ABSTRACT
Background: Various studies have examined the psychological ‘typhoon eye’ and ‘ripple’ effects in mental disorders following COVID-19. However, these studies only considered the disorders as entities and assessed severity, and overlooked the differences in specific symptoms of disorders.
Objectives: This aim of the study is to assess the psychological typhoon eye and ripple effects at the symptom-level in posttraumatic stress disorder (PTSD), which is considered as a common psychopathology following the COVID-19 epidemic.
Method: In total, 1150 undergraduates, including 271 students from the Hubei province (e.g. epidemic centre) and 879 students from other provinces, completed the self-report questionnaire. The networks were estimated and compared using the R packages.
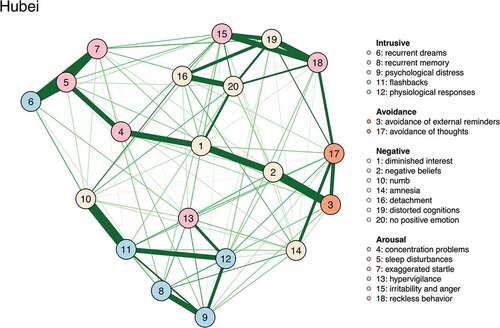
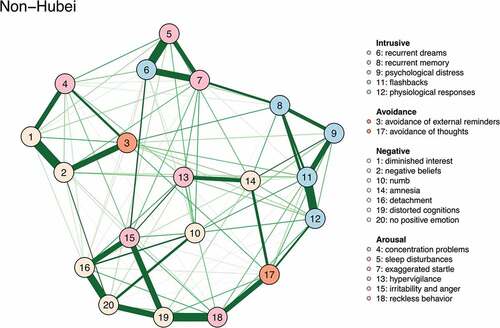
Results: Although the PTSD networks of Hubei and non-Hubei undergraduates were similarly connected and shared some symptoms with high centrality (e.g. flashbacks, irritability and anger), there were differences across the networks. Distorted cognition and no positive emotion only exhibited high centrality in the Hubei network. Physiological responses and exaggerated startle only exhibited high centrality in the non-Hubei network.
Conclusion: These findings suggested that the psychological typhoon eye and ripple effects may co-exist at the symptom level. Targeted and distinct psychological services for college students in Hubei and non-Hubei provinces should be emphasized following COVID-19.
HIGHLIGHTS
Irritability and anger flashbacks showed high levels of strength in both networks.
Distorted cognition and no positive emotion were the most central symptoms only in the Hubei network.
Physiological responses and exaggerated startle exhibited higher strength only in the non-Hubei network.
There was no significant difference in global connectivity between Hubei and non-Hubei PTSD network.
Antecedentes: Varios estudios han examinado los efectos psicológicos del ‘ojo del huracán’ y del ‘efecto dominó’ en los trastornos mentales posteriores al COVID-19. Sin embargo, estos estudios solo consideraron los trastornos como entidades y evaluaron la gravedad, pasando por alto las diferencias en los síntomas específicos de los trastornos.
Objetivos: El objetivo del estudio es evaluar los efectos psicológicos del ojo del huracán y el efecto dominó a nivel de los síntomas en el trastorno de estrés postraumático (TEPT), que se considera una psicopatología común después de la epidemia de COVID-19.
Método: En total, 1150 estudiantes de pregrado, incluyendo 271 estudiantes de la provincia de Hubei (por ejemplo, centro de la epidemia) y 879 estudiantes de otras provincias, completaron el cuestionario de autoinforme. Las redes se estimaron y compararon utilizando los paquetes R.
Resultados: Aunque las redes de TEPT de estudiantes universitarios de Hubei y que no eran de Hubei estaban conectadas de manera similar y compartían algunos síntomas con alta centralidad (por ejemplo, flashbacks, irritabilidad e ira), hubo diferencias entre las redes. La cognición distorsionada y sin emoción positiva solo mostraron una alta centralidad en la red de Hubei. Las respuestas fisiológicas y el sobresalto exagerado solo exhibieron una alta centralidad en la red que no era de Hubei.
Conclusión: Estos hallazgos sugirieron que los efectos psicológicos del ojo del huracán y el efecto dominó pueden coexistir al nivel de los síntomas. Se deben enfatizar los servicios psicológicos específicos y distintos para los estudiantes universitarios en las provincias de Hubei y que no eran de Hubei después de COVID-19.
背景: 各种研究考查了COVID-19后精神障碍的心理‘台风眼’和‘涟漪’效应。但是, 这些研究仅将疾病视为实体评估其严重性, 而忽略了特定疾病症状的差异。
目的: 本研究旨在评估COVID-19疫情后的常见的精神障碍——创伤后应激障碍 (PTSD) 在症状水平上的心理台风眼和涟漪效应。
方法: 共计1150名大学生, 包括271名湖北省 (例如疫情中心) 的学生和879名其他省份的学生, 完成了自我报告问卷。使用R包对网络进行估计和比较。
结果: 尽管湖北省和非湖北省大学生的PTSD网络具有相似的连接, 并共享一些高中心性症状 (例如, 闪回, 易激惹和愤怒), 网络之间存在差异。认知歪曲, 没有积极情绪仅在湖北网络中表现出高中心性。生理反应和过度的惊跳反应只在非湖北网络中表现出高中心性。
结论: 这些发现表明心理台风眼和涟漪效应可能在症状水平上并存。在COVID-19之后, 应强调针对湖北省和非湖北省大学生有针对性和区别性的心理服务。
PALABRAS CLAVE:
1. Introduction
The coronavirus disease 2019 (COVID-19) epidemic represented the first serious emergent public health crisis since the severe acute respiratory syndrome (SARS) outbreak. When a crisis threatens people’s lives, it may bring a series of negative psychological reactions. In the context of COVID-19, this was exacerbated by the high infectivity and fatality rates. Psychological problems in people following COVID-19 have attracted a large amount of research interest. A key focus area is posttraumatic stress disorder (PTSD), which is considered a common negative outcome in this context (Kang et al., Citation2020; Karatzias et al., Citation2020). For example, one study reported that the prevalence of PTSD was 12.8% (Liang et al., Citation2020), and Tang, Hu et al. (Citation2020) found that 2.7% of undergraduate students in Chongqing and Chengdu cities reported PTSD. In addition, Liu et al. (Citation2020) investigated adults in China’s hardest-hit area (i.e. Wuhan city) and found that 7.0% of adults were identified as probable PTSD cases following COVID-19.
Although the majority of available studies assessed the prevalence of PTSD following COVID-19, there is no consensus on this issue. A possible explanation is that different studies selected different participants in distinct areas, and the distance from the trauma epicentre may have various effects on PTSD (Wozniak et al., Citation2020). Two important but diametrically opposite mechanisms have been proposed to explain these effects. One mechanism is the psychological ‘ripple effect’ (Slovic, Citation1987), wherein a ripple is a vivid metaphor for the impact of risks associated with a crisis. For example, when a rock sinks to the bottom of a pool of water, the point of impact has the biggest wave and the wave then decreases with increasing distance from that point. That is, the nearer people are to the risk centre, the stronger their negative emotions (Slovic, 1978). Frans, Åhs, Bihre, and Åhs (Citation2018) explained this phenomenon as a conditional response, wherein the defensive responses of people closer to the epicentre were more likely to be reinforced by repeated exposure to trauma-related cues. Consequently, extinction of these memories and conditioned fear were exhibited, which is considered an important risk factor for PTSD. Research has shown that participants from the area hardest-hit by COVID-19 (Wuhan city) exhibited the most serious psychological symptoms (e.g. anxiety, insomnia), followed by people from the rest of Hubei and those from non-Hubei areas (Zhu et al., Citation2020).
In contrast to the psychological ‘ripple’ effect, the psychological ‘typhoon eye’ effect suggests that people may become calmer as the traumatic event is approached (Li et al., Citation2009). In this context, cognitive dissonance theory indicates there was a conflict between living in the devastated area and the idea that the devastated area was dangerous (Festinger & Carlsmith, Citation1959). As people in the devastated area found it hard to migrate to other places, they had to change their cognition of residence for their adjustment. Therefore, they might feel that the devastated area was not dangerous. However, people living in non-devastated areas might insist that the risk centre was dangerous because of the lack of such conflict. Research has demonstrated that people in areas hardest-hit by disasters showed fewer psychological symptoms than those in periphery areas of disasters (Tang et al., Citation2020; Xie, Stone, Zheng, & Zhang, Citation2011; Zheng et al., Citation2015).
Irrespective of these two contrasting theories and associated findings, we noted that previous studies focused on the incidence and severity of psychological disorders (Liang et al., Citation2020; Liu et al., Citation2020; Salehi et al., Citation2021; Tang, Zhang et al., Citation2020), and explained the difference in people’s psychological reaction in distinct areas from a latent disorder level (e.g. Li et al., Citation2009; Slovic, Citation1987). However, those studies had several limitations. First, they tended to consider a disorder an entity. Such studies were based on the commonsense hypothesis that a disorder can be considered a latent construct that gives rise to a set of symptoms (Armour, Fried, Deserno, Tsai, & Pietrzak, Citation2017; Borsboom & Cramer, Citation2013). In contrast to that hypothesis, network theory assumes that disorders are constructed based on the dynamic interactions of symptoms, and each symptom has its own function (Borsboom & Cramer, Citation2013; Robinaugh, Hoekstra, Toner, & Borsboom, Citation2020). A disorder is visualized with nodes and edges, which represent symptoms and the connections between these symptoms, respectively. In a symptom network, the importance of a symptom is highlighted by centrality. Symptoms with high centrality usually affect or influence other symptoms. Mental disorders arise when groups of symptoms actively maintain each other, leading to a cluster of psychopathological symptoms that becomes self-sustaining (Borsboom, Citation2017). Network theory suggests that differences in disorders among people from distinct areas may also reflect differences in specific symptoms, especially symptom centrality or connectivity.
Second, both the psychological ‘typhoon eye’ effect and the ‘ripple’ effect were developed from the perspective of the disorder as a whole. However, in terms of specific symptoms, some symptoms within a disorder may exhibit a psychological ‘typhoon eye’ effect, whereas others may exhibit a ripple effect. For example, people near the SARS epicentre exhibited higher levels of worry or fear during the outbreak than those further from the epicentre, suggesting a psychological ‘typhoon eye’ effect for anxiety symptoms (Xie et al., Citation2011). However, people in the area worst hit by COVID-19 were found to have more depressed affect than people in other areas (Tang, Hu et al., Citation2020), indicating the existence of a ripple effect. Therefore, we hypothesized that the two effects may co-occur within individuals at the symptom level.
A network analysis approach is an alternative way to address the limitations in the studies discussed above. As a new method, network analysis has been widely used to clarify the structure of PTSD and identify its core symptoms (Price, Legrand, Brier, & Hébert-Dufresne, Citation2019; Ross, Murphy, & Armour, Citation2018). However, no research has investigated the influence of trauma proximity, although individuals who were closer to a traumatic event may develop more posttraumatic stress symptoms than those further from the event (Wozniak et al., Citation2020). Therefore, the influence of trauma proximity on the PTSD network remains unclear. In addition, although PTSD networks have been examined in many studies (Armour et al., Citation2017; Bartels et al., Citation2019; Fried et al., Citation2018; Greene, Gelkopf, Epskamp, & Fried, Citation2018; Lazarov et al., Citation2019; Ross et al., Citation2018), no study has examined PTSD networks following a public health crisis. However, it is widely acknowledged that trauma type is a critical risk factor for PTSD (Hetzel-Riggin & Roby, Citation2013; Kessler et al., Citation2017). A public health crisis differs from human-made trauma or natural disasters, and has some unique features. For example, it usually breaks out suddenly and has huge and far-reaching impact on the public. In addition, the high infectivity and incubation period makes diseases such as COVID-19 risky and uncontrollable, which may interfere with people’s basic coping strategies. In this context, people were forced to adopt new approaches to deal with the crisis (Horesh & Brown, Citation2020). To eliminate the chance of being infected with COVID-19, people were advised to stay at home. However, personal quarantine may inhibit social support, which is a critical protective factor for PTSD (Blais et al., Citation2021; Nickerson et al., Citation2017). To advance these issues, we applied network analysis with PTSD. This will not only shed light on the relationship between the symptoms, but will also help to inform treatment priorities and improve treatment efficiency. The aims of this study were to: 1) estimate two PTSD symptom networks in two samples from Hubei and non-Hubei areas; 2) identify core symptoms in the two networks; 3) compare the two networks to assess the influence of distance on symptom association underlying the disorder and extend assumptions about the psychological typhoon eye and ripple effects.
2. Methods
2.1. Participants and procedures
This study was started on 9 May 2020, when COVID-19 was under control and alleviated in China. We conducted an Internet-based survey to assess psychological responses among college students because many universities had remained closed to reduce the likelihood of teachers and students being infected with COVID-19. The survey was administered via the WeChat platform, which is a free messaging and calling app commonly used in China. We contacted college counsellors and asked them to distribute the questionnaires to their students for completion. The response rate in this study was 86.92%. The exclusion criteria were: 1) missing area information; 2) participants who were graduate students; and 3) participants who did not answer carefully (e.g., choose the same option for all items). With this method, we recruited 1150 participants across several provinces in China; 271 students from Hubei province and 879 students from other provinces. Of the participants from Hubei province, 53.9% were female and the mean age was 19.95 (standard deviation [SD] = 1.85) years. Of participants from other provinces, 51.8% were female and the mean age was 20.33 (SD = 1.39) years. Preliminary analysis indicated a significant difference between Hubei and non-Hubei participants (t = −1.964, p = 0.050, df = 1148).
This project was approved by the Research Ethics Committee of the School of Medicine, Zhejiang University (No. 2019-051). Informed consent was obtained from all participants. No compensation was provided to participants, and graduate students were excluded from this study.
2.2. Measures
2.2.1. PTSD
Participants were asked to complete the self-report PTSD Checklist from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) (Weathers, Citation2013). This is a 20-item self-report scale designed to assess the occurrence and frequency of PTSD symptoms in relation to an event experienced by an individual. In the present study, participants rated the frequency of PTSD symptoms during the last 2 weeks on a 5-point scale from 0 (not at all/only once) to 4 (almost every day). The instrument has four subscales: intrusions, negative cognition and emotion alteration, avoidance, and hyperarousal. The sum of the subscale scores provides an estimation of overall PTSD severity score. To improve the validity of the measurement, we used COVID-19 as the item description. Cronbach’s α values for the Hubei group, non-Hubei group, and total sample were 0.95, 0.96, and 0.96, respectively.
2.3. Data analysis
2.3.1. Network estimation and visualization
We estimated regularized partial correlation networks based on the Gaussian graphical model using the R-package qgraph (Epskamp et al., Citation2012). The networks comprised nodes and edges, which represented the symptoms and association between two symptom nodes, respectively. The thickness of an edge reflected how closely the two symptoms were partially correlated and indicated the relationship between those two nodes independent of other nodes. We applied the graphic least absolute shrinkage and selection operator (GLASSO) as the penalization factor to remove some weak edges in the network graph. The tuning parameter (λ) was set at 0.5. We used the Fruchterman-Reingold algorithm for network visualization (Fruchterman & Reingold, Citation1991). With this method, stronger associations were depicted as thick edges and highly correlated nodes were arranged in closer proximity. Missing data were excluded from these analyses.
2.3.2. Stability
The stability of the network comprises edge stability and node centrality stability. Using the R-package bootnet (Epskamp et al., Citation2018), we sampled the data 1000 times with replacement, and then generated a distribution for the edge weight. The edge stability was represented by the 95% confidence interval (CI). Large and overlapping CIs indicated poor stability. Node centrality stability was characterized by the correlation stability (CS) coefficient using subset bootstraps, which resulted in dropping some participants and re-estimating the network. The CS coefficient means that the maximum percentage of the sample can be dropped, while the new network and the original network remain highly correlated. The threshold of the correlation coefficient was set at 0.7. Therefore, in this study, the CS coefficient equalled the maximum percentage of original participants when the correlation between the original and new networks was higher than 0.7. It is recommended that the CS coefficient should be above 0.5 and not below 0.25 (Epskamp et al., Citation2018).
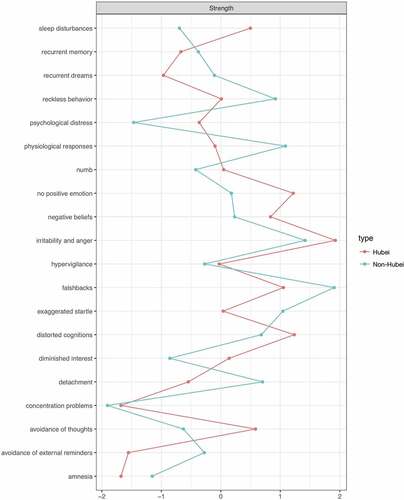
2.3.3. Centrality
As the closeness and betweenness were suggested to be unstable (Epskamp et al., Citation2018), centrality was measured only by the strength, quantified by the sum of the absolute value of the edge weight between a node and all of its neighbour nodes. With R-package bootnet (Epskamp et al., Citation2018), we plotted the normalized value of strength for each node in both networks. Higher strength values indicated a stronger influence on other symptoms. In addition, we conducted bootstrap analysis with resampling 1000 times to investigate differences in the centrality between a node and other nodes in each network.
2.3.4. Network comparisons
Following Lazarov et al. (Citation2019), we used simple random sampling to select 271 cases from the non-Hubei group to equalize the number of cases compared. Next, we tested the difference between the PTSD networks in the Hubei and non-Hubei groups using the R-package NCT (Van Borkulo, Citation2016). Network structure across groups was tested using the omnibus test, which calculates the invariance of the network. We also calculated the difference in global connectivity for 1000 times with the EBIC parameter set at 0.5, following the GLASSO procedure. Specifically, this evaluated the null hypothesis that the network connectivity was similar in the randomly regrouped permutations of participants. We also compared local connectivity across the Hubei and non-Hubei networks using the mean strength derived from the bootstrapped results in the stability assessment.
3. Results
3.1. Regularized partial correlation networks
The PTSD symptom networks of the Hubei and non-Hubei groups are depicted in , respectively. shows the centrality in the two networks. The correlations between the centrality values and their standard deviations in the Hubei and non-Hubei networks were 0.26 (p = .33) and −0.17 (p = .51), respectively. For the PTSD network in the Hubei group, we found that except for a weak edge for sleep disturbances-to-amnesia, all associations in this network were positive. The CS coefficient for strength in this network was 0.36 (see Figure S1, online supplementary data), which was considered acceptable in our standard. The edge weight accuracy is depicted in Figure S2, online supplementary data. Strong edges emerged for numb-to-flashbacks, sleep disturbances-to-recurrent dreams, negative beliefs-to-avoidance of external reminders, recurrent dreams-to-exaggerated startle, and diminished interest-to-negative beliefs. In this network, symptoms with the highest centrality included irritability and anger, distorted cognitions, no positive emotion, and flashbacks.
In the non-Hubei group network, most edges were positive. The edge weight accuracy is depicted in Figure S3, online supplementary data. The CS coefficient for strength was 0.60 (see Figure S4, online supplementary data), indicating that the non-Hubei network was highly stable. There were strong edges for diminished interest-to-negative beliefs, sleep disturbances-to-recurrent dreams, reckless behaviour-to-distorted cognitions, flashbacks-to-physiological responses, and detachment-to-no positive emotion. In the non-Hubei network, symptoms with the highest centrality were flashbacks, irritability and anger, physiological responses, and exaggerated startle. It is worth noting that the bootstrap results showed few significant differences between the centrality of symptoms in both networks (see Figures S5 and S6, online supplementary data). Therefore, the order of centrality should be interpreted with caution.
3.2. Network comparison
The network comparison test revealed that the network structure of the Hubei group was similar to that of the non-Hubei group (M = 0.23, p = 0.74). The difference in global connectivity in the two networks was not significant (S = 0.04, p = 0.79). Next, we conducted an independent samples t-test to compare the local connectivity of each node across groups. The results are shown in . Except for some symptoms in the NACM and arousal cluster (e.g. diminished interest, sleep disturbances), most nodes showed higher strength in the non-Hubei network.
Table 1. Comparison of node strength
4. Discussion
To our knowledge, this was the first study to examine and compare undergraduate students’ DSM-5-based PTSD networks between the COVID-19 epidemic centre (Hubei group) and other areas (non-Hubei group). We found the symptoms with high centrality differed between the two networks. Distorted cognition and no positive emotion appeared to be the most central symptoms in the Hubei PTSD network, but their characteristic of high strength disappeared in the non-Hubei PTSD network. Instead, physiological responses and exaggerated startle were the most central symptoms in the non-Hubei network. These findings provided new insights into the boundaries of the psychological typhoon eye and ripple effects, suggesting that these two effects may co-occur in individuals at the symptom level. Moreover, these findings helped to elucidate the relationship between trauma proximity and PTSD symptoms, and may inform targeted mental health interventions after public health crises.
Consistent with previous studies (Epskamp et al., Citation2018; Lazarov et al., Citation2019; Segal et al., Citation2020), we observed that flashbacks had high centrality in both networks with a robust effect. This finding indicated that flashbacks may play an important role in the development and maintenance of PTSD across different trauma types. Therefore, the flashback symptom should be at the core of intervention plans for PTSD in both Hubei and non-Hubei areas following the COVID-19 epidemic. Moreover, we found high centrality for irritability and anger in both networks. Although Sullivan et al. (Citation2018) reported similar results, high centrality of this symptom has rarely been reported in PTSD networks in other studies (Bryant et al., Citation2017; Pfeiffer et al., Citation2019). This inconsistent finding may be attributable to the distinctiveness of various traumatic events. In this study, we focused on COVID-19, which was a major public health crisis event with high infectivity and fatality rates. Human-to-human transmission of COVID-19 also meant the public tended to blame infected people and generated anger towards them (Trnka & Lorencova, Citation2020). During the COVID-19 outbreak, quarantine not only protected people from getting infected, but also limited their freedom, which might have increased family conflict (Guo, Feng, Wang, & van Ijzendoorn, Citation2020) and led to deteriorated interpersonal relationships. Subsequently, irritability and anger may stand out as a result of inner energy accumulation.
Interestingly, we found that the physiological responses and exaggerated startle symptoms exhibited higher strength in the non-Hubei network than in the Hubei network, suggesting that the psychological ‘typhoon eye’ effect may exist at the PTSD symptom level. This variation was also supported by the results of the local connectivity comparison, as the strength of the two nodes was significantly higher in the non-Hubei network. This extended evidence from extant studies that the psychological typhoon eye effect existed in traumatized individuals in terms of the severity of psychological diagnosis (Li et al., Citation2009; Zheng et al., Citation2015), and suggested this effect may also be reflected in the influence of symptoms. Undergraduates outside Hubei used various media to learn about the COVID-19 situation; unlike undergraduates in Hubei who could automatically correct exaggerated information, the lack of direct experience might have led to unnecessary speculation among those outside of Hubei. As a result, they might have been more sensitive to COVID-19-related cues in their daily life. From a theoretical perspective, this result echoed the mere exposure theory (Melber et al., Citation1977). That is, repeated and directed exposure to the pandemic reduced sensitivity to it. As participants in Hubei might have become used to the situation of someone around them contracting COVID-19, they might have been calmer than participants outside Hubei. Therefore, the physiological responses and exaggerated startle symptoms would be less likely to occur and influence other symptoms in the network.
We also found the psychological ‘ripple’ effect at the PTSD symptom level, wherein distorted cognition and no positive emotion were the most central symptoms in the Hubei network. However, this high centrality disappeared in the non-Hubei network. The results for local connectivity showed that no positive emotion was stronger in the Hubei network, which was consistent with alterations in core symptoms. This suggested that the psychological ripple effect may be reflected in both the severity of a psychological diagnosis and the influence at the symptom level. This shed light on reports from extant studies that the psychological ripple effect existed in the severity of psychopathologies (Frans et al., Citation2018). The shattered assumptions theory posits that people’s beliefs about the self, others, and the world are stable before trauma, but the traumatic event challenges existing belief systems, thereby causing a series of negative psychological reactions (Janoff-Bulman, Citation2010). For participants in Hubei, severe exposure to the pandemic led to an imbalance in their stable belief system, which might have induced a series of negative beliefs. Consequently, negative emotion was more likely to be activated.
Although we found differences in specific nodes in local connectivity between the two groups of college students, the global connectivity of PTSD networks in the Hubei and non-Hubei groups was similar, indicating that psychological interventions for those in non-Hubei areas required the same attention as those in the Hubei area. Network theory suggests that mental disorders arise because of the presence of hysteresis in strongly connected symptom networks, implying that symptoms continue to activate each other even after the triggering cause of the disorder has disappeared, meaning the disorder persists for a long time (Borsboom, Citation2017; McNally, Citation2016; Robinaugh et al., Citation2020). Therefore, the present study indicated that participants in both areas might be prone to the hysteresis that contributes to the persistence of PTSD. The finding of similar global connectivity of the Hubei and non-Hubei PTSD networks has two possible explanations. First, COVID-19 was a worldwide public health crisis that affected everyone; therefore, people might have similar psychological responses when confronted with the disease. Second, the amount of information about COVID-19 from various media channels was overwhelming. People living non-Hubei provinces might have perceived the negative effect of the COVID-19 epidemic on others and therefore suffered from vicarious trauma (McCann & Pearlman, Citation1990). Consequently, they would exhibit similar PTSD networks to people in Hubei.
This study had several limitations that should be noted. First, this was a cross-sectional study, and we could not draw conclusions about causal relationships among these symptoms and elucidate the change tendency of symptoms in the PTSD networks. Second, although we divided the sample into a Hubei group and a non-Hubei group, the difference in the number of participants in the two groups might have influenced the accuracy of our results. Moreover, only including a sample of college students exposed to COVID-19 limited the generalizability of the present results. Finally, the assumptions of node distinctiveness and exchanges were not completely met, which might affect the accuracy of the results (Bringmann et al., Citation2019; Bulteel et al., Citation2016; Hallquist et al., Citation2019).
Despite these limitations, this study examined and compared DSM-5 criteria-based PTSD networks in undergraduate students between the COVID-19 epidemic centre and other areas. We found that psychological ‘typhoon eye’ and ‘ripple’ effects co-existed at the symptom level. Although the global connectivity was similar in the two networks, they had distinct symptoms with high centrality. Our study has extended previous findings of PTSD networks after different traumatic events (Li et al., Citation2009; Zheng et al., Citation2015). In addition, this study clarified the effect of distance on PTSD from a network perspective. From a practical perspective, it is important to highlight that although attention has been directed to the mental health status of people in the epicentre, people in periphery areas should not be ignored. Targeted plans for psychological interventions should be emphasized for people in both Hubei and non-Hubei areas. In addition to an emphasis on flashbacks and irritability in both areas, more effort is needed to relieve negative alterations in cognition and mood for people in Hubei. For people in peripheral areas, more attention should be directed to relieving intrusive and arousal symptoms.
Supplemental Material
Download ()Data availability statement
The data that support the findings of this study are available from the first author, RS, upon reasonable request.
Supplementary material
Supplemental data for this article can be accessed here.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Armour, C., Fried, E. I., Deserno, M. K., Tsai, J., & Pietrzak, R. H. (2017). A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in U.S. military veterans. Journal of Anxiety Disorders, 45, 49–10. doi:10.1016/j.janxdis.2016.11.008
- Bartels, L., Berliner, L., Holt, T., Jensen, T., Jungbluth, N., Plener, P., … Sachser, C. (2019). The importance of the DSM-5 posttraumatic stress disorder symptoms of cognitions and mood in traumatized children and adolescents: Two network approaches. Journal of Child Psychology and Psychiatry, 60(5), 545–554. doi:10.1111/jcpp.13009
- Blais, R. K., Tirone, V., Orlowska, D., Lofgreen, A., Klassen, B., Held, P., … Zalta, A. K. (2021). Self-reported PTSD symptoms and social support in U.S. military service members and veterans: A meta-analysis. European Journal of Psychotraumatology, 12(1), 1851078. doi:10.1080/20008198.2020.1851078
- Borsboom, D. (2017). A network theory of mental disorders. World Psychiatry, 16(1), 5–13. doi:10.1002/wps.20375
- Borsboom, D., & Cramer, A. O. J. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9(1), 91–121. doi:10.1146/annurev-clinpsy-050212-185608
- Bringmann, L. F., Elmer, T., Epskamp, S., Krause, R. W., Schoch, D., Wichers, M., … Snippe, E. (2019). What do centrality measures measure in psychological networks? Journal of Abnormal Psychology, 128(8), 892–903. doi:10.1037/abn0000446
- Bryant, R. A., Creamer, M., O’Donnell, M., Forbes, D., McFarlane, A. C., Silove, D., & Hadzi-Pavlovic, D. (2017). Acute and chronic posttraumatic stress symptoms in the emergence of posttraumatic stress disorder: A network analysis. JAMA Psychiatry, 74(2), 135. doi:10.1001/jamapsychiatry.2016.3470
- Bulteel, K., Tuerlinckx, F., Brose, A., & Ceulemans, E. (2016). Using raw VAR regression coefficients to build networks can be misleading. Multivariate Behavioral Research, 51(2–3), 330–344. doi:10.1080/00273171.2016.1150151
- Epskamp, S., Borsboom, D., & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212. doi:10.3758/s13428-017-0862-1
- Epskamp, S., Cramer, A. O. J., Waldorp, L. J., Schmittmann, V. D., & Borsboom, D. (2012). qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software, 48(4). doi:10.18637/jss.v048.i04
- Festinger, L., & Carlsmith, J. M. (1959). Cognitive consequences of forced compliance. The Journal of Abnormal and Social Psychology, 58(2), 203–210. doi:10.1037/h0041593
- Frans, Ö., Åhs, J., Bihre, E., & Åhs, F. (2018). Distance to threat and risk of acute and posttraumatic stress disorder following bank robbery: A longitudinal study. Psychiatry Research, 267, 461–466. doi:10.1016/j.psychres.2018.06.050
- Fried, E. I., Eidhof, M. B., Palic, S., Costantini, G., Huisman-van Dijk, H. M., Bockting, C. L. H., … Karstoft, K.-I. (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: A cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science, 6(3), 335–351. doi:10.1177/2167702617745092
- Fruchterman, T. M. J., & Reingold, E. M. (1991). Graph drawing by force-directed placement. Software: Practice and Experience, 21(11), 1129–1164. doi:10.1002/spe.4380211102
- Greene, T., Gelkopf, M., Epskamp, S., & Fried, E. (2018). Dynamic networks of PTSD symptoms during conflict. Psychological Medicine, 48(14), 2409–2417. doi:10.1017/S0033291718000351
- Guo, J., Feng, X. L., Wang, X. H., & van Ijzendoorn, M. H. (2020). Coping with COVID-19: Exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. International Journal of Environmental Research and Public Health, 17(11), 3857. doi:10.3390/ijerph17113857
- Hallquist, M. N., Wright, A. G. C., & Molenaar, P. C. M. (2019). Problems with centrality measures in psychopathology symptom networks: Why network psychometrics cannot escape psychometric theory. Multivariate Behavioral Research, 1–25. doi:10.1080/00273171.2019.1640103
- Hetzel-Riggin, M. D., & Roby, R. P. (2013). Trauma type and gender effects on PTSD, general distress, and peritraumatic dissociation. Journal of Loss and Trauma, 18(1), 41–53. doi:10.1080/15325024.2012.679119
- Horesh, D., & Brown, A. D. (2020). Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy, 12(4), 331–335. doi:10.1037/tra0000592
- Janoff-Bulman, R. (2010). Shattered assumptions. New York: Simon and Schuster.
- Kang, L., Li, Y., Hu, S., Chen, M., Yang, C., Yang, B. X., … Liu, Z. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry, 7(3), e14. doi:10.1016/S2215-0366(20)30047-X
- Karatzias, T., Shevlin, M., Murphy, J., McBride, O., Ben‐Ezra, M., Bentall, R. P., … Hyland, P. (2020). Posttraumatic stress symptoms and associated comorbidity during the COVID‐19 pandemic in Ireland: A population-based study. Journal of Traumatic Stress, jts.22565. doi:10.1002/jts.22565
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., … Koenen, K. C. (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. doi:10.1080/20008198.2017.1353383
- Lazarov, A., Suarez-Jimenez, B., Levi, O., Coppersmith, D. D. L., Lubin, G., Pine, D. S., … Neria, Y. (2019). Symptom structure of PTSD and co-morbid depressive symptoms – A network analysis of combat veteran patients. Psychological Medicine, 1–17. doi:10.1017/S0033291719002034
- Li, S., Rao, -L.-L., Ren, X.-P., Bai, X.-W., Zheng, R., Li, J.-Z., … Liu, H. (2009). Psychological typhoon eye in the 2008 Wenchuan earthquake. PLoS ONE, 4(3), e4964. doi:10.1371/journal.pone.0004964
- Liang, L., Gao, T., Ren, H., Cao, R., Qin, Z., Hu, Y., … Mei, S. (2020). Post-traumatic stress disorder and psychological distress in Chinese youths following the COVID-19 emergency. Journal of Health Psychology, 25(9), 1164–1175. doi:10.1177/1359105320937057
- Liu, N., Zhang, F., Wei, C., Jia, Y., Shang, Z., Sun, L., … Liu, W. (2020). Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Research, 287, 112921. doi:10.1016/j.psychres.2020.112921
- McCann, I. L., & Pearlman, L. A. (1990). Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress, 3(1), 131–149. doi:10.1007/BF00975140
- McNally, R. J. (2016). Can network analysis transform psychopathology? Behaviour Research and Therapy, 86, 95–104. doi:10.1016/j.brat.2016.06.006
- Melber, B. D., Nealey, S. M., Hammersla, J., & Rankin, W. L. (1977). Nuclear power and the public: Analysis of collected survey research (PNL-2430, 5234344). doi:10.2172/5234344
- Nickerson, A., Creamer, M., Forbes, D., McFarlane, A. C., O’Donnell, M. L., Silove, D., … Bryant, R. A. (2017). The longitudinal relationship between post-traumatic stress disorder and perceived social support in survivors of traumatic injury. Psychological Medicine, 47(1), 115–126. doi:10.1017/S0033291716002361
- Pfeiffer, E., Sukale, T., Müller, L. R. F., Plener, P. L., Rosner, R., Fegert, J. M., … Unterhitzenberger, J. (2019). The symptom representation of posttraumatic stress disorder in a sample of unaccompanied and accompanied refugee minors in Germany: A network analysis. European Journal of Psychotraumatology, 10(1), 1675990. doi:10.1080/20008198.2019.1675990
- Price, M., Legrand, A. C., Brier, Z. M. F., & Hébert-Dufresne, L. (2019). The symptoms at the center: Examining the comorbidity of posttraumatic stress disorder, generalized anxiety disorder, and depression with network analysis. Journal of Psychiatric Research, 109, 52–58. doi:10.1016/j.jpsychires.2018.11.016
- Robinaugh, D. J., Hoekstra, R. H. A., Toner, E. R., & Borsboom, D. (2020). The network approach to psychopathology: A review of the literature 2008–2018 and an agenda for future research. Psychological Medicine, 50(3), 353–366. doi:10.1017/S0033291719003404
- Ross, J., Murphy, D., & Armour, C. (2018). A network analysis of DSM-5 posttraumatic stress disorder and functional impairment in UK treatment-seeking veterans. Journal of Anxiety Disorders, 57, 7–15. doi:10.1016/j.janxdis.2018.05.007
- Salehi, M., Amanat, M., Mohammadi, M., Salmanian, M., Rezaei, N., Saghazadeh, A., & Garakani, A. (2021). The prevalence of post-traumatic stress disorder related symptoms in Coronavirus outbreaks: A systematic-review and meta-analysis. Journal of Affective Disorders, 282, 527–538. doi:10.1016/j.jad.2020.12.188
- Segal, A., Wald, I., Lubin, G., Fruchter, E., Ginat, K., Ben Yehuda, A., … Bar-Haim, Y. (2020). Changes in the dynamic network structure of PTSD symptoms pre-to-post combat. Psychological Medicine, 50(5), 746–753. doi:10.1017/S0033291719000539
- Slovic, P. (1987). Perception of risk. Science, 236(4799), 280–285. doi:10.1126/science.3563507
- Sullivan, C. P., Smith, A. J., Lewis, M., & Jones, R. T. (2018). Network analysis of PTSD symptoms following mass violence. Psychological Trauma: Theory, Research, Practice, and Policy, 10(1), 58–66. doi:10.1037/tra0000237
- Tang, P. M., Zhang, S. X., Li, C. H., & Wei, F. (2020). Geographical identification of the vulnerable groups during COVID ‐19 crisis: Psychological typhoon eye theory and its boundary conditions. Psychiatry and Clinical Neurosciences, 74(10), 562–563. doi:10.1111/pcn.13114
- Tang, W., Hu, T., Hu, B., Jin, C., Wang, G., Xie, C., … Xu, J. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of Affective Disorders, 274, 1–7. doi:10.1016/j.jad.2020.05.009
- Trnka, R., & Lorencova, R. (2020). Fear, anger, and media-induced trauma during the outbreak of COVID-19 in the Czech Republic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(5), 546–549. doi:10.1037/tra0000675
- Van Borkulo, C. D. (2016). NetworkNetworkComparisonTest: Statistical comparison of two networks based on three invariance measures. Retrieved from https://CRAN.R-project.org/package=NetworkComparisonTest
- Weathers, F. W. (2013, November). The PTSD checklist for DSM–5 (PCL-5): Development and initial psychometric analysis. Paper presented at the 29th annual meeting of the International Society for Traumatic Stress Studies, Philadelphia, PA.
- Wozniak, J. D., Caudle, H. E., Harding, K., Vieselmeyer, J., & Mezulis, A. H. (2020). The effect of trauma proximity and ruminative response styles on posttraumatic stress and posttraumatic growth following a university shooting. Psychological Trauma: Theory, Research, Practice, and Policy, 12(3), 227–234. doi:10.1037/tra0000505
- Xie, X.-F., Stone, E., Zheng, R., & Zhang, R.-G. (2011). The ‘Typhoon Eye Effect’: Determinants of distress during the SARS epidemic. Journal of Risk Research, 14(9), 1091–1107. doi:10.1080/13669877.2011.571790
- Zheng, R., Rao, -L.-L., Zheng, X.-L., Cai, C., Wei, Z.-H., Xuan, Y.-H., & Li, S. (2015). The more involved in lead-zinc mining risk the less frightened: A psychological typhoon eye perspective. Journal of Environmental Psychology, 44, 126–134. doi:10.1016/j.jenvp.2015.10.002
- Zhu, X., Hu, Y., Wang, T., Zhong, J., Yan, Y., Guo, X., … Jiang, G. (2020). Psychological symptoms of the public during the COVID-19 epidemic. Chinese Mental Health Journal, 34, (8), 703–709. doi:10.3969/j..1000-6729.2020.8.013