antecedentes: la inclusión del trastorno por estrés postraumático complejo (TEPTC) en la CIE-11 representa un punto de inflexión para el campo del estrés traumático, con evidencia acumulativa de este trastorno en refugiados y poblaciones desplazadas.
Objetivo: Los objetivos de esta revisión sistemática son examinar, en poblaciones de refugiados y desplazados: 1) la prevalencia de TEPTC; 2) factores contribuyentes al TEPTC; y 3) y asociaciones entre TEPTC y otros trastornos mentales comunes como: TEPT, depresión, ansiedad y somatización.
Método: Seguimos la Metodología del Instituto Joanna Briggs para Revisiones Sistemáticas. Se incluyeron artículos publicados en idioma inglés, con fecha de publicación entre 1987 y junio de 2019. Se buscó en seis bases de datos relevantes: MEDLINE, PsycINFO, Embase, Scopus, CINAHL y PILOTS, y la literatura gris. Se incluyeron estudios observacionales con datos de prevalencia de TEPTC.
Resultados: 19 artículos cumplieron con todos los criterios de inclusión. Se realizó una evaluación de calidad en cada estudio incluido utilizando la lista de verificación de apreciación crítica del Instituto Joanna Briggs para estudios que informan datos de prevalencia. Sobre esta base, 13 estudios de calidad moderada y alta fueron incluidos en nuestra síntesis narrativa. Los estudios incluidos informaron sobre la prevalencia de TEPTC en refugiados y poblaciones desplazadas en un rango del 2% al 86%.
Conclusiones: Las razones de la amplia variación en la prevalencia pueden incluir diferencias contextuales y geográficas, la influencia de dificultades post-migratorias y características de la muestra de la población, como población general versus en búsqueda de tratamiento. Encontramos tasas de prevalencia más altas (rango: 16-82%) en más estudios con muestras de búsqueda de tratamiento, seguidas de muestras de conveniencia y por bola de nieve (40-51%), y tasas más bajas en más estudios que utilizan técnicas de muestreo aleatorio (2-86%). De forma consistente con la literatura más amplia, los estudios en nuestra revisión apoyaron una asociación para el trastorno de estrés postraumático complejo con trauma prolongado, repetido y dificultades de vida post-migratorias, siendo esta última asociación específica para las poblaciones de refugiados y desplazados. Se requiere mayor investigación sobre este constructo en este grupo de población, incluyendo tratamientos efectivos.
背景: ICD-11中复杂性创伤后应激障碍 (CPTSD) 的纳入, 以及这种疾病在难民和流离失所者中的累积证据, 代表了创伤应激领域的一个转折点。
目的: 本次系统综述的目的是在难民和流离失所者中考查:1) CPTSD的流行率,2) CPTSD的促进因素,3) CPTSD与其他常见精神障碍 (PTSD, 抑郁, 焦虑和躯体化) 的关联。
方法: 我们遵循了乔安娜·布里格斯研究所系统综述方法。纳入以英语发表且发表日期在1987年至2019年6月期间的论文。我们检索了6个相关数据库:MEDLINE, PsycINFO, Embase, Scopus, CINAHL和PILOTS, 以及灰色文献。我们纳入了具有CPTSD流行率数据的观察性研究。
结果: 19篇文章符合全部纳入标准。使用乔安娜·布里格斯研究所报告流行率数据的研究关键评估检查表对每个纳入的研究进行了质量评估。基于此, 我们的叙述性综合中包括13项中等和高质量的研究。纳入的研究报告了难民和流离失所者中从2%到86%不等的CPTSD流行率。
结论: 流行率有大幅差异的原因可能包括背景和地理差异, 移民后困难的影响以及样本人群的特征, 如寻求治疗的和一般人群。我们发现, 在更多寻求治疗样本的研究中报告了较高的流行率 (范围:16- 82%), 其次是方便和滚雪球样本 (40-51%), 而在更多利用随机抽样技术的研究中, 流行率较低 (2-86%) 。与更广泛的文献一致, 我们的研究支持了复杂性创伤后应激障碍与长期, 反复的创伤和移民后生活困难的关联, 后种关联尤其针对难民和流离失所者。需要对此人群中的这个构念, 包括有效的治疗方法, 进行进一步研究。
1. Introduction
A complex form of post-traumatic stress disorder (PTSD) was first described in survivors of World War II concentration camps (Chodoff, Citation1968). It has been well studied in Western populations, including survivors of mass conflict and human rights violations, and survivors of prolonged and repeated interpersonal trauma under conditions of captivity and violence (Herman, Citation1992), with much of the literature focused on sexual assault and childhood abuse (Cloitre et al., Citation2009; Roth, Newman, Pelcovitz, Van Der Kolk, & Mandel, Citation1997). The emerging consensus is that individuals exhibiting a constellation consistent with complex post-traumatic stress disorder (CPTSD) are at risk of psychological comorbidities and severe impairment, to a greater degree than those with PTSD (Dokkedah, Oboke, Ovuga, & Elklit, Citation2015), and may not respond to the conventional trauma-focused clinical treatments (Kissane, Szymanski, Upthegrove, & Katona, Citation2014). Furthermore, past studies indicated that survivors of repeated and prolonged trauma showed a high dropout rate to conventional trauma-focused psychotherapies (Purgato et al., Citation2018), prompting concerns about the utility of the PTSD category, and the associated treatment guidelines, which typically involve exposure-based therapies focusing on single-incident traumatic experiences. Subsequent investigations into complex traumatic stress reactions to prolonged and repeated trauma have gradually shifted the focus in treatment from exposure-based approaches to more integrated approaches focusing on self-regulatory skills-building across affective, interpersonal, and cognitive domains, aimed at restoring the fragmented self, belief systems, and associated schemas.
Prior to the introduction of CPTSD in the International Classification of Diseases 11th edition (ICD-11), there were two precursor formulations of a complex form of PTSD in the literature. Disorder of Extreme Stress Not Otherwise Specified (DESNOS) was one such formulation proposed for inclusion in the Diagnostic and Statistical Manual of Mental Disorders 4th edition (DSM-IV) but was ultimately excluded due to the lack of validity for the proposed category (Roth et al., Citation1997). The second formulation of a complex form of PTSD is Enduring Personality Change After Catastrophic Experience (EPCACE), which was included in the ICD-10 (WHO, Citation1992), and described alterations in self-organisation following trauma. Clinicians working with survivors of complex trauma (e.g. refugees, childhood abuse survivors) at the time recognised the clinical utility of EPCACE, although there was limited empirical evidence for this construct in these populations (Beltran & Silove, Citation1999). In addition to the conventional tripartite constellation, the DSM-5 (APA, Citation2013) broadened the definition of PTSD (Brewin et al., Citation2017), with the addition of a fourth constellation including negative alterations in cognitions and mood, symptoms that relate to impairment in regulatory capacities following exposure to traumatic events, as well as a dissociative subtype.
The inclusion of CPTSD in ICD-11 represents a turning point for the field of traumatic stress (WHO, Citation2018). The ICD-11 formulation of CPTSD was built on the DSM-IV field research, and was guided partially by converging studies undertaken with surveys of expert clinicians (Brewin et al., Citation2017). The diagnosis of ICD-11 CPTSD mandates one or more symptoms from the three domains constituting Disturbances in Self-Organisation (DSO): 1) problems in affect regulation; 2) altered self-concept; and 3) impaired interpersonal relations (WHO, Citation2018), in addition to one or more symptoms of re-experiencing, avoidance, and hyperarousal.
Prompted by the recognition of CPTSD as a new category in the ICD-11, there is now a growing body of studies supporting CPTSD as being a distinct construct that is distinguishable from its PTSD ‘sibling’, and other common mental disorders (CMDs). These studies have been conducted primarily with survivors of interpersonal trauma (Cloitre, Garvert, Brewin, Bryant, & Maercker, Citation2013; Elklit, Hyland, & Shevlin, Citation2014; Sachser, Keller, & Goldbeck, Citation2017), childhood abuse (Cloitre, Garvert, Weiss, Carlson, & Bryant, Citation2014), institutional abuse (Knefel, Garvert, Cloitre, & Lueger-Schuster, Citation2015) and other forms of interpersonal trauma (Karatzias et al., Citation2016; Perkonigg et al., Citation2016). Additional studies have found increased sleep disturbances to be a strong predictor of CPTSD symptoms, with one recent study with Yazidi women showing those in the CPTSD group had a eighteenfold increase in risk of insomnia compared to those in the no-PTSD group (Grossman et al., Citation2019).
In general however, few studies of CPTSD have been conducted with refugee and post-conflict populations. The numbers of refugees and displaced populations have now exceeded 79.5 million people worldwide (UNHCR, Citation2020). Refugees and displaced persons are often exposed to traumatic events including war, torture, and denied access to basic human rights including healthcare and secure housing and furthermore, this population is particularly vulnerable to CPTSD and thus it is important to understand the response pattern in these specific groups. Furthermore, the task of clarifying this issue has been complicated by the successive modifications in modern classification systems of the definition of complex traumatic stress. The heterogeneity in terms used to describe this complex pattern of reactions to extreme trauma has contributed to the wide variations in the prevalence of this putative disorder defined according to previous formulations (DESNOS and EPCACE). The recent efforts by the ICD-11 aimed at a universal category of CPTSD have brought coherence to this body of work, with the accumulation of a small but growing body of literature in recent years examining the prevalence and construct of CPTSD in refugee and displaced populations. A key focus of these studies has investigated the patterns of associations between CPTSD and a broad array of key determinants of relevance to this disorder including Potentially Traumatic Events (PTEs), trauma load, types of trauma, chronicity of PTE exposure, setting, gender, ongoing adversities and deprivations, post-migration living difficulties, and displacement-related factors. As yet however, there have been no systematic attempts at synthesizing this literature.
As indicated, the accumulative evidence supports CPTSD as a disorder on its own with distinctive features – characterized by symptoms of DSO – that set it apart from its PTSD sibling. The common mental disorders that have been frequently examined in relationship to CPTSD include PTSD, depression, anxiety, and somatization, comorbid response patterns that were described as salient in the original formulations of complex PTSD. An additional focus of our review is to examine the pattern of associations of CPTSD with the other comorbid CMDs. Furthermore, the extant studies of CPTSD have primarily used self-report instruments (International Trauma Questionnaire, and clinical diagnostic interviews as case-finding tools, raising questions about the accuracy of deriving diagnostic prevalence from these studies. Hence, for purposes of this review, we refer to probable CPTSD to designate the provisional status of this order.
As indicated, although the evidence base for psychological treatments of complex PTSD has steadily developed in high-income countries involving primarily survivors of childhood abuse and intimate partner violence, there are relatively fewer studies with refugee and forcibly displaced groups in either resettlement countries or conflict zones. There have been promising developments over recent years in this field, but no definitive conclusions can be drawn from the literature given the limited evidence. In parallel however, prevalence data are now accumulating on CPTSD in post-conflict and refugee populations, providing a timely opportunity to examine these issues in our review on CPTSD in these populations.
The objectives of this systematic review are to examine, in refugee and displaced populations: 1) the reported prevalence of CPTSD (based on the ICD-11 definition of CPTSD), and the precursor formulations (DESNOS and EPCACE); 2) factors which may predict CPTSD; and 3) an association between CPTSD and other CMDs including: PTSD, depression, anxiety and somatisation.
2. Methods
2.1. Literature search
We followed the Joanna Briggs Institute (JBI) Methodology for Systematic Reviews (Aromataris & Munn, Citation2017). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. Papers published in English language were included, with date of publication between 1987 and October 2017. The search was repeated in June 2019 to identify eligible papers published since the initial search was conducted.
2.2. Eligibility criteria
This systematic review included refugee or displaced populations exposed to mass conflict and adversity of a recurring, chronic nature. All ages were included. The main diagnostic condition of interest was CPTSD. We also included the precursor formulations of CPTSD prior to the ICD-11 definition: DESNOS and EPCACE. All sources of diagnosis were included, which were standardised questionnaires, self-report symptom checklists, and diagnostic/clinical interviews. Studies from all countries were included. Populations remaining in their country of origin, either exposed to conflict or as internally displaced people, as well as populations displaced to other countries with statuses of: living in a refugee camp, asylum seekers, and permanently resettled, were included. We included study populations recruited using different sampling methods including random samples, snowball samples, and convenience samples; the study populations included members of local communities as well as patients from refugee background undergoing treatment. Both inpatient and outpatient settings were included. We included observational studies that reported on the prevalence of CPTSD. We excluded studies with a sample size smaller than 10, and those that recruited participants with the aim to evaluate treatment.
2.3. Search strategy
The first step involved a limited search of MEDLINE and CINAHL, followed by analysis of the index terms and text words in the title and abstracts. In the second step all identified keywords and index terms were used to search all included databases. The third step was to screen the reference list of all identified papers for additional studies. We searched six relevant databases: MEDLINE, PsycINFO, Embase, Scopus, CINAHL, and PILOTS. The initial keywords used for the search, including full search strategy for one database, PILOTS, is presented as an example in Appendix . Following this, a search of the grey literature was conducted using the keyword search terms.
In the first instance, duplicates were removed from the different database searches. Then two independent reviewers (RM and BM for the first database search, and RM and AW for the grey literature search and second search) screened the title and abstracts of the results to assess for relevance, and discrepancies were discussed with a third reviewer (AT). The full text article was retrieved for all studies that met the inclusion criteria previously established. After this, two independent reviewers (RM and BM for the first database search, and RM and AW for the grey literature search and second search) screened the full text articles for suitability for final inclusion. Discrepancies were resolved by the third reviewer (AT). In addition, reference lists of all included studies were checked for possible studies by one reviewer (RM). Data was extracted by one reviewer (RM) into excel. The table of included studies presented in Appendix summarises this information.
2.4. Study quality
Quality assessment was performed on each included study using the JBI Critical Appraisal Checklist for Studies Reporting Prevalence Data. The checklist and an example can be found in Appendix . Two authors (RM and BM for the first database search, and RM and AW for the grey literature search and second search) independently assessed the studies against these criteria and resolved discrepancies through discussion.
3. Results
3.1. Study selection
The study selection process is shown in the PRISMA diagram in . Database searching identified 303 items, with a further 122 found in searching the grey literature. The second search in 2019 identified an additional 90 items. After duplicates were removed, 447 out of 515 records were identified as potentially relevant. Title and abstracts of these were screened, resulting in 159 that met inclusion criteria. Full-text articles of these 159 items were assessed against eligibility criteria, and 19 articles met all inclusion criteria. Endnote software was used to organise and review the results.
3.2. Study characteristics
The nineteen studies (see Appendix ) included participants from over 30 different countries of origin located in Africa, Middle East, Eastern Europe and Asia Pacific. Ten studies used the ICD-11 based CPTSD formulation (Al Ibraheem, Kira, Aljakoub, & Al Ibraheem, Citation2017; Dokkedah et al., Citation2015; Frost et al., Citation2019; Hecker, Huber, Maier, & Maercker, Citation2018; Hoffman et al., Citation2018; Hyland et al., Citation2018; Kira, Shuwiekh, Rice, Al Ibraheem, & Aljakoub, Citation2017; Nickerson et al., Citation2016; Silove et al., Citation2018; Tay, Rees, Chen, Kareth, & Silove, Citation2015), three studies used formulations that overlapped but preceded ICD-11 CPTSD category, these formulations were derived from the seminal work on complex traumatic syndromes by (Chodoff, Citation1968), (Herman, Citation1992) van der Kolk, and (Roth et al., Citation1997) on the preliminary observations from the DSM-IV field trials (Al-Rasheed, Citation2004; Kissane et al., Citation2014; Kyung, Citation2014), five studies used DESNOS (De Jong, Komproe, Spinazzola, Van Der Kolk, & Van Ommeren, Citation2005; Morina & Ford, Citation2008; Palic & Elklit, Citation2014; Teodorescu, Heir, Hauff, Wentzel-Larsen, & Lien, Citation2012; Weine et al., Citation1998), and one study compared CPTSD (as defined in the literature at the time), DESNOS and EPCACE in the same population (Evans, Citation2012). There was large variation in outcome measure used, fifteen different tools were utilised. The majority of these tools were self-report questionnaires; thus, the diagnosis should be considered provisional in these studies. In contrast, six studies used clinical interviews to make the diagnosis (Al Ibraheem et al., Citation2017; De Jong et al., Citation2005; Kira et al., Citation2017; Silove et al., Citation2018; Tay et al., Citation2015; Teodorescu et al., Citation2012). Fourteen of the reviewed studies reported on predictors related to CPTSD, which included trauma type, trauma count, gender, and post-migration living difficulties (Al Ibraheem et al., Citation2017; Al-Rasheed, Citation2004; Dokkedah et al., Citation2015; Evans, Citation2012; Frost et al., Citation2019; Hecker et al., Citation2018; Hoffman et al., Citation2018; Hyland et al., Citation2018; Kissane et al., Citation2014; Kyung, Citation2014; Palic & Elklit, Citation2014; Silove et al., Citation2018; Tay et al., Citation2015; Teodorescu et al., Citation2012). Ten studies reported on the association between CPTSD and CMDs (Al-Rasheed, Citation2004; Dokkedah et al., Citation2015; Evans, Citation2012; Kira et al., Citation2017; Kyung, Citation2014; Morina & Ford, Citation2008; Nickerson et al., Citation2016; Tay et al., Citation2015; Teodorescu et al., Citation2012; Weine et al., Citation1998) and eight different tools were used to measure the CMDs.
Given the heterogeneity in samples, contexts, and measures of CPTSD, trauma, and CMDs, it was decided that the data could not be meaningfully pooled in a meta-analysis for any of the three objectives, and thus a narrative synthesis would be conducted.
3.3. Risk of bias within studies
The quality criteria ratings suggest that the quality of the studies was moderate, as five or more of the nine criteria were met by majority (68%) of the studies (see results of critical appraisal in Appendix ). The main issues identified by the quality rating tools were: the validity of the measurement tool (most were not validated in the cultural setting) (Al-Rasheed, Citation2004; De Jong et al., Citation2005; Dokkedah et al., Citation2015; Evans, Citation2012; Frost et al., Citation2019; Kissane et al., Citation2014; Kyung, Citation2014; Morina & Ford, Citation2008; Nickerson et al., Citation2016; Palic & Elklit, Citation2014; Teodorescu et al., Citation2012; Weine et al., Citation1998), non-random sampling method (Al Ibraheem et al., Citation2017; Dokkedah et al., Citation2015; Evans, Citation2012; Hecker et al., Citation2018; Hoffman et al., Citation2018; Hyland et al., Citation2018; Kira et al., Citation2017; Kissane et al., Citation2014; Kyung, Citation2014; Nickerson et al., Citation2016; Palic & Elklit, Citation2014; Teodorescu et al., Citation2012; Weine et al., Citation1998), and inadequate sample size (Al Ibraheem et al., Citation2017; Dokkedah et al., Citation2015; Evans, Citation2012; Hecker et al., Citation2018; Hoffman et al., Citation2018; Hyland et al., Citation2018; Kira et al., Citation2017; Kissane et al., Citation2014; Morina & Ford, Citation2008; Palic & Elklit, Citation2014; Weine et al., Citation1998). Based on the quality criteria, we identified a group of thirteen moderate and high-quality studies (those scoring 5 or more) to include in our analysis. The six studies scoring 4 or less were considered low quality and were omitted from our results (Evans, Citation2012; Kissane et al., Citation2014; Kyung, Citation2014; Morina & Ford, Citation2008; Palic & Elklit, Citation2014; Weine et al., Citation1998).
3.4. Results of individual studies
3.4.1. Prevalence
shows the formulations of CPTSD and the outcome measure tool used to evaluate these categories. All studies reported on prevalence of CPTSD or DESNOS, are shown in . The range of prevalence for all formulations was between 2% (De Jong et al., Citation2005) and 86% (Al-Rasheed, Citation2004). Ten studies used the ICD-11 CPTSD provisional diagnosis and reported prevalence rates between 3% and 51% (Al Ibraheem et al., Citation2017; Dokkedah et al., Citation2015; Frost et al., Citation2019; Hecker et al., Citation2018; Hoffman et al., Citation2018; Hyland et al., Citation2018; Kira et al., Citation2017; Nickerson et al., Citation2016; Silove et al., Citation2018; Tay et al., Citation2015). One study used a definition of complex traumatic stress as it was recognized at the time, derived from the work of Herman (1992) and reported a prevalence rate of 86% (Al-Rasheed, Citation2004). Of the two studies examining DESNOS; one found prevalence rates between 2–13% in three different populations (De Jong et al., Citation2005), the other study reported a current prevalence of 16% and a lifetime prevalence of 82% in the same population (Teodorescu et al., Citation2012). This was the only study to report data separately for both current and lifetime prevalence, see . Al-Rasheed (Al-Rasheed, Citation2004) reported a lifetime prevalence of 86%. The ITQ measures symptoms over the past month, and the two studies using this tool (Hecker et al., Citation2018; Hyland et al., Citation2018) reported prevalence rates of 21% and 36%. The remaining majority of studies did not comment on the diagnostic timeframe used however, based on the abovementioned findings we can infer that diagnostic timeframe has a significant influence on prevalence rate and may partially account for the variation in rates across our included studies.
Table 1. Formulation of CPTSD and outcome measure
Table 2. Prevalence according to the different formulations by country of origin and assessment
A noteworthy observation is that most studies yielding provisional diagnoses of CPTSD have primarily used self-report measurement tools. However, when examining the results from the six studies using clinical diagnostic-based interviews as a case-finding tool, there is no greater consistency in the reported prevalence, and no clear discrepancy between prevalence rates found in these studies compared to those using self-report measurements.
We investigated prevalence rates according to sample type and, as expected, found more studies reporting higher prevalence rates in treatment seeking samples, 16–82% (Al Ibraheem et al., Citation2017; Aromataris & Munn, Citation2017; De Jong et al., Citation2005; Kira et al., Citation2017), followed by convenience and snowball samples, 40–51% (Nickerson et al., Citation2016; Silove et al., Citation2018; Tay et al., Citation2015), and more studies reporting lower rates among those utilising random sampling techniques, 2–86%, (Dokkedah et al., Citation2015; Frost et al., Citation2019; Hecker et al., Citation2018; Hyland et al., Citation2018; Kyung, Citation2014; UNHCR, Citation2020). Prevalence rates for all formulations were higher in studies based in the Middle East (36–86%) compared to those based in the Asia Pacific region (2–9%) or resettled in Western countries (5–33%).
3.4.2. Predictors associated with CPTSD
Ten studies reported on predictors of CPTSD (Al Ibraheem et al., Citation2017; Al-Rasheed, Citation2004; Dokkedah et al., Citation2015; Frost et al., Citation2019; Hecker et al., Citation2018; Hoffman et al., Citation2018; Hyland et al., Citation2018; Silove et al., Citation2018; Tay et al., Citation2015; Teodorescu et al., Citation2012), the key findings of these studies, including measurements of predictors associated with CPTSD and statistical tests implemented to quantify those associations, are presented in .
Table 3. Predictors associated with CPTSD
3.4.2.1. Trauma type
Seven studies measured an association between trauma type and CPTSD (Al Ibraheem et al., Citation2017; Al-Rasheed, Citation2004; Dokkedah et al., Citation2015; Frost et al., Citation2019; Hyland et al., Citation2018; Silove et al., Citation2018; Tay et al., Citation2015). Using correlation methods, Al-Rasheed (Al-Rasheed, Citation2004) reported a significant association with armed conflict and war zone trauma, as did Al Ibraheem et al. (Al Ibraheem et al., Citation2017) with Syrian Oppression Experience (a trauma type uniquely defined in the study). Using regression methods three studies have reported a significant association for CPTSD with a wide array of potentially traumatic events (PTEs) of diverse types involving personal injury, witnessing violence, deaths, participating in armed groups and sexual abuse (Dokkedah et al., Citation2015), persecution and displacement, childhood trauma and adversity (Silove et al., Citation2018), and physical abuse, neglect, sexual assault and serious accident (Frost et al., Citation2019). In a series of Multi-Indicators-Multiple-Causes (MIMIC) analyses, Tay et al. (Tay et al., Citation2015) reported a significant, albeit non-specific, association of intrusion and avoidance symptoms with witnessing murder as well as the interaction of witnessing murder and injustice, noting the same symptom domains constituting PTSD were also implicated in these associations. That study however found no association of these traumatic experiences and feelings of injustice with the CPTSD-specific DSO domain. Similarly, Hyland et al. (Hyland et al., Citation2018) found no significant association for CPTSD with forced displacement, exposure to bomb blasts, sudden and unexpected death of a loved one or exposure to warfare ().
3.4.2.2. Trauma count
Three studies tested the association between trauma count and CPTSD (). Teodorescu et al. (Teodorescu et al., Citation2012) used correlation methods and found an association between the total number of the types of PTEs endorsed and the severity of DESNOS (r = 0.326, p < 0.05). Hecker et al. (Hecker et al., Citation2018) found no association (non-significant result) using multiple regression. In a multinomial logistic regression analysis, Frost et al. (Frost et al., Citation2019) found a step-wise association between the mean number of PTEs and the likelihood of CPTSD (two traumas OR = 5.81, three traumas OR = 19.93, four traumas OR = 29.62; p < 0.001) ().
3.4.2.3. Gender
Four of the five studies reporting on gender found no significant association between gender and CPTSD (Dokkedah et al., Citation2015; Hecker et al., Citation2018; Hyland et al., Citation2018; Tay et al., Citation2015). The remaining study by Frost et al. (Frost et al., Citation2019) found that CPTSD prevalence in female participants was significantly higher than male ().
3.4.2.4. Post migration living difficulties and lack of social support
Our reviewed studies found that the lack of social support (Hecker et al., Citation2018) and presence of post-migration living difficulties such as lack of shelter, food, water, clothing and toilets; safety concerns; and limited prospects for vocational activity (Hecker et al., Citation2018; Hoffman et al., Citation2018; Silove et al., Citation2018) are significant predictors of CPTSD ().
3.4.3. Association with CMDs
Five studies quantified statistically the relationship between CPTSD and one or more CMDs (Al-Rasheed, Citation2004; Dokkedah et al., Citation2015; Kira et al., Citation2017; Nickerson et al., Citation2016; Tay et al., Citation2015), as shown in . Using correlation analysis, four of the five reviewed studies found a significant association between CPTSD and PTSD (Al-Rasheed, Citation2004; Dokkedah et al., Citation2015; Kira et al., Citation2017; Nickerson et al., Citation2016; Tay et al., Citation2015) which is as expected considering that CPTSD is an extended construct whereby the PTSD criteria must be initially satisfied. In a confirmatory factor analysis, Nickerson et al. (Nickerson et al., Citation2016) found support for a bi-dimensional model of CPTSD comprising two separate (but correlated) factors comprising both the PTSD and the CPTSD DSO constellations.
Table 4. Association between CPTSD and CMDs
4. Discussion
We found prevalence rates of ICD-11 CPTSD ranging from 3% to 51%. Prevalence of a former definition of CPTSD based on the work of Herman was 86%. The prevalence rates of DESNOS ranged between 2% and 82%. The inclusion of former formulations of the construct could account for some of the wide variation reported, with the higher prevalence rates being attributable to the previous studies preceding the inclusion of CPTSD in ICD-11. Relatively less variability however was recorded amongst the studies that applied the provisional diagnosis based on the ICD-11 criteria, a finding reflected partially in the refinement of the operationalization and the measurement of CPTSD following its formal recognition in the ICD-11.
Prevalence rates for CPTSD and DESNOS were substantially higher in studies involving populations in the Middle East (36–86%) compared to those based in the Asia Pacific region (2–9%) or resettled in Western countries (5–33%). This finding could be related to the combination of a long history of geopolitical instability with recurring periods of armed conflict in the Middle East and North African (MENA) region, with a wide array of ongoing stressors and postmigration living difficulties (PMLDs) impacting on vulnerable populations across a range of settings including refugees, asylum seekers, and forcibly displaced persons.
It is noteworthy that the pivotal role of contextual stressors in CPTSD has been noted in several studies included in this review, with a demonstrable association with CPTSD. Although not mentioned in the studies included in this review, a reasonable postulation is that exposure to these ongoing hardships and PMLDs, such as ongoing exposure to threats, violence, conditions of insecurity, as well as the lack of secure housing, food, water, and access to healthcare and basic services remains elevated in the populations in and North African (MENA) region compared with those in the Western countries. It is therefore possible that the variations in geopolitical, historical, socioeconomic, sociocultural contexts could account partially for the wide variations recorded in prevalence rates of CPTSD across these studies.
The highest reported prevalence rate (86%) was in a group of Kuwaiti women remaining in Kuwait following Iraqi occupation (Al-Rasheed, Citation2004). It is possible that the elevated prevalence in this population could be related to the long legacy of violence and oppression in the region and the preponderance of women in this cohort. Notably, one of the five studies that included gender in our review reported higher rates of CPTSD in female participants (Frost et al., Citation2019), although this finding should be interpreted with caution given the usual caveats associated with retrospective bias and the method used for deriving a probable CPTSD diagnosis, which was based on an amalgamation of PTSD and DSO symptom clusters, the former elicited from a clinical interview measure focusing on Alcohol Use Disorder, whereas the latter was derived from a separate associated interview schedule, both predated the ICD-11 definition of CPTSD.
A previous study by Karatzias et al. (Karatzias et al., Citation2017) reported prevalence of CPTSD using the International Trauma Questionnaire (ITQ) in various Western countries. Prevalence rates generated by the ITQ ranged from 3.3% in a nationally representative sample in the USA, 2–3% in a German sample of the general population, to 76% in a sample of individuals referred for psychological therapy at a specialist trauma centre in Scotland. These findings highlight that variation in prevalence rates of CPTSD may be attributable to features specific to the sample population in addition to the geographical location. Extrapolating these observations into the current review, we found broadly similar patterns in which studies differ in their prevalence rates of CPTSD with studies involving a general refugee population (such as Tay et al. (Tay et al., Citation2015)) yielding a much lower prevalence of 3%, compared to a prevalence of 33% found in studies based on clinic-based samples of patients actively engaged in psychotherapeutic treatment (such as Nickerson et al. (Nickerson et al., Citation2016)).
A key factor that could potentially account for the variation in the reported prevalence rates is whether studies measured and reported CPTSD symptoms based on point prevalence and/or lifetime prevalence. Most studies in our review did not specify the onset of symptoms or the timeframe that was measured, and only one study by Teodorescu et al. (Teodorescu et al., Citation2012) reported both, and found a 16% point prevalence and a 82% lifetime prevalence rate in the same population. Additional factors that could influence prevalence rates include the type, duration, and the number of PTEs witnessed and/or experienced, the influence of PMLDs, and the contextual psychosocial factors (Tay, Rees, Tam, Kareth, & Silove, Citation2019). We however could not adjust for the confounding effects of these variables because most of the studies did not report these factors. Furthermore, the aim of our review is to provide a systematic overview of the literature, rather than a meta-analysis, which precluded meta regression analyses of key predictors of aggregated outcomes, the latter proved to be statistically unviable however considering the substantial heterogeneity in definitions, design, sampling methods, settings, and measurement tools used across studies (see , , ).
Large-scale studies are needed to provide robust estimates of prevalence rates of CPTSD with refugee and forcibly displaced populations across a range of settings including those remaining in prolonged conditions of displacement and deprivation, as well as those seeking treatment in countries of resettlement or transition. Future studies building on the foundation of current research need to exercise additional efforts in formulating, adapting, and testing culturally and contextually valid measurement tools aimed at improving accuracy and replicability of the research across cultures and populations. Further consideration is needed to ensure precision in measurement of point and/or lifetime prevalence of symptoms, as well as the time since trauma and the length of trauma exposure.
The original conception of CPTSD involved prolonged or repeated exposure to extreme interpersonal trauma (Karatzias et al., Citation2019). The studies included in this review reported a multitude of trauma types, with the preponderance of the PTEs endorsed commonly regarded as sustained or repeated forms of interpersonal trauma (see ). In support of our core hypothesis, the majority of the studies in our review found an association between the type of trauma, the number of potentially traumatic events (PTEs), and postmigration living difficulties (PMLDs). Frost et al. (Frost et al., Citation2019) found a typical dose response relationship in that the likelihood of CPTSD increased with an increasing number of exposures to PTEs. Applying latent class analysis approach a recent study by Liddell et al. (Liddell et al., Citation2019) on a traumatized refugee population also found that higher trauma load significantly predicted membership in CPTSD and PTSD classes. These data are consistent with a systematic review by Steel et al. (Steel et al., Citation2009) on populations exposed to mass conflict and displacement, in which exposure to torture and other PTEs accounted for higher rates of PTSD and depression. Contrary to the long standing convention about the female sex conferring a specific vulnerability to CPTSD, the four out of five studies in our review did not identify an association with gender, with only one recording CPTSD to be more prevalent in females.
The studies in our review that reported a significant association of CPTSD with PTSD (Al Ibraheem et al., Citation2017; Al-Rasheed, Citation2004; Nickerson et al., Citation2016), admixture depression/anxiety (Dokkedah et al., Citation2015) and somatisation (Dokkedah et al., Citation2015) are largely expected given the pattern of multiple comorbidities commonly found in refugee and forcibly displaced populations. Notably, results from a psychometric analysis conducted in one study found evidence for CPTSD as a distinct disorder from the other CMDs (Nickerson et al., Citation2016).
From a clinical perspective, further to the development of a research base supporting identification and diagnosis of CPTSD in refugees, effective treatments must be available. A recent review and meta-analysis by Karatzias et al. (Karatzias et al., Citation2019) examined interventions for CPTSD. While recognising the lack of existing research on interventions for this novel condition, they included studies looking at treatments for PTSD and the additional DSO symptoms of CPTSD. Established treatments for PTSD including cognitive behavioural therapy, exposure therapy, and eye movement desensitisation and reprocessing (EMDR) were found to have some effect on disturbed relationships and negative self-concept, but few studies reported on affect dysregulation. The expert opinion guidelines currently used by clinicians in Australia and New Zealand to direct treatment of CPTSD recommend a phase-based treatment approach and are based on research of treatment in individuals exposed to childhood abuse, therefore relevance to refugees is unknown (ACMPH, Citation2013; Cloitre et al., Citation2012). Karatzias et al. (Karatzias et al., Citation2019) provide detailed research priorities for this field, and in addition, while there have been promising developments in the formulation and testing of psychotherapy for CPTSD in the refugee trauma field (Tay et al., Citation2020), future studies are urgently needed on effective interventions that specifically include refugee and displaced populations.
5. Limitations
The wide heterogeneity in sampling methods, study design, sample characteristics, context, setting, case-finding methods, predictor variables measured, precluded the use of meta-analytic and regression-based strategies to derive weighted estimates and further examination of the key predictor variables of relevance to CPTSD. Furthermore, most extant studies did not measure the length of trauma exposure, PMLDs, relevant psychosocial or contextual variables, or other CMDs, making it difficult to ascertain the extent to which these effects influence CPTSD prevalence in refugee populations. An additional caveat is that the majority of the studies using self-report measures did not specify the timeframe or course of symptoms, thus it was unknown whether point or lifetime prevalence was reported. Furthermore, the lack of data reporting on time since traumatic exposure and the duration of exposure should be considered while interpreting the results. Future studies investigating CPTSD in refugees and survivors of complex trauma will need to broaden the scope of assessment to include a core set of predictors of specific relevance to CPTSD such as symptom onset, duration, nature, type of trauma exposure, and associated psychosocial responses. From a clinical perspective, a focus on the psychosocial and interpersonal factors – including attachment patterns, role and identity disruptions, a sense of injustice, and meaning – is thus critical to advancing research in this field especially amongst refugee populations. Furthermore, our review might have missed some relevant studies as it was limited to the English language. Many studies that preceded the inclusion of CPTSD in the ICD-11 had applied a variety of formulations derived from a set of clinical observations by practitioners working with survivors of complex trauma, While we broadened the scope of our review to include all extant formulations, the questions remain about the accuracy of the prevalence generated from the literature. Nevertheless, our review provides the first historical overview of the literature on the evolution of CPTSD, tracing the course of contemporary studies of this newly recognised disorder within refugee and displaced populations.
6. Conclusions
The prevalence of CPTSD and prior formulations in refugees and displaced populations ranged from 2% to 86% in the studies included in our review. Consistent with elsewhere in the literature, the studies in our review supported an association of CPTSD with prolonged, repeated trauma as well as it being more specific to refugee and displaced populations, with PMLDs playing a potential moderating or mediating role post-migration living difficulties. Further research on this construct in this population group, including effective treatments, is required.
6.1. Recommendations for research
The review identifies several key evidence gaps. Future research needs to address (i) the development of culturally validated tools to measure CPTSD in refugee and displaced populations; (ii) the use of consistent measurement tools for CPTSD, trauma and CMDs in research in this field; (iii) studies with prospective designs; (iv) the need to broaden the scope of future studies to include relevant psychosocial factors and other risk factors of specific relevance to CPTSD; (v) studies examining effective treatment of CPTSD in refugees and displaced populations.
Authors’ contributions
The study was designed by AT, RJ and RM. The literature search was conducted by RM with the guidance of a medical librarian. The first database literature screening was conducted independently by RM and BM, with guidance from AT. The grey literature screening was conducted independently by RM and AW, with guidance from AT. The second database and grey literature screening was conducted independently by RM and AW, with guidance from AT. Data extraction, analysis, and draft manuscript was from RM with guidance from AT, RJ and MM. All authors approved the final manuscript.
Acknowledgments
Many thanks to Karen Hill, Reference Librarian, Mental Health (SA Health Library Service), for her guidance of the literature search.
Data availability statement
The data and materials that support the results or analyses are presented and fully available in our paper.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- ACMPH. (2013). Australian guidelines for the treatment of acute stress disorder and posttraumatic stress disorder. Melbourne, Victoria: Australian Centre for Posttraumatic Mental Health (ACPMH). Retrieved from: https://www.ranzcp.org/practice-education/guidelines-and-resources-for-practice/ptsd-endorsed-guidelines
- Al Ibraheem, B., Kira, I. A., Aljakoub, J., & Al Ibraheem, A. (2017). The health effect of the Syrian conflict on IDPs and refugees. Peace and Conflict: Journal of Peace Psychology, 23(2), 140–20.
- Al-Rasheed, M. (2004). Civilian war-zone traumas, complex PTSD, and psychopathology: The case of Kuwaiti women. Dissertation Abstracts International Section A: Humanities and Social Sciences, 65(5–A), 1962.
- APA. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association.
- Aromataris, E., & Munn, Z. (2017). Joanna Briggs Institute reviewer’s manual. Retrieved from https://reviewersmanual.joannabriggs.org/
- Beltran, R. O., & Silove, D. (1999). Expert opinions about the ICD-10 category of enduring personality change after catastrophic experience. Comprehensive Psychiatry, 40(5), 396–403.
- Brewin, C. R., Cloitre, M., Hyland, P., Shevlin, M., Maercker, A., Bryant, R. A., Reed, G. M. (2017). A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clinical Psychology Review, 58, 1–15.
- Chodoff, P. (1968). Late effects of the concentration camp syndrome. Archives of General Psychiatry, 8, 323–333.
- Cloitre, M., Courtois, C. A., Ford, J. D., Green, B. L., Alexander, P., Briere, J., Van der Hart, O. (2012). The ISTSS expert consensus treatment guidelines for complex PTSD in adults. Retrieved from http://www.istss.org/ISTSS_Main/media/Documents/ISTSS-Expert-Consensus-Guidelines-For-Complex-PTSD-Updated-060315.pdf
- Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4(1), 20706.
- Cloitre, M., Garvert, D. W., Weiss, B., Carlson, E. B., & Bryant, R. A. (2014). Distinguishing PTSD, complex PTSD, and borderline personality disorder: A latent class analysis. European Journal of Psychotraumatology, 5(1), 25097.
- Cloitre, M., Stolbach, B. C., Herman, J. L., van der Kolk, B., Pynoos, R., Wang, J., Petkova, E. (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22(5), 399–408.
- De Jong, J. T. V. M., Komproe, I. H., Spinazzola, J., Van Der Kolk, B. A., & Van Ommeren, M. H. (2005). DESNOS in three postconflict settings: Assessing cross-cultural construct equivalence. Journal of Traumatic Stress, 18(1), 13–21.
- Dokkedah, S., Oboke, H., Ovuga, E., & Elklit, A. (2015). ICD-11 trauma questionnaires for PTSD and complex PTSD: Validation among civilians and former abducted children in Northern Uganda. Journal of Psychiatry, 18(6). doi:10.4172/2378-5756.1000335
- Elklit, A., Hyland, P., & Shevlin, M. (2014). Evidence of symptom profiles consistent with posttraumatic stress disorder and complex posttraumatic stress disorder in different trauma samples. European Journal of Psychotraumatology, 5(1), 24221.
- Evans, J. A. (2012). Is complex post traumatic stress disorder a valid construct in refugee survivors of torture and war trauma? Australia: Griffith University.
- Frost, R., Hyland, P., McCarthy, A., Halpin, R., Shevlin, M., & Murphy, J. (2019). The complexity of trauma exposure and response: Profiling PTSD and CPTSD among a refugee sample. Psychological Trauma: Theory, Research, Practice, and Policy, 11(2), 165–175.
- Grossman, E. S., Hoffman, Y. S. G., Shrira, A., Kedar, M., Ben-Ezra, M., Dinnayi, M., & Zivotofsky, A. Z. (2019). Preliminary evidence linking complex-PTSD to insomnia in a sample of Yazidi genocide survivors. Psychiatry Research, 271, 161–166.
- Hecker, T., Huber, S., Maier, T., & Maercker, A. (2018). Differential associations among PTSD and complex PTSD symptoms and traumatic experiences and postmigration difficulties in a culturally diverse refugee sample. Journal of Traumatic Stress, 31(6), 795–804.
- Herman, J. L. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5(3), 377–391.
- Hoffman, Y. S. G., Grossman, E. S., Shrira, A., Kedar, M., Ben-Ezra, M., Dinnayi, M., & Zivotofsky, A. Z. (2018). Complex PTSD and its correlates amongst female Yazidi victims of sexual slavery living in post-ISIS camps. World Psychiatry: Official Journal of the World Psychiatric Association (WPA), 17(1), 112–113.
- Hyland, P., Ceannt, R., Daccache, F., Abou Daher, R., Sleiman, J., Gilmore, B., … Vallières, F. (2018). Are posttraumatic stress disorder (PTSD) and complex-PTSD distinguishable within a treatment-seeking sample of Syrian refugees living in Lebanon? Global Mental Health, 5, e14.
- Karatzias, T., Cloitre, M., Maercker, A., Kazlauskas, E., Shevlin, M., Hyland, P., Brewin, C. R. (2017). PTSD and complex PTSD: ICD-11 updates on concept and measurement in the UK, USA, Germany and Lithuania. European Journal of Psychotraumatology, 8(sup7), 1418103.
- Karatzias, T., Murphy, P., Cloitre, M., Bisson, J., Roberts, N., Shevlin, M., Hutton, P. (2019). Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychological Medicine, 49(11), 1761–1775.. https://doi.org/10.1017/S0033291719000436
- Karatzias, T., Shevlin, M., Fyvie, C., Hyland, P., Efthymiadou, E., Wilson, D., Cloitre, M. (2016). An initial psychometric assessment of an ICD-11 based measure of PTSD and complex PTSD (ICD-TQ): Evidence of construct validity. Journal of Anxiety Disorders, 44, 73–79.
- Kira, I. A., Shuwiekh, H., Rice, K., Al Ibraheem, B., & Aljakoub, J. A. (2017). Threatened identity: The mental health status of Syrian refugees in Egypt and its etiology. Identity, 17(3), 176–190.
- Kissane, M., Szymanski, L., Upthegrove, R., & Katona, C. (2014). Complex posttraumatic stress disorder in traumatised asylum seekers: A pilot study. The European Journal of Psychiatry, 28(3), 137–144.
- Knefel, M., Garvert, D. W., Cloitre, M., & Lueger-Schuster, B. (2015). Update to an evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse by Knefel & Lueger-Schuster (2013): A latent profile analysis. European Journal of Psychotraumatology, 6, 25290.
- Kyung, K. H. (2014). Differences in the symptoms of complex PTSD and PTSD in North Korean defectors by trauma type. Korean Social Sciences Review, 4(1), 65–92.
- Liddell, B. J., Nickerson, A., Felmingham, K. L., Malhi, G. S., Cheung, J., Den, M., Bryant, R. A. (2019). Complex posttraumatic stress disorder symptom profiles in traumatized refugees. Journal of Traumatic Stress, 32(6), 822–832.
- Morina, N., & Ford, J. D. (2008). Complex sequelae of psychological trauma among Kosovar civilian war victims. International Journal of Social Psychiatry, 54(5), 425–436.
- Nickerson, A., Cloitre, M., Bryant, R. A., Schnyder, U., Morina, N., & Schick, M. (2016). The factor structure of complex posttraumatic stress disorder in traumatized refugees. European Journal of Psychotraumatology, 7, 33253.
- Palic, S., & Elklit, A. (2014). Personality dysfunction and complex posttraumatic stress disorder among chronically traumatized Bosnian refugees. Journal of Nervous and Mental Disease, 202(2), 111–118.
- Perkonigg, A., Hofler, M., Cloitre, M., Wittchen, H. U., Trautmann, S., & Maercker, A. (2016). Evidence for two different ICD-11 posttraumatic stress disorders in a community sample of adolescents and young adults. European Archives of Psychiatry and Clinical Neuroscience, 266(4), 317–328.
- Purgato, M., Gastaldon, C., Papola, D., van Ommeren, M., Barbui, C., & Tol, W. A. (2018). Psychological therapies for the treatment of mental disorders in low- and middle-income countries affected by humanitarian crises. The Cochrane Database of Systematic Reviews, 7, Cd011849.
- Roth, S., Newman, E., Pelcovitz, D., Van Der Kolk, B., & Mandel, F. S. (1997). Complex PTSD in victims exposed to sexual and physical abuse: Results from the DSM‐IV field trial for posttraumatic stress disorder. Journal of Traumatic Stress, 10(4), 539–555.
- Sachser, C., Keller, F., & Goldbeck, L. (2017). Complex PTSD as proposed for ICD-11: Validation of a new disorder in children and adolescents and their response to trauma-focused cognitive behavioral therapy. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 58(2), 160–168.
- Silove, D., Rees, S., Mohsin, M., Tam, N., Kareth, M., & Tay, A. K. (2018). Differentiating ICD-11 complex post-traumatic stress disorder from other common mental disorders based on levels of exposure to childhood adversities, the traumas of persecution and postmigration living difficulties among refugees from West Papua. BJPsych Open, 4(5), 361–367.
- Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA, 302(5), 537–549.
- Tay, A. K., Rees, S., Chen, J., Kareth, M., & Silove, D. (2015). The structure of post-traumatic stress disorder and complex post-traumatic stress disorder amongst West Papuan refugees. BMC Psychiatry, 15(111). doi:10.1186/s12888-015-0480-3
- Tay, A. K., Rees, S., Tam, N., Kareth, M., & Silove, D. (2019). Developing a measure of adaptive stress arising from the psychosocial disruptions experienced by refugees based on a sample of displaced persons from West Papua. International Journal of Methods in Psychiatric Research, 28(1), e1770.
- Tay, A. K. M. H., Miah, M. A. A., Balasundaram, S., Ventevogel, P., Badrudduza, M., Badrudduza, M., & Spiegel, P. B. (2020). An integrative adapt therapy for common mental health symptoms and adaptive stress amongst Rohingya, Chin, and Kachin refugees living in Malaysia: A randomized controlled trial. PLoS Medicine, 17(3), e1003073.
- Teodorescu, D. S., Heir, T., Hauff, E., Wentzel-Larsen, T., & Lien, L. (2012). Mental health problems and post-migration stress among multi-traumatized refugees attending outpatient clinics upon resettlement to Norway. Scandinavian Journal of Psychology, 53(4), 316–332.
- UNHCR. (2020). Figures at a glance. Retrived from https://www.unhcr.org/en-au/figures-at-a-glance.html
- Weine, S. M., Becker, D. F., Vojvoda, D., Hodzic, E., Sawyer, M., Hyman, L., & McGlashan, T. H. (1998). Individual change after genocide in Bosnian survivors of “ethnic cleansing”: Assessing personality dysfunction. Journal of Traumatic Stress, 11(1), 147–153.
- WHO. (1992). The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organisation.
- WHO. (2018). World Health Organisation: International statistical classification of diseases and related health problems (11th Revision), Geneva, Switzerland.
Appendix
Table A1. Search strategy for PsycINFO database
Table A2. Example of critical appraisal checklist completed for one study
Table A3. Details of the 19 studies that met inclusion criteria
Table A4. Results of critical appraisal of studies meeting inclusion criteria showing decision to include or exclude from narrative synthesis