ABSTRACT
Background: Given that the validity of applying complex posttraumatic stress disorder (CPTSD) in nonclinical children remains unclear.
Objectives: The current study aimed to explore the factor structure, discriminant validity, and risk factors of ICD-11 posttraumatic stress disorder (PTSD) and CPTSD using the International Trauma Questionnaire.
Methods: A total of 3478 trauma-exposed Chinese children aged 9–12 years were included in this study. All participants were assessed for PTSD and CPTSD using the International Trauma Questionnaire (ITQ). Confirmatory factor analysis (CFA) was conducted to explore the factor structure of CPTSD in a sample of Chinese children. Latent class analysis (LCA) was employed to evaluate the discriminant validity of CPTSD symptoms. Multinomial logistic regression analyses determined associations between the different classes and traumatic events.
Results: The CFA results showed that the first-order six-factor model was identified as the best-fitting model in Chinese children aged 9–12 years. Four different classes, CPTSD symptoms, PTSD symptoms, disturbances in self-organization (DSO) symptoms, and a low symptom class were found by LCA. Both prolonged interpersonal trauma and other types of trauma were risk factors for the CPTSD class and the PTSD class.
Conclusions: The results of this study partially support the factorial validity and strongly support the discriminant validity of the ICD-11 proposals for PTSD and CPTSD in Chinese children, supporting the conceptualization of PTSD and CPTSD as sibling diagnoses based on the ICD-11. However, findings suggest the need for careful consideration of identified trauma types in the ICD-11 proposals.
HIGHLIGHTS
• The first-order six-factor model was identified as the best-fitting model in Chinese children, indicating that symptom structure among a nonclinical population could somehow be different from that among a clinical population.
• Four different classes were found, including a class with both PTSD and DSO symptoms, a class with PTSD symptoms, a class with DSO symptoms, and a low symptom class.
• More children fell into the PTSD class than into the CPTSD class.
• Both prolonged interpersonal trauma and other types of trauma could predict class differences.
Antecedentes: Dado que la validez de aplicar el diagnóstico de Trastorno de estrés postraumático complejo (TEPT-C) en población infantil no clínica es incierto.
Objetivos: el presente estudio está dirigido a explorar la estructura de factores, validez de discriminación y factores de riesgo del TEPT y TEPT-C de la CIE-11 usando el Cuestionario Internacional de Trauma.
Método: Un total de 3478 niños chinos expuestos a un evento traumático de 9 a 12 años de edad fueron incluidos en este estudio. Todos los participantes fueron evaluados para TEPT y TEPT-C usando el Cuestionario Internacional de Trauma (ITQ por sus siglas en inglés). Se realizó un análisis factorial confirmatorio (CFA por sus siglas en inglés) para explorar la estructura factorial del TEPT-C en una muestra de niños chinos. Se realizó un análisis de clases latentes (LCA) para evaluar la validez de discriminación de los síntomas de TEPT-C. Se realizó una regresión logística multinomial para determinar la asociación entre las diferentes clases y los eventos traumáticos.
Resultados: Los resultados del CFA mostraron que el modelo de seis-factores de primer-orden fue identificado como el modelo más acertado en niños chinos de 9 a 12 años de edad. El LCA encontró cuatro clases diferentes, síntomas de TEPT-C, síntomas de TEPT, alteraciones en la auto-organización (DSO por sus siglas en inglés) y una clase de síntomas baja. Tanto el trauma interpersonal prolongado y otros tipos de trauma fueron factores de riesgo para las clases de TEPT y de TEPT-C.
Conclusiones: Los resultados de este estudio apoyan parcialmente la validez factorial y apoyan contundentemente la validez discriminatoria de las propuestas del CIE-11 para TEPT y TEPT-C en niños chinos, apoyando la conceptualización del TEPT y el TEPT-C como diagnósticos hermanos basados en el CIE-11. Sin embargo, los hallazgos sugieren la necesidad de una consideración cuidadosa de los tipos de trauma identificados en las propuestas del CIE-11.
背景: 由于在非临床儿童中应用复杂性创伤后应激障碍 (CPTSD) 的有效性尚不清楚, 故本研究旨在用国际创伤问卷探讨 ICD-11 创伤后应激障碍 (PTSD) 和 CPTSD 的因子结构, 区分效度和风险因素。
方法: 选取 3478 名 4-5 年级暴露于创伤的中国儿童作为研究对象。使用国际创伤问卷 (ITQ) 对参与者进行 PTSD 和 CPTSD 的评估。并采用验证性因子分析 (CFA) 探讨 CPTSD 在中国儿童中的因子结构, 潜类别分析(LCA)评价 CPTSD 症状的区分效度, 多项 logistic 回归分析不同组别与创伤事件类型之间的联系。
结果: CFA 显示一阶六因素模型是最适合中国 9-12 岁儿童的模型。 LCA 发现了四种不同的组别, 分别为: CPTSD组, PTSD 组, DSO 组和低症状组。长期的人际创伤和其他类型的创伤均是 CPTSD 和 PTSD 组的风险因素。
结论: 研究结果部分支持 ICD-11 提出的 CPTSD 因子结构, 强烈支持将 PTSD 和 CPTSD 概念化为同胞诊断疾病。然而, 需要仔细考虑 ICD-11 中提出的创伤事件类型。
1. Introduction
According to the 11th revision of the International Classification of Diseases (ICD-11) manual, complex posttraumatic stress disorder (CPTSD) is a broader clinical disorder that includes core posttraumatic stress disorder (PTSD) symptoms but is conceptually distinguishable from PTSD on the basis of symptoms that reflect ‘disturbances in self-organization’ (DSO) (Herman, Citation1992; Hyland, Shevlin, Brewin, Cloitre, & Roberts, Citation2017c). A diagnosis of CPTSD requires fulfiling the PTSD criteria in addition to the fulfilment of three impaired symptom clusters: affective dysregulation (AD), negative self-concepts (NSC), and disturbances in relationships (DR) (Brewin et al., Citation2017). Those who had experienced interpersonal traumas that were repeated, prolonged and in multiple forms were more likely to have a CPTSD profile (Cloitre, Garvert, Brewin, Bryant, & Maercker, Citation2013). This proposal was derived from the substantial body of literature suggesting that prolonged exposure to interpersonal traumas, such as sexual, physical, and verbal abuse (Finkelhor, Turner, Shattuck, & Hamby, Citation2013), can have a negative impact on the development of emotional regulatory capacities and result in dysfunctional beliefs about oneself and problematic interpersonal functioning (Dvir, Ford, Hill, & Frazier, Citation2014; Pratchett & Rachel, Citation2011; Shipman, Edwards, Brown, Swisher, & Jennings, Citation2005).
Although most studies have lent support to a CPTSD diagnosis from the construct validity of CPTSD, there are also some divergent findings and limitations to note. First, the number of identified factors is different in the existing literature. In the majority of confirmatory factor analysis (CFA) studies, a two-factor higher-order model was considered to be the best fit, providing support for the distinction between PTSD and DSO, in line with the ICD-11 proposals (Karatzias et al., Citation2016; Kazlauskas, Gegieckaite, Hyland, Zelviene, & Cloitre, Citation2018; Nickerson et al., Citation2016; Shevlin et al., Citation2017). Additionally, some divergent findings are also found in other studies. For example, one study tested the symptom structure and factorial validity of CPTSD in 932 adolescents (Kazlauskas et al., Citation2020). The CFA results showed that a correlated six-factor first-order model was the best fitting model. The same results were also found in a nationally representative sample from Israel. Ben-Ezra, Karatzias, Hyland, Brewin, and Shevlin (Citation2018) found that a correlated first-order model with seven latent variables (re-experiencing, avoidance, sense of threat, hyperactivation, hypoactivation, negative self-concept and disturbed relationship factors) was the best.
Second, it remains controversial whether CPTSD does describe a class of individuals that is different from the class of individuals with PTSD by the individuals having a more ‘complex’ symptom profile, rather than by the individuals responding at different levels of intensity (e.g. low, medium, high) to the same underlying disorder. To date, most studies supported a 3-class solution (PTSD, CPTSD, and low symptoms class) (Cloitre et al., Citation2013; Elklit, Hyland, & Shevlin, Citation2014; Haselgruber, Solva, & Lueger-Schuster, Citation2019; Murphy, Elklit, Dokkedahl, & Shevlin, Citation2016; Perkonigg et al., Citation2016; Zerach, Shevlin, Cloitre, & Solomon, Citation2019). Several studies found a 4-class solution (CPTSD, PTSD, DSO, and low symptom class) (Ben-Ezra et al., Citation2018; Cloitre, Garvert, Weiss, Carlson, & Bryant, Citation2014; Knefel, Garvert, Cloitre, & Luegerschuster, Citation2015; Liddell et al., Citation2019; Perkonigg et al., Citation2016). Also, two studies reported a 2-class solution (CPTSD, PTSD) (Karatzias et al., Citation2017; Sachser, Keller, & Goldbeck, Citation2017). Although these divergent findings may be due to the limitations of latent class analysis (LCA) and latent profile analysis (LPA) in the application, these studies were mostly supportive of the results for distinguishing CPTSD and PTSD symptoms (Achterhof, Huntjens, Meewisse, & Kiers, Citation2019). Only one study called this into question, as it showed a 4-class solution with classes differing in severity (Wolf et al., Citation2015b).
Third, the findings related to the role of trauma type as risk factors of distinguishing CPTSD symptoms and PTSD symptoms have been somewhat controversial. Many studies have supported the ICD-11 proposes and believed that exposure to prolonged or repeated interpersonal traumas were risk factors for CPTSD (Dokkedah, Oboke, Ovuga, & Elklit, Citation2015; Hyland et al., Citation2017a). However, other studies found that individuals with some interpersonal traumas (physical assault, captivity, and sexual assault not by a caregiver, etc.) were more likely to develop PTSD (Cloitre et al., Citation2019; Wolf et al., Citation2015a). For example, one study showed that childhood sexual abuse was more strongly associated with PTSD symptoms than with CPTSD symptoms (Hyland et al., Citation2017a). Another study found similar findings that neither physical abuse nor sexual abuse was risk factors for CPTSD (Ben-Ezra et al., Citation2020). Given the conflicting conclusion and insufficient evidence, further research needs to assess predictors that might enable differentiation between the two.
Why do these differences exist? One main potential explanation is that samples of prior studies had different ages, which may have a significant effect on the necessity of a CPTSD class. When a conceptualization is first introduced, it needs more testing in various populations. To date, the necessity of a CPTSD class has obtained support among various adult samples. However, few studies have investigated its applicability in children. Previous studies have found that cumulative trauma and interpersonal trauma can all predict increasing symptom complexity in children (Hagan, Gentry, Ippen, & Lieberman, Citation2017; Solva, Haselgruber, & Luegerschuster, Citation2020). Due to their high incidence of exposure to multiple, repeated traumas (Liang, Zhou, & Liu, Citation2019), children would be considered at high risk of developing CPTSD given its aetiology and development. To date, only one study has empirically evaluated the factorial and construct validity of ICD-11 CPTSD in foster children (Haselgruber et al., Citation2019). However, the relatively small size and the nature of foster children in this study limited the generalizability of the findings. Therefore, more studies should assess the validity of CPTSD among a sample of children from the general population.
Another potential explanation is possible that samples in prior studies were from different cultural and political contexts. Children from different countries would experience different types of traumatic events and have differences in the comprehension and coping styles of traumas. These differences may need to further widen under the influence of different political systems and historical-cultural backgrounds. For example, in China, emotional neglect, emotional abuse, and physical abuse are considered effective parenting strategies to control child behaviour, which has resulted in more than half of Chinese children experiencing different types of child maltreatment (Wang, Xing, & Zhao, Citation2014; Zhou, Liang, Cheng, Zheng, & Liu, Citation2019). Meanwhile, individuals prefer to adapt to circumstances rather than seek outward change in Chinese culture (Aubert, Daigle, & Daigle, Citation2004). This may result in Chinese children tend to direct their pain and sorrow inwardly. Perhaps, in consequence, we believe that Chinese children have a more complex traumatic response, and CPTSD symptoms also present in Chinese children. To date, two studies have assessed CPTSD validity in samples of the Chinese youth population (Ho et al., Citation2020, Citation2019). However, it is not clear whether Chinese children have different factor structures, distinct classes, and these different classes related to the nature of trauma experience.
Given the validity of applying the construct of complex posttraumatic stress disorder (CPTSD) in Chinese children remained unclear. Therefore, the current study aimed to (1) use CFA to test the factorial validity of CPTSD, (2) use LCA to test the discriminant validity of ICD-11 PTSD and CPTSD. In addition, this study was to assess associations between the different classes and traumatic events.
2. Methods
2.1. Participants and procedures
A cross-sectional study was conducted in Henan Province in October 2019. Seven primary schools in two cities were selected from Henan Province through a convenience sampling method. With IRB approval from the Chinese Ethics Committee of Registering Clinical Trials (ChiECRCT-20,180,191), the survey was conducted with school classes as the unit. The headteacher of each class introduced the purpose and content of the survey to children and their guardians. All children were informed that their answers could be strictly confidential and would not be disclosed to anyone within or outside the school. After that, we collected informed consent/assents from children and their guardians. In total, 2.13% of guardians refused to participate and none of the children with guardians’ consent refused to participate. Children who agreed to participate in this study were given questionnaires. Data were collected by 16 social work students (five were master students and 11 were college students). They were trained and supervised during the data collection process by an expert in child and adolescent mental health. One trained social work student in each class assisted children in filling out the questionnaire, explaining each questionnaire item, and answering any questions that arose. All collected data and information were kept confidential and only be used for research purposes. Those children, who had a traumatic experience and met PTSD criteria, would be invited for further diagnosis. If they still met PTSD criteria, we and the trained psychology teachers would provide follow-up intervention services or referral services.
A community study was carried out, with 5,143 students in grades 4 to 5 participating. Of these, 21 children (0.41%) who had large amounts of missing data (>50% on the ITQ) and 1644 children (31.97%) who reported not having experienced any kind of trauma were excluded. Eventually, 3,478 children were included in this study.
2.2. Measurements
2.2.1. Traumatic exposure
The questionnaire about traumatic exposure was composed of 10 items that were frequently reported by Chinese children in our prior study (Li et al., Citation2019). Specifically, it included the following: a serious traffic accident, a fire and explosion, a life-threatening illness (self or someone close), separation (e.g. sudden death of a close one, or separation of the child from the parents), abuse and neglect (e.g. receiving inadequate care from or being physically hurt by one’s caretakers in childhood), a natural disaster (e.g. earthquake, typhoon or flood), robbery (e.g. being kidnapped or robbed), sexual assault (e.g. a victim of sexual abuse), community violence (e.g. use of dangerous drugs or weapons, acts of self-injury or interpersonal violence by others in one’s community), and school violence (e.g. threatened, or beaten). The answer to each item was ‘Yes’ (1) or ‘No’ (0). Additionally, if participants were exposed to multiple events, they were asked to answer regarding the worst one.
2.2.2. ICD-11 criterion for PTSD and CPTSD
The Chinese version of the International Trauma Questionnaire (ITQ) is a self-report PTSD and CPTSD symptom scale with 18 items (Cloitre et al., Citation2018; Ho et al., Citation2019). First, 20 children in grades 4 to 5, two Chinese primary school teachers, and two children mental health experts were interviewed before the formal investigation to test the Chinese questionnaire on them. Based on the feedback, we changed some words to fit the children’s level of understanding. For example, ‘on guard’ was modified to ‘overly careful’. Additionally, we gave some examples to explain the items according to the developmental characteristics of Chinese children, like ‘I feel numb or emotionally shut down (e.g. have no feelings, don’t like to show my feelings to others)’. Details of all items can be seen in Table S1.
All respondents were instructed to answer questions in relation to how much they had been bothered over the past month by each PTSD and DSO symptom on a five-point Likert scale ranging from ‘Not at all’ (0) to ‘Extremely’ (4). Among these, six items were divided into the three clusters of PTSD symptoms: re-experiencing (RE), avoidance (AV), and sense of threat (TH), and six items were divided into three clusters of DSO symptoms: affect dysregulation (AD), negative self-concept (NSC) and interpersonal disturbances (DR). Additionally, participants were asked to rate the degree of functional impairment due to the PTSD and DSO symptoms.
In the current study, the internal reliability was good for six PTSD items (Cronbach’s α = 0.80), six DSO items (Cronbach’s α = 0.88), and 18 CPTSD items (Cronbach’s α = 0.91). This shows that the ITQ has good psychometric properties in our sample.
2.3. Statistical analysis
CFA was employed to test the symptom structure and factorial validity of CPTSD in children. Seven specified structure models have been tested in samples of foster children (Haselgruber et al., Citation2019) in prior studies. Considering that studies exploring the symptom structure of CPTSD in nonclinical children are scarce, these structural models were all included. Model 1 was a one-factor model where 12 symptoms are loaded onto the single latent variable CPTSD. Model 2 was a first-order six-factor model (RE, AV, TH, AD, NSC, and DR). Model 3 was a second-order model comprising six first-order factors and one single second-order factor (CPTSD). Model 4 was a two-factor higher-order model in which RE, AV, and TH factors were loaded on a second-order PTSD factor and AD, NSC, and DR factors were loaded on a second-order DSO factor. In Model 5, the PTSD factor was composed of 6-item PTSD symptoms, while the DSO factor was composed of its first-order factors (AD, NSC, DR), which included their respective symptoms. In Model 6, the PTSD factor was composed of its first-order factors (AV, RE, TH), which included their respective symptoms, while DSO was composed of 6-item symptoms. In Model 7, the PTSD factor and DSO factor were directly composed of their respective symptoms. More details about the seven structure models can be seen in .
Each model was estimated using the robust weighted least square mean and variance adjusted estimator (WLSMV). Goodness of fit was assessed for each model with a range of fit indices: the chi-square test, the comparative fit index (CFI), the Tucker-Lewis index (TLI), the root-mean-square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). As suggested by prior studies, a nonsignificant chi-square result showed a good model fit (Kline, Citation2011). CFI ≥ 0.95, TLI ≥ 0.95, RMSEA ≤ 0.06, and SRMR < 0.05 were indicative of a strong model fit (Hu & Bentler, Citation1998; McDonald & Ho, Citation2002). Changes in the RMSEA value (ΔRMSEA ≥ 0.015) were considered evidence of a meaningful difference when the optimal fitting model was determined (Chen, Citation2007).
LCA was used to identify the classes of CPTSD symptoms, including PTSD, AD, NSC, and DR symptoms, by using Mplus 8.0. The following indices were examined to determine the degree of model fit: the Akaike information criterion (AIC), the Bayesian information criterion (BIC), the sample size-adjusted Bayesian information criterion (SS-BIC), the bootstrap likelihood ratio test (BLRT), and the Vuong-Lo-Mendell-Rubin test (VLMRT) (Akaike, Citation1987; Nylund, Asparouhov, & Muthén, Citation2007; Yungtai, Mendell, & Rubin, Citation2001). The model with the lowest AIC and BIC values can be judged as the best class solution (Nylund et al., Citation2007). A nonsignificant value (P > 0.05) suggested that the model with one less class should be accepted. The entropy statistic was not used in this study because its fitness index is easily affected by large sample sizes. Finally, multinomial logistic regression analysis was conducted to explore associations between the different classes and traumatic events.
3. Results
3.1. Trauma exposure and description of the ITQ items
The mean age of the final sample was 10.03 years (SD = 0.76), with fewer girls (42.58%, n = 1469) than boys (57.42%, n = 1981). The frequency of traumas was as follows: separation (68.45%), traffic accident (44.52%), fire and explosion (22.65%), life-threatening illness (18.90%), school violence (13.61%), natural disaster (6.58%), community violence (4.01%), abuse and neglect (2.27%), robbery (1.66%) and sexual assault (1.37%). A total of 50.35% of the sample reported one traumatic event, 27.60% reported two traumatic events, and 22.07% reported more than three traumatic events. showed the mean and standard deviation for each ITQ item, and there was a slight difference between the gender.
Table 1. Mean and standard deviation for each item
3.2. The factorial validity of ICD-11 CPTSD
The fit indices for each model are shown in . Models 2, 4 and 5 were good fitting models according to RMSEA (< 0.08). Model 2 was the best fitting model based on it having the highest CFI (0.995) and TLI (0.991) and the lowest RMSEA (0.041; 95% CI = 0.037–0.046) and SRMR (0.017). Model 4, which was in line with the theoretical structure of ICD-11 CPTSD, also fits the data very well. Although the chi-square was statistically significant, it should not lead to model rejection because the power of the chi-square test is positively related to sample size and tends to reject models based on the large sample size (Tanaka, Citation1987). According to the ΔRMSEA (ΔRMSEA > 0.015), there was a significant difference between Model 2 and Model 4. Thus, Model 2 was finally considered the optimal model. The factor loadings and factor correlations for Model 2 are shown in table S1. All factor loadings and correlations among the latent factors were significant at p < 0.001.
Table 2. Model fit statistics for confirmatory factor models of ICD-11 CPTSD
3.3. The discriminant validity of ICD-11 CPTSD
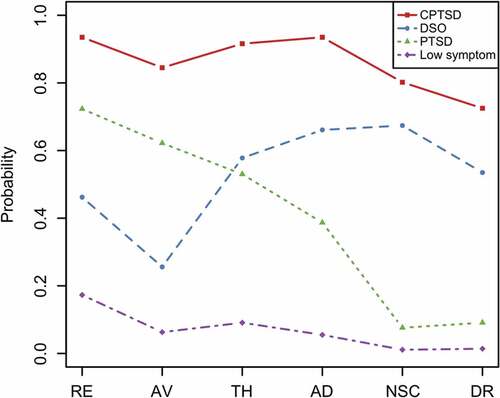
The fit indices of the LCAs for participants with trauma are shown in . The 5-class solution was excluded based on a nonsignificant VLMRT. The 4-class solution seemed to be the best model based on it having the lowest AIC and SS-BIC values. The distinct symptom prevalence in each of the three classes is also reported in table S2.
Table 3. Model fit statistics for latent class models of ICD-11 CPTSD
Class 1 (comprising 13.08% of the sample) included participants with a combination of symptoms of PTSD, affective dysregulation (AD), negative self-concept (NSC), and disturbed relationships (DR). This class was labelled the ‘CPTSD’ class. Class 2 (7.64%) had a high probability of meeting the diagnostic criteria for AD, NSC and DR but a relatively low probability of meeting the diagnostic criteria for PTSD. This class was labelled the ‘DSO’ class. Class 3 (26.97%) had a high probability of meeting the diagnostic criteria for PTSD but a relatively low probability of meeting the diagnostic criteria for AD, NSC and DR; this class was labelled the ‘PTSD’ class. In class 4 (52.31%), none of the symptoms of PTSD, AD, NSC and DR were present; this class was labelled the ‘low symptom’ class ().
3.4. Traumatic events and distinct classes
showed the results of a multinomial logistic analysis. When the low symptom class was designated as the reference category, results showed that school violence was the strongest predictor of the CPTSD class, followed by the separation, abuse and neglect, community violence, road traffic accident, life-threatening illness, fire and explosion. Five traumatic events were significant predictors of the DSO class: school violence, sexual assault, life-threatening illness, abuse and neglect, separation. Seven traumatic events were significant predictors of the PTSD class: school violence, life-threatening illness, community violence, separation, a road traffic accident, fire and explosion, and natural disaster. When the PTSD class was designated as the reference category, three traumatic events were significant predictors of the CPTSD class: school violence, separation, and a road traffic accident. One traumatic event, school violence, was a significant predictor of the DSO class.
Table 4. Multinomial logistic regression between traumatic events and the different classes
4. Discussion
The main aim of this study was to test the necessity of distinguishing CPTSD from PTSD among Chinese children aged 9–12 years by examining the factor structure and discriminant validity. Overall, the results supported the distinction of PTSD and CPTSD, which has important clinical implications for the screening or recognition of CPTSD among children.
Testing the factorial validity of ICD-11 CPTSD, the first-order six-factor model (Model 2) was identified as the best-fitting model in children aged 9–12 years. As the best-fitting structure of CPTSD proposed by the ICD-11, the two-factor higher-order model (Model 4) was not as good as Model 2. This result was inconsistent with a prior study, in which the two-factor higher-order model was the best-fitting model in children (Haselgruber et al., Citation2019). The important difference is that our sample was heterogeneous and predominantly consisted of nonclinical children who had experienced diverse types of traumatic experiences. To date, the extant research evidence appears to support the construct validity of the ICD-11 proposal of PTSD and CPTSD in clinical populations. However, the evidence in nonclinical populations is insufficient. For example, Ben-Ezra et al. (Citation2018) and Kazlauskas et al. (Citation2020) also found that the first-order six-factor model was the best fitting model in a nationally representative adult sample from Israel and a sample of adolescents from the general population in Lithuania, respectively. The type of traumatic events and the severity of disorders may have an effect on the validity of the findings. However, the factor loadings for Model 4 supported the necessity of the existence of a second-order factor. This model simply and accurately captures the relationships of CPTSD’s six dimensions and provides more information about the distinction between PTSD and DSO symptomatology. Also, the two-factor higher-order model also fits the data very well and was superior to other models. Therefore, the two-factor higher-order model should be considered as a plausible alternative in this study.
Four different classes were found, including a class with both PTSD and DSO symptoms, a class with PTSD symptoms, a class with DSO symptoms, and a low symptom class. Our findings add to the evidence base for the ICD-11 conceptualization, namely, that two distinct subgroups (PTSD and CPTSD) can be diagnosed in children following exposure to traumatic events. Similarly, the conceptualization of CPTSD was composed of two components, PTSD and DSO, which also seemed to reasonable (Brewin et al., Citation2017; First, Reed, Hyman, & Saxena, Citation2015). These results were in line with those of previous studies. These studies have reported distinct classes of PTSD and CPTSD: in one study among a community sample of adolescents and young adults (Perkonigg et al., Citation2016), in another among a clinical sample of children and adolescents (Sachser et al., Citation2017), and in the other among a sample of Austrian foster children (Haselgruber et al., Citation2019). The presence of CPTSD in children was noteworthy, particularly regarding where there were negative consequences for children’s development.
Inconsistent with fundamental assumptions of the ICD–11 proposal, the types of events associated with the risk for CPTSD and PTSD were overlapping and similar. Within multinomial logistic models, both prolonged interpersonal trauma and other types of trauma were risk factors for the CPTSD class and the PTSD class when compared to the low symptom class. Similar results have been reported in some prior studies, in which other types of traumatic events, such as near-drowning and sudden or violent death of a close, can also significantly predict the CPTSD class (Hyland et al., Citation2017b; Kazlauskas et al., Citation2020). Furthermore, other types of trauma (such as separation and road traffic accident) remained significant when the PTSD class was set as the reference category. It is possible that children exposed to non-interpersonal trauma are also likely to have DSO symptoms (i.e. emotion regulation, self-concept, and relational capacities (Flahault, Dolbeault, Sankey, & Fasse, Citation2018; Forresi et al., Citation2020). These results indicated that CPTSD might not be predicted in the context of a particular form of trauma. The main reason may be that mental illness stigma was pervasive and severe in Chinese groups (Yang et al., Citation2013). Most children were not inclined to seek professional help when they suffered from psychological trauma symptoms but directed their pain, sorrow, and other emotions inwardly (Chen & Mak, Citation2008). This could result in traumatized children in China having a more complex traumatic response. Given the lack of support for hypothesized links to trauma types, clinicians should work to avoid stereotyping when they face Chinese children exposed to non-interpersonal trauma. Moreover, they should clearly understand that the differential diagnosis between PTSD and CPTSD is determined by the symptom profile rather than the individual’s trauma types (Maercker et al., Citation2013).
The results showed that our adaptation ITQ scale had good internal reliability and all items exhibited acceptable factor loadings, which indicated that our revision had certain rationality. The revised scale helped us identify children who had PTSD/CPTSD symptoms. However, it is not clear whether the adult’s diagnostic algorithm can be applied in children, and thus this study did not report PTSD and CPTSD prevalence. However, we can find that the proportion of the PTSD class was higher than that of the CPTSD class among our sample, which was inconsistent with some findings from a clinical population. In clinical populations, a substantially higher prevalence of CPTSD than PTSD was found (Karatzias et al., Citation2016). Our results confirmed once more that ICD-11 PTSD was more common in the nonclinical population than CPTSD.
5. Limitations
The sample size was large in this study, which had enough evidence to support theoretical assumptions. However, there were still several limitations. First, the sample was drawn from one province in China, and it may not be nationally representative. Second, all data were based on self-report questionnaires, and recall bias maybe could not be excluded. Given the relatively young sample, face-to-face interviews should be used in the next step. Third, all children in this study were in grades 4 and 5. Children in other grades should be included in further studies.
Fourth, as the children and adolescent version of ITQ (ITQ-CA) was unavailable at the time of our data collection, the Chinese version of ITQ for adults was revised and adopted in this study. Although the phrasing of ITQ was adjusted to correspond with that age group, ensuring that every symptom of ITQ was consistent with a child’s developmental characteristics was a difficult proposition. Comprehending the problems associated with certain elements (e.g. I feel numb or emotionally shut down) could impact the accuracy of the results to a certain extent. Hence, the current results should be interpreted with some caution. Furthermore, the results’ replication using a special measure (e.g. the ITQ-CA) in future studies is essential.
6. Conclusions
The CFA results partially supported the factorial validity of CPTSD, and the LCA results strongly supported the discriminant validity of the ICD-11 proposals for PTSD and CPTSD in Chinese children. More children fall in the PTSD class, and both prolonged interpersonal trauma and other types of trauma could predict class differences.
Contributions
Jina Li primarily conducted the statistical analyses and interpretation of the data as well as wrote the first draft of the manuscript. Weiwei Wang and Weijun Zhang revised the manuscript critically for important statistical content and provided general advice. Wei Hu, Ziyue Yuan and Ruifu Zhou facilitated data collection. Zhiyong Qu conceptualized and designed the study. All authors have approved the final manuscript.
Date availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Supplemental Material
Download ()Acknowledgments
We are grateful to data collectors, such as Jingwen He, Boyuan Li, Mengmeng Miao, Juanjuan Han, for providing support for this study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Achterhof, R., Huntjens, R. J. C., Meewisse, M. L., & Kiers, H. A. L. (2019). Assessing the application of latent class and latent profile analysis for evaluating the construct validity of complex posttraumatic stress disorder: Cautions and limitations. European Journal of Psychotraumatology, 10(1), 1698223. doi:10.1080/20008198.2019.1698223
- Akaike, H. (1987). Factor analysis and AIC. Psychometrika, 52(3), 317–11. doi:10.1007/BF02294359
- Aubert, P., Daigle, M. S., & Daigle, J. G. (2004). Cultural traits and immigration: Hostility and suicidality in Chinese Canadian students. Transcultural Psychiatry, 41(4), 514–532. doi:10.1177/1363461504045647
- Ben-Ezra, M., Hyland, P., Karatzias, T., Maercker, A., Hamama-Raz, Y., Lavenda, O., … Shevlin, M. (2020). A cross-country psychiatric screening of ICD-11 disorders specifically associated with stress in Kenya, Nigeria and Ghana. European Journal of Psychotraumatology, 11(1), 1720972. doi:10.1080/20008198.2020.1720972.
- Ben-Ezra, M., Karatzias, T., Hyland, P., Brewin, C. R., & Shevlin, M. (2018). Posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) as per ICD-11 proposals: A population study in Israel. Journal of Depression and Anxiety, 35. doi:10.1002/da.22723
- Brewin, C. R., Cloitre, M., Hyland, P., Shevlin, M., Maercker, A., Bryant, R. A., … Rousseau, C. (2017). A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clinical Psychology Review, 58, 1–15. doi:10.1016/j.cpr.2017.09.001.
- Chen, F. F. (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504 doi:10.1080/10705510701301834.
- Chen, S. X., & Mak, W. W. (2008). Seeking professional help: Etiology beliefs about mental illness across cultures. Journal of Counseling Psychology, 55(4), 442–450. doi:10.1037/a0012898.
- Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4(1), 20706. doi:10.3402/ejpt.v4i0.20706.
- Cloitre, M., Garvert, D. W., Weiss, B. J., Carlson, E. B., & Bryant, R. A. (2014). Distinguishing PTSD, complex PTSD, and borderline personality disorder: A latent class analysis. European Journal of Psychotraumatology, 5(1), 25097. doi:10.3402/ejpt.v5.25097.
- Cloitre, M., Hyland, P., Bisson, J. I., Brewin, C. R., Roberts, N. P., Karatzias, T., & Shevlin, M. (2019). ICD-11 posttraumatic stress disorder and complex posttraumatic stress disorder in the USA: A Population-based study. Journal of Traumatic Stress, 32(6), 833–842. doi:10.1002/jts.22454
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The international trauma questionnaire: Development of a self‐report measure of ICD‐11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. doi:10.1111/acps.12956.
- Dokkedah, S., Oboke, H., Ovuga, E., & Elklit, A. (2015). ICD-11 trauma questionnaires for PTSD and complex PTSD: Validation among civilians and former abducted children in Northern Uganda. Journal of Psychiatry, 18(6). doi:10.4172/2378-5756.1000335
- Dvir, Y., Ford, J. D., Hill, M., & Frazier, J. A. (2014). Childhood maltreatment, emotional dysregulation, and psychiatric comorbidities. Harvard Review of Psychiatry, 22(3), 149–161. doi:10.1097/HRP.0000000000000014.
- Elklit, A., Hyland, P., & Shevlin, M. (2014). Evidence of symptom profiles consistent with posttraumatic stress disorder and complex posttraumatic stress disorder in different trauma samples. European Journal of Psychotraumatology, 5(1), 24221. doi:10.3402/ejpt.v5.24221.
- Finkelhor, D., Turner, H. A., Shattuck, A., & Hamby, S. L. (2013). Violence, crime, and abuse exposure in a national sample of children and youth an update. JAMA Pediatrics, 167(7), 614–621. doi:10.1542/peds.2009-0467
- First, M. B., Reed, G. M., Hyman, S. E., & Saxena, S. (2015). The development of the ICD-11 clinical descriptions and diagnostic guidelines for mental and behavioural disorders. World Psychiatry, 14(1), 82–90. doi:10.1002/wps.20189.
- Flahault, C., Dolbeault, S., Sankey, C., & Fasse, L. (2018). Understanding grief in children who have lost a parent with cancer: How do they give meaning to this experience? Results of an interpretative phenomenological analysis. Death Studies, 42(8), 483–490. doi:10.1080/07481187.2017.1383951.
- Forresi, B., Soncini, F., Bottosso, E., Di Pietro, E., Scarpini, G., Scaini, S., … Righi, E. (2020). Post-traumatic stress disorder, emotional and behavioral difficulties in children and adolescents 2 years after the 2012 earthquake in Italy: An epidemiological cross-sectional study. European Child & Adolescent Psychiatry, 29(2), 227–238. doi:10.1007/s00787-019-01370-0.
- Hagan, M. J., Gentry, M., Ippen, C. G., & Lieberman, A. F. (2017). PTSD with and without dissociation in young children exposed to interpersonal trauma. Journal of Affective Disorders, 227, 536–541. doi:10.1016/j.jad.2017.11.070.
- Haselgruber, A., Solva, K., & Lueger-Schuster, B. (2019). Validation of ICD-11 PTSD and complex PTSD in foster children using the International trauma questionnaire. Acta Psychiatrica Scandinavica, 1–14. http://doi.org/10.1111/acps.13100
- Herman, J. L. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5(3), 377–391. doi:10.1007/bf00977235.
- Ho, G. W. K., Hyland, P., Shevlin, M., Chien, W. T., Inoue, S., Yang, P. J., … Karatzias, T. (2020). The validity of ICD-11 PTSD and complex PTSD in East Asian cultures: Findings with young adults from China, Hong Kong, Japan, and Taiwan. European Journal of Psychotraumatology, 11(1), 1717826. doi:10.1080/20008198.2020.1717826.
- Ho, G. W. K., Karatzias, T., Cloitre, M., Chan, A. C. Y., Bressington, D., Chien, W. T., … Shevlin, M. (2019). Translation and validation of the Chinese ICD-11 International trauma questionnaire (ITQ) for the assessment of posttraumatic stress disorder (PTSD) and Complex PTSD (CPTSD). European Journal of Psychotraumatology, 10(1), 1608718. doi:10.1080/20008198.2019.1608718.
- Hu, L. T., & Bentler, P. M. (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3(4), 424–453. doi:10.1037//1082-989X.3.4.424.
- Hyland, P., Murphy, J., Shevlin, M., Vallières, F., Mcelroy, E., Elklit, A., … Cloitre, M. (2017a). Variation in post-traumatic response: The role of trauma type in predicting ICD-11 PTSD and CPTSD symptoms. Social Psychiatry and Psychiatric Epidemiology, 52(6), 1–10. doi:10.1007/s00127-017-1350-8.
- Hyland, P., Murphy, J., Shevlin, M., Vallieres, F., Mcelroy, E., Elklit, A., … Cloitre, M. (2017b). Variation in post-traumatic response: The role of trauma type in predicting ICD-11 PTSD and CPTSD symptoms. Social Psychiatry and Psychiatric Epidemiology, 52(6), 727–736. doi:10.1007/s00127-017-1350-8.
- Hyland, P., Shevlin, M., Brewin, C. R., Cloitre, M., & Roberts, N. P. (2017c). Validation of post-traumatic stress disorder (PTSD) and complex PTSD using the International trauma questionnaire. Acta Psychiatrica Scandinavica, 136(3), 313–322. doi:10.1111/acps.13100.
- Karatzias, T., Shevlin, M., Fyvie, C., Hyland, P., Efthymiadou, E., Wilson, D., … Cloitre, M. (2017). Evidence of distinct profiles of posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD) based on the new ICD-11 trauma questionnaire (ICD-TQ). Journal of Affective Disorders, 207, 181–187. doi:10.1016/j.jad.2016.09.032.
- Karatzias, T., Shevlin, M., Fyvie, C., Hyland, P., Efthymiadou, E., Wilson, D., … Cloitre, M. (2016). An initial psychometric assessment of an ICD-11 based measure of PTSD and complex PTSD (ICD-TQ): Evidence of construct validity. Journal of Anxiety Disorders, 44, 73–79. doi:10.1016/j.janxdis.2016.10.009.
- Kazlauskas, E., Gegieckaite, G., Hyland, P., Zelviene, P., & Cloitre, M. (2018). The structure of ICD-11 PTSD and complex PTSD in Lithuanian mental health services. European Journal of Psychotraumatology, 9(1), 1414559. doi:10.1080/20008198.2017.1414559.
- Kazlauskas, E., Zelviene, P., Daniunaite, I., Hyland, P., Kvedaraite, M., Shevlin, M., & Cloitre, M. (2020). The structure of ICD-11 PTSD and complex PTSD in adolescents exposed to potentially traumatic experiences. Journal of Affective Disorders, 265, 169–174. doi:10.1016/j.jad.2020.01.061.
- Kline, R. B. (2011). Principles and practice of structural equation modeling (3rd ed., pp. xvi, 427–xvi, 427). New York: Guilford Press.
- Knefel, M., Garvert, D. W., Cloitre, M., & Luegerschuster, B. (2015). Update to an evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse by Knefel & Lueger-Schuster (2013): A latent profile analysis. European Journal of Psychotraumatology, 6(1), 25290. doi:10.3402/ejpt.v6.25290.
- Li, J., Zhang, W., Chen, W., Yuan, H., Zhang, S., Tian, M., & Qu, Z. (2019). Applications of the Chinese version of the primary care PTSD screen for DSM-5 (PC-PTSD-5) for children. Journal of Affective Disorders, 254, 109–114. doi:10.1016/j.jad.2019.05.021.
- Liang, Y., Zhou, Y., & Liu, Z. (2019). Traumatic experiences and posttraumatic stress disorder among Chinese rural-to-urban migrant children. Journal of Affective Disorders, 257, 123–129. doi:10.1016/j.jad.2019.07.024.
- Liddell, B. J., Nickerson, A., Felmingham, K. L., Malhi, G. S., Cheung, J., Den, M. L., … Bryant, R. A. (2019). Complex posttraumatic stress disorder symptom profiles in traumatized refugees. Journal of Traumatic Stress, 32(6), 822–832. doi:10.1002/jts.22453.
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., Reed, G. M., Van Ommeren, M., … Llosa, A. E. (2013). Proposals for mental disorders specifically associated with stress in the International classification of diseases-11. Lancet, 381(9878), 1683–1685. doi:10.1016/S0140-6736(12)62191-6.
- McDonald, R. P., & Ho, M. H. R. (2002). Principles and practice in reporting structural equation analyses. . Psychological Methods, 7(1), 64–82. doi:10.1037/1082-989x.7.1.64.
- Murphy, S., Elklit, A., Dokkedahl, S. B., & Shevlin, M. (2016). Testing the validity of the proposed ICD-11 PTSD and complex PTSD criteria using a sample from Northern Uganda. European Journal of Psychotraumatology, 7(1), 32678. doi:10.3402/ejpt.v7.32678.
- Nickerson, A., Cloitre, M., Bryant, R. A., Schnyder, U., Morina, N., & Schick, M. (2016). The factor structure of complex posttraumatic stress disorder in traumatized refugees. European Journal of Psychotraumatology, 7(1), 33253. doi:10.3402/ejpt.v7.33253.
- Nylund, K. L., Asparouhov, T., & Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A monte carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. doi:10.1080/10705510701575396.
- Perkonigg, A., Hofler, M., Cloitre, M., Wittchen, H., Trautmann, S., & Maercker, A. (2016). Evidence for two different ICD-11 posttraumatic stress disorders in a community sample of adolescents and young adults. European Archives of Psychiatry and Clinical Neuroscience, 266(4), 317–328. doi:10.1007/s00406-015-0639-4.
- Pratchett, L. C., & Rachel, Y. (2011). Foundations of posttraumatic stress disorder: Does early life trauma lead to adult posttraumatic stress disorder? Development and Psychopathology, 23(2), 477–491. doi:10.1017/S0954579411000186.
- Sachser, C., Keller, F., & Goldbeck, L. (2017). Complex PTSD as proposed for ICD-11: Validation of a new disorder in children and adolescents and their response to trauma-focused cognitive behavioral therapy. Journal of Child Psychology and Psychiatry, 58(2), 160–168. doi:10.1111/jcpp.12640.
- Shevlin, M., Hyland, P., Karatzias, T., Fyvie, C., Roberts, N. P., Bisson, J. I., … Cloitre, M. (2017). Alternative models of disorders of traumatic stress based on the new ICD‐11 proposals. Acta Psychiatrica Scandinavica, 135(5), 419–428. doi:10.1111/acps.12695.
- Shipman, K., Edwards, A., Brown, A., Swisher, L. M., & Jennings, E. (2005). Managing emotion in a maltreating context: A pilot study examining child neglect. Child Abuse & Neglect, 29(9), 1015–1029. doi:10.1016/j.chiabu.2005.01.006.
- Solva, K., Haselgruber, A., & Luegerschuster, B. (2020). The relationship between cumulative traumatic experiences and ICD-11 post-traumatic symptoms in children and adolescents in foster care: The mediating effect of sense of coherence. Child Abuse & Neglect, 101, 104388. doi:10.1016/j.chiabu.2020.104388.
- Tanaka, J. S. (1987). “How big is big enough?”: Sample size and goodness of fit in structural equation models with latent variables. Child Development, 58(1), 134–146. doi:10.2307/1130296.
- Wang, M., Xing, X., & Zhao, J. (2014). Intergenerational transmission of corporal punishment in China: The moderating role of marital satisfaction and gender. Journal of Abnormal Child Psychology, 42(8), 1263–1274. doi:10.1007/s10802-014-9890-9.
- Wolf, E. J., Miller, M. W., Kilpatrick, D., Resnick, H. S., Badour, C. L., Marx, B. P., … Friedman, M. J. (2015a). ICD–11 complex PTSD in U.S. National and Veteran samples. Clinical Psychological Science, 3(2), 215–229. doi:10.1177/2167702614545480.
- Wolf, E. J., Miller, M. W., Kilpatrick, D. G., Resnick, H. S., Badour, C. L., Marx, B. P., … Friedman, M. J. (2015b). ICD–11 complex PTSD in U.S. National and Veteran samples. Clinical Psychological Science, 52(2), 215–229. doi:10.1177/2167702614545480.
- Yang, L. H., Purdie-Vaughns, V., Kotabe, H., Link, B. G., Saw, A., Wong, G., & Phelan, J. C. (2013). Culture, threat, and mental illness stigma: Identifying culture-specific threat among Chinese-American groups. Social Science & Medicine, 88, 56–67. doi:10.1016/j.socscimed.2013.03.036.
- Yungtai, L., Mendell, N. R., & Rubin, D. B. (2001). Testing the number of components in a normal mixture. Biometrika, 767–778. http://doi.org/10.1093/biomet/88.3.767
- Zerach, G., Shevlin, M., Cloitre, M., & Solomon, Z. (2019). Complex posttraumatic stress disorder (CPTSD) following captivity: A 24-year longitudinal study. European Journal of Psychotraumatology, 14(1), 1616488. doi:10.1080/20008198.2019.1616488.
- Zhou, Y., Liang, Y., Cheng, J., Zheng, H., & Liu, Z. (2019). Child maltreatment in western China: Demographic differences and associations with mental health. International Journal of Environmental Research and Public Health, 16(19), 3619. doi:10.3390/ijerph16193619.