ABSTRACT
Background: In recent years, eye movement desensitization and reprocessing (EMDR) has been applied to different psychiatric conditions beyond post-traumatic stress disorder (PTSD), and an increasing number of studies have evaluated its effect on depression. To date, no quantitative synthesis of the efficacy of EMDR on depression has been conducted.
Objective: To meta-analytically review the studies on EMDR for depression as the primary target for treatment.
Method: Studies with a controlled design evaluating the effect of EMDR on depression were searched on six electronic databases (PubMed, Embase, CINAHL, PsycINFO, Cochrane database, and Francine Shapiro Library) and then selected by two independent reviewers. A systematic review and meta-analysis was conducted.
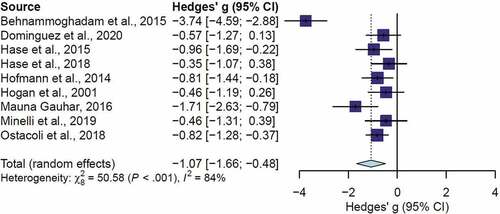
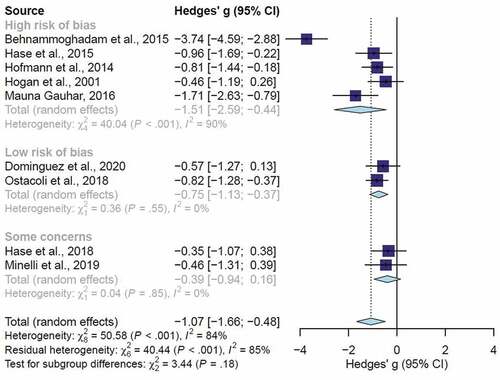
Results: Eleven studies were included for qualitative synthesis. Nine studies were included in the meta-analysis, involving 373 participants. The overall effect size of EMDR for depressive symptoms is large (n = 9, Hedges’ g = – 1.07; 95%CI [–1.66; – 0.48]), with high heterogeneity (I2 = 84%), and corresponds to a ‘number needed to treat’ of 1.8. At follow-up (range 3–6 months), the effect remains significant but moderate (n = 3, Hedges’ g = – 0.62; 95%CI [–0.97; – 0.28]; I2 = 0%). The effect of EMDR compared with active controls is also moderate (n = 7, g = – 0.68; 95%CI [–0.92; – 0.43]; I2 = 0%). No publication bias was found, although the results are limited by the small number and poor methodological quality of the included studies.
Conclusions: Review findings suggest that EMDR may be considered an effective treatment for improving symptoms of depression, with effects comparable to other active treatments. However, findings need to be interpreted in light of the limited number of the studies and their quality. Further research is required to understand the longer-term of effects EMDR in treating depression and preventing depression relapse.
Protocol registration: PROSPERO (CRD42018090086).
HIGHLIGHTS
This review summarizes the current evidence on the effects of EMDR for depression.
Findings show that one-third of people with depression could benefit from EMDR.
EMDR could be considered as an alternative to first-line treatments for depression, pending further research.
Antecedentes: En los últimos años, la desensibilización y reprocesamiento por movimientos oculares (EMDR) se ha aplicado a diferentes condiciones psiquiátricas más allá del trastorno de estrés postraumático (TEPT), y un número creciente de estudios ha evaluado su efecto en la depresión. Hasta la fecha, no se ha realizado ninguna síntesis cuantitativa de la eficacia de la EMDR en la depresión.
Objetivo: Revisar meta-analíticamente los estudios de EMDR para la depresión como objetivo principal del tratamiento.
Método: Se buscaron estudios con un diseño controlado que evaluaran el efecto de la EMDR en la depresión en seis bases de datos electrónicas (PubMed, Embase, CINAHL, PsycINFO, base de datos Cochrane y Francine Shapiro Library) y luego fueron seleccionados por dos revisores independientes. Se realizó una revisión sistemática y un metanálisis.
Resultados: Se incluyeron once estudios para la síntesis cualitativa. Se incluyeron nueve estudios en el meta-análisis, con 373 participantes. El tamaño del efecto global de la EMDR para los síntomas depresivos es grande (n = 9, g de Hedges = −1,07; IC del 95% [−1,66; −0,48]), con alta heterogeneidad (I2 = 84%), y corresponde a un ‘número necesario a tratar’ de 1,8. En el seguimiento (rango 3-6 meses), el efecto sigue siendo significativo pero moderado (n = 3, g de Hedges = −0,62; IC del 95% [−0,97;-0,28]; I2 = 0%). El efecto del EMDR en comparación con los controles activos también es moderado (n = 7, g = −0,68; IC del 95% [−0,92;-0,43]; I2 = 0%). No se encontró ningún sesgo de publicación, aunque los resultados están limitados por el pequeño número y la pobre calidad metodológica de los estudios incluidos.
Conclusiones: Los resultados de la revisión sugieren que la EMDR puede considerarse un tratamiento eficaz para mejorar los síntomas de la depresión, con efectos comparables a los de otros tratamientos activos. Sin embargo, los hallazgos deben interpretarse a la luz del número limitado de los estudios y su calidad. Se requiere investigación adicional para comprender los efectos a largo plazo de la EMDR en el tratamiento de la depresión y la prevención de la recaída de la depresión.
Registro del protocolo: PROSPERO (CRD42018090086).
背景:近年来, 眼动脱敏和再加工 (EMDR) 已被应用到创伤后应激障碍 (PTSD) 以外的不同精神疾病中, 并且越来越多的研究评估了其对抑郁的影响。至今尚未对EMDR对抑郁症疗效进行定量综合分析。
目的:以元分析方法综述以抑郁症为主要治疗目标的EMDR研究。
方法:在六个电子数据库 (PubMed, Embase, CINAHL, PsycINFO, Cochrane数据库和Francine Shapiro库) 中搜索包含评估EMDR对抑郁症影响的对照设计的研究, 然后由两名独立的审阅者进行选择。进行了系统综述和元分析。
结果:纳入了11项定性综合研究。元分析包括九项研究, 共373名参与者。 EMDR对抑郁症状的总体效应量较大 (n = 9, Hedges’ g= −1.07; 95%CI [−1.66; −0.48]), 异质性较高 (I2 = 84%), 对应于1.8的’需要治疗的数量’。在随访时 (3-6个月), 效果仍然显著但中等 (n = 3, Hedges’ g= −0.62; 95%CI [−0.97; −0.28]; I2 = 0%) 。与主动对照组相比, EMDR的作用也中等 (n = 7, g= −0.68; 95%CI [−0.92; −0.43];I2 = 0%) 。没有发现发表偏倚, 尽管结果受限于纳入研究的数量较少和方法质量较差。
结论:综述结果表明, EMDR可以被认为是一种有效改善抑郁症状的治疗方法, 其效果可与其他主动疗法相比较。但是, 结果需要在依据有限数量的研究及其质量的前提下解释。需要进一步的研究来了解EMDR在治疗抑郁和预防抑郁复发方面的长期作用。
协议注册:PROSPERO (CRD42018090086) 。
1. Introduction
Depression is widespread in the world with a prevalence that ranges between 2.6% (among males in the Western Pacific Region) and 5.9% (among females in the African Regions), with a peak in late adulthood and a higher rate for women than for men (World Health Organization, Citation2017). This disease impacts on people’s quality of life and functioning. In this regard, in 2017 the World Health Organization identified depression as one of the major causes of reduced life years due to mortality and disability (James et al., Citation2018). According to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), depression assumes clinical relevance when it leads to significant distress or impairment in social, occupational, or other important areas of functioning and meets the diagnostic criteria for an episode of major depressive disorder (American Psychiatric Association, Citation2013).
The treatment of depression has greatly evolved over the last few years and there are now various therapeutic options that combine pharmacology and psychotherapy (National Institute for Health and Care Excellence, Citation2009, Citation2018). However, less than half of the treated patients (Johnston, Powell, Anderson, Szabo, & Cline, Citation2019) show a positive response to drug therapy (i.e. a reduction in depressive symptoms) and, although the introduction of cognitive behavioural therapy (CBT) has allowed a doubling of the percentage of responders (Hofmann et al., Citation2014), recurrence rates at 1 and 2 years remain high at 29% and 54%, respectively (Vittengl, Clark, Dunn, & Jarrett, Citation2007).
Among the main risk factors for depression, traumatic events play a crucial role. This seems particularly evident when considering that psychiatric patients show an 89.9% prevalence of early traumatic experiences compared to 50% for the general population (Schalinski et al., Citation2016). The causal relationship between traumatic events and the onset of a depressive disorder is complex and has yet to be fully outlined. However, it is likely that the impact of traumatic experiences is mediated by an individual’s epigenetic, immunological, endocrine (Caldji et al., Citation1998; Huot, Plotsky, Lenox, & McNamara, Citation2002; Ladd et al., Citation2000; Liu, Citation1997; Meaney et al., Citation1996; Plotsky & Meaney, Citation1993), neurobiological (Andersen et al., Citation2008; Davey, Yücel, & Allen, Citation2008; Ernst, Pine, & Hardin, Citation2006) and psychological modifications (Aldao, Nolen-Hoeksema, & Schweizer, Citation2010a; Courtney, Kushwaha, & Johnson, Citation2008; Crow, Cross, Powers, & Bradley, Citation2014; Maciejewski & Mazure, Citation2006; Wright, Crawford, & Del Castillo, Citation2009). Exposure to adverse events during childhood and adolescence is not only a significant risk factor for developing a depressive disorder but also influences the course, prognosis, and response to treatments. Indeed, this exposure has been shown to be one of the main factors in recurrence, persistence, and resistance to the treatment of depression (Nanni, Uher, & Danese, Citation2012; Nelson, Klumparendt, Doebler, & Ehring, Citation2017). Furthermore, it seems to increase the individual sensitivity of the disorder to psychotherapeutic interventions, which in these cases are more effective than drug therapy (Nemeroff et al., Citation2003). Relying on these findings, some authors proposed considering trauma-associated depression as a particular subtype, which would require a different approach compared to the traditional one proposed by the guidelines (Minelli et al., Citation2019; Nanni et al., Citation2012; Nelson et al., Citation2017; Paterniti, Sterner, Caldwell, & Bisserbe, Citation2017).
Eye movement desensitization and reprocessing (EMDR) is a first-choice therapy in post-traumatic stress disorder (PTSD) and is based on the adaptive information processing (AIP) model proposed by Shapiro (Shapiro, Citation2018). Such a model proposes the influence of dysfunctional memories that have not been completely processed underlying various psychiatric disorders (such as PTSD, mood disorders, chronic pain, and drug addiction). These memories could be triggered by internal or external stimuli, thus assuming an intrusive nature and accompanying appearance of PTSD symptoms and other disorders (Hase et al., Citation2018). According to Barry and collaborators (Barry, Naus & Rehm, Citation2006), dysfunctional memories are characterized by a lack of ‘memory awareness’ as a consequence of their incomplete processing. EMDR therapy targets this lack of awareness by reprocessing such pathogenic memories with the use of alternate bilateral stimulations (e.g. eye movements), thus enabling their transformation and integration into already existing semantic links (Hase, Balmaceda, Ostacoli, Liebermann, & Hofmann, Citation2017; Solomon & Shapiro, Citation2008).
Recently, a specific EMDR therapy protocol for the treatment of depressive disorders (DeprEND®) has been published (Hofmann et al., Citation2016). Research findings have shown that EMDR could contribute to a significant reduction of depressive symptoms associated with PTSD when compared to waitlist/usual care or non-trauma-focused CBT. However, these findings are supported by very low-quality evidence (Bisson, Roberts, Andrew, Cooper, & Lewis, Citation2013; Cuijpers, van Veen, Sijbrandij, Yoder, & Cristea, Citation2020).
Moreover, in recent years EMDR has been applied to the treatment of psychiatric disorders beyond PTSD, such as depression, although it is not currently recommended by the guidelines (Cuijpers et al., Citation2020; Valiente-Gómez et al., Citation2017). Therefore, it is essential to determine whether EMDR is an evidence-based treatment for depression.
Previous reviews addressing this topic have been published (Carletto et al., Citation2017; Malandrone, Carletto, Hase, Hofmann, & Ostacoli, Citation2019; Wood & Ricketts, Citation2013), suggesting the potentiality of EMDR for depression but also highlighting the paucity of methodologically sound studies conducted until then. As other studies have been conducted in recent years, including some randomized controlled trials (RCTs), the present systematic review and meta-analysis aims to update and add a quantitative analysis on the efficacy of EMDR for the treatment of depression.
2. Methods
2.1. Protocol registration
The review protocol was registered in the PROSPERO repository (CRD42018090086). The original protocol recorded on PROSPERO has undergone some variations. In particular, the search has been updated and the meta-analysis focused on depression considered as a primary diagnosis and outcome.
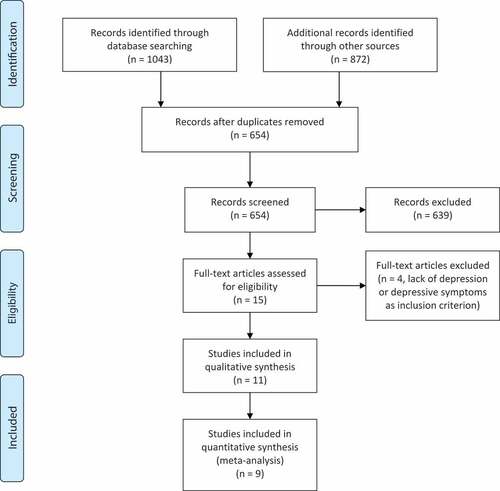
The systematic review and meta-analysis was carried out following the PRISMA statement and the PRISMA checklist (Moher, Liberati, Tetzlaff, & Altman, Citation2010) and it was drafted following the Cochrane Handbook Guidelines (Higgins et al., Citation2019).
2.2. Search strategy for identification of studies
Searches were conducted in the following databases on 30 September 2020: PubMed, Embase, CINAHL, PsycINFO and the Cochrane Central Register of Controlled Trials. Moreover, we performed a search with the keyword ‘depress’ in the Francine Shapiro Library, which is an online compendium of conference presentations, scholarly articles, and other important grey literature related to EMDR. From selected studies, cross-references were checked manually (see Supplementary Material S1 for details of the search strategy).
2.3. Eligibility criteria
2.3.1. Design
We included studies with a controlled trial design, either randomized or not. No year or language restrictions were applied.
2.3.2. Population
Trials included patients of any age with depression as a primary diagnosis and primary outcome of the study. Depression is defined as either major depressive disorder or depressive symptoms (above or below a predefined cut-off on the questionnaires employed in each study). There was no restriction by concurrent organic disease.
2.3.3. Intervention and comparison
We included studies that evaluated EMDR intervention alone or in addition to another treatment in comparison with no intervention, waiting list, treatment as usual, or other types of intervention (e.g. antidepressant medication, CBT, psychodynamic therapy).
2.3.4. Outcome
We included studies with depression as a primary outcome. Studies were supposed to include quantitative data on depressive scores, as measured by standardized psychometric scales, before and after the intervention/s. Finally, in order to be included in the meta-analysis, studies also had to provide enough data to calculate effect sizes.
2.4. Data collection and analysis
2.4.1. Study selection and appraisal
Two authors (S.C. and F.M.) independently conducted standardized assessments to determine study eligibility according to the inclusion criteria. They screened the abstracts and then retrieved and analysed the full texts for all material deemed relevant. Any disagreement was discussed with a third author (L.O.) before agreement was reached.
2.4.2. Data extraction
Data from the selected studies were inserted into a standard template by two independent researchers (S.C. and F.M.). Extracted data covered publication year, publication type, language, study design, population, primary diagnosis, sample size (for both experimental and control groups), duration and type of intervention, duration and type of comparator, depression measure and length of follow-up. Article authors were contacted via email for missing information.
2.4.3. Risk of bias in individual studies
The internal validity of the RCTs was assessed using Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) (Sterne et al., Citation2019), which consists of five domains (randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, selection of the reported result) and a categorization of the overall risk of bias. Risk of bias of controlled studies was assessed using the MINORS scale (Slim et al., Citation2003; Zeng et al., Citation2015). For all included studies, quality was also assessed using the platinum standard (PS) (Hertlein & Ricci, Citation2004), which was specifically designed to evaluate effectiveness in EMDR research. Assessment of the risk of bias was made by two independent coders (S.C. and F.M.) and any disagreements were discussed and resolved with a third reviewer (L.O.).
2.4.4. Summary measures
For each study, the mean change from baseline (post-score – baseline score) was computed. Because the included studies used different scales for measuring depression, effect sizes were computed as the standardized mean difference based on Hedges’ g method (Hedges & Olkin, Citation1985). Moreover, as the correlation coefficient between the post- and baseline scores is needed for computing the standard error, the value of 0.7 was assigned, as suggested by Rosenthal (Citation1991).
The DerSimonian and Laird random-effects model was used to pool estimates across studies (DerSimonian & Laird, Citation1986). Average effect size and 95% confidence interval (95%CI) were computed using the Jackson method. The number needed to treat (NNT) was calculated with the formulae provided by Kraemer and Kupfer (Citation2006). To estimate heterogeneity between studies, Cochran’s Q test and the Higgins I2 statistic were used. Similarly, subgroup analyses were carried out using random-effects models by considering the risk of bias. The extent to which different treatment doses affect the effect size was examined by applying a univariate meta-regression. To identify influential studies that resulted in variation, a sensitivity analysis was carried out using GOSH (graphical display of study heterogeneity) plots, which fit the same meta-analysis model for all the possible study combinations and look for specific patterns by performing clustering with k-means, DBSCAN (density-based spatial clustering of applications with noise) and Gaussian mixed models (Olkin, Dahabreh, & Trikalinos, Citation2012). Publication bias was examined by visual inspection of funnel plots and using Egger’s test (Egger, Smith, Schneider, & Minder, Citation1997). Analyses were carried out using R version 3.6.1 (R Development Core Team, Citation2019).
3. Results
3.1. Study selection and study characteristics
The PRISMA flowchart describing the selection process, including reasons for exclusion, is presented in . The search retrieved 11 studies: 10 articles on adult patients and one on adolescents (). Meta-analysis included 9 studies, as two studies (Lei & Zhen-Ying, Citation2007; Tang et al., Citation2015) was excluded due to there being no usable data for calculating the effect sizes.
Table 1. EMDR for depression or depressive symptoms as a primary outcome
The meta-analysis involved 373 participants, with 177 allocated to EMDR treatment and 196 controls.
Ten studies were published in journals and one was a PhD dissertation thesis. All except one were in English. The first published study dates back to 2007 and the last in 2020. Regarding the study design, eight studies were RCTs and three were controlled studies (CS). None of the studies included patients with a PTSD diagnosis. The presence of traumatic experiences was considered as an inclusion criterion in only one of the studies (Minelli et al., Citation2019), whereas in the other studies it was assessed among other variables. Concerning the use of medication, one study considered it to be an exclusion criterion, one study reported no information, and nine studies chose to keep stable or not exclude the use of antidepressants. In five studies, the efficacy of EMDR was investigated as an add-on to other psychotherapies, medications, or psychoeducation, and six studies compared EMDR as a stand-alone treatment. When EMDR was investigated as a stand-alone treatment, two studies compared EMDR with a waiting list/no treatment control group, whereas four studies compared EMDR with an active control. Among the latter, all studies compared EMDR with CBT. The average amount of EMDR therapy administered is 16.97 hours (SD = 16.53) and the average amount of control treatment is 19.08 hours (SD = 15.94). Although six studies planned a follow-up evaluation, only four studies provided data for including in the meta-analysis.
3.2. Risk of bias within studies
The risk of bias for each study is reported in and Figure S2. Eight RCTs were assessed with RoB 2. The quality of the included studies was not optimal: the overall risk of bias was rated as low in only 22.2% of the studies. The major issues identified were related to deviation from the intended intervention, in particular the lack of intention-to-treat analysis and inadequate reporting of allocation concealment.
Table 2. Risk of bias
The three controlled studies showed a high risk of bias, mainly related to missing methodological information. Quality assessment according to the PS is reported in Supplementary Material S3. The total PS score for each study ranged from 6.5 to 11.5 (maximum of 13), with a mean of 8.73 (SD = 1.63). Almost all studies were judged to have clearly defined target symptoms, reliable and valid measures and used a control or comparison group. Moreover, almost all studies reported the level of therapist(s) training and applied a manualized, replicable, specific EMDR treatment. The lowest PS scores are mainly related to not reporting information regarding the assessors’ training, effect size and level of treatment adherence. Finally, in only two studies was the treatment length 11 or more sessions, which is considered the threshold to achieve an effect according to the PS guidelines (Hertlein & Ricci, Citation2004). Overall, the PS scores were largely consistent with the judgement of risk of bias provided by RoB 2/MINORS.
3.3. Synthesis of results
The forest plot of the overall effect of EMDR is reported in . EMDR results in a large significant effect on depressive symptoms (n = 9, Hedges’ g = – 1.07; 95%CI [–1.66, – 0.48]), with high heterogeneity (I2 = 84%). The effect size corresponds to an NNT of 1.8. Exclusion of one outlier resulted in a smaller but still moderately significant effect size for post-treatment (n = 8, g = – 0.75; 95%CI [–0.99, – 0.50], NNT = 2.5; forest plot S5), with low heterogeneity (I2 = 2%). At follow-up, the effect is still significant (n = 3, g = – 0.62; 95%CI [–0.97, – 0.28]; forest plot S6) with no heterogeneity (I2 = 0%). As can be seen in , low-quality studies showed a higher effect size than those of high quality. Considering only the latter, EMDR showed a moderate effect (n = 2, g = – 0.75; 95%CI [–1.13, – 0.37]) with no heterogeneity (I2 = 0%; ). The effect of EMDR was compared with an active control group in seven studies, showing a moderate effect (n = 7; g = – 0.68; 95%CI [–0.92, – 0.43]; forest plot S7) with no heterogeneity (I2 = 0%). In three studies, EMDR was compared to CBT, resulting in a still significant moderate effect size (n = 3, g = – 0.68; 95%CI [–1.03, – 0.33]; forest plot S8) with no heterogeneity (I2 = 0%). In four studies, EMDR was an add-on to another treatment, showing a moderate effect (g = – 0.68; 95%CI [–1.02, – 0.33] with no heterogeneity (I2 = 0%). The forest plot is reported in Supplementary Material S9. A dose–response effect on EMDR effect size at post-treatment was not observed (n = 7, β = 0.0003; p = 0.4231).
4. Discussion
The aim of this systematic review and meta-analysis was to update the state of the art and add a quantitative analysis on EMDR therapy for depression as the primary target for treatment.
To our knowledge, this is the first meta-analysis on this topic. Although EMDR is typically associated with the treatment of PTSD, the AIP model (Shapiro, Citation2001) opens up the possibility to treat other mental health conditions with a trauma-focused approach (Hase et al., Citation2017).
The results from the nine studies included in the present meta-analysis show that EMDR has a large effect, although high heterogeneity was found and only two studies present a low risk of bias. The statistical effect also reflects clinical significance, as one-third of people with depression benefit from EMDR therapy. In the limited number of studies where follow-up data was available positive effect of EMDR treatment were maintained but with a smaller effect. It should be noted that this latter finding is based on only three studies, so future studies are needed. The effect was moderate even when EMDR is compared with active controls and when compared directly with CBT. These results are strengthened by the absence of heterogeneity, therefore EMDR could be considered as an effective trauma-focused treatment for depression. The effectiveness of EMDR appeared not to be related to the treatment dose received. This is in line with previous studies, which showed no psychotherapy dose–response relationship for depression (Barth et al., Citation2013; Stulz, Lutz, Kopta, Minami, & Saunders, Citation2013). Furthermore, it is important to consider the limited range of EMDR sessions in the studies conducted so far. The effect sizes obtained in this meta-analysis are similar or superior to other meta-analyses evaluating the effects of CBT and other psychotherapies for depression (Cuijpers, Huibers, Daniel Ebert, Koole, & Andersson, Citation2013; Cuijpers, Van Straten, Andersson, & Van Oppen, Citation2008) that are currently recommended as effective treatments for depression in the clinical guidelines (National Institute for Health and Care Excellence, Citation2018; Parikh et al., Citation2009). This finding is in line with evidence showing that different types of psychotherapies have comparable effects (Barth et al., Citation2013; Cuijpers, Quero, Dowrick, & Arroll, Citation2019; Cuijpers et al., Citation2008). However, our meta-analysis included only 9 studies, compared to more than 100 studies in other meta-analyses, thus highlighting the need for high-quality studies to further evaluate the effect of EMDR for depression.
4.1. Strengths and limitations of the studies
In general, the studies have several limitations. As expected from studies in a field that is still in its infancy, several methodological limitations were found, such as small sample size, high risk of bias, and high heterogeneity. Less than half of the studies evaluated the long-term effect of EMDR on depression. Treatment fidelity was independently checked and considered as adequate in only three studies.
The studies also have some strengths. In most articles, the outcome evaluation criteria were well explained and the assessment tools were all validated. Furthermore, in recent years an increasing number of RCTs addressing the effectiveness of EMDR in treating depression as a primary outcome have been published, along with an increase in their methodological quality. A manualized treatment protocol was applied in the great majority of studies and data on the competence of the therapists were provided in all but one of the studies.
4.2. Strengths and limitations of this review
To our knowledge, this is the first meta-analysis on the effectiveness of EMDR in the treatment of depression as a primary outcome, going beyond previous research that evaluated its effect as an associated symptom in patients with PTSD (Bisson et al., Citation2013; Cuijpers et al., Citation2020). Moreover, the Francine Shapiro Library was consulted to retrieve grey literature, thus conducting a comprehensive review as suggested in the Cochrane handbook (Higgins et al., Citation2019). This meta-analysis does have some limitations. First of all, the number of included studies is small, indicating that the interest in research on the application of EMDR for depression is still in its infancy. Secondly, the majority of the studies were characterized by low methodological quality and only a few studies examined long-term effects, thus limiting interpretation of the results of this meta-analysis. Finally, another limitation was represented by the impossibility of retrieving data for two studies, which therefore were not included in our quantitative synthesis.
4.3. Implications for clinical practice and research
The results of this study can inform clinical practice by considering EMDR effective at reducing depression, thus adding an additional therapeutic option for clinicians treating this disorder. The increase of therapeutic strategies for depression is of particular importance as it allows better personalization to be provided according to patients’ preferences. In fact, studies have shown that receiving a preferred treatment is associated with stronger therapeutic alliance, lower dropout rates, and positive treatment outcomes (Lindhiem, Bennett, Trentacosta, & McLear, Citation2014; Swift, Callahan, Cooper, & Parkin, Citation2018; Windle et al., Citation2020). It is also essential to routinely evaluate the presence of adverse childhood experiences and traumatic events in people with depression in order to identify if trauma-focused psychotherapies such as EMDR could be more effective for patients with a history of maltreatment. Previous studies have shown that exposure to childhood maltreatment predicts a poorer response to drug treatment (Nanni et al., Citation2012; Williams, Debattista, Duchemin, Schatzberg, & Nemeroff, Citation2016) and a better response to psychotherapy (Nemeroff et al., Citation2003) in patients with depression. Therefore, trauma-focused therapies could represent a valid option for patients with depression, who are less likely to respond to usual treatments and may require specific interventions focused on their maltreatment history. It may also be useful to consider whether different types of adverse childhood experiences play a role in predicting the outcome of treatment, in line with findings supporting a significant association of childhood maltreatment, especially emotional abuse and neglect, with depression (Humphreys et al., Citation2020; Mandelli, Petrelli, & Serretti, Citation2015; Nelson et al., Citation2017).
Among EMDR clinicians, evaluation of the type and sequence of treatment targets (e.g. current episode trigger; event(s) that gave rise to the series of recurring depressive episodes; belief system related to attachment history events) could be useful for improving therapeutic outcomes. More studies should also consider adopting the DeprEnd® protocol (Hofmann et al., Citation2016) as an EMDR intervention specific for depression, or at least report a more specific description of the intervention offered to patients, in line with current checklists such as the template for intervention description and replication (Hofmann et al., Citation2014). As effect sizes could be inflated by the inclusion of low-quality studies, further studies with better methodological quality are needed to obtain more reliable effect estimates. Future studies should include longer-term follow-up (i.e. after 1 and 2 years). This would make it possible to investigate whether EMDR could be effective not only for reducing depressive symptoms but also preventing relapses, particularly in comparison with other interventions already recommended by clinical guidelines. Although treatment duration was not identified as a potential moderator of intervention efficacy either in this study or in previous reviews on CBT (Barth et al., Citation2013; Santoft et al., Citation2019), further studies should try to identify the ideal number of sessions to achieve a successful outcome. As emotional dysregulation is a common clinical feature in patients with depression (Aldao et al., Citation2010a; Sloan et al., Citation2017), and previous research has found that this association is mediated by the exposition to traumatic events (Christ et al., Citation2019), it would be interesting for future research to explore the impact of EMDR on emotional regulation. Furthermore, no study has been conducted so far to evaluate the neurobiological effects of EMDR in depression.
To date, there is preliminary evidence on the effects of EMDR therapy on adolescents with depression (Bae, Kim, & Park, Citation2008; Paauw, De Roos, Tummers, De Jongh, & Dingemans, Citation2019). Previous reviews have shown encouraging, although limited, results on the effectiveness of EMDR in reducing depressive symptoms secondary to PTSD in children and adolescents (Manzoni et al., Citation2021; Moreno-Alcázar et al., Citation2017). Future controlled studies are needed to further evaluate the effects of EMDR for depression as a primary target of the treatment among children and adolescents. Future studies should analyse possible adverse effects and rates of attrition from EMDR treatment, as these aspects are essential to inform clinical practice. Finally, it would be interesting to investigate the impact on the economic and social costs of treating depression with EMDR compared to other psychotherapies or pharmacotherapy.
5. Conclusion
The findings from this review suggest EMDR can be considered as an effective trauma-focused treatment for reducing symptoms of depression, although several methodological weaknesses were found in the included studies. Further studies are required in order to replicate these findings, improve methodological quality, and evaluate longer-term effects.
Data availability
The data that support the findings of this study are openly available in the GitHub repository at https://github.com/berkeley3/Eye-movement-desensitization-and-reprocessing-for-depression.
Data transparency statement
The authors declare that there are no previously published or in press works stemming from this same dataset.
Ethic statement
No institutional review board approval and informed consent were obtained as the study did not involve participants.
Supplemental Material
Download ()Disclosure statement
M.H., A.H. and L.O. are EMDR supervisors, M.H. and A.H. are EMDR trainers, S.C., M.H., A.H. and L.O. have been invited speakers at national and international EMDR conferences and S.C., M.H., A.H. and L.O. are the authors of four of the included studies. F.M., P.B., F.O. and N.C. declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010a). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–14. doi:10.1016/j.cpr.2009.11.004.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author. doi:10.1176/appi.books.9780890425596.
- Andersen, S. L., Tomada, A., Vincow, E. S., Valente, E., Polcari, A., & Teicher, M. H. (2008). Preliminary evidence for sensitive periods in the effect of childhood sexual abuse on regional brain development. JNP, 20(3), 292–301. doi:10.1176/jnp.2008.20.3.292.
- Bae, H., Kim, D., & Park, Y. C. (2008). Eye movement desensitization and reprocessing for adolescent depression. Psychiatry Investigation, 5(1), 60. doi:10.4306/pi.2008.5.1.60.
- Barry, E. S., Naus, M. J., & Rehm, L. P. (2006). Depression, implicit memory, and self: A revised memory model of emotion. Clinical Psychology Review, 26(6), 719–745. doi:10.1016/j.cpr.2005.06.003.
- Barth, J., Munder, T., Gerger, H., Nüesch, E., Trelle, S., Znoj, H., … Cuijpers, P. (2013). Comparative efficacy of seven psychotherapeutic interventions for patients with depression: A network meta-analysis. PLoS Medicine, 10(5), e1001454. doi:10.1371/journal.pmed.1001454.
- Behnammoghadam, M., Alamdari, A. K., Behnammoghadam, A., & Darban, F. (2015). Effect of eye movement desensitization and reprocessing (EMDR) on depression in patients with myocardial infarction (MI). Global journal of health science, 7(6), 258.
- Bisson, J. I., Roberts, N. P., Andrew, M., Cooper, R., & Lewis, C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.CD003388.pub4
- Caldji, C., Tannenbaum, B., Sharma, S., Francis, D., Plotsky, P. M., & Meaney, M. J. (1998). Maternal care during infancy regulates the development of neural systems mediating the expression of fearfulness in the rat. Proceedings of the National Academy of Sciences, 95(9), 5335–5340. doi:10.1073/pnas.95.9.5335.
- Carletto, S., Ostacoli, L., Colombi, N., Calorio, L., Oliva, F., Fernandez, I., & Hofmann, A. (2017). EMDR for depression: A systematic review of controlled studies. Clinical Neuropsychiatry: Journal of Treatment Evaluation, 15(5), 306–312.
- Christ, C., De Waal, M. M., Dekker, J. J. M., Van Kuijk, I., Van Schaik, D. J. F., Kikkert, M. J., … Messman-Moore, T. L. (2019). Linking childhood emotional abuse and depressive symptoms: The role of emotion dysregulation and interpersonal problems. PLoS ONE, 14(2), e0211882. doi:10.1371/journal.pone.0211882.
- Courtney, E., Kushwaha, M., & Johnson, J. (2008). Childhood emotional abuse and risk for hopelessness and depressive symptoms during adolescence. Journal of Emotional Abuse, 8(3), 281–298. doi:10.1080/10926790802262572.
- Crow, T., Cross, D., Powers, A., & Bradley, B. (2014). Emotion dysregulation as a mediator between childhood emotional abuse and current depression in a low-income African-American sample. Child Abuse & Neglect, 38(10), 1590–1598. doi:10.1016/j.chiabu.2014.05.015.
- Cuijpers, P., Huibers, M., Daniel Ebert, D., Koole, S. L., & Andersson, G. (2013). How much psychotherapy is needed to treat depression? A metaregression analysis. Journal of Affective Disorders, 149(1–3), 1–13. doi:10.1016/j.jad.2013.02.030.
- Cuijpers, P., Quero, S., Dowrick, C., & Arroll, B. (2019). Psychological treatment of depression in primary care: Recent developments. Current Psychiatry Reports, 21(12), 1–10. Amsterdam: Springer. doi:10.1007/s11920-019-1117-x.
- Cuijpers, P., Van Straten, A., Andersson, G., & Van Oppen, P. (2008). Psychotherapy for depression in adults: A meta-analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology, 76(6), 909–922. doi:10.1037/a0013075.
- Cuijpers, P., van Veen, S. C., Sijbrandij, M., Yoder, W., & Cristea, I. A. (2020). Eye movement desensitization and reprocessing for mental health problems: A systematic review and meta-analysis. Cognitive Behaviour Therapy, 49(3), 165–180. doi:10.1080/16506073.2019.1703801.
- Davey, C. G., Yücel, M., & Allen, N. B. (2008). The emergence of depression in adolescence: Development of the prefrontal cortex and the representation of reward. Neuroscience and Biobehavioral Reviews, 32(1), 1–19. doi:10.1016/j.neubiorev.2007.04.016.
- DerSimonian, R., & Laird, N. (1986). Meta-analysis in clinical trials. Controlled Clinical Trials, 7(3), 177–188. doi:10.1016/0197-2456(86)90046-2.
- Dominguez, S., Drummond, P., Gouldthorp, B., Janson, D., & Lee, C. W. (2021). A randomized controlled trial examining the impact of individual trauma‐focused therapy for individuals receiving group treatment for depression. Psychology and Psychotherapy: Theory, Research and Practice, 94(1), 81–100. doi:10.1111/papt.12268
- Egger, M., Smith, G. D., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. doi:10.1136/bmj.315.7109.629.
- Ernst, M., Pine, D. S., & Hardin, M. (2006). Triadic model of the neurobiology of motivated behavior in adolescence. Psychological Medicine, 36(3), 299–312. doi:10.1017/S0033291705005891.
- Gauhar, Y. W. (2016). The efficacy of EMDR in the treatment of depression. Journal of EMDR Practice and Research, 101, 59–69. doi:10.1891/1933-3196.10.2.59
- Hase, M., Balmaceda, U. M., Hase, A., Lehnung, M., Tumani, V., Huchzermeier, C., & Hofmann, A. (2015). Eye movement desensitization and reprocessing (EMDR) therapy in the treatment of depression: a matched pairs study in an inpatient setting. Brain and Behavior, 5(6), e00342. doi:10.1002/brb3.342
- Hase, M., Balmaceda, U. M., Ostacoli, L., Liebermann, P., & Hofmann, A. (2017). The AIP model of EMDR therapy and pathogenic memories. Frontiers in Psychology, 8, 1578. doi:10.3389/fpsyg.2017.01578.
- Hase, M., Plagge, J., Hase, A., Braas, R., Ostacoli, L., Hofmann, A., & Huchzermeier, C. (2018). Eye movement desensitization and reprocessing versus treatment as usual in the treatment of depression: A randomized-controlled trial. Frontiers in Psychology, 9, 1384. doi:10.3389/fpsyg.2018.01384.
- Hedges, L. V., & Olkin, I. (1985). Statistical methods for meta-analysis. Orlando, FL: Academic Press.
- Hertlein, K. M., & Ricci, R. J. (2004). A systematic research synthesis of EMDR studies: Implementation of the platinum standard. Trauma, Violence & Abuse, 5(3), 285–300. doi:10.1177/1524838004264340.
- Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M., & Welch, V. (2019). Cochrane handbook for systematic reviews of interventions (2nd ed). Chichester: John Wiley.
- Hofmann, A., Hase, M., Liebermann, P., Ostacoli, L., Lehnung, M., Ebner, F., … Tumani, V. (2016). DeprEnd©—EMDR therapy protocol for the treatment of depressive disorders. In M. Luber (Ed.), Eye movement desensitization and reprocessing (EMDR) therapy scripted protocols and summary sheets: Treating anxiety, obsessive-compulsive, and mood-related conditions (pp. 289–311). New York, NY: Springer Publishing Co.
- Hofmann, A., Hilgers, A., Lehnung, M., Liebermann, P., Ostacoli, L., Schneider, W., & Hase, M. (2014). Eye movement desensitization and reprocessing as an adjunctive treatment of unipolar depression: A controlled study. Journal of EMDR Practice and Research, 8(3), 103–112. doi:10.1891/1933-3196.8.3.103.
- Hogan, W. A. (2001). The comparative effects of eye movement desensitization and reprocessing (EMDR) and cognitive behavioral therapy (CBT) in the treatment of depression. Dissertation Abstracts International: Section B: The Sciences and Engineering, 62(2–B), 1082.
- Humphreys, K. L., LeMoult, J., Wear, J. G., Piersiak, H. A., Lee, A., & Gotlib, I. H. (2020). Child maltreatment and depression: A meta-analysis of studies using the childhood trauma questionnaire. Child Abuse & Neglect, 102, 104361. doi:10.1016/j.chiabu.2020.104361.
- Huot, R. L., Plotsky, P. M., Lenox, R. H., & McNamara, R. K. (2002). Neonatal maternal separation reduces hippocampal mossy fiber density in adult long evans rats. Brain Research, 950(1–2), 52–63. doi:10.1016/S0006-8993(02)02985-2.
- James, S. L., Abate, D., Abate, K. H., Abay, S. M., Abbafati, C., Abbasi, N., … Murray, C. J. L. (2018). Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the global burden of disease study 2017. The Lancet, 392(10159), 1789–1858. doi:10.1016/S0140-6736(18)32279-7.
- Johnston, K. M., Powell, L. C., Anderson, I. M., Szabo, S., & Cline, S. (2019). The burden of treatment-resistant depression: A systematic review of the economic and quality of life literature. Journal of Affective Disorders, 242, 195–210. doi:10.1016/j.jad.2018.06.045.
- Kraemer, H. C., & Kupfer, D. J. (2006). Size of treatment effects and their importance to clinical research and practice. Biological Psychiatry, 59(11), 990–996. doi:10.1016/j.biopsych.2005.09.014.
- Ladd, C. O., Huot, R. L., Thrivikraman, K. V., Nemeroff, C. B., Meaney, M. J., & Plotsky, P. M. (2000). Long-term behavioral and neuroendocrine adaptations to adverse early experience. Progress in brain research 122, 81–103. doi:10.1016/s0079-6123(08)62132-9.
- Lei, S., & Zhen-Ying, W. (2007). Comparative study of sertraline combined with EMDR in the treatment of depression. Journal of Clinical Psychosomatic, 4, 307–308.
- Lindhiem, O., Bennett, C. B., Trentacosta, C. J., & McLear, C. (2014). Client preferences affect treatment satisfaction, completion, and clinical outcome: A meta-analysis. Clinical Psychology Review, 34(6), 506–517. doi:10.1016/j.cpr.2014.06.002.
- Liu, D. (1997). Maternal care, hippocampal glucocorticoid receptors, and hypothalamic-pituitary-adrenal responses to stress. Science, 277(5332), 1659–1662. doi:10.1126/science.277.5332.1659.
- Maciejewski, P. K., & Mazure, C. M. (2006). Fear of criticism and rejection mediates an association between childhood emotional abuse and adult onset of major depression. Cognitive Therapy and Research, 30(1), 105–122. doi:10.1007/s10608-006-9012-2.
- Malandrone, F., Carletto, S., Hase, M., Hofmann, A., & Ostacoli, L. (2019). A brief narrative summary of randomized controlled trials investigating EMDR treatment of patients with depression. Journal of EMDR Practice and Research, 13(4), 302–306. doi:10.1891/1933-3196.13.4.302.
- Mandelli, L., Petrelli, C., & Serretti, A. (2015). The role of specific early trauma in adult depression: A meta-analysis of published literature. Childhood trauma and adult depression. European Psychiatry, 30(6), 665–680. doi:10.1016/j.eurpsy.2015.04.007.
- Manzoni, M., Fernandez, I., Bertella, S., Tizzoni, F., Gazzola, E., Molteni, M., & Nobile, M. (2021). Eye movement desensitization and reprocessing: The state of the art of efficacy in children and adolescent with post traumatic stress disorder. Journal of Affective Disorders, 282, 340–347. doi:10.1016/j.jad.2020.12.088.
- Meaney, M. J., Diorio, J., Francis, D., Widdowson, J., LaPlante, P., Caldji, C., … Plotsky, P. M. (1996). Early environmental regulation of forebrain glucocorticoid receptor gene expression: Implications for adrenocortical responses to stress. Developmental Neuroscience, 18(1–2), 61–72. doi:10.1159/000111396.
- Minelli, A., Zampieri, E., Sacco, C., Bazzanella, R., Mezzetti, N., Tessari, E., … Bortolomasi, M. (2019). Clinical efficacy of trauma-focused psychotherapies in treatment-resistant depression (TRD) in-patients: A randomized, controlled pilot-study. Psychiatry Research, 273, 567–574. doi:10.1016/j.psychres.2019.01.070.
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2010). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery, 8(5), 336–341. doi:10.1016/j.ijsu.2010.02.007.
- Moreno-Alcázar, A., Treen, D., Valiente-Gómez, A., Sio-Eroles, A., Pérez, V., Amann, B. L., & Radua, J. (2017). Efficacy of eye movement desensitization and reprocessing in children and adolescent with post-traumatic stress disorder: A meta-analysis of randomized controlled trials. Frontiers in Psychology, 8. doi:10.3389/fpsyg.2017.01750
- Nanni, V., Uher, R., & Danese, A. (2012). Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. AJP, 169(2), 141–151. doi:10.1176/appi.ajp.2011.11020335.
- National Institute for Health and Care Excellence. (2009). Depression in adults: Recognition and management. Clinical guideline [CG90]. https://www.nice.org.uk/guidance/cg90
- National Institute for Health and Care Excellence. (2018). Depression in adults: Treatment and management. NICE Guideline: Short Version Draft for Second Consultation. https://www.nice.org.uk/guidance/gid-cgwave0725/documents/short-version-of-draft-guideline
- Nelson, J., Klumparendt, A., Doebler, P., & Ehring, T. (2017). Childhood maltreatment and characteristics of adult depression: Meta-analysis. British Journal of Psychiatry, 210(2), 96–104. doi:10.1192/bjp.bp.115.180752.
- Nemeroff, C. B., Heim, C. M., Thase, M. E., Klein, D. N., Rush, A. J., Schatzberg, A. F., … Keller, M. B. (2003). Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma. Proceedings of the National Academy of Sciences, 100(24), 14293–14296. doi:10.1073/pnas.2336126100.
- Olkin, I., Dahabreh, I. J., & Trikalinos, T. A. (2012). GOSH - a graphical display of study heterogeneity: all-subsets meta-analysis for heterogeneity. Research Synthesis Methods, 3(3), 214–223. doi:10.1002/jrsm.1053.
- Ostacoli, L., Carletto, S., Cavallo, M., Baldomir-Gago, P., Di Lorenzo, G., Fernandez, I., ... & Hofmann, A. (2018). Comparison of eye movement desensitization reprocessing and cognitive behavioral therapy as adjunctive treatments for recurrent depression: The European Depression EMDR Network (EDEN) randomized controlled trial. Frontiers in psychology, 9, 74. doi:10.3389/fpsyg.2018.00074
- Paauw, C., De Roos, C., Tummers, J., De Jongh, A., & Dingemans, A. (2019). Effectiveness of trauma-focused treatment for adolescents with major depressive disorder. European Journal of Psychotraumatology, 10(1), 1682931. doi:10.1080/20008198.2019.1682931.
- Parikh, S. V., Segal, Z. V., Grigoriadis, S., Ravindran, A. V., Kennedy, S. H., Lam, R. W., & Patten, S. B. (2009). Canadian network for mood and anxiety treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. II. Psychotherapy alone or in combination with antidepressant medication. Journal of Affective Disorders, 117, S15–S25. doi:10.1016/j.jad.2009.06.042.
- Paterniti, S., Sterner, I., Caldwell, C., & Bisserbe, J.-C. (2017). Childhood neglect predicts the course of major depression in a tertiary care sample: A follow-up study. BMC Psychiatry, 17(1), 113. doi:10.1186/s12888-017-1270-x.
- Plotsky, P. M., & Meaney, M. J. (1993). Early, postnatal experience alters hypothalamic corticotropin-releasing factor (CRF) mRNA, median eminence CRF content and stress-induced release in adult rats. Molecular Brain Research, 18(3), 195–200. doi:10.1016/0169-328X(93)90189-V.
- R Development Core Team. (2019). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing.
- Rosenthal, R. (1991). Meta-analytic procedures for social research. London: SAGE. doi:10.4135/9781412984997
- Santoft, F., Axelsson, E., Öst, L. G., Hedman-Lagerlöf, M., Fust, J., & Hedman-Lagerlöf, E. (2019). Cognitive behaviour therapy for depression in primary care: Systematic review and meta-analysis. Psychological Medicine, 49(8), 1266–1274. Cambridge: Cambridge University Press. doi:10.1017/S0033291718004208.
- Schalinski, I., Teicher, M. H., Nischk, D., Hinderer, E., Müller, O., & Rockstroh, B. (2016). Type and timing of adverse childhood experiences differentially affect severity of PTSD, dissociative and depressive symptoms in adult inpatients. BMC Psychiatry, 16(1), 295. doi:10.1186/s12888-016-1004-5.
- Shapiro, F. (2001). Eye movement desensitization and reprocessing: Basic principles, protocols, and procedures (2nd ed.). New York: Guilford Press.
- Shapiro, F. (2018). Eye movement desensitization and reprocessing (EMDR) therapy: Basic principles, protocols, and procedures (3rd ed.). Guilford Press. http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2017-40757-000&site=ehost-live
- Slim, K., Nini, E., Forestier, D., Kwiatkowski, F., Panis, Y., & Chipponi, J. (2003). Methodological index for non-randomized studies (\textitMINORS): Development and validation of a new instrument: Methodological index for non-randomized studies. ANZ Journal of Surgery, 73(9), 712–716. doi:10.1046/j.1445-2197.2003.02748.x.
- Sloan, E., Hall, K., Moulding, R., Bryce, S., Mildred, H., & Staiger, P. K. (2017). Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clinical Psychology Review, 57, 141–163. Elsevier Inc. doi:10.1016/j.cpr.2017.09.002.
- Solomon, R. M., & Shapiro, F. (2008). EMDR and the adaptive information processing modelpotential mechanisms of change. Journal of EMDR Practice and Research, 2(4), 315–325. doi:10.1891/1933-3196.2.4.315.
- Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., … Higgins, J. P. T. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ, l4898. doi:10.1136/bmj.l4898
- Stulz, N., Lutz, W., Kopta, S. M., Minami, T., & Saunders, S. M. (2013). Dose–effect relationship in routine outpatient psychotherapy: Does treatment duration matter? Journal of Counseling Psychology, 60(4), 593–600. doi:10.1037/a0033589.
- Swift, J. K., Callahan, J. L., Cooper, M., & Parkin, S. R. (2018). The impact of accommodating client preference in psychotherapy: A meta-analysis. Journal of Clinical Psychology, 74(11), 1924–1937. doi:10.1002/jclp.22680.
- Tang, T. C., Yang, P., Yen, C. F., & Liu, T. L. (2015). Eye movement desensitization and reprocessing for treating psychological disturbances in Taiwanese adolescents who experienced Typhoon Morakot. The Kaohsiung journal of medical sciences, 31(7), 363–369.
- Valiente-Gómez, A., Moreno-Alcázar, A., Treen, D., Cedrón, C., Colom, F., Pérez, V., & Amann, B. L. (2017). EMDR beyond PTSD: A systematic literature review. Frontiers in Psychology, 8, 1668. doi:10.3389/fpsyg.2017.01668.
- Vittengl, J. R., Clark, L. A., Dunn, T. W., & Jarrett, R. B. (2007). Reducing relapse and recurrence in unipolar depression: A comparative meta-analysis of cognitive-behavioral therapy’s effects. Journal of Consulting and Clinical Psychology, 75(3), 475–488. doi:10.1037/0022-006X.75.3.475.
- Williams, L. M., Debattista, C., Duchemin, A.-M., Schatzberg, A. F., & Nemeroff, C. B. (2016). Childhood trauma predicts antidepressant response in adults with major depression: Data from the randomized international study to predict optimized treatment for depression. Translational Psychiatry, 6(5), e799–e799. doi:10.1038/tp.2016.61.
- Windle, E., Tee, H., Sabitova, A., Jovanovic, N., Priebe, S., & Carr, C. (2020). Association of patient treatment preference with dropout and clinical outcomes in adult psychosocial mental health interventions. JAMA Psychiatry, 77(3), 294. doi:10.1001/jamapsychiatry.2019.3750.
- Wood, E., & Ricketts, T. (2013). Is EMDR an evidenced-based treatment for depression? A review of the literature. Journal of EMDR Practice and Research, 7(4), 225–236. doi:10.1891/1933-3196.7.4.225.
- World Health Organization. (2017). World health statistics 2017: Monitoring health for the SDGs, sustainable development goals. https://apps.who.int/iris/handle/10665/255336
- Wright, M. O., Crawford, E., & Del Castillo, D. (2009). Childhood emotional maltreatment and later psychological distress among college students: The mediating role of maladaptive schemas. Child Abuse & Neglect, 33(1), 59–68. doi:10.1016/j.chiabu.2008.12.007.
- Zeng, X., Zhang, Y., Kwong, J. S. W., Zhang, C., Li, S., Sun, F., … Du, L. (2015). The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review: Methodological quality assessment tools. Journal of Evidence-Based Medicine, 8(1), 2–10. doi:10.1111/jebm.12141.