ABSTRACT
Background: Sexual assault (SA) is highly prevalent in Belgium. In order to mitigate the negative consequences for victims of acute SA, Sexual Assault Care Centres (SACCs) were piloted from October 2017 to October 2018 in three Belgian hospitals. SACCs offer medical and psychological care, forensic examination and the possibility to report to the police at the SACC.
Objective: Aiming to improve SACC services, we quantitatively assessed the number and characteristics of victims attending the SACC, the SA they experienced, and the care they received over 12 months upon admission.
Method: Data on victims presenting at the SACC were routinely collected in electronic patient files by the SACC personnel between 25 October 2017 and 31 October 2019. These data were analysed in IBM SPSS Statistics 25.
Results: Within the first year 931 victims attended the SACCs. Mean age was 24.5 years (SD = 12.8), and one-third were under 18. The majority were female (90.5%) and 63.1% presented for rape. About one-third of the victims were considered vulnerable due to previous SA (35.6%), prior psychiatric consultation (38.7%) or disability (8.5%). The assailant was known to the victim in 59.2% of the cases. Of all SACC presentations, 35.2% self-referred to the SACC while 40.9% were referred by the police. Two out of three victims attended the SACC within 72 h post-assault. Respectively 74.7% of victims received medical care, 60.6% a forensic examination, 50.2% psychological care, and 68.7% reported to the police.
Conclusion: Despite the absence of promotion campaigns, the SACCs received a high number of victims during the pilot year. Use of acute and follow-up services was high, although new approaches to offer more accessible psychological support should be explored. The big proportion of vulnerable victims warrants careful monitoring and adaptation of care pathways.
HIGHLIGHTS
Belgian Sexual Assault Centres received 931 victims in the 1st year, mostly being young women raped by a known assailant.
Uptake of medical care, forensic examination and police reporting was high.
Easier accessible psychological follow-up support is needed.
Antecedentes: El asalto sexual (SA en si sigla en inglés) es altamente prevalente en Bélgica. Para mitigar las consecuencias negativas para las víctimas de SA agudo, los Centros de Atención de Asalto Sexual (SACCs en su sigla en inglés) fueron piloteados desde octubre de 2017 hasta octubre 2018 en tres hospitales belgas. Los SACCs ofrecen atención médica y psicológica, examen forense y la posibilidad de reportar a la policía en el SACC.
Objetivo: Para mejorar los servicios SACC, medimos cuantitativamente el número y las características de las víctimas atendidas por el SACC, el SA que experimentaron y la atención que recibieron a lo largo de los 12 meses desde su admisión.
Método: Fueron recolectados rutinariamente los datos en las víctimas que se presentaron en el SACC por el personal de SACC en los archivos electrónicos de los pacientes entre el 25 de octubre 2017 y 31 de octubre de 2019. Estos datos fueron analizados en el Programa Estadístico IBM SPSS 25.
Resultados: Dentro del primer año, 931 victimas asistieron a los SCCs. La edad media fue 24,5 (DE = 12.8), y un tercio eran menores de 18 años. La mayoría eran mujeres (90.5%) y 63.1% se presentaron por violación. Alrededor de un tercio de las víctimas fueron consideradas vulnerables debido a SA previos (35.6%), consulta psiquiátrica anterior (38.7%) o discapacidad (8.5%). El asaltante era un conocido de la víctima en 59.2% de los casos. De todas las presentaciones SACC, el 35.2% se autoderivaron a SACC, mientras que 40.9% fueron derivados por la policía. Dos de cada tres víctimas asistieron al SACC dentro de las primeras 72 horas luego del asalto. Respectivamente, el 74.7% de las víctimas recibieron atención médica, el 60.6% un examen forense, el 50.2% atención psicológica, y el 68.7% reportaron a la policía.
Conclusión: A pesar de la ausencia de campañas de promoción, los SACCs recibieron un gran número de víctimas durante el año piloto. El uso de servicios agudos y de seguimiento fueron altos, aunque nuevas perspectivas para ofrecer más apoyo psicológico más accesible deberían ser exploradas. La mayor proporción de víctimas vulnerables garantiza un monitoreo cuidadoso y la adaptación de las vías de atención.
背景: 性侵犯 (SA) 在比利时非常普遍。为了减轻对急性SA患者的负性影响, 自2017年10月至2018年10月, 在比利时的三家医院试行了性侵犯护理中心 (SACC) 。SACC提供医疗和心理护理, 法医检查, 并可以在SACC报警。
目的: 为了改善SACC服务, 我们定量评估了参加SACC的受害者的人数和特征, 他们所经历的SA以及入院后12个月内所获得的护理。
方法: 在2017年10月25日至2019年10月31日之间, SACC人员定期收集SACC的受害者数据到电子病人档案。这些数据在IBM SPSS Statistics 25中进行了分析。
结果:第一年有931名受害者参加了SACC。平均年龄为24.5岁 (SD = 12.8), 三分之一未满18岁。大多数为女性 (90.5%), 有63.1%的人报告了被强奸。大约三分之一的受害者由于先前的SA (35.6%), 先前的精神科咨询 (38.7%) 或残疾 (8.5%) 而被视为易感。在59.2%的案件中, 受害者认识袭击者。在所有SACC报告中, 有35.2%是自己承认的, 而40.9%是由警察指出的。三分之二的受害者在袭击后72小时内参加了SACC。分别有74.7%的受害者接受了医疗护理, 60.6%接受了法医检查, 50.2%接受了心理护理, 以及68.7%报了警。
结论: 尽管没有开展宣传运动, 但在试行年度, SACC接待了大量受害者。尽管应该探索新方法以提供更容易获得的心理支持, 急诊和后续服务的使用率很高。很大一部分易感的受害者需要对照料途径进行仔细的监测和调整。
PALABRAS CLAVE:
1. Introduction
Sexual assault (SA) is highly prevalent in Europe. The World Health Organization (WHO) estimates that 25.4% of European women experienced physical and/or sexual violence by their partner or ex-partner, and 5.2% were sexually victimized by another type of assailant (García-Moreno et al., Citation2013). A systematic review states that 11.5% of women in Western Europe ever experienced non-partner sexual violence (Abrahams et al., Citation2014). In European young adults, approximately 20% to 52% of females and 10% to 56% of males reported having experienced at least one event of physical sexual victimization since the age of legally consenting to sex. More specifically in Belgium, incidence of sexual violence since the age of 16 was 20.4% for women and 10.1% for men between 18 and 27 years (Krahe et al., Citation2015). A study in Flanders found lifetime sexual victimization to be respectively 13.8% and 2.4% for adult women and men (Buysse et al., Citation2013) and a recent Belgian survey showed that 20% of women and 14% of men had ever been raped (Etude des opinions et des comportements, Citation2019). However, representative prevalence data regarding sexual victimization in Belgium is lacking (Keygnaert et al., Citation2018). Some groups are considered to be at an even higher risk of SA, such as children and adolescents (Finkelhor, Shattuck, Turner, & Hamby, Citation2014; Vrolijk-Bosschaart, Brilleslijper-Kater, Benninga, Lindauer, & Teeuw, Citation2018), refugees and migrants (De Schrijver, Vander Beken, Krahe, & Keygnaert, Citation2018), and lesbian, gay, bisexual and/or transgender people (European Union lesbian, gay, bisexual and transgender survey, Citation2013).
Victims of SA are at increased risk of developing long-term sexual, reproductive, physical and mental health problems (Dworkin, Menon, Bystrynski, & Allen, Citation2017; García-Moreno et al., Citation2013; Jina & Thomas, Citation2013; Linden, Citation2011; Santaularia et al., Citation2014; Sena et al., Citation2015). Consequently, these problems may negatively impact on the victims’ wellbeing and their capabilities to participate in society (Perilloux, Duntley, & Buss, Citation2012; Rees et al., Citation2011). Hence, adapted care for victims of SA is needed to mitigate these negative consequences.
The response to victims of SA has often been inadequate. Few victims report to health services or to the police, victims risk secondary traumatization when seeking post-assault care, and formal support services often fail to address the victim’s diverse needs (Campbell R, Citation2008). To tackle these problems, it is internationally recommended to provide comprehensive patient-centred and age-adapted care to victims of SA, whereby medical, forensic, and psychosocial needs are addressed both in the direct aftermath of the assault as during follow-up (CDC, Citation2015; Eogan, McHugh, & Holohan, Citation2013; Garcia-Moreno et al., Citation2015; NICE, Citation2018; WHO, Citation2015, Citation2017a, Citation2004, Citation2017b). Research has shown that coordinated and comprehensive care leads to a better quality of care, increased use of services, better recovery, and improved legal outcomes (Campbell et al., Citation2014; Campbell, Patterson, & Bybee, Citation2012; Campbell, Patterson, & Lichty, Citation2005; Greeson & Campbell, Citation2013; Nesvold, Worm, Vala, & Agnarsdottir, Citation2005).
In order to provide such comprehensive care, several European countries such as the UK, Scandinavian countries and the Netherlands, successfully established sexual assault centres (SACs) since the mid 1980s (Bicanic et al., Citation2014; Hagemann et al., Citation2013; Ingemann-Hansen, Sabroe, Brink, Knudsen, & Charles, Citation2009; Kerr, Cottee, Chowdhury, Jawad, & Welch, Citation2003; Larsen, Hilden, & Lidegaard, Citation2015; Nesvold, Friis, & Ormstad, Citation2008; Nesvold et al., Citation2005; Tiihonen Moller, Backstrom, Sondergaard, Helstrom, & Dalal, Citation2014; Vik, Nottestad, Schei, Rasmussen, & Hagemann, Citation2019; Zijlstra et al., Citation2017). European SACs predominantly reach young women. Several studies have reported that an important share of SA victims has a prior vulnerability due to mental health issues, previous sexual victimization, cognitive or physical disabilities (Bicanic et al., Citation2014; Brooker & Durmaz, Citation2015; Brooker, Tocque, & Paul, Citation2018; Creighton & Jones, Citation2012; Larsen et al., Citation2015; Majeed‐Ariss, Rodriguez, & White, Citation2020; Manning, Majeed-Ariss, Mattison, & White, Citation2019; Nesvold et al., Citation2008; Vik et al., Citation2019; Zijlstra et al., Citation2017). Service utilization is overall noted as high with a majority of victims receiving medical care, a forensic examination, follow-up by a case manager and reporting to the police (Bicanic et al., Citation2014; Kerr et al., Citation2003; Larsen et al., Citation2015; Nesvold et al., Citation2008, Citation2005; Zijlstra et al., Citation2017). However, some SACs observe a poorer attendance for medical and psychological follow-up appointments (Kerr et al., Citation2003; Nesvold et al., Citation2008). SACs in the UK experience challenges in referring victims to appropriate mental health services (Brooker & Durmaz, Citation2015). Several SACs observed differences in victim and SA characteristics among minors and adults (Khadr et al., Citation2018; Zijlstra et al., Citation2017), and developed age-specific care paths.
Until recently, post-rape care in Belgium remained fragmented and suboptimal for both adults and minors. Many hospitals lack standardized protocols, and health care workers are often short of knowledge and experience in dealing with these victims (Gilles et al., Citation2019; Gilles, Van Loo, & Rozenberg, Citation2010; Hendriks, Vandenberghe, Peeters, Roelens, & Keygnaert, Citation2018; Vandenberghe, Hendriks, Peeters, Roelens, & Keygnaert, Citation2018). Rape victims deplore the absence of patient-centred services, the lack of services free of charge, the necessity for police involvement in order to get a forensic examination which is generally experienced as traumatizing and invasive, and the absence of longer-term follow-up care (Peeters et al., Citation2019). Additionally, as few as 10% of Belgian SA cases are estimated to be reported to the police (Veiligheidsmonitor België Citation2008–2009) and a minority of victims seeks medical care (Roelens, Verstraelen, Van Egmond, & Temmerman, Citation2008). Belgium’s ratification of the Convention of Istanbul in 2016 (Europe Co, Citation2011), obliges its governments to develop appropriate care for victims of SA. A feasibility study (Hendriks et al., Citation2018; Peeters et al., Citation2019; Vandenberghe et al., Citation2018), including a broad consultation of stakeholders, such as victims, health care workers, police officers and prosecutors, generated the development of a model of Sexual Assault Care Centres (SACCs) adapted to the Belgian context. Subsequently, from October 2017 until October 2018, the SACCs were piloted in three cities representative for the main regions in Belgium: Ghent for Flanders, Brussels for the Brussels region and Liège for Wallonia.
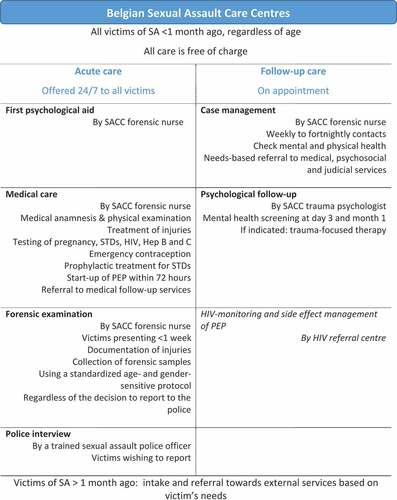
The Belgian SACC-model () is the articulation of a close partnership between hospitals, psycho-social services, the police and the judicial system. The SACC is located in a separate unit in the hospital. All SACC personnel, including forensic nurses, trauma-psychologists and sexual assault police officers, receive a specific SACC-training and abide by Standard Operating Procedures (SOPs). Victims can self-refer regardless of their residence, come accompanied by an officer of the collaborating police zones, or be referred by another professional. SACCs offer both acute and follow-up care to people who were sexually victimized less than a month ago, regardless of age. During the pilot year, the pathways were as follows. At the victim’s presentation to the SACC, first psychological aid, medical care, and a forensic examination are offered by a forensic nurse. Medical care consists of a medical anamnesis, a physical examination, treatment of injuries, testing of STDs, HIV, Hepatitis B and C, the provision of emergency contraception and prophylactic treatment for sexually transmitted diseases (STDs), the start-up of HIV post-exposure prophylaxis (PEP) within 72 h and the referral to medical follow-up services, such as the HIV referral centre for monitoring and side effect management. A forensic examination is offered to all victims presenting within 1 week after the assault, dependent on whether the type of SA warrants such an examination, and regardless of their decision to report to the police. The examination encompasses the documentation of injuries and the collection of forensic samples based on a newly developed standardized patient-centred, age- and gender-sensitive protocol. Specialized physicians (e.g. gynaecologists, emergency physicians) supervise the forensic nurses and assist them when the required care exceeds the SOPs. Victims wishing to report to the police receive a filmed interview by SA police officers at the SACC, who are on call 24 h a day to rejoin the SACC if needed. For victims who do not decide to report, forensic samples are stored for 12 months. These samples can be claimed by the prosecutor in case of the victim’s delayed reporting to the police. Victims under 18 years old receive age-adapted care. A paediatrician always assists during acute care for those below the age of 15, while victims aged 16–17 years do not need a caretaker present to receive care according to Belgian law. The forensic examination of a minor can range from a minimal clinical examination of external lesions to the full array of forensic samples being taken. In case of reporting, victims below the age of 18 undergo an audiovisual interview by trained police officers within a few days upon the acute care, using specific hearing techniques and adapted infrastructure at the police station. After the first presentation to the SACC, case management is started and victims are contacted weekly to fortnightly by phone by the forensic nurse. The forensic nurse inquires about the mental and physical health and refers victims to medical, psychosocial and judicial services when needed. Additionally, a SACC trauma psychologist routinely offers a mental health screening at day 3 and month 1 post the first presentation to the SACC, including a general anamnesis and screening for depression, anxiety, alcohol and drug abuse, and post-traumatic stress disorder (PTSD). All victims and their confidants are offered psycho-education, while active monitoring or trauma-focused cognitive behavioural therapy and EMDR is proposed according to the NICE-guidelines in effect (NICE, Citation2005). Children and adolescents have access to the same package of follow-up care but tailored to their needs.
The SACC is a new model of care for victims of sexual violence in Belgium and so far, no evidence existed on the characteristics of victims and their use of specialized services. Moreover, the Belgian SACCs are unique as a one-stop model in Europe, through its combination of nurse-led acute care and case management, in addition to the offer of long-term psychological follow-up care and the possibility of a police interview at the SACC. Hence, this study intends to broaden the knowledge regarding the set-up of SACs in Europe.
The present study is part of a broader mixed-method evaluation of the acceptability and accessibility of the SACCs. This specific study primarily aims to gain insight in the number and characteristics of victims attending the SACCs, the SA they experienced and the care they received over 12 months upon admission. A secondary aim is to identify differences in characteristics and care needs of adult and minor victims of SA presenting at the SACC. This knowledge will allow further improvement of specialized services for future victims of SA in Belgium and beyond.
2. Methods
2.1. Study sites
The study was conducted in the three SACC pilot sites namely the Ghent University Hospital, the University Hospital Saint Pierre in Brussels, and the Liège University Hospital. The target population of the SACCs was defined as the inhabitants of the collaborating police zone that could refer victims to SACCs, and was estimated at 266,000, 260,000 and 197,000 inhabitants for the police zone Brussels Capital Ixelles, the Ghent and the Liège police zone respectively on 1 January 2018 (Wettelijke bevolking, Citation2018). All sites applied the same SOPs for care, except in SACC Brussels where victims under 16 were referred to the hospital’s specialized child abuse services for follow-up.
2.2. Study participants and data collection
All victims of SA, regardless of age, who attended one of the three SACC sites at least once in person between 25 October 2017 and 31 October 2018, were included in the study. Data were prospectively and routinely collected through the hospital’s electronic patient file by the forensic nurses and the trauma psychologists. Hence, no specific informed consent was obtained. All data collected within 12 months upon the victim’s first presentation to the SACC were included.
2.3. Measurement and definitions
Prior to the start of the SACC pilot, technical working groups consisting of service providers and experts on SA, identified the variables to be included in the electronic patient file, based on their experience and a review of the peer-reviewed literature (Bicanic et al., Citation2014; Mukhtar et al., Citation2018; Zijlstra et al., Citation2017). Items were grouped into victim characteristics, assault characteristics, and service characteristics.
Victim characteristics included age, legal gender (sex assigned at birth, codified as male or female), transgender victim, sexual orientation (for adults only), country of origin, resident status (documented or undocumented), living situation, cognitive/physical disability (as per observation of the forensic nurse) and prior psychiatric consultation.
Assault characteristics included type of sexual violence (sexual harassment defined as any form of unwanted sexual advances or attention, requests for sexual favours or exposure without body contact; physical sexual violence without penetration defined as any unwanted (attempted) threat of physical sexual advances such as touching, pinching, kissing; (attempted) rape defined as the (attempted) penetration of any body part with a sexual organ, or of the anal or genital opening with any body part or object against one’s will), assailant’s gender, number of assailants, victim-assailant relationship and prior SA. Additionally, for victims of rape who presented within 1 week the following was collected: type of penetration, physical violence (light physical violence defined as the victim reporting being bitten, spitted at, immobilized; moderate to severe physical violence defined as the victim reporting being beaten, threatened with weapon or violence against the victim’s throat or neck), and self-reported (voluntary or involuntary) use of alcohol or drugs before or during the assault.
Service characteristics included referral source, SACC site (i.e. SACC where the victim presented for acute care), delay of presentation to SACC, forensic examination (defined as the delivery of a top-to-toe examination looking for injuries and/or taking samples that may be used as evidence in a police investigation and any subsequent prosecution), medical care (defined as the delivery of at least one medical test or treatment at presentation with the aim to improve the victims’ health), reporting to the police (defined as a victim or his/her confidant reporting the SA to the police within 12 months of their first presentation to the SACC), timing of decision to report, case management (defined as a victim having received at least one follow-up phone call from the forensic nurse), median number of case management follow-up contacts, follow-up by trauma psychologist (defined as a victim having received at least one consultation with the SACC psychologist), and median number of contacts with the psychologist. For all victims presenting for rape within 1 week, the following variables were collected: Hepatitis B assessment, Hepatitis C test, HIV test, Chlamydia Trachomatis test, Gonorrhoea test, Syphilis test, pregnancy test, start of HIV Post-Exposure Prophylaxis (for presentations within 72 h only), Hepatitis B vaccine, STD treatment, emergency contraception (for women only), and presence at HIV reference centre within 1 week after admission at SACC (for whom PEP was started only).
2.4. Data analysis
Pseudonymised data were exported from the hospital’s electronic patient files and subsequently merged into a central dataset. Statistical analyses were conducted using SPSS (IBM SPSS Statistics for Windows, Version 25.0). Descriptive statistics were calculated for all victims, as well as separately for minors (aged 0–18 years) and adults (aged 18 years and above), linked to differences in vulnerability and care. Chi-square tests were performed to identify significant associations between age group and victim, assault or service characteristics. The Fisher’s exact test was used in case the Chi-Square test assumptions were not met. Data of victims below the age of 16 from SACC Brussels were excluded from the post-acute care analysis, due to a different follow-up protocol at that study site. SACC attendance rates per 100.000 inhabitants were calculated by dividing the number of admissions per SACC site by the target population of that SACC site.
2.5. Ethical considerations
Ethical approvals were granted by the Medical Ethics Committees of Ghent University Hospital (EC/2017/1011), University Hospital Saint Pierre in Brussels, and Liège University Hospital. The study is compliant with the European General Data Protection Regulation and uses secondary pseudonymised data that was primarily gathered for routine monitoring and evaluation of the SACC services by the SACCs and the Belgian Institute for Equality of Women and Men (IEWM). The legal ground for processing of the data is public interest. Victims were informed of the transfer of their pseudonymised data through the privacy statements of the hospitals.
3. Results
The three SACC sites were attended by 931 victims during the pilot year, of which 49.6% in SACC Brussels, 26.9% in SACC Ghent and 23.5% in SACC Liège. One-third of the victims self-referred to the SACC (35.2%), 40.9% of referrals were facilitated by the police and 18.8% by other professionals.
3.1. Victim characteristics
represents the characteristics of the 931 victims who attended a SACC in one of the three sites during the pilot year. Mean age at admission was 24.5 years (standard deviation = 12.8, median = 22, range = 83), and one-third of the victims were minor. The majority of both minor and adult victims presenting to the SACC were female. Victims showed specific vulnerabilities, that differed for adults and minors: one in five adult victims originated from a country outside the EU, one in ten minor victims lived in foster or residential care like a psychiatric hospital or residential youth services, and one in four adult victims reported a prior consultation with a psychiatrist. Nearly 10% of all victims had a cognitive and/or physical disability.
Table 1. Characteristics of 931 victims by age group attending one of three Belgian SACCs between 25 October 2017 and 31 October 2018
3.2. Assault characteristics
The SA characteristics are shown in . The majority of victims reported rape or attempted rape. The assailant was most often somebody known to the victim, such as an acquaintance, (ex-) partner or family member, and minor victims more often knew their assailant than adult victims. More than one in three victims had previously been exposed to SA, though this was more frequent in adult victims. Of the 447 rape victims presenting within 1 week after the SA (), one-third reported moderate to severe physical violence, and nearly half of the victims had, voluntarily or by force, used alcohol or drugs before or during the assault. However, minors reported fewer incidents of moderate to severe physical violence and alcohol or drug use than adults.
Table 2. Assault characteristics by age group of 931 victims attending one of three Belgian SACCs between 25 October 2017 and 31 October 2018
Table 3. Additional assault characteristics by age for 447 victims presenting for rape within 1 week of the assault at one of three Belgian SACCs between 25 October 2017 and 31 October 2018
3.3. Service characteristics
describes the use of acute care services offered at the SACC. Victims mostly presented at the SACC within 72 h post-assault, although minors tended to present later than adults. Respectively 74.7% of victims received medical care, 60.6% underwent a forensic examination, and 68.7% reported to the police. Minors less often had a forensic examination, but reported more often to the police than adults.
Table 4. Characteristics of acute care by age group for 931 victims attending one of three Belgian SACCs between 25 October 2017 and 31 October 2018
presents the medical acute and follow-up care offered to the 447 victims who presented for rape within a week at the SACC. The big majority of victims received necessary testing of STIs and blood-borne viruses, and post-exposure prophylactic treatment, though minors less than adults. One in five victims were vaccinated for Hepatitis B. More than half of female victims underwent a pregnancy test and one-third received emergency contraception. Four in five victims who started HIV post-exposure prophylaxis were present at the HIV reference centre for follow-up.
Table 5. Medical acute and follow-up care characteristics for 447 victims presenting for rape within 1 week at one of three Belgian SACCs between 25 October 2017 and 31 October 2018
Findings on follow-up care of victims are presented in . More than 90% of victims accepted the case management and half of the victims attended at least one consultation with the trauma psychologist, with a median of 2 contacts. No differences were observed among age groups.
Table 6. Characteristics of follow-up care by age group for 849 victims attending one of three Belgian SACCs between 25 October 2017 and 31 October 2018 (victims below 16 years of SACC Brussels excluded)
4. Discussion
The present study shows that Belgian Sexual Assault Care Centres were attended by 931 victims within the first year, of which one-third were minors. Despite limited promotion of the SACCs, the three pilot SACCs instantly received a high number of victims. While referral to the SACCs was guaranteed due to a close collaboration with specific police zones referring 41% of the victims, it is remarkable that more than one-third of victims self-referred to the SACC. The existence of specialized services in combination with an improved collaboration with the police, may actually lead to a higher utilization of services as has been suggested in previous research (Campbell et al., Citation2005; Greeson & Campbell, Citation2013; Nesvold et al., Citation2005). This hypothesis is supported by the fact that hospitals estimate a two- to threefold increase in attendance of SA victims since the establishment of the SACC, although this needs confirmation through a pre/post analysis. Other assumptions are that SA became less of a taboo in Belgium given unexpected events during the pilot year, such as the MeToo campaign, which may have unintentionally promoted the existence of the SACCs through Belgian media. However, accurate prevalence data regarding sexual victimization in Belgium are needed, in order to evaluate if SACCs are successful in reaching victims of acute SA in need of care.
The majority of victims attending the Belgian SACCs were young women. Yet, also 9% of the victims were male and 1% identified as transgender. Vulnerability of victims attending the Belgian SACCs was high: more than one-third of victims had a history of at least one psychiatric consultation, one-third had experienced prior SA, one in ten victims had a cognitive or physical disability, and 20% of victims originated from outside the EU. Minors more often lived in residential or foster care, and less frequently had a psychiatric consultation than adults. These findings are confirmed by other European SAC studies reporting similar high vulnerability rates among victims (Bicanic et al., Citation2014; Brooker & Durmaz, Citation2015; Creighton & Jones, Citation2012; Majeed‐Ariss et al., Citation2020; Manning et al., Citation2019; Nesvold et al., Citation2008; Vik et al., Citation2019; Zijlstra et al., Citation2017). As in other European countries, the Belgian SACCs will equally need to monitor and adapt care pathways for these vulnerable victims with specific needs.
Victims mainly presented for rape by a known assailant. These assault characteristics are similar to the typology in other European SACs, although the findings on reported physical violence and assault by a stranger are hard to compare due to differences in definitions used (Bicanic et al., Citation2014; Hagemann et al., Citation2013; Ingemann-Hansen et al., Citation2009; Kerr et al., Citation2003; Larsen et al., Citation2015; Nesvold et al., Citation2008; Vik et al., Citation2019; Zijlstra et al., Citation2017). Nearly half of the victims reported voluntary or involuntary alcohol or drug intake before or during the assault, and moderate to severe physical violence was reported in one-third of the cases, though this was observed less in minors than in adults. This could be explained by the fact that assailants of minors were more frequently known to the victim, whereby the SA often takes place in a context of psychological, emotional or material manipulation (WHO, Citation2017b).
The majority of victims reported within 72 h post-assault to the SACC. Minors generally presented later, what is possibly related to the fact that children often do not disclose spontaneously or only at a later stage (Vrolijk-Bosschaart et al., Citation2018) and mostly need the support of an adult to seek formal help. We observed a high use of services at the Belgian SACCs, which confirms the need for comprehensive care for victims of SA and thus the appropriateness of the SACC model.
Uptake of acute care services was high: 61% of victims agreed to a forensic examination and 75% received medical care. These observations are again very similar to other European SACs (Campbell et al., Citation2014, Citation2005; Eogan et al., Citation2013; Greeson & Campbell, Citation2013; WHO, Citation2017b; Zijlstra et al., Citation2017). Notably, only 60% of female rape victims underwent a pregnancy test and one-third received emergency contraception, possibly because these women were on secure contraception, refused emergency contraception, or did not experience vaginal penetration. Additionally, only a quarter of rape victims received a Hepatitis B vaccine, what may be due to prior vaccination, immunity or refusal. Minors less often underwent a forensic examination than adults, what can be predominantly explained by their delayed presentation to the SACC but also to the precautious measures not to expose children to invasive forensic examinations if not well indicated. Minors less frequently received medical tests nor received STI treatment, what may be related to less frequent vaginal penetration, more chronic sexual abuse by a known assailant, and higher Hepatitis B vaccination coverage within this age group. However, these assumptions need confirmation by a follow-up study looking into medical outcomes.
Uptake of follow-up services such as medical follow-up appointments, case management and psychological consultations was variable. Firstly, attendance to medical follow-up appointments at the HIV reference centre was high with 80% of victims on HIV-post exposure prophylaxis reporting for their appointment. This is higher than what was observed in SACs in Norway or the UK, where only 46% to 55% of victims attended for medical follow-up (Kerr et al., Citation2003; Nesvold et al., Citation2008). Secondly, victims’ acceptance of case management was 90% and similar to what was observed in the Netherlands (Bicanic et al., Citation2014; Zijlstra et al., Citation2017). Thirdly, only half of the victims consulted the psychologist, with a median of two contacts. This suggests that few victims engage in a longer trauma-focused therapy, despite the fact that victims expressed a clear need for such free support during the Belgian SACC feasibility study (Peeters et al., Citation2019). There are several hypotheses that may explain this low uptake of psychological support services. Firstly, victims may not yet want to engage in trauma-oriented therapy in the immediate aftermath of the assault, what could be a sign of avoidance which is commonly observed in victims suffering from PTSD after SA (NICE, Citation2018). A second hypothesis is that an important proportion of victims with pre-existing mental health issues are already being treated by a psychologist or psychiatrist. Lastly, the distance to the SACC and the limited working hours of its psychologists may pose a barrier to attend for follow-up care. As such, alternative ways to offer psychological support should be tested in order to increase the proportion of victims receiving appropriate support. Following strategies could be considered: SACC-antennas for psychological support closer to victims’ location with active outreach, an increased availability of and referral to external trauma psychologists within short distance from the victim’s home, improved referral for specialized care regarding other comorbidities such as substance use or depression, and the embedment of psychological support in blended help through internet or mobile-based interventions (Ebert, Harrer, Apolinario-Hagen, & Baumeister, Citation2019).
As part of the comprehensive support, SACCs also liaise with the police and the legal system. Nearly 70% of victims reported to the police, what is similar to observations in Nordic assault centres with 50% to 70% of victims reporting the SA (Larsen et al., Citation2015; Nesvold et al., Citation2008). This high reporting in Belgian SACCs stands in sharp contrast to the national reporting rates for SA which are estimated to be as low as 10% (Veiligheidsmonitor België Citation2008–2009). As the police are the primary source for referrals to the SACC and most SACC cases are acute, implying an increased probability of successful prosecution, a high reporting rate is thus to be expected. However, the SACCs can also remove barriers to file a complaint by discussing the advantages and disadvantages of reporting to the police at first admission and during follow-up, through the possibility of an interview by a trained sexual assault police officer at the SACC and by performing a forensic examination regardless of the victim’s decision to report to the police. Hence, the implementation of SACCs may contribute to an increased proportion of victims reporting SA, although this can only be confirmed by a longitudinal study of sexual victimization reporting rates at the police before and after the implementation of SACCs. Whether the SACCs also have an impact on the prosecution of SA cases in Belgium, as suggested in research from the United States (Campbell et al., Citation2014, Citation2012), should be further investigated.
There are several limitations to this study. First, this study used data that were routinely collected in the SACC during the pilot year. However, the SACC data collection system was also subject to testing during that same period. Several shortcomings in the data collection system were thus identified such as reporting difficulties for victims with a black-out, the ill-definition of date rape assailants as well as cognitive disability, and the lack of identification of victims attending the SACC multiple times due to sexual revictimization. Necessary adaptations in the registration system are ongoing. Secondly, the study was limited to the information that was available to the SACC personnel. Especially data on the medical follow-up care offered by other health care providers, longer-term health outcomes, and information on the judicial follow-up was often not known to the SACC personnel. A prospective longitudinal study taking these components into account would allow further documentation of the impact of SACC on both an individual and societal level. Thirdly, this quantitative study does not shed light on what makes the SACC services appropriate for its users. Explanatory qualitative research is ongoing to understand these mechanisms of action of the SACC.
Despite these study limitations, this is however the first study of a large cohort of victims attending comprehensive SA care services in Belgium with a one-year follow-up period, considering a myriad of factors related to the victim, the SA and the care pathways.
In conclusion, this study allowed to gain a better understanding of the population using the SACCs and the care offered. The high attendance of victims of SA together with a good uptake of the services, encouraged a rapid national scale-up of the model in Belgium. In complement with exploratory qualitative research, this study facilitated adaptations to the SACC model such as the improvement of the training of personnel, the revision of certain SACC procedures and the definition of targeted service-promotion strategies.
Acknowledgments
We would like to thank all SACC personnel and their coordinators for rigorously collecting or supporting the collection of the data and assisting victims of sexual assault on a daily basis, the students for assisting in the data-analysis, the Belgian Institute for the Equality of Women and Men and the Belgian Secretary of State of Equality for funding the piloting of the SACCs and its scientific evaluation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The research complies with the European General Data Protection Regulation and the data set can as such not be made publicly available.
Additional information
Funding
References
- Abrahams, N., Devries, K., Watts, C., Pallitto, C., Petzold, M., Shamu, S., & García-Moreno, C. (2014). Worldwide prevalence of non-partner sexual violence: A systematic review. The Lancet, 383(9929), 1648–12. doi:10.1016/S0140-6736(13)62243-6
- Bicanic, I., Snetselaar, H., & De Jongh, A., Van de Putte E. (2014). Victims’ use of professional services in a Dutch sexual assault centre. European Journal of Psychotraumatology, 5, 1. doi:10.3402/ejpt.v5.23645
- Brooker, C., & Durmaz, E. (2015). Mental health, sexual violence and the work of sexual assault referral centres (SARCs) in England. Journal of Forensic and Legal Medicine, 31, 47–51. doi:10.1016/j.jflm.2015.01.006
- Brooker, C., Tocque, K., & Paul, S. (2018). Assessment of the mental health status of a one year cohort attending a two sexual assault referral centres in England. Journal of Forensic and Legal Medicine, 54, 44–49. doi:10.1016/j.jflm.2017.12.018
- Buysse, A., Enzlin, P., Lievens, J., T’sjoen, G., Van Houtte, M., & Vermeersch, H. (2013). Sexpert: Basisgegevens van de survey naar seksuele gezondheid in Vlaanderen. Ghent: Academia Press.
- Campbell R. (2008). The psychological impact of rape victims’ experiences with the legal, medical, and mental health systems. American Psychologist, 63(8), 702–717.
- Campbell, R., Bybee, D., Townsend, S. M., Shaw, J., Karim, N., & Markowitz, J. (2014). The impact of sexual assault nurse examiner programs on criminal justice case outcomes: A multisite replication study. Violence against Women, 20(5), 607–625. doi:10.1177/1077801214536286
- Campbell, R., Patterson, D., & Bybee, D. (2012). Prosecution of adult sexual assault cases: A longitudinal analysis of the impact of a sexual assault nurse examiner program. Violence against Women, 18(2), 223–244. doi:10.1177/1077801212440158
- Campbell, R., Patterson, D., & Lichty, L. F. (2005). The effectiveness of sexual assault nurse examiner (SANE) programs: A review of psychological, medical, legal, and community outcomes. Trauma, Violence, & Abuse, 6(4), 313–329. doi:10.1177/1524838005280328
- CDC. (2015). Sexual assault and abuse and STD’s. Author. https://www.cdc.gov/std/tg2015/sexual-assault.htm
- Creighton, C. D., & Jones, A. C. (2012). Psychological profiles of adult sexual assault victims. Journal of Forensic and Legal Medicine, 19(1), 35–39. doi:10.1016/j.jflm.2011.10.007
- De Schrijver, L., Vander Beken, T., Krahe, B., & Keygnaert, I. (2018). Prevalence of sexual violence in migrants, applicants for international protection, and refugees in Europe: A critical interpretive synthesis of the evidence. International Journal of Environmental Research and Public Health, 15(9), 9. doi:10.3390/ijerph15091979
- Dworkin, E. R., Menon, S. V., Bystrynski, J., & Allen, N. E. (2017). Sexual assault victimization and psychopathology: A review and meta-analysis. Clinical Psychology Review, 56, 65–81. doi:10.1016/j.cpr.2017.06.002
- Ebert, D. D., Harrer, M., Apolinario-Hagen, J., & Baumeister, H. (2019). Digital interventions for mental disorders: Key features, efficacy, and potential for artificial intelligence applications. Advances in Experimental Medicine and Biology, 1192, 583–627.
- Eogan, M., McHugh, A., & Holohan, M. (2013). The role of the sexual assault centre. Best Practice & Research Clinical Obstetrics & Gynaecology, 27(1), 47–58. doi:10.1016/j.bpobgyn.2012.08.010
- Etude des opinions et des comportements de la population belge en matière de violences sexuelles. (2019). Brussels, Belgium: Amnesty International Belgium, SOS Viol.
- European Union lesbian, gay, bisexual and transgender survey: Results at a glance. (2013). Luxemburg: Publication Office of the European Union: European Union Agency for Fundamental Rights.
- Europe Co. (2011). Council of Europe convention on preventing and combating violence against women and domestic violence. Istanbul: Council of Europe.
- Finkelhor, D., Shattuck, A., Turner, H. A., & Hamby, S. L. (2014). The lifetime prevalence of child sexual abuse and sexual assault assessed in late adolescence. Journal of Adolescent Health, 55(3), 329–333. doi:10.1016/j.jadohealth.2013.12.026
- García-Moreno, C., Pallitto, C., Devries, K., Stöckl, H., Watts, C., & Abrahams, N. (2013). Global and regional estimates of violence against women: Prevalence and health effects of partner violence and sexual non-partner violence. Geneva: World Health Organization.
- Garcia-Moreno, C., Hegarty, K., d’Oliveira, A. F., Koziol-McLain, J., Colombini, M., & Feder, G. (2015). The health-systems response to violence against women. The Lancet, 385(9977), 1567–1579. doi:10.1016/S0140-6736(14)61837-7
- Gilles, C., Manigart, Y., Rousseau, C., Libois, A., Gennotte, A. F., & Rozenberg, S. (2019). Implementation of a protocol and staff educational sessions improves the care of survivors of sexual assault. Maturitas, 124, 39–42. doi:10.1016/j.maturitas.2019.03.004
- Gilles, C., Van Loo, C., & Rozenberg, S. (2010). Audit on the management of complainants of sexual assault at an emergency department. European Journal of Obstetrics & Gynecology and Reproductive Biology, 151(2), 185–189. doi:10.1016/j.ejogrb.2010.03.014
- Greeson, M. R., & Campbell, R. (2013). Sexual assault response teams (SARTs): An empirical review of their effectiveness and challenges to successful implementation. Trauma, Violence, & Abuse, 14(2), 83–95. doi:10.1177/1524838012470035
- Hagemann, C. T., Helland, A., Spigset, O., Espnes, K. A., Ormstad, K., & Schei, B. (2013). Ethanol and drug findings in women consulting a sexual assault center – Associations with clinical characteristics and suspicions of drug-facilitated sexual assault. Journal of Forensic and Legal Medicine, 20(6), 777–784. doi:10.1016/j.jflm.2013.05.005
- Hendriks, B., Vandenberghe, A. M. J. A., Peeters, L., Roelens, K., & Keygnaert, I. (2018). Towards a more integrated and gender-sensitive care delivery for victims of sexual assault: Key findings and recommendations from the Belgian sexual assault care centre feasibility study. International Journal for Equity in Health, 17(1), 152. doi:10.1186/s12939-018-0864-3
- Ingemann-Hansen, O., Sabroe, S., Brink, O., Knudsen, M., & Charles, A. V. (2009). Characteristics of victims and assaults of sexual violence – Improving inquiries and prevention. Journal of Forensic and Legal Medicine, 16(4), 182–188. doi:10.1016/j.jflm.2008.07.004
- Jina, R., & Thomas, L. S. (2013). Health consequences of sexual violence against women. Best Practice & Research Clinical Obstetrics & Gynaecology, 27(1), 15–26. doi:10.1016/j.bpobgyn.2012.08.012
- Kerr, E., Cottee, C., Chowdhury, R., Jawad, R., & Welch, J. (2003). The haven: A pilot referral centre in London for cases of serious sexual assault. BJOG: An International Journal of Obstetrics and Gynaecology, 110(3), 267–271. doi:10.1046/j.1471-0528.2003.02233.x
- Keygnaert, I., Vandeviver, C., Nisen, L., De Schrijver, L., Depraetere, J., Nobels, A., Cismaru Inescu, A., Lemonne, A., Renard, B., & Vander Beken, T. (2018). Seksueel geweld in België: Eerste representatieve prevalentiestudie naar de aard, omvang en impact van seksueel geweld in België (pp. 28–31). Science Connection (Nederlandse Ed). Brussels: Belspo.
- Khadr, S., Clarke, V., Wellings, K., Villalta, L., Goddard, A., Welch, J., … Viner, R. (2018). Mental and sexual health outcomes following sexual assault in adolescents: A prospective cohort study. The Lancet Child & Adolescent Health, 2(9), 654–665. doi:10.1016/S2352-4642(18)30202-5
- Krahe, B., Berger, A., Vanwesenbeeck, I., Bianchi, G., Chliaoutakis, J., Fernandez-Fuertes, A. A., … Zygadło, A. (2015). Prevalence and correlates of young people’s sexual aggression perpetration and victimisation in 10 European countries: A multi-level analysis. Culture, Health & Sexuality, 17(6), 682–699. doi:10.1080/13691058.2014.989265
- Larsen, M.-L., Hilden, M., & Lidegaard, O. (2015). Sexual assault: A descriptive study of 2500 female victims over a 10-year period. BJOG: An International Journal of Obstetrics & Gynaecology, 122(4), 577–584. doi:10.1111/1471-0528.13093
- Linden, J. A. (2011). Clinical practice. Care of the adult patient after sexual assault. New England Journal of Medicine, 365(9), 834–841. doi:10.1056/NEJMcp1102869
- Majeed‐Ariss, R., Rodriguez, P. M., & White, C. (2020). The disproportionately high prevalence of learning disabilities amongst adults attending Saint Marys sexual assault referral centre. Journal of Applied Research in Intellectual Disabilities, 33(3), 595–603. doi:10.1111/jar.12703
- Manning, D., Majeed-Ariss, R., Mattison, M., & White, C. (2019). The high prevalence of pre-existing mental health complaints in clients attending Saint Mary’s sexual assault referral centre: implications for initial management and engagement with the independent sexual violence advisor service at the centre. Journal of Forensic and Legal Medicine, 61, 102–107. doi:10.1016/j.jflm.2018.12.001
- Mukhtar, S. A., Smith, D. A., Phillips, M. A., Kelly, M. C., Zilkens, R. R., & Semmens, J. B. (2018). Capturing sexual assault data: An information system designed by forensic clinicians and healthcare researchers. Health information Management: Journal of the Health Information Management Association of Australia, 47(1), 46–55. doi:10.1177/1833358316687575
- Nesvold, H., Friis, S., & Ormstad, K. (2008). Sexual assault centers: Attendance rates, and differences between early and late presenting cases. Acta Obstetricia et Gynecologica Scandinavica, 87(7), 707–715. doi:10.1080/00016340802189847
- Nesvold, H., Worm, A.-M., Vala, U., & Agnarsdottir, G. (2005). Different Nordic facilities for victims of sexual assault: A comparative study. Acta Obstetricia et Gynecologica Scandinavica, 84(2), 177–183. doi:10.1111/j.0001-6349.2005.00641.x
- National Collaborating Centre for Mental Health (UK). (2005). Post-traumatic stress disorder (PTSD): The management of PTSD in adults and children in primary and secondary care. Gaskell: National Institute of Health and Care Excellence.
- NICE. (2018). Post-traumatic stress disorder: NICE guideline. London: National Institute of Health and Care Excellence.
- Peeters, L., Vandenberghe, A., Hendriks, B., Gilles, C., Roelens, K., & Keygnaert, I. (2019). Current care for victims of sexual violence and future sexual assault care centres in Belgium: The perspective of victims. BMC International Health and Human Rights, 19(1), 21. doi:10.1186/s12914-019-0207-5
- Perilloux, C., Duntley, J. D., & Buss, D. M. (2012). The costs of rape. Archives of Sexual Behavior, 41(5), 1099–1106. doi:10.1007/s10508-011-9863-9
- Rees, S., Silove, D., Chey, T., Ivancic, L., Steel, Z., Creamer, M., … Forbes, D. (2011). Lifetime prevalence of gender-based violence in women and the relationship with mental disorders and psychosocial function. JAMA, 306(5), 513–521. doi:10.1001/jama.2011.1098
- Roelens, K., Verstraelen, H., Van Egmond, K., & Temmerman, M. (2008). Disclosure and health-seeking behaviour following intimate partner violence before and during pregnancy in Flanders, Belgium: A survey surveillance study. European Journal of Obstetrics & Gynecology and Reproductive Biology, 137(1), 37–42. doi:10.1016/j.ejogrb.2007.04.013
- Santaularia, J., Johnson, M., Hart, L., Haskett, L., Welsh, E., & Faseru, B. (2014). Relationships between sexual violence and chronic disease: A cross-sectional study. BMC Public Health, 14(1), 1286. doi:10.1186/1471-2458-14-1286
- Sena, A. C., Hsu, K. K., Kellogg, N., Girardet, R., Christian, C. W., Linden, J., & Hammerschlag, M. R. (2015). Sexual assault and sexually transmitted infections in adults, adolescents, and children. Clinical Infectious Diseases, 61(Suppl 8), S856–64. doi:10.1093/cid/civ786
- Tiihonen Moller, A., Backstrom, T., Sondergaard, H. P., Helstrom, L., & Dalal, K. (2014). Identifying risk factors for PTSD in women seeking medical help after rape. PLoS One, 9(10), e111136. doi:10.1371/journal.pone.0111136
- Vandenberghe, A., Hendriks, B., Peeters, L., Roelens, K., & Keygnaert, I. (2018). Establishing sexual assault care centres in Belgium: Health professionals’ role in the patient-centred care for victims of sexual violence. BMC Health Services Research, 18(1), 807. doi:10.1186/s12913-018-3608-6
- Veiligheidsmonitor België 2008–2009. Federale Politie Directie Operationele Informatie/Politiebeleidsondersteuning Dienst Beleidsgegevens. Brussels.
- Vik, B. F., Nottestad, J. A., Schei, B., Rasmussen, K., & Hagemann, C. T. (2019). Psychosocial vulnerability among patients contacting a Norwegian sexual assault center. Journal of Interpersonal Violence, 34(10), 2138–2157. doi:10.1177/0886260516659657
- Vrolijk-Bosschaart, T. F., Brilleslijper-Kater, S. N., Benninga, M. A., Lindauer, R. J. L., & Teeuw, A. H. (2018). Clinical practice: Recognizing child sexual abuse—what makes it so difficult? European Journal of Pediatrics, 177(9), 1343–1350. doi:10.1007/s00431-018-3193-z
- Wettelijke bevolking. (2018). Wettelijke bevolking per gemeente op 1 januari 2018: Statbel. Retrieved from https://statbel.fgov.be/nl/themas/bevolking/structuur-van-de-bevolking#panel-12
- WHO. (2004). Clinical management of rape survivors: Developing protocols for use with refugees and internally displaced persons. Geneva: Author.
- WHO. (2015). Strengthening the medico-legal response to sexual violence. Geneva: World Health Organization.
- WHO. (2017a). Strengthening health systems to respond to women subjected to intimate partner violence or sexual violence: A manual for health managers. Geneva: World Health Organization.
- WHO. (2017b). Responding to children and adolescents who have been sexually abused: WHO clinical guidelines. Geneva: World Health Organization.
- Zijlstra, E., Esselink, G., Moors, M. L., LoFoWong, S., Hutschemaekers, G., & Lagro-Janssen, A. (2017). Vulnerability and revictimization: Victim characteristics in a Dutch assault center. Journal of Forensic and Legal Medicine, 52, 199–207. doi:10.1016/j.jflm.2017.08.003