ABSTRACT
Background: Potentially traumatic stressors can lead to various transdiagnostic outcomes beyond PTSD alone but no brief screening tools exist for measuring posttraumatic responses in a transdiagnostic manner.
Objective: Assess the psychometric characteristics of a new 22-item transdiagnostic screening measure, the Global Psychotrauma Screen (GPS).
Method: An internet survey was administered with English speaking participants recruited passively via the website of the Global Collaboration on Traumatic Stress (GC-TS) (nGC-TS = 1,268) and actively via Amazon’s MTurk (nMTurk = 1,378). Exploratory factor analysis, correlational analysis, sensitivity and specificity analysis, and comparisons in response between the two samples and between male and female respondents were conducted.
Results: Exploratory factor analysis revealed a single factor underlying symptom endorsements in both samples, suggesting that such problems may form a unitary transdiagnostic, posttraumatic outcome. Convergent validity of the GPS symptom and risk factors was established with measures of PTSD and dissociative symptoms in the MTurk sample. Gender differences were seen primarily at the item level with women more often endorsing several symptoms and specific risk factors in the MTurk sample, and the GC-TS recruited sample endorsed more symptoms and risk factors than the MTurk sample, suggesting that the GPS may be sensitive to group differences. A GPS symptom cut-off score of 8 identified optimized sensitivity and specificity relative to probable PTSD based on PCL-5 scores.
Conclusions: The current results provide preliminary support for the validity of the GPS as a screener for the concurrent measurement of several transdiagnostic outcomes of potentially traumatic stressors and the apparent unifactorial structure of such symptoms is suggestive of a single or unitary posttraumatic outcome. Future research is needed to evaluate whether similarly strong psychometric properties can be yielded in response to completion of the GPS in other languages.
HIGHLIGHTS
Global Psychotrauma Screen (GPS) is validated in English.
Antecedentes: Los factores de estrés potencialmente traumáticos pueden conducir a varios resultados transdiagnósticos más allá del solo diagnóstico de TEPT, pero no existen herramientas de detección breves para medir las respuestas postraumáticas de una manera transdiagnóstica.
Objetivo: Evaluar las características psicométricas de una nueva medida de cribado transdiagnóstico de 22 ítems, El Mapeo Global de Psicotrauma (Global Psychotrauma Screen o GPS en inglés).
Método: Se administró una encuesta por Internet con participantes de habla inglesa reclutados pasivamente a través del sitio web de la Global Collaboration on Traumatic Stress (GC-TS) (nGC-TS = 1,268) y activamente a través de MTurk de Amazon (nMTurk = 1,378). Se realizaron análisis factoriales exploratorios, análisis correlacionales, análisis de sensibilidad y especificidad, y comparaciones en respuesta entre las dos muestras y entre encuestados masculinos y femeninos.
Resultados: El análisis factorial exploratorio reveló un solo factor subyacente a la aprobación de los síntomas en ambas muestras, lo que sugiere que tales problemas pueden formar un resultado postraumático transdiagnóstico unitario. La validez convergente del síntoma GPS y los factores de riesgo se estableció con medidas de TEPT y síntomas disociativos en la muestra de MTurk. Las diferencias de género se observaron principalmente a nivel de ítem y las mujeres a menudo respaldaron varios síntomas y factores de riesgo específicos en la muestra de MTurk, y la muestra reclutada por GC-TS aprobó más síntomas y factores de riesgo que la muestra de MTurk, lo que sugiere que el GPS puede ser sensible a las diferencias de grupo. Una puntuación de corte de síntomas de GPS de 8 identificó una sensibilidad y especificidad optimizadas en relación con el probable TEPT según las puntuaciones de PCL-5.
Conclusiones: Los resultados actuales proporcionan un apoyo preliminar para la validez del GPS como un filtro para la medición concurrente de varios resultados transdiagnósticos de factores estresantes potencialmente traumáticos y la aparente estructura unifactorial de tales síntomas sugiere un resultado postraumático único o unitario. Se necesitan investigaciones futuras para evaluar si se pueden producir propiedades psicométricas igualmente fuertes en respuesta al completar el GPS en otros idiomas.
背景: 潜在的创伤性应激源可导致除PTSD以外的各种跨诊断结果, 但尚无用于以跨诊断方式测量创伤后反应的简短筛查工具。
目的: 评估一项新的22条目跨诊断筛查测量——全球心理创伤筛查 (GPS) 的心理测量学特性。
方法: 在由全球创伤协作网站 (GC-TS) 被动招募 (nGC-TS = 1,268) 及亚马逊MTurk主动招募的 (nMTurk = 1,378) 讲英语的参与者中, 进行了一项互联网调查。进行了探索性因素分析, 相关性分析, 敏感性和特异性分析, 并比较了两个样本之间以及男, 女受访者之间的反应。
结果: 探索性因素分析揭示了两个样本中出现症状的一个单因素, 表明此类问题可能形成单一的跨诊断, 创伤后结果。通过PTSD和MTurk样本中的解离症状的测量确立了GPS症状和风险因素的收敛效度。性别差异主要体现在条目层面, MTurk样本中的女性更常出现一些症状和特定风险因素, 而GC-TS招募的样本中女性出现的症状和风险因素比MTurk样本更多, 这表明GPS可能对组间差异较敏感。通过与基于PCL-5评分可能的PTSD的最优敏感性和特异性相关确定了GPS症状划界分为8。
结论: 目前的结果为GPS作为同时测量潜在创伤应激源几种跨诊断结果的筛查方法的有效性提供了初步的支持, 并且此类症状明显的单因素结构提示了创伤后的单一或统一结果。需要进一步的研究来评估其他语言的GPS完成后是否也有类似强的心理测量学特性。
Several brief measures have been validated for the purposes of screening posttraumatic stress disorder (PTSD) such as the Trauma Screening Questionnaire (Brewin et al., Citation2002) and the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5; Prins et al., Citation2016) (for a review of PTSD screening instruments see Mouthaan, Sijbrandij, Reitsma, Gersons, & Olff, Citation2014). Further, for complex PTSD recently a shortened version of the International Trauma Questionnaire has also been developed (Bondjers et al., Citation2019; Cloitre et al., Citation2018; Shevlin et al., Citation2018).
However, it is widely recognized that the immediate and long-term mental health consequences of exposure to potentially traumatic life events often extend beyond the symptoms of any single psychological disorder, be it PTSD or otherwise (e.g., Clemens et al., Citation2018; Gribble, Goodwin, & Fear, Citation2019; Hoppen & Morina, Citation2019; Kim et al., Citation2019; McLaughlin, Colich, Rodman, & Weissman, Citation2020; Nordin & Perrin, Citation2019; Pietrzak et al., Citation2015; Sambuco, Bradley, Herring, Hillbrandt, & Lang, Citation2020; Zoellner, Pruitt, Farach, & Jun, Citation2014). Rather, response to traumatic stressors tends to follow the principle of multifinality (Cicchetti & Rogosch, Citation1996) from myriad forms of resilience to psychopathology where similar stressors can lead to various transdiagnostic outcomes across different persons and cultures.
To our knowledge there are no currently validated brief screening measures appropriate to the transdiagnostic assessment of trauma-related outcomes. Instead, current transdiagnostic measures are either lengthy and so less appropriate for screening purposes (e.g., the Trauma Symptom Inventory – 2 has 120 items; Briere, Citation2011) or both lengthy and lacking the context of a posttraumatic response (e.g., the Personality Assessment Inventory has 344 items and does not inquire directly about posttraumatic responses; Morey, Citation1991). Screening for potential transdiagnostic mental health consequences of trauma is therefore an essential step towards diagnosis and needs assessment and could enhance prevention or treatment of mental health disorders (Lewis, Roberts, Andrew, Starling, & Bisson, Citation2020; Olff et al., Citation2020; Roberts, Kitchiner, Kenardy, Lewis, & Bisson, Citation2019).
Among other posttraumatic outcomes to screen, anxiety and depression are also very common and one of the currently most common screening tools for these responses is the four item version of the Patient Health Questionnaire (PHQ-4; Kroenke, Spitzer, Williams, & Löwe, Citation2009). Sleep problems can occur as an independent problem but are often assessed within a measure for PTSD, anxiety or depression. Chronic trauma-related dissociative reactions are also important to screen such as can be accomplished by administering a 2-item screener for assessing the derealization and depersonalization symptoms of the dissociative subtype of PTSD (Frewen, Brown, Steuwe, & Lanius, Citation2015). Additional relevant responses to screen for after trauma include substance abuse, possibly as a way of palliative coping with the distressing experience (e.g., Olff, Langeland, & Gersons, Citation2005). Finally, instead of stress reactions some individuals show resilient responses which are equally important to consider such as can be evaluated by the Resilience Evaluation Scale (Van der Meer et al., Citation2018) and other similar survey tools. Further, in addition to psychological outcomes, in order to predict the course of symptoms and vulnerability it would also be helpful to screen for known risk factors such as the occurrence of other stressful events, history of childhood trauma, history of mental illness, and protective factors such as social support and perceived psychological resilience.
A practical problem however is that a very extensive test battery would be needed to assess this wide range of potential reactions to trauma as well as risk or protective factors. This concern owes to the fact that few brief screening tools exist for measuring posttraumatic responses in a transdiagnostic manner that also include measurement of known risk and protective factors. As described in a previous article (Olff et al., Citation2020), we therefore compiled 17 survey items as much as possible from the aforementioned previous screening measures of PTSD, complex PTSD, anxiety, depression, sleep problems, self-injurious behaviour, dissociation, and substance abuse and added five brief descriptions of risk and protective factors. Together, we titled the resulting 22-item survey as a Global Psychotrauma Screen (GPS; Olff et al., Citation2020). The GPS was meant to be a useful screening tool that is sensitive to the presence of symptoms and that would be appropriate to administer in general population studies and with various highly traumatized groups (e.g., after mass trauma, in refugee camps, etc.). With the goal of developing a screening instrument with a preference towards ease of completion ultimately by persons of various languages a dichotomous yes/no format was chosen to ensure understanding and ease of translation as a means of assessing symptom presence instead of a Likert scale format that is normally used to assess severity, frequency or intensity of symptoms (Brewin, Citation2002; Brewin et al., Citation2002). However, to ensure that the GPS measured posttraumatic responses the items are preceded by an introduction on trauma exposure whereby if individuals did not have any trauma or unusual events to report (a minority in the general population (De Vries & Olff, Citation2009; Kessler et al., Citation2017) subsequent assessment could be discontinued.
Based on its item composition (face validity) Olff et al. (Citation2020) recommended that the GPS could either be scored by evaluating response to the single items (e.g., insomnia, substance use, self-harm) or domain scores (i.e., PTSD, complex PTSD, anxiety, depression, dissociation) pertaining to specific posttraumatic responses or, for the sake of parsimony and ease of administration, it could also be scored as a total symptom score (17-item) and risk/protective (5-item) score. However, research is needed to empirically-validate or refine such recommendations beyond only the pilot results tabulating GPS descriptive statistics, internal reliabilities, and correlations with other measures of DSM-5 PTSD or with other subdomain measures that have so far been published (Oe et al., Citation2020; Olff et al., Citation2020).
The aim of this study is therefore to more fully investigate the psychometric properties of the GPS as administered in English to participants aged 18 and older who were recruited online as general population samples of convenience. We conducted an exploratory factor analysis to determine the adequacy of recommending an overall total score assessment for its symptoms as well as correlations and sensitivity and specificity with other self-report measures of PTSD symptoms.
1. Methods
1.1. GPS item selection
The rationale influencing GPS item selection was described previously (Olff et al., Citation2020) but is summarized here for context. In brief, the Global Collaboration on Traumatic Stress (GC-TS), an international, multidisciplinary team of investigators first reached consensus on the domains that would cover a range of posttraumatic responses, as well as risk and protective factors, balancing on the one hand an eye towards being inclusive in the transdiagnostic sense while on the other the practical need for a brief screening instrument that would have clinical utility. Regarding the latter goal, in comparison with the goal of assessment which includes consideration of an indicator of clinical severity, the purpose of screening is to identify individuals at potentially high risk for a specific condition or disorder, while not being definitively diagnositic; as a result, screening tends to employ brief measures as compared with the more complete clinical picture of an individual that is the goal of assessment (American Psychological Association [APA], Citation2014). Accordingly, the primary symptom domains identified were: PTSD, complex PTSD, anxiety, depression, sleep problems, self-injurious behaviour, dissociation, and substance abuse. Further, to include additional outcomes of potential clinical significance beyond those already mentioned it was also decided to query whether ‘other’ (non-specific) physical, emotional or social problems were present for the individual. Moreover, a number of known risk and protective factors were also identified for inclusion: the occurrence of other ongoing stressors, history of childhood trauma exposure, previous mental health diagnosis, present social support and the degree to which persons perceived themselves to be psychologically resilient.
Next, GPS items were compiled as much as possible for each set of posttraumatic responses from existing validated brief screening instruments that were already available in the public domain as referenced previously. Importantly, as such, development of the GPS attempted to avoid ‘reinventing the wheel’ by utilizing already validated screening items compiled from other brief screening tools; to the degree this was possible, the GPS could itself be conceived of as a battery of previously validated screening measures that adopted a common and simplified (yes/no) response format to ensure comparibility across measures, as well as seeking to situate the assessment within a particular timeline (last month) and context (posttraumatic). However, in cases where there was no short screener available, the GC-TS team reached a consensus based decision to sample from highest loading items from factor analyses of more lengthy instruments. In some cases, however, the items decided upon were rephrased in a minor way to improve clarity and to ensure they were crossculturally understandable when it came time to translate the items for use in international studies. Thus the GPS items were gathered from existing screening tools and/or short-versions of questionnaires although it is important to note that this required adaptation to match a common timeframe of assessment, chosen for the GPS to be over the previous month.
First, referring to descriptions of PTSD symptoms, items screening for nightmares, avoidance, hypervigilance and startle reactivity, emotional numbing and detachment, and guilt and self-blame were gathered from the full PC-PTSD-5 (Prins et al., Citation2016) representing GPS items 1–5. Further, to screen for affective dysregulation and negative self-concept as part of the Disturbances in Self-Organization (DSO) of Complex PTSD we selected the two most relevant items from the Brief Symptom Inventory (BSI, i.e., items 13 and 50; Derogatis, Citation1993; Derogatis & Melisaratos, Citation1983) as GPS items 6 and 7. Here we note that while aiming to keep the GPS as brief as possible we determined that it would not be sufficient to measure PTSD symptom responses by a mere one or two items. Instead, multiple survey items were required to screen for the distinct PTSD symptom clusters that have been identified in past research (e.g., reviewed by Armour, Műllerová, & Elhai, Citation2016).
Transdiagnostic assessment of other posttraumatic outcomes beyond PTSD also aimed to be brief. Consequently, to screen for anxiety (GPS 8–9) and depression (GPS 10–11) we included all 4 items of the PHQ-4 (Kroenke et al., Citation2009). Next we screened for sleep problems (GPS 12) based on the single-item expression contained in the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5, item 20). Due to most other measures of self-harm being highly nuanced it was decided to incorporate a more simplified general phrasing to screen for these concerns as GPS problem item 13. Dissociative experiences in the form of derealization and depersonalization were also included (as GPS 14–15; hereafter DPTSD items) based on the singular items validated as an addendum to the PTSD Checklist for DSM-5 (PCL-5) described in Frewen et al. (Citation2015). Further, a single-item screener for substance use problems was included (as GPS 18) based on item 16 from the Utrecht Coping List measuring substance use as a form of palliative coping (Turner, Bryant-Waugh, Peveler, & Bucks, Citation2012). In addition, we included a general item asking about ‘other physical, emotional or social problems’ as GPS item 16 that were not already directly assessed by other items; in the context of clinical use what the patient refers to could be clarified on a case by case basis. Note that, as a result, the GPS was comprised of seven PTSD-DSO items together with ten other symptoms measuring anxiety, depression, sleep problems, self-harm, dissociation, substance abuse, and other (non-specific) physical-emotional-social symptoms, consistent with the goal of instituting a transdiagnostic screening tool. If scoring as a sum across these 17 items, note that relative to any other specific symptom domain, PTSD symptoms would receive a higher weighting. However, considering PTSD specific symptoms vs. the other collective transdiagnostic outcomes measured (i.e., anxiety, depression, sleep problems, self-injurious behaviour, dissociation, and substance abuse), the latter received the higher weighting, again emphasizing the transdiagnostic content of the GPS.
Further, as regards measurement of the recognized list of risk and protective factors (GPS item 18 and items 19–22), we constructed these items through face-valid descriptions in order to maximize clarity, brevity, and ease of translation. These were comprised of 4 risk factors, specifically current (non-traumatic) stressors, lack of social support, childhood trauma history, and previous psychiatric diagnosis or treatment, and a single protective factor, that is, self-reported resilience, which was reverse-scored as rather a lack of experienced resilience. These five items were summed as a single total score in the current study.
The full resulting list of 22 items of the GPS together with instructions is available online (https://www.global-psychotrauma.net/gps) and is included in full in the supplementary materials. Accordingly, the GPS is considered to be in the public domain and free to responsible use by researchers and clinicians alike.
1.1.1. Participants
Individuals were recruited to complete the GPS as an online survey either passively via the websites of the Global Collaboration on Traumatic Stress (GC-TS) (nGC-TS = 1,268) or actively via Amazon’s MTurk (nMTurk = 1,378). The MTurk sample is the same as that briefly described in a prior publication apart from the use of data imputation herein (while not in the previously published analyses; Olff et al., Citation2020) as the cause of some resulting differences in sample size, scoring, and obtained results. Use of the MTurk worker ID prevented such participants from participating more than once in the current study, although the same cannot be guaranteed in the case of the GC-TS sample. Due to the fact the GC-TS sample was recruited via a website featuring content of particular relevance to persons who have experienced trauma exposure, trauma-related symptoms, and possibly other mental health problems, we hypothesized that participants recruited via the GC-TS website might endorse a greater number of GPS symptoms than participants recruited via MTurk.
Demographics and some clinical characteristics are reported in where it can be seen that indeed the GC-TS sample was comprised of a slight majority of persons with currently diagnosed mental health problems (51%) and a strong female majority (81%) whereas approximately one in four persons in the MTurk sample reported having a currently diagnosed mental health problem (28%) and were more evenly distributed by gender (41% female). These differing demographic and clinical profiles together with the distinctive recruitment approach necessitated that results be presented separately for the two samples. It is further important to point out that neither sample were pre-selected for demographics in any way; the only stipulated inclusion criterion was that participants self-reported being aged 18 or older. Further, being that this is an online survey study, it is important to point out that it is not possible to verify participants’ self-reported demographic data (e.g., gender, ethnicity) via any other means.
Table 1. Sample demographics
1.1.2. Procedure and other measures
The procedure received ethical approval at Western University in London, Ontario, Canada and all participants provided informed consent by button press on the internet website before participating after reading a letter of information that fully detailed the study procedure and provided the contact details of the first author in case participants would like to ask further questions before consenting to participate. Both groups of participants were invited to participate in a ‘research study about individuals’ recollections of the quality of their relationships with their family members during childhood, and of relational traumatic experiences occurring during childhood’ in which they would ‘be asked about your current mood, personality, and psychological symptoms.’ The first group (GC-TS) were not compensated and completed the GPS before completing the Childhood Attachment and Relational Trauma Screen (CARTS; Frewen et al., Citation2013); due to complexity of the analysis of the CARTS, however, such results will be reported more fully elsewhere. As to the second group (MTurk), participants were compensated nominally ($1 USD) and completed the GPS in addition to a short of battery of additional questionnaires to assess convergent validity; participants could only participate once for payment via MTurk.
Referring to the additional measures completed by MTurk participants, these included measures of trauma and stressor history, and other measures of PTSD and related symptoms. Specifically, MTurk participants completed the Life Events Checklist for DSM-5 (LEC-5; Gray, Litz, Hsu, & Lombardo, Citation2004; Weathers et al., Citation2013) which assesses participant’s experience of 17 different potentially traumatic events typically encountered during adulthood, such as ‘natural disaster’ (for example, flood, hurricane, tornado, earthquake)’ and ‘fire or explosion’. They also completed an abbreviated 12 item sub-selection of events from the Life Events Survey (LES; Sarason, Johnson, & Siegel, Citation1978) which is a measure of stressful life events that however are unlikely to meet PTSD criterion A as a traumatic life event, for example, including items such as ‘Foreclosure on mortgage or loan’, ‘Trouble with in-laws’ and ‘abortion’; these 12 items were selected from the complete LES as those that were significantly correlated at r ≥ .30 with increasing PTSD symptoms in a prior study (Frewen, Zhu, & Lanius, Citation2019). Further, as a third measure of trauma and stressor exposure, participants completed the Adverse Childhood Experiences Questionnaire (ACE; Felitti et al., Citation1998), which measures participants exposure to ten different categories of abuse, neglect and caregiver dysfunction during childhood. Additionally, regarding other measures of posttraumatic symptoms, participants completed the PTSD Checklist for DSM-5 (PCL-5; Blevins, Weathers, Davis, Witte, & Domino, Citation2015), the International Trauma Questionnaire (ITQ; Cloitre et al., Citation2018), and the Trauma-related Altered States of Consciousness survey (TRASC; Frewen, Brown, & Lanius, Citation2017), the latter a 10-item survey of dissociative experiences. Note further that a single additional brief survey with 33 items that also queried trauma and stressor exposure was developed and piloted for the first time with the MTurk respondents as the last measure of the survey battery, but response to this survey will be described as the principal subject of a future report after additional data is collected.
It is important to point out that for both the GC-TS and MTurk samples participants could take part from anyplace around the globe provided they had an internet connection. However, participation in each sample is likely to be biased due to the recruitment methods employed. In other words, due to the GC-TS website probably being better known to educated mental health professionals with an interest in the study of traumatic stress, participation in that sample is likely to be biased towards inclusiveness of such persons, while on the other, it is known that the majority of participants who access MTurk reside in the USA, despite that participants around the world are able to access the service and there is also a large population of persons who do so residing in India (Litman & Robinson, Citation2020). In either case, as a study limitation it was not possible for us to determine the location where participants completed the surveys.
1.1.3. Analysis
Results presented below are derived separately from two samples (nGC-TC = 1,268; nMTurk = 1,378). Due to an interest in conducting item-level analyses participants had GPS item-level data imputed and were included in the final sample if they had no more than 3 items missing out of the 17 GPS symptom items; this choice was somewhat arbitrary but allowed participants who completed the majority of the test to be included, excluding those with an elevated rate of missingness. Comparably, response to other questionnaires was of interest only at the summary scale level rather than the individual item level, and data was therefore not imputed in these cases but rather only those with full datasets in response to each survey were used (i.e., pairwise deletion). This analytic decision allowed for the inclusion of 97 participants (7.6% of final sample) with any (1–3 GPS items of) missing data and resulted in the removal of only 9 participants in the GC-TS sample. In the MTurk sample, this resulted in the inclusion of 130 participants (9.4% of final sample) with missing data, and removal of 90 participants. Predictive mean matching was used to impute missing data across the 17 GPS items using the R studio software package mice (van Buuren & Groothuis-Oudshoorn, Citation2011). For both samples, twenty-five imputed datasets were created, combined, and this combined imputed dataset was used to compute a tetrachoric correlation matrix. This tetrachoric correlation matrix was used as input for the factor analyses.
First, descriptive statistics at the item level were calculated and compared between male and female respondents using odds ratios. Exploratory factor analysis (EFA) was then used to identify the latent structure and appropriate summative scoring of the 17 GPS symptoms; note that the additional five items intended to screen for risk and protective factors were not included in the EFA in so far as we did not assume these heterogenous items would form a unifactorial structure together with or independent of the 17 symptom items. To assess the factor structure of the GPS, two stages of analyses were conducted. First, exploratory tetrachoric factor analyses were conducted to examine the factor structure of the GPS. Tetrachoric exploratory factor analysis was chosen given dichotomous (yes/no) measurement scales were used and research showing factor solutions based on tetrachoric correlations perform better than product-moment correlations with dichotomous data (Babakus, Ferguson, & Jöreskog, Citation1987; Muthén, Citation1978; Watkins, Citation2018). Principal axis factoring was selected because we aimed to identify constructs underlying factors, and analyses were conducted using oblique rotation methods because multiple factors, if present, were presumed to correlate (Tabachnick & Fidell, Citation2013). Retained factors had to meet minimally the eigenvalue greater than one criterion, and we also attended to the scree plot. To further identify the number of factors to retain in the solution, we employed category probability-adjusted parallel analysis (Horn, Citation1965; Lubbe, Citation2019), Velicer’s MAP criterion, and very simple structure (VSS) informed by guidelines recommending and simulation research supporting their use (Cho, Li, & Bandalos, Citation2009; Choi & Jeong, Citation2019; Courtney, Citation2013; Garrido, Abad, & Ponsoda, Citation2011, Citation2013, Citation2016) including recent simulation research suggesting that accounting for differing rates of category endorsement for categorical items improves the accuracy of parallel analysis (Lubbe, Citation2019). Note however that the procedure developed by Lubbe (Citation2019) does not allow for a correlation matrix to be used as input for parallel analysis, thus in order to use the imputed data we randomly selected five datasets from the 25 imputed datasets as input (5 datasets were used to confirm that the number of factors to retain was not idiosyncratic to a single imputed dataset).
It is important to emphasize that all 17 symptom items were retained in the final recommended use of the GPS. However, specifically in order to assess the adequacy and interpretability of a proposed factor solution, the following information was examined: factor loadings > .3; absence of cross-loading items; the residual correlation matrix, to confirm low residual correlations; variance accounted for by the factors; and the items’ communalities > .4, which can be interpreted as the variance in each item accounted for by the factors. However, given that multiple indices were used to identify the number of factors to retain, it was possible that different indices would suggest differing factor solutions. In this instance, we conducted a series of factor analyses that retained a different number of factors, assessing each factor solution using the above-stated criteria (e.g., factor loadings, examining residual correlation matrix, etc.). Moreover, the factor solutions were compared across the two samples and in the case that more than one factor was suggested for retention, we planned to examine whether the same items loaded onto the factors in both samples. Further, in the case that multiple factors were identified, we planned to submit each factor’s items to further tests of unidimensionality in order to facilitate the interpretation that a single latent construct is indeed responsible for scores on the set of items contained in the factor. Using guidelines recommended by Slocum-Gori and Zumbo (Citation2011), the following statistics were examined to assess unidimensionality in each factor: the variance accounted for by the first factor should be greater than 20% (Reckase, Citation1979); ratio of variance accounted for by a first factor to variance accounted for by a second factor (f1/f2) should be greater than 3; and category probability-adjusted parallel analysis should indicate only a single factor with an eigenvalue above that of randomly generated data. Similarity of the factor loadings across the samples was further assessed using the coefficient of congruence, which has a range of – 1.0 to +1.0. Values of the coefficient of congruence > +.85 suggest similarity in factor loadings while values > +.95 suggest factor loadings can be considered effectively identical (Lorenzo-Seva & Ten Berge, Citation2006). The R psych package was used for the factor analysis (Revelle, Citation2018), the userfriendlyscience package was used to assess the resulting scale reliabilities (coefficient alpha; Peters, Citation2018), and a software program developed by Watkins (Citation2020) was used to compute the coefficient of congruence.
Thereby, concurrent validity of the resulting subscale score(s) was evaluated in reference to Spearman correlation coefficients between the GPS subscale scores and the LES items, LEC-5, ACE, PCL-5, ITQ, DPTSD items and TRASC. Moreover, we used sensitivity and specificity analysis to establish optimal values for establishing concurrent validity with the PCL-5 cut-off score of 33, which is often taken to indicate probable PTSD as assessed by interview (Weathers et al., Citation2013) albeit that Weathers et al. caution that additional research is needed to validate choice of different cut-off scores in different populations and for different screening purposes. Our approach had a preference to maximizing sensitivity relative to specificity as the GPS is considered a screening instrument where we regard false negatives as compared to false positives to be the graver error. Thus, the sample was dichotomized into those with and without a PCL-5 ≥ 33 and GPS symptom sum scores from 1 to 17 were examined in terms of the accuracy of categorizing participants, operationalized as those who score above a given GPS sum score and having a PCL-5 score ≥ 33 as true positive, while those scoring below a given GPS sum score and having a PCL-5 score ≥ 33 as true negative, and so on. Sensitivity, in this context, is defined as the proportion of participants identified as having a PCL-5 score ≥ 33 that score above a given score on the GPS, while specificity is defined as the proportion of participants identified as not having a PCL-5 score ≥ 33 that score below a given score on the GPS. We sought to identify the GPS count score that yielded: 1) minimally 90% sensitivity; 2) minimally 90% specificity; 3) minimally 80% sensitivity while minimizing the difference between sensitivity and specificity.
2. Results
2.1. Item-level endorsement
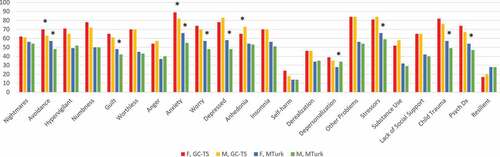
Differences at the individual item (symptom or risk factor) level are illustrated in with statistics fully reported as tables in the Supplementary Materials. Referring to the GC-TS sample, a higher percentage of women endorsed symptoms of avoidance and anxiety, whereas a higher percentage of men endorsed anhedonia. In comparison, within the MTurk sample, a higher percentage of women endorsed symptoms of avoidance, guilt, anxiety, worry, depression, other stressors, childhood trauma history, and the presence of a psychiatric diagnosis, whereas a higher percentage of men endorsed the experience of depersonalization.
2.2. Exploratory factor analysis
Prior to running the factor analyses in both samples, diagnostics of the item data were conducted; the sample size was assumed adequate, assuming a wide communality spread, F2, and p/f ratio of 3 (nGC-TS = 1,268; nMTurk = 1,378, greater than minimum recommended sample of 160; Mundform, Shaw, & Ke, Citation2005); there were no univariate or multivariate outliers; multivariate normality was present; collinearity/singularity were absent (individual items’ unadjusted squared multiple correlations ranged from .34–.81 [GC-TS] and .38–.69 [MTurk]); and the correlation matrices were factorable (KMO = 0.92 [GC-TS] and 0.93 [MTurk]; 97.8% [GC-TS] and 98.5% [MTurk] inter-item correlations were > .30, see Supplemental Materials; inter-item partial correlation matrix showed marked decreases from zero-order correlations). Further, all items had MSA > .60. These results suggest the data were suitable for conducting exploratory factor analysis.
Statistics to identify the number of factors to retain provided the most support for a single factor solution in both samples (i.e., category probability-adjusted parallel analysis, Velicer’s MAP, and very simply structure criterion supported retention of a single factor; for further description please see the Supplemental Materials). Factor loadings for the items in the two samples were above .3 in all cases (see ). The factor accounted for 50.4% (GC-TS sample) and 49.3% (MTurk sample) of the variance in item scores. Notably, the rate of large residual correlations was somewhat elevated (see Supplemental Materials) and the communalities for four items were below .4, suggesting that the presence of multiple factors cannot be fully discounted. This point notwithstanding, given that a one factor solution was supported, the planned second step of analyses to test unidimensionality of factors was not applicable. However, all three criteria for unidimensionality identified above would be met in both samples for the single factor solution (first factor accounts for > 20% of variance; eigenvalue ratio was > 3; and parallel analysis indicates a single factor to retain). Moreover, the coefficient of congruence was Rc = .995, suggesting factor loadings were highly similar across the two samples. Coefficient alpha for the 17 GPS symptom items was .94 in both samples.
Table 2. Factor (pattern) loadings for the GPS
2.3. Sex and group differences
Given that a single factor solution was supported for the GPS symptoms, M and SD were scored accordingly. Referring to differences between men and women, no differences were seen for the GC-TS sample, whereas in the MTurk sample women scored slightly higher specifically on the risk factor subscale score, with a trend towards scoring higher also on the overall symptom score (see ). Further, consistent with predictions, endorsement of GPS scores were higher in the GC-TS sample as compared to the MTurk sample referring to both women and men as regards specifically the symptom (females, t(1636) = 12.04, p < .001, d = .64; males, t(969) = 6.11, p < .001, d = .52) and risk factor sum scores (females, t(1636) = 10.34, p < .001, d = .56; males, t(969) = 8.54, p < .001, d = .69), thus revealing a sensitivity of the GPS to recruitment method.
Table 3. Comparison of females and males on GPS scale scores across two samples
2.4. Concurrent validity of subscale scores and sensitivity-specificity analysis
shows that the GPS symptom total scores correlated with all other symptom measures (PCL-5, ITQ, TRASC), and with measures of trauma and stressor history (LES, LEC-5, ACE; correlations were also seen with the risk factor score. Further, in reference to PCL-5 scores, we determined that a GPS symptom count of 6 was the maximum required to yield minimally 90% sensitivity (sensitivity = .91.2%; specificity = .578; true/false positives = 563/321; true/false negatives = 440/54); a GPS symptom count of 13 was the minimum required to yield minimally 90% specificity (sensitivity = .306; specificity = .930; true/false positives = 189/53; true/false negatives = 709/428); and a GPS symptom count of 8 produced the optimum sensitivity (83.0%) relative to specificity (71.1%) trade off that achieved a sensitivity of minimally 80% (true/false positives = 512/220; true/false negatives = 541/105). Further, the proposed GPS symptom count of 8 had an AUC = .839 for predicting PCL-5 group membership. The sensitivity and specificity values achieved for all possible GPS symptom total scores from 1 to 17 are reported in the Supplementary Materials.
Table 4. Correlations between the GPS and correlates
3. Discussion
Whereas several brief measures exist for PTSD symptom screening, to our knowledge, there were no screening measures validated for screening of transdiagnostic posttraumatic symptoms prior to the conduct of this research that also included screening of relevant risk and protective factors. The aim of this study was therefore to explore the psychometric properties of the GPS (Olff et al., Citation2020), a screening measure developed along these lines, as administered in English to general population samples of online participants aged 18 and older.
In brief, the current results provide initial support for the interpretability of the GPS as administered in English. A single factor solution was identified for the symptoms that it assesses, indicating that a single latent transdiagnostic outcome may partially underlie endorsement of many of the specific, comorbid problems frequently occurring following trauma exposure. Such symptoms, together with measured risk factors, were also seen to correlate with other measures of PTSD symptoms, demonstrating convergent validity. Further, the pattern of factor loadings seems indicative of high loadings for symptoms frequently associated with depression (e.g., numbing, worthlessness, depressed mood, and anhedonia). Cut-off scores were also identified for GPS symptom counts that optimized sensitivity and specificity for identifying persons with probable PTSD based on their scores on the PCL-5, although such scores were identified within the context of online survey administration to general population samples and their generalizability to other populations would require further research. Further, while factor loadings were seen to be similar across the two samples, the GPS was also sensitive to differences in recruitment methods whereby participants who were recruited via the GC-TS website for a study on the late impact of childhood maltreatment scored higher than did participants recruited via MTurk, consistent with the higher proportion of female respondents and a greater preponderance of the former group endorsing currently diagnosed psychiatric problems.
Note that while the single factor structure allows us to use the GPS total symptom scores as a transdiagnostic measure in itself, future research may profitably examine whether the GPS can also be used to examine the risk of developing specific problems by examining response to the items that screen for various specific transdiagnostic outcomes, for example, depression, anxiety, dissociation, insomnia, substance abuse, and self-harm. Consistent with this, whereas the heterogenous, transdiagnostic symptoms that are screened by the GPS did not yield prominent gender differences at the total symptom or risk factor levels, item-level analyses showed that women more often endorsed several cognitive and affective symptoms of avoidance, anxiety, depression, and specific risk factors, consistent with much prior evidence (e.g., Olff, Citation2017; Olff, Langeland, Draijer, & Gersons, Citation2007) and the relevance of also attending to specific outcomes beyond an overall unidimensional symptom burden.
We conclude that the current results provide initial support for the psychometric validity of the GPS as a screener for the concurrent measurement of several transdiagnostic outcomes of traumatic stressors as administered in English. The GPS is easily administered to acquire rapid information concerning myriad problems that often represent the consequence of traumatic life events beyond PTSD alone. Indeed the need for a brief, transdiagnostic measure such as the GPS to screen for posttraumatic outcomes on a global scale has become even more salient in the context of the current COVID-19 pandemic, including administration via the internet as conducted herein as has typically been required of research conducted during the quarantine period; a future study will specifically assess traumatic stress attributable to the COVID-19 pandemic specifically.
Nevertheless, limitations of the present study include lacking the quality assurance often considered particular to the clinical interview method, and the fact that we did not deploy methods to identify participants whose responses were likely dishonest or unreliable in some way, or to assess the English language proficiency of our survey respondents. Moreover, both samples were comprised of a preponderance of Caucasian and highly educated persons, thus we caution against generalizing the current results to other demographic groups. Still, recent research has tended to support the generalizability of findings collected from MTurk participants concerning relationships between PTSD symptoms and other trauma-related transdiagnostic outccomes such as depression and generalized anxiety (e.g., Engle, Talbot, & Samuelson, Citation2020). Further, our measures of the convergent validity of the GPS were largely focused on trauma exposure and PTSD symptom assessments to the neglect of including other measures of transdiagnostic outcomes (e.g., depression); this limitation of the present research should be rectified in future studies.
Future research may profitably continue examining psychometric properties of the GPS, such as cross-validation of the proposed cut-score, further assessment of validity via multi-trait multi-method designs and, beyond the coefficient of congruence measuring similarity of factor loadings, whether measurement demonstrates invariance across samples and sexes. Research is also required to evaluate responses to the GPS collected from other settings, including potentially clinical settings (e.g. at the general practitioner), and to compare the possible clinical significance of responses to the symptom vs. risk/protective factor items of the GPS. However, if similarly strong psychometric properties can be yielded in response to completion of the GPS in other languages, the GPS would seem to be appropriate for screening of several transdiagnostic outcomes of trauma exposure in international and cross-cultural studies. Given that trauma is a global issue and in the end the aim is to develop a screening tool that is culturally sensitive, several other articles are beginning to examine the GPS in other languages and cultures accordingly (Haghi, in prep; Oe et al., Citation2020; Rossi, in prep).
Supplemental Material
Download ()Disclosure statement
The authors report no conflicts of interest relating to this research.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, PF, upon reasonable request.
Supplemental Material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- American Psychological Association. (2014). The American Psychological Association and American Psychological Association Practice Organization Work Group on Screening and Psychological Assessment included members of the Board of Professional Affairs, Committee for the Advancement of Professional Practice, and Committee on Psychological Tests and Assessment. Retrieved from https://www.apaservices.org/practice/reimbursement/billing/assessment-screening
- Armour, C., Műllerová, J., & Elhai, J. D. (2016). A systematic literature review of PTSD's latent structure in the Diagnostic and Statistical Manual of Mental Disorders: DSM-IV to DSM-5. Clinical Psychology Review, 44, 60–13. doi:10.1016/j.cpr2015.12.003
- Babakus, E., Ferguson, C. E., & Jöreskog, K. G. (1987). The sensitivity of confirmatory maximum likelihood factor analysis to violations of measurement scale and distributional assumptions. Journal of Marketing Research, 24, 222–228.
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 281, 489–498. https://doi.org/10.1002/jts.22059
- Bondjers, K., Hyland, P., Roberts, N. P., Bisson, J. I., Willebrand, M., & Arnberg, F. K. (2019). Validation of a clinician-administered diagnostic measure of ICD-11 PTSD and complex PTSD: The international trauma interview in a Swedish sample. European Journal of Psychotraumatology, 10(1), 1665617. doi:10.1080/20008198.2019.1665617
- Brewin, C. R. (2002). Screening for PTSD. The British Journal of Psychiatry: The Journal of Mental Science, 181(6), 535.
- Brewin, C. R., Rose, S., Andrews, B., Green, J., Tata, P., McEvedy, C., … Foa, E. B. (2002). Brief screening instrument for post-traumatic stress disorder. The British Journal of Psychiatry: The Journal of Mental Science, 181(2), 158–162. doi:10.1017/s00071250001j61896
- Briere, J. (2011). Trauma symptom inventory–2 (TSI–2). Odessa, FL: Psychological Assessment Resources.
- Cho, S.-J., Li, F., & Bandalos, D. (2009). Accuracy of the parallel analysis procedure with polychoric correlations. Educational and Psychological Measurement, 69(5), 748–759. doi:10.1177/0013164409332229
- Choi, I., & Jeong, H. (2019). Model selection for factor analysis: Some new criteria and performance comparisons. Econometric Reviews, 38(6), 577–596. doi:10.1080/07474938.2017.1382763
- Cicchetti, D., & Rogosch, F. A. (1996). Equifinality and multifinality in developmental psychopathology. Development and Psychopathology, 8(4), 597–600. doi:10.1017/S0954579400007318
- Clemens, V., Huber-Lang, M., Plener, P. L., Brähler, E., Brown, R. C., & Fegert, J. M. (2018). Association of child maltreatment subtypes and long-term physical health in a German representative sample. European Journal of Psychotraumatology, 9(1), 1510278. doi:10.1080/20008198.2018.1510278
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The international trauma questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546.
- Courtney, M. G. R. (2013). Determining the number of factors to retain in EFA: Using the SPSS R-Menu v2. 0 to make more judicious estimations. Practical Assessment, Research & Evaluation, 18, 1–14.
- de Vries, G. J., & Olff, M. (2009). The lifetime prevalence of traumatic events and posttraumatic stress disorder in the Netherlands. Journal of Traumatic Stress, 22(4), 259–267. https://doi.org/10.1002/jts.20429
- Derogatis, L. R. (1993). Brief symptom inventory: Administration, scoring and procedures manual (4th ed.). Minneapolis, MN: NCS, Pearson, Inc.
- Derogatis, L. R., & Melisaratos, N. (1983). The brief symptom inventory: An introductory report. Psychological Medicine, 13(3), 595–605.
- Engle, K., Talbot, M., & Samuelson, K. W. (2020). Is Amazon’s Mechanical Turk (MTurk) a comparable recruitment source for trauma studies? Psychological Trauma: Theory, Research, Practice and Policy, 12(4), 381–388.
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., … Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. doi:10.1016/s0749-3797(98)00017-8
- Frewen, P., Zhu, J., & Lanius, R. (2019). Lifetime traumatic stressors and adverse childhood experiences uniquely predict concurrent PTSD, complex PTSD, and dissociative subtype of PTSD symptoms whereas recent adult non-traumatic stressors do not: Results from an online survey study. European Journal of Psychotraumatology, 10(1), 1606625. doi:10.1080/20008198.2019.1606625
- Frewen, P. A., Brown, M. F., Steuwe, C., & Lanius, R. A. (2015). Latent profile analysis and principal axis factoring of the DSM-5 dissociative subtype. European Journal of Psychotraumatology, 6(1), 26406. doi:10.3402/ejpt.v6.26406
- Frewen, P. A., Brown, M. F. D., & Lanius, R. A. (2017). Trauma-related altered states of consciousness (TRASC) in an online community sample: Further support for the 4-D model of trauma-related dissociation. Psychology of Consciousness: Theory, Research, and Practice, 4(1), 92–114. doi:10.1037/cns0000091
- Frewen, P. A., Evans, B., Goodman, J., Halliday, A., Boylan, J., Moran, G., … Lanius, R. A. (2013). Development of a Childhood Attachment and Relational Trauma Screen (CARTS): A relational-socioecological framework for surveying attachment security and childhood trauma history. European Journal of Psychotraumatology, 4(1), 20232. doi:10.3402/ejpt.v4i0.20232
- Garrido, L. E., Abad, F. J., & Ponsoda, V. (2011). Performance of Velicer’s minimum average partial factor retention method with categorical variables. Educational and Psychological Measurement, 71(3), 551–570. doi:10.1177/0013164410389489
- Garrido, L. E., Abad, F. J., & Ponsoda, V. (2013). A new look at Horn’s parallel analysis with ordinal variables. Psychological Methods, 18(4), 454–474. doi:10.1037/a0030005
- Garrido, L. E., Abad, F. J., & Ponsoda, V. (2016). Are fit indices really fit to estimate the number of factors with categorical variables? Some cautionary findings via Monte Carlo simulation. Psychological Methods, 21(1), 93–111. doi:10.1037/met0000064
- Gray, M., Litz, B., Hsu, J., & Lombardo, T. (2004). Psychometric properties of the Life Events Checklist. (PDF) Assessment, 11, 330–341. doi:10.1177/1073191104269954
- Gribble, R., Goodwin, L., & Fear, N. T. (2019). Mental health outcomes and alcohol consumption among UK military spouses/partners: A comparison with women in the general population. European Journal of Psychotraumatology, 10(1), 1654781. doi:10.1080/20008198.2019.1654781
- Hoppen, T. H., & Morina, N. (2019). The prevalence of PTSD and major depression in the global population of adult war survivors: A meta-analytically informed estimate in absolute numbers. European Journal of Psychotraumatology, 10(1), 1578637. doi:10.1080/20008198.2019.1578637
- Horn, J. L. (1965). A rationale and test for the number of factors in factor analysis. Psychometrika, 30, 179–185. doi:10.1007/BF02289447
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., … Koenen, K. C. (2017). Trauma and PTSD in the WHO World Mental Health Surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. doi:10.1080/20008198.2017.1353383
- Kim, D., Kim, D., Lee, H., Cho, Y., Min, J. Y., & Kim, S. H. (2019). Prevalence and clinical correlates of dissociative subtype of posttraumatic stress disorder at an outpatient trauma clinic in South Korea. European Journal of Psychotraumatology, 10(1), 1657372. doi:10.1080/20008198.2019.1657372
- Kroenke, K., Spitzer, R. L., Williams, J. B., & Löwe, B. (2009). An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics, 50(6), 613–621. doi:10.1176/appi.psy.50.6.613
- Lewis, C., Roberts, N. P., Andrew, M., Starling, E., & Bisson, J. I. (2020). Psychological therapies for post-traumatic stress disorder in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1729633. doi:10.1080/20008198.2020.1729633
- Litman, L., & Robinson, J. (2020). Conducting online research on Amazon Mechanical Turk and beyond. New York, NY: Sage Publishing. https://us.sagepub.com/en-us/nam/conducting-online-research-on-amazon-mechanical-turk-and-beyond/book257367
- Lorenzo-Seva, U., & Ten Berge, J. M. F. (2006). Tucker’s congruence coefficient as a meaningful index of factor similarity. Methodology: European Journal of Research Methods for the Behavioral and Social Sciences, 2(2), 57–64. doi:10.1027/1614-2241.2.2.57
- Lubbe, D. (2019). Parallel analysis with categorical variables: Impact of category probability proportions on dimensionality assessment accuracy. Psychological Methods, 24(3), 339–351. doi:10.1037/met0000171
- McLaughlin, K. A., Colich, N. L., Rodman, A. M., & Weissman, D. G. (2020). Mechanisms linking childhood trauma exposure and psychopathology: A transdiagnostic model of risk and resilience. BMC Medicine, 18(1), 96. doi:10.1186/s12916-020-01561-6
- Morey, L. C. (1991). Personality assessment inventory (PAI): Professional manual. Odessa, FL: Psychological Assessment Resources.
- Mouthaan, J., Sijbrandij, M., Reitsma, J. B., Gersons, B. P., & Olff, M. (2014). Comparing screening instruments to predict posttraumatic stress disorder. PloS One, 9(5), e97183. doi:10.1371/journal.pone.0097183
- Mundfrom, D. J., Shaw, D. G., & Ke, T. L. (2005). Minimum sample size recommendations for conducting factor analyses. International Journal of Testing, 5(2), 159–168. doi:10.1207/s15327574ijt0502_4
- Muthén, B. (1978). Contributions to factor analysis of dichotomous variables. Psychometrika, 43(4), 551–560. doi:10.1007/BF02293813
- Nordin, L., & Perrin, S. (2019). Pre-treatment pain predicts outcomes in multimodal treatment for tortured and traumatized refugees: A pilot investigation. European Journal of Psychotraumatology, 10(1), 1686807. doi:10.1080/20008198.2019.1686807
- Oe, M., Kobayashi, Y., Ishida, T., Chiba, H., Matsuoka, M., Kakuma, T., … Olff, M. (2020). Screening for psychotrauma related symptoms: Japanese translation and pilot testing of the Global Psychotrauma Screen. European Journal of Psychotraumatology, 11(1), 1810893. doi:10.1080/20008198.2020.1810893
- Olff, M. (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8(4), 1351204. doi:10.1080/20008198.2017.1351204
- Olff, M., Amstadter, A., Armour, C., Birkeland, M. S., Bui, E., Cloitre, M., … Thoresen, S. (2019). A decennial review of psychotraumatology: What did we learn and where are we going? European Journal of Psychotraumatology, 10(1), 1672948. doi:10.1080/20008198.2019.1672948
- Olff, M., Bakker, A., Frewen, P., Aakvaag, H., Ajdukovic, D., Brewer, D., … Schnyder, U. (2020). Screening for consequences of trauma - an update on the global collaboration on traumatic stress. European Journal of Psychotraumatology, 11(1), 1752504. doi:10.1080/20008198.2020.1752504
- Olff, M., Langeland, W., Draijer, N., & Gersons, B. P. (2007). Gender differences in posttraumatic stress disorder. Psychological Bulletin, 133(2), 183–204. doi:10.1037/0033-2909.133.2.183
- Olff, M., Langeland, W., & Gersons, B. P. (2005). The psychobiology of PTSD: Coping with trauma. Psychoneuroendocrinology, 30(10), 974–982. doi:10.1016/j.psyneuen.2005.04.009
- Peters, G. (2018). userfriendlyscience [Computer software]. Retrieved from https://userfriendlyscience.com
- Pietrzak, R. H., Rosenheck, R. A., Cramer, J. A., Vessichio, J. C., Tsai, J., Southwick, S. M., & Krystal, J. H.; VA CSP 504 Collaborative Group. (2015). Elucidating the transdiagnostic dimensional structure of trauma-related psychopathology: Findings from VA cooperative study 504 - risperidone treatment for military service related chronic post traumatic stress disorder. Journal of Affective Disorders, 172, 331–336. doi:10.1016/j.jad.2014.10.025
- Prins, A., Bovin, M. J., Smolenski, D. J., Marx, B. P., Kimerling, R., Jenkins-Guarnieri, M. A., … Tiet, Q. Q. (2016). The primary care PTSD screen for DSM-5 (PC-PTSD-5): Development and evaluation within a veteran primary care sample. Journal of General Internal Medicine, 31(10), 1206–1211.
- Reckase, M. D. (1979). Unifactor latent trait models applied to multifactor tests: Results and implications. Journal of Educational Statistics, 4(3), 207–230. doi:10.3102/10769986004003207
- Revelle, W. (2018). Psych: Procedures for personality and psychological research [Computer software]. https://CRAN.R-project.org/package=psych.
- Roberts, N. P., Kitchiner, N. J., Kenardy, J., Lewis, C. E., & Bisson, J. I. (2019). Early psychological intervention following recent trauma: A systematic review and meta-analysis. European Journal of Psychotraumatology, 10(1), 1695486. doi:10.1080/20008198.2019.1695486
- Sambuco, N., Bradley, M., Herring, D., Hillbrandt, K., & Lang, P. J. (2020). Transdiagnostic trauma severity in anxiety and mood disorders: Functional brain activity during emotional scene processing. Psychophysiology, 57(1), e13349. doi:10.1111/psyp.13349
- Sarason, I. G., Johnson, J. H., & Siegel, J. M. (1978). Assessing the impact of life changes: Development of the Life Experiences Survey. Journal of Consulting and Clinical Psychology, 46(5), 932–946. doi:10.1037//0022-006x.46.5.932
- Shevlin, M., Hyland, P., Roberts, N. P., Bisson, J. I., Brewin, C. R., & Cloitre, M. (2018). A psychometric assessment of disturbances in self-organization symptom indicators for ICD-11 complex PTSD using the international trauma questionnaire. European Journal of Psychotraumatology, 9(1), 1419749. doi:10.1080/20008198.2017.1419749
- Slocum-Gori, S. L., & Zumbo, B. D. (2011). Assessing the unidimensionality of psychological scales: Using multiple criteria from factor analysis. Social Indicators Research, 102(3), 443–461. doi:10.1007/s11205-010-9682-8
- Tabachnick, B. G., & Fidell, L. S. (2013). Using multivariate statistics. Boston: Pearson.
- Turner, H., Bryant-Waugh, R., Peveler, R., & Bucks, R. S. (2012). A psychometric evaluation of an English version of the Utrecht Coping List. European Eating Disorders Review: The Journal of the Eating Disorders Association, 20(4), 339–342. doi:10.1002/erv.2173
- van Buuren, S., & Groothuis-Oudshoorn, K. (2011). mice: Multivariate imputation by chained equations in R.”. Journal of Statistical Software, 45, 1–67. Retrieved from https://www.jstatsoft.org/v45/i03/
- Van der Meer, C. A. I., Te Brake, H., Van der Aa, N., Dashtgard, P., Bakker, A., & Olff, M. (2018). Assessing psychological resilience: Development and psychometric properties of the English and Dutch version of the Resilience Evaluation Scale (RES). Frontiers in Psychiatry, 9. doi:10.3389/fpsyt.2018.00169
- Watkins, M. W. (2018). Exploratory factor analysis: A guide to best practice. Journal of Black Psychology, 44(3), 219–246. doi:10.1177/0095798418771807
- Watkins, M. W. (2020). Rc: Coefficient of congruence [Computer software]. Phoenix, AZ: Ed & Psych Associates, Inc.
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The Life Events Checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov
- Weiss, D. S., & Marmar, C. R. (1997). The impact of event scale-revised. In J. P. Wilson & T. M. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399–411). New York: Guilford Press.
- Zoellner, L. A., Pruitt, L. D., Farach, F. J., & Jun, J. J. (2014). Understanding heterogeneity in PTSD: Fear, dysphoria, and distress. Depression and Anxiety, 31(2), 97–106. doi:10.1002/da.22133