ABSTRACT
Background: Moral injury (MI) describes emotional, spiritual, and social suffering that can arise following psychological trauma. Prior research in military populations indicates the relevance of MI to adverse psychological outcomes, such as post-traumatic stress disorder (PTSD) and suicidal behaviours, and shows evidence for MI as a unique construct. Minimal studies of MI have been implemented in civilians, usually restricted to small samples with a specific set of traumatic experiences, despite the conceptual relevance of MI to non-military trauma reactions more broadly (e.g. feelings of betrayal towards a perpetrator of sexual abuse).
Objective: To address this problem, we assessed MI in trauma-exposed civilians to examine ways in which this construct was related to and distinct from trauma and traumatic stress-related problems, including PTSD and depression.
Method: We adapted an existing MI scale, Moral Injury Events Scale (MIES) and administered this measure to 81 men and women along with measures of trauma exposure, PTSD and depression, and also asked participants about past suicide attempts.
Results: We observed that both greater exposure and distress related to potentially morally injurious events were associated with higher trauma exposure, particularly childhood maltreatment, as well as post-traumatic and depressive psychopathology. However, even after accounting for current PTSD and depression symptoms, MI exposure (F = 6.05, p = .017) was significantly higher among participants who had previously attempted suicide.
Conclusions: These pilot data reveal the ways in which MI is associated with trauma exposure, PTSD and depression and highlight the salience of MI in civilians. Similarly, these data demonstrate the unique relevance of MI to suicide behaviours, independent of post-traumatic psychopathology, indicating that this construct may be an understudied contributor to suicide risk in civilians.
HIGHLIGHTS
Moral injury (MI) describes emotional, spiritual, and social suffering emerging after psychological trauma.
Despite conceptual relevance to civilian trauma, it has been largely assessed in military populations.
We assessed MI in a sample of high trauma-exposed civilians, finding associations with interpersonal trauma, PTSD, and depression, as well as past suicide attempt.
Antecedentes: El daño moral (DM) describe el sufrimiento emocional, espiritual y social que puede surgir después de un trauma psicológico. Investigaciones previas en poblaciones militares indican la relevancia del DM para los desenlaces psicológicos adversos, como trastorno de estrés postraumático (TEPT) y las conductas suicidas, y muestran evidencia de que el DM es un constructo único. Se han implementado mínimos estudios de DM en civiles, usualmente restringidos a pequeñas muestras con un conjunto específico de experiencias traumáticas, a pesar de la relevancia conceptual de DM para las reacciones de trauma no militares más amplias (p.Ej., Sentimientos de traición hacia un perpetrador de abuso sexual).
Objetivo: Para abordar este problema, evaluamos el DM en civiles expuestos a trauma para examinar las formas en que este constructo se relacionaba y se diferenciaba de los problemas relacionados con el trauma y el estrés traumático, incluidos el trastorno de estrés postraumático y la depresión.
Método: Adaptamos una escala de DM existente, la Escala de eventos de daños morales y administramos esta medida a 81 hombres y mujeres junto con medidas de exposición al trauma, TEPT y depresión, y también preguntamos a los participantes sobre intentos suicidas pasados.
Resultados: Observamos que tanto una exposición mayor como la angustia relacionada con eventos de potencial daño moral se asociaron con mayor exposición a trauma, particularmente al maltrato infantil, así como a psicopatología postraumática y depresiva. Sin embargo, incluso después de tener en cuenta los síntomasde TEPT actuales y depresión, la exposición a DM (F = 6.05, p = .017) fue significativamente mayor entre los participantes que habían intentado suicidio previamente.
Conclusiones: Estos datos piloto revelan las formas en que el DM se asocia con la exposición al trauma, TEPT y depresión y resaltan la importancia del DM en la población civil. De manera similar, estos datos demuestran la relevancia única del DM para los comportamientos suicidas, independientemente de la psicopatología postraumática, lo que indica que este constructo puede ser un contribuyente subestudiado del riesgo de suicidio en la población civil.
背景: 道德伤害 (MI) 描述了心理创伤后可能出现的情绪, 精神和社会痛苦。先前对军人群体的研究表明 MI 与不良心理结果的相关性, 例如创伤后应激障碍 (PTSD) 和自杀行为, 并表现出MI 作为一种独特构念的证据。尽管 MI 与非军事创伤反应的概念相关性更广泛 (例如, 对性虐待犯罪者的背叛感), 在平民中对 MI 的少量研究通常仅限于具有一组特定创伤经历的小样本。
目的: 为解决这个问题, 我们评估了创伤暴露平民中的 MI, 以考查此构念与创伤和包括 PTSD 和抑郁的创伤应激相关问题相关和不同的方式。
方法: 我们采用了现有的 MI 量表——道德伤害事件量表, 对 81 名男性和女性进行了这项测量, 同时测量了创伤暴露, PTSD 和抑郁, 还询问了参与者过去的自杀尝试。
结果: 我们观察到, 更多与潜在道德伤害事件相关的暴露和痛苦都与更高的创伤暴露有关, 尤其是童年期虐待, 以及创伤后和抑郁的精神疾病。然而, 即使考虑到当前的 PTSD 和抑郁症状, 在之前曾试图自杀的参与者中, MI 暴露 (F = 6.05, p= .017) 也显著更高。
结论: 这些试点数据揭示了 MI 与创伤暴露, PTSD 和抑郁相关的方式, 并强调了平民中MI的突出性。同样, 这些数据证明了 MI 与自杀行为独立于创伤后精神疾病的独特相关性, 表明此构念可能是导致平民自杀风险的一个未充分研究的因素。
1. Introduction
Moral injury (MI) is an emerging construct capturing the emotional, social, and spiritual suffering that can arise following events that violate deeply held moral beliefs and values. Litz et al. (Citation2009) defined MI as “disruption in an individual’s confidence and expectations about one’s own or others’ motivation to behave in a just and ethical manner … brought about by perpetrating, failing to prevent, bearing witness to, or learning about acts that transgress deeply held moral beliefs and expectations’ (Litz et al., Citation2009) Assuming a more macro-level view, Shay (Citation1994) earlier highlighted the painful consequences of potentially morally injurious events (PMIEs) that entail a betrayal of trust from authority figures in high-stakes situations (Shay, Citation1994). Although researchers and clinicians have not reached a consensus on the essential features of a morally injured state, there is agreement about distinguishing between exposure to these two continua of PMIEs (i.e. perpetration- and betrayal-based events) and distress symptomatology that may emerge afterwards (Griffin et al., Citation2019).
A growing research base has affirmed the utility of the moral injury (MI) construct for working with traumatized patients. Drawing on Nash et al.’s (Citation2013) Moral Injury Events Scale (MIES; Nash et al., Citation2013), large-scale studies with returning veterans documented exposure rates of roughly one-quarter for both perpetration- and betrayal-based events (e.g. Wisco et al., Citation2017). Other work has found that exposure to PMIEs was uniquely associated with risk for post-traumatic stress disorder (PTSD), major depressive disorder, and suicidal behaviour (for a review, see Griffin et al., Citation2019). When considering the diverse types of traumas that might lead veterans to seek PTSD treatment, Litz et al. (Citation2018) found PMIEs are often reported as most distressing and linked with more complexity in posttraumatic symptoms (Litz et al., Citation2018). Focusing on MIES scores in 26 post-9/11 veterans seeking care at a US. Veterans Affairs (VA) medical centre, neuroimaging findings (spontaneous resting-state brain fluctuations and functional connectivity) revealed dissociable neural underpinnings and behaviourally distinct components of morally injurious events and PTSD symptomatology (Sun et al., Citation2018). Notably, extant MI measures assess either exposure to morally injurious events or related symptoms, with a couple exceptions. Similar to Nash et al. (Citation2013), Braitman et al. (Citation2018) assessed both exposure and distress in a military sample with the Moral Injury Questionnaire (MIQ); using an exploratory factor analysis, they found that PMIE exposure, psychological consequences of MI/MI distress and betrayal emerged as factors (Braitman et al., Citation2018).
Despite these and other findings, the utility of the MI construct has rarely been examined outside military populations. Some exceptions include studies with refugees that indicated high rates of exposure to PMIEs that were associated with high severity of mental health symptomatology (Hoffman, Liddell, Bryant, & Nickerson, Citation2019; Nickerson et al., Citation2015). Studies with teachers in El Salvador (Currier, Holland, Rojas-Flores, Herrera, & Foy, Citation2015) showed MI was linked with PTSD symptoms and burnout. Studies of journalists in the context of covering the refugee crisis show relationships between MI and guilt (Feinstein, Pavisian, & Storm, Citation2018). A recent study (Chaplo, Kerig, & Wainryb, Citation2019); tested the psychometric properties of a civilian MI measure for youths, with items derived in part from existing MI assessments (e.g. C. J. Bryan et al., Citation2016; Nash et al., Citation2013); trauma was not assessed, but the authors assessed relationships between the measure subscales with PTSD and depression symptoms. The authors reported a five-factor latent structure for this measure: Acts of commission with agency or under duress, acts of omission, witnessing MI events and betrayal-related factors. Notably, acts of commission with agency and betrayal were associated with depression, whereas only betrayal was associated with PTSD. These studies reveal the relevance of civilian MI to trauma and stress-related disorders, while also highlighting the fact that substantially more research is needed to assess MI in non-military populations and understand its relationship with other trauma-related sequelae.
Similarly, the mental health impact of MI, including exposure to PMIEs and related distress, has not been studied among civilians who have experienced multiple types of trauma exposure. When considering the moral wrongdoing and/or possible betrayal of human-perpetrated events with chronic and repeated exposures to trauma in particular (e.g. domestic violence, child abuse and rape), MI might complicate the clinical picture and contribute to adverse mental health outcomes, including suicide-related behaviours. A growing amount of research suggests the contributions of MI in suicide risk (Ames et al., Citation2019; A. O. Bryan, Bryan, Morrow, Etienne, & Ray-Sannerud, Citation2014; C. J. Bryan, Bryan, Roberge, Leifker, & Rozek, Citation2018; Kelley et al., Citation2019; Wisco et al., Citation2017; Yan, Citation2016), with some data suggesting that MI-related distress has phenomenological qualities distinct from PTSD (e.g. loss of purpose/meaning, sense of betrayal, difficulty forgiving self or others) that uniquely contribute to suicide risk.
Despite the clear need for understanding the role of MI in non-veteran populations, few studies have assessed both MI exposure and related distress in civilians; further, there is a lack of research examining specific associations between exposure to PMIEs and related distress with types of trauma exposure and trauma-related psychopathology. Thus, in this pilot study, we adapted the MIES (Nash et al., Citation2013) for a civilian population, making items applicable to civilian trauma, and administered it to a trauma-exposed civilian population as part of one of the largest and longest-running studies of trauma in the United States, the Grady Trauma Project (GTP). Although trauma exposure was not a criterion for participation in GTP, trauma history was extensively assessed; prior data suggests that nearly all participants in this population have experienced at least one type of trauma (Gillespie et al., Citation2009). Our first objective was to pilot the adapted measure of MI with this population, examining extent of participants’ exposure to morally injurious events, which included acts of omission and commission by the self or other, acts of betrayal, and whether these events caused distress (i.e. feeling troubled by morally injurious acts of omission or commission or betrayal). We assessed whether these responses were related to a traumatic event, as defined by PTSD diagnostic criteria in the DSM-5, or if they were more applicable to other types of events, giving participants the opportunity to write in their responses. Further, we examined associations of MI exposure and distress with frequency of exposure to different types of trauma, including childhood maltreatment and adult trauma. Finally, we assessed relationships of MI exposure and distress with severity of depression, PTSD, and past suicide attempt. We present pilot data on a sample of participants enrolled in this project, a majority of whom were seeking medical treatment, and some of whom were seeking treatment for PTSD.
2. Methods
2.1. Participants
Eighty-three total participants were recruited for this study from an ongoing study of trauma and PTSD (GTP), and 25 GTP participants also completed a mindfulness intervention study for trauma-exposed individuals with PTSD symptoms (NCT02754557). As part of the GTP, participants are approached in the general medical clinics (obstetrics/gynaecology, diabetes and internal medicine) of a publicly funded hospital serving low-income individuals in inner-city Atlanta, Georgia, U.S.A; some participants for the intervention study were recruited via community advertisements. The total sample predominantly self-reported as female (90.4%; one person did not report their sex or gender) and was aged 18–65 (M = 40.1, SD = 12.9). The self-identified racial and ethnic breakdown of participants was as follows: 77.1% African American, 1.2% Hispanic/Latino, 2.4% Asian, 12% Caucasian, 4.8% mixed, and 2.4% other. Other demographic and clinical characteristics, including trauma exposure frequency by type, are provided in ).
Table 1(a). Demographics (N = 83)
Table 1(b). Clinical characteristics
Table 1(c). Trauma exposure frequency, by type
The eligibility criterion for participation in the current study included the ability to understand English (assessed by a study researcher) and willingness to provide informed consent. The recruitment strategy has been previously detailed (Fani et al., Citation2012; Gillespie et al., Citation2009). Participants completed a 45-to-60 minute interview consisting of clinical assessments administered by trained research assistants. Participants were compensated $15 for their time. Informed consent was approved by Emory University Institutional Review Board. The data that support the findings of this study are openly available in Open Science Framework at https://osf.io/hkmfe/?view_only=a3d8b91df2184dfa8a4d5717abca743c
2.2. Clinical assessments
Participants completed measures to gauge trauma exposure, stress-related psychopathology and history of suicide attempt, as described below:
The Traumatic Events Inventory (TEI) is an 18-item measure of civilian trauma exposure throughout the lifetime that was developed in the context of the GTP assessing a range of events (e.g. sexual assault), as detailed previously (Gillespie et al., Citation2009). Participants responded to the items if they experienced, witnessed, or learned about the event based on a Likert-type scale from 0 (one time or less) to 8 (more than 20 times); the responses were summed to create a frequency score. Frequencies of traumas endorsed on the TEI are detailed in ), Cronbach’s alpha = .77.
The Beck Depression Inventory-II (BDI-II Beck, Steer, & Brown, Citation1996), is a widely-used self-report measure that assesses severity of current depressive symptoms; Cronbach’s alpha = .91. This measure has been validated in populations similar to our own (Grothe et al., Citation2005). The 20-item PTSD Checklist for DSM-5 (PCL-5; (Blevins, Weathers, Davis, Witte, & Domino, Citation2015), was used to assess PTSD symptoms the participant has experienced in the previous month (Cronbach’s alpha = .91); PCL-5 data were available for 64 participants, as other participants had received an older measure of PTSD with items derived from DSM-IV PTSD criteria (PTSD Symptom Scale; Foa, Riggs, Dancu, & Rothbaum, Citation1993). Summed scores for BDI-II and PCL-5 items were used in analyses; scores for each measure were examined separately. The PCL-5 has been designed for use with both military and non-military populations.
Past suicide attempt. Using a ‘yes’ or ‘no’ format, participants answered a single question ‘Have you ever attempted suicide?’ to assess for past suicide attempt.
2.2.1. Moral Injury Exposure and Symptom Scale-Civilian (MIESS-C)
The MIESS-C is a 10-item scale that we adapted from a prior measure, the MIES (Nash et al., Citation2013), a 9-item scale, which assesses exposure to potentially morally injurious events and distress related to moral injury in civilians. The MIESS-C measure () was administered after the TEI; however, participants were not required to anchor their responses to a particular traumatic event. Items 1–6 of the MIESS-C are identical to the original MIES (Nash et al., Citation2013) measure. Items 7–9 of the original measure reflected betrayal with respect to military experiences, and were thus modified to be applicable to civilian experiences. The following changes were applied to the original items: Item 7: I feel betrayed by leaders who I once trusted; MIESS-C Item 7: I feel betrayed by people who I once trusted. Item 8. I feel betrayed by fellow service members who I once trusted; MIESS-C Item 8: I am troubled by this betrayal by specific people. Item 9: I feel betrayed by others outside the US military who I once trusted; MIESS-C Item 9. I feel betrayed by the institutions that I am supposed to trust. (for example, police, church, schools and governmental workers). MIESS-C Item 10 reflects distress associated with the betrayal identified in item 9: I am troubled by this betrayal by the institutions that I am supposed to trust. As such, the items are in sequential pairs, with the first item of each pair reflecting exposure to morally injurious events (items 1, 3, 5, 7, 9) and the second item of each pair reflecting distress related to those events (items 2, 4, 6, 8, 10). Participants responded to questions using a Likert-type scale (1–6), with responses ranging from strongly agree to strongly disagree; higher scores suggest higher exposure and/or distress. Two summed subscale scores were created to distinguish exposure to morally injurious events (MI exposure subscale, items 1, 3, 5, 7, 9; possible score range = 5–30) from distress related to morally injurious events (MI distress subscale, items 2, 4, 6, 8, 10; possible score range = 5–30).
Table 2. Correlations of MIESS-C subscales with trauma exposure, PTSD, and depression symptoms
Following the 10 MIESS-C items, participants were asked to rate: ‘How much did you understand what the questions were about?’ using the same 1–6 Likert scale, with higher scores indicating greater understanding of items and application to trauma experiences, respectively. They were also asked, ‘Do you think the questions on this (MIESS-C) scale apply to your trauma experiences? (referencing the TEI).’ They were asked to provide examples of other non-trauma experiences, if any, that they were responding to outside of those listed on the TEI. Participants were provided space for written responses for these two items. Qualitative data on types of non-trauma experiences endorsed were missing for 3 participants.
2.3. Data analyses
Correlations among the MI indices and types of trauma exposure, as well as current PTSD (total score and symptom clusters) and depressive symptoms, were calculated using IBM SPSS Version 25, using p < .05 significance threshold; Spearman’s Rho correlations were conducted with the TEI child abuse variable, which ranged from 0 to 3 (indicating presence or absence of exposure to sexual, physical, or emotional abuse). Using two separate analyses of covariance (ANCOVA), we examined potential differences in MI exposure and distress among participants with and without past suicide attempts, after accounting for variance associated with current PTSD (PCL-5 total) and depression (BDI-II). PTSD and depressive symptoms were used as covariates given that our objective was to isolate the variance associated with MI from PTSD and depression (which have an established relationship with suicide behaviour).
3. Results
3.1. Descriptive characteristics of the MIESS-C
Cronbach’s alpha for the MIESS-C = .82. The mean for the MIESS-C exposure subscale was 21.1 (SD = 5.37) and distress subscale was 19.3 (SD = 6.12). The distribution of scores for the MIESS-C exposure subscale was not Gaussian (Shapiro–Wilk statistic = .96, p = .006) due to the presence of two significant outliers, which was not improved by rescaling (i.e. natural log and log 10); as such, analyses with the MIESS-C were conducted without the data from these participants. The distributions of MIESS-C distress scores were Gaussian (Shapiro–Wilk statistic = .97, p = .06). Items for the MIESS-C scale (including mean and standard deviations for items) and their relationships with exposure and distress subscales are provided in .
Table 3. MIESS-C items in relation to exposure and distress subscales. Mean score and standard deviation provided for each item
Most participants gave high ratings on the clarity of the MIESS-C questions, with 6 being the highest score possible (M = 5.06, SD = 1.36, Median = 6, Mode = 6). Regarding trauma-relatedness of MIESS-C items, participants endorsed a range of written responses that fell into three categories: 1) high trauma-relatedness of items: ‘yes,’ ‘yeah’; 2) low trauma-relatedness of items: ‘no,’ ‘not really’ ‘not in particular’; and 3) moderate or uncertain degree of trauma-relatedness of items: ‘somewhat,’ ‘slightly,’ ‘probably,’ ‘some,’ ‘somewhat,’ ‘maybe,’ ‘some of them.’ A total of 47 (59%) participants stated that they were thinking about a trauma endorsed on the TEI when responding to the MIESS-C questions (1; high trauma-relatedness of items). Twenty-one participants (26%) stated that the items did not apply to TEI items endorsed (2; low trauma-relatedness of items) and 12 (15%) reported uncertainty about whether MIESS-C items applied to their trauma experiences (3; moderate/uncertain trauma-relatedness of items). Some examples of endorsed morally injurious events: police response to an accident; racist incident in a hospital from police; feeling guilt after a parent’s death; witnessing bullying during childhood.
3.2. Clinical correlations
MIESS-C exposure and distress subscales were significantly and positively correlated with current PTSD and depression symptom severity (see ). When PTSD symptom clusters were examined individually, the strongest positive association was observed between MIESS-C distress and re-experiencing. Current depression severity was also significantly positively correlated with moral injury exposure and distress. The MIESS-C subscale scores were both significantly and positively associated with childhood abuse exposure. MIESS-C distress but not exposure was also positively associated with interpersonal violence exposure in adulthood.
3.3. Associations of moral injury exposure and distress with past suicide attempt
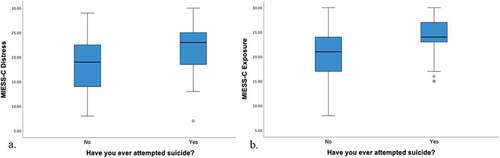
Results of two separate ANCOVAs with MIESS-C distress and exposure variables, respectively, indicated that, after accounting for PTSD-related variance (PCL total) and depression (BDI total), participants with a prior suicide attempt had higher mean MIESS-C exposure scores (M = 24.7, SD = 3.88) compared to those without a prior suicide attempt (M = 22.1, SD = 4.02; F1,59 = 6.05, p = .017; η2 = .093; ). In a similar model including MIESS-C distress scores, we observed that participants with a prior suicide attempt had marginally (non-statistically significant) higher MIESS-C distress scores (F1,59 = 3.51, p = .066, M = 22.9, SD = 5.25, η2 = .057) as compared to participants without a prior suicide attempt (M = 19.9, SD = 5.57).
4. Discussion
In this study, we examined relationships of moral injury exposure and distress with types of trauma exposure as well as trauma-related psychopathology, namely, PTSD and depression symptoms, in a high trauma-exposed, predominantly African-American sample. We also examined moral injury in relation to suicidal behaviour, partialing out PTSD and depression-related variance. Our findings indicate that MIESS-C subscales were correlated with PTSD and depression measures. Participants’ ratings on the clarity of MIESS-C items were high, and the majority considered traumatic experiences morally injurious events, although other types of stressors were also endorsed as ‘index’ events. These data indicated that moral injury severity, particularly distress, was significantly associated with greater trauma exposure, PTSD and depression severity. Finally, we found that exposure to morally injurious events was uniquely associated with suicidal behaviour, even when accounting for PTSD and depressive symptoms.
Consistent with earlier research (Griffin et al., Citation2019), we found that exposure to morally injurious events and related distress were each positively correlated with trauma exposure, in particular, interpersonal trauma. This included childhood maltreatment and interpersonal trauma in adulthood. Notably, exposure to morally injurious events was associated with experiences of childhood maltreatment but not adult interpersonal trauma exposure, whereas distress related to MI was related to both childhood maltreatment and adult interpersonal trauma exposure. It is possible that MI has a kindling effect with respect to trauma, such that increasing exposure to trauma heightens levels of moral distress over time, ultimately increasing risk for negative health outcomes, as indicated in earlier research (Currier, Holland, & Malott, Citation2015). Overall, MI exposure and distress were also moderately associated with severity of PTSD and depressive symptoms. These data extend earlier findings from studies using veteran samples (Battles et al., Citation2018; Wisco et al., Citation2017), indicating that exposure to morally injurious events and related distress can emerge in civilians as well, and is similarly linked to clinical impairment. These data highlight the salience of MI in civilians, which is increasingly being recognized across clinical and research settings (Chaplo et al., Citation2019; Hoffman, Liddell, Bryant, & Nickerson, Citation2018; Nickerson et al., Citation2018, Citation2015), and the related value of assessing moral injury-related phenomena across both veteran and civilian populations.
Further, after accounting for PTSD and depression symptoms, we found that exposure to morally injurious events was higher in participants with past suicidal behaviour. This demonstrates evidence for MI as a distinct trauma-related response that may independently contribute to risk for suicidal behaviour. Our results echo findings of a recent large-scale (N ~ 1000) study indicating that MI, irrespective of PTSD, predicted suicidal ideations and behaviour in National Guard personnel (C. J. Bryan et al., Citation2018). Using structural equation modelling, Bryan and colleagues observed that some trauma-related responses, including anger, grief, guilt and anhedonia, were distinctly associated with a moral injury ‘factor,’ (symptoms of re-experiencing, insomnia and hyperarousal were more related to a PTSD ‘factor’), and that risk for suicide attempt was higher for personnel who reported these symptoms of moral injury, irrespective of their PTSD status (C. J. Bryan et al., Citation2018). A recent study indicates that veterans with relatively greater exposure to morally injurious events had significantly more suicide-related ideation and behaviour compared to veterans with less exposure to these events (Levi-Belz, Greene, & Zerach, Citation2020). A growing body of literature reveals evidence for a MI syndrome that stands apart from PTSD in some ways (Griffin et al., Citation2019). Our data provides further compelling evidence for the uniqueness of MI and its salience as a potential contributor of trauma-related risk for suicidal behaviour.
When examined as part of a growing body of research on MI, these preliminary data on civilians indicate both the utility of a brief measure of MI as well as the need for further comprehensive MI assessment for civilians. This assessment has significant value from a research and clinical standpoint. Mechanistically, little is known about the psychological processes and related neurobiology of moral injury – to our knowledge, only one study has assessed aspects of MI using neurobiological (in this case, neuroimaging) methods (Sun et al., Citation2019). Much is left to be discovered on neurobiological processes that may subserve distress related to MI. As indicated by veteran studies, MI is not a rare phenomenon (Griffin et al., Citation2019), but as of yet it has not been assessed in trauma-exposed treatment-seeking civilians. Given the known barriers to engaging in and completing first-line PTSD treatments (i.e. cognitive processing and prolonged exposure therapy), a lack of MI assessment in trauma-exposed civilians can further endanger proper treatment selection and increase the likelihood of treatment dropout. As such, the findings from this preliminary study show the clinical and research value of developing a MI scale for civilians and testing its psychometric qualities in diverse civilian populations.
We acknowledge several limitations of this study. Our adapted measure of MI was brief (10 items), unlike an existing 24-item measure of MI in youths (Chaplo et al., Citation2019). An expanded MI measure with more items that detail acts of commission and omission (with agency and under duress) as well as witnessing morally injurious events and betrayal, is better suited to examine associations of these facets of MI with exposure to specific traumatic events and psychopathology, as in prior studies (C. J. Bryan et al., Citation2016; Chaplo et al., Citation2019). The brevity of our measure may also be a strength, reducing the burden to participants. Our limited sample size precluded our ability to conduct an exploratory factor analysis to confirm the exposure and distress subscales as distinct factors. However, in one of the two extant MI assessments that measures both exposure and distress, exploratory factor analysis revealed that exposure to MI events and psychological distress related to morally injurious events emerged as two distinct factors, in addition to a betrayal-related factor (Braitman et al., Citation2018). We also sampled a population (GTP population) that has relatively high trauma exposure and is predominantly female and African American, (Fani et al., Citation2013, Citation2019, Citation2012; Gillespie et al., Citation2009; Powers et al., Citation2019). This could be perceived as a limitation to generalizability. However, we believe that the present findings reveal important information for a population that is at disproportionately higher risk for adverse physical and mental health outcomes but has been frequently excluded from trauma/PTSD research. Further, the fact that we assessed MI in a population that has experienced racism-related stressors (e.g. racial discrimination) provided a unique opportunity to examine how MI relates to different types of trauma exposure beyond DSM5 Criterion A stressors. Notably, a number of participants reported witnessing acts of racism as their index stressor for the MI measure. This highlights the need for future MI assessment in racially diverse populations and consideration of racism-related stressors as index traumas for these assessments. We gathered qualitative data for this pilot study to examine the range of non-trauma events endorsed; as such, categories of these events will be created as we develop a more comprehensive civilian MI assessment, to be tested in a large community sample. Given the cross-sectional nature of this investigation, we were unable to assess whether MI preceded suicide attempt, thus precluding our ability to confirm whether MI was, in fact, a risk factor for suicide attempt in this population. Finally, although these data show preliminary evidence for the utility of this measure in civilian samples, further research in larger samples is needed to comprehensively test the psychometric properties of the MIESS-C. We are expanding this measure and administering it to a large, diverse civilian population to identify a range of non-trauma-related stressors that may contribute to MI distress and a broader array of MI reactions; we plan to use exploratory factor analysis to confirm that there are at least two ‘factors’ in this measure related to MI exposure and distress.
In summary, we found that MI is related to extent of trauma exposure, and that moral distress is closely linked to trauma-related responses, including PTSD and depression. However, higher levels of distress related to MI was observed in participants with past suicidal behaviour, even after accounting for PTSD and depressive symptoms. These data support the development and testing of a comprehensive measure of MI in civilians, including populations with exposure to a variety of traumas. Given the prevalence of trauma exposure and suicide in some communities in the United States, the findings from this study bring attention to a construct that has significant public health relevance.
Acknowledgments
We wish to thank the staff and volunteers of the Grady Trauma Project and Fani Affective Neuroscience Lab for their support for this study, as well as all the participants who volunteered their time for this project.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are openly available in Open Science Framework at https://osf.io/hkmfe/?view_only=c8d103008cc54f5abdbcc006c8288629.
Additional information
Funding
References
- Ames, D., Erickson, Z., Youssef, N. A., Arnold, I., Adamson, C. S., Sones, A. C., … Koenig, H. G. (2019). Moral injury, religiosity, and suicide risk in U.S. veterans and active duty military with PTSD symptoms. Military Medicine, 184(3–4), e271–10. doi:10.1093/milmed/usy148
- Battles, A. R., Bravo, A. J., Kelley, M. L., White, T. D., Braitman, A. L., & Hamrick, H. C. (2018). Moral injury and PTSD as mediators of the associations between morally injurious experiences and mental health and substance use. Traumatology, 24(4), 246–254. doi:10.1037/trm0000153
- Beck, A. T., Steer, R. A., & Brown, G. (1996). Manual for Beck Depression Inventory II (BDI-II). San Antonio, Texas: Psychology Corporation.
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. doi:10.1002/jts.22059
- Braitman, A. L., Battles, A. R., Kelley, M. L., Hamrick, H. C., Cramer, R. J., Ehlke, S., & Bravo, A. J. (2018). Psychometric properties of a modified moral injury questionnaire in a military population. Traumatology (Tallahass Fla), 24(4), 301–312. doi:10.1037/trm0000158
- Bryan, A. O., Bryan, C. J., Morrow, C. E., Etienne, N., & Ray-Sannerud, B. (2014). Moral injury, suicidal ideation, and suicidal attempts in a military sample. Traumatology, 20(3), 154–160. doi:10.1037/h0099852
- Bryan, C. J., Bryan, A. O., Anestis, M. D., Anestis, J. C., Green, B. A., Etienne, N., … Ray-Sannerud, B. (2016). Measuring moral injury: Psychometric properties of the moral injury events scale in two military samples. Assessment, 23(5), 557–570. doi:10.1177/1073191115590855
- Bryan, C. J., Bryan, A. O., Roberge, E., Leifker, F. R., & Rozek, D. C. (2018). Moral injury, posttraumatic stress disorder, and suicidal behavior among National Guard personnel. Psychological Trauma : Theory, Research, Practice and Policy, 10(1), 36–45. doi:10.1037/tra0000290
- Chaplo, S. D., Kerig, P. K., & Wainryb, C. (2019). Development and validation of the moral injury scales for youth. Journal of Traumatic Stress, 32(3), 448–458. doi:10.1002/jts.22408
- Currier, J. M., Holland, J. M., & Malott, J. (2015). Moral injury, meaning making, and mental health in returning veterans. Journal of Clinical Psychology, 71(3), 229–240. doi:10.1002/jclp.22134
- Currier, J. M., Holland, J. M., Rojas-Flores, L., Herrera, S., & Foy, D. (2015). Morally injurious experiences and meaning in Salvadorian teachers exposed to violence. Psychological Trauma : Theory, Research, Practice and Policy, 7(1), 24–33. doi:10.1037/a0034092
- Fani, N., Gutman, D., Tone, E. B., Almli, L., Mercer, K. B., Davis, J., … Ressler, K. J. (2013). FKBP5 and attention bias for threat: Associations with hippocampal function and shape. JAMA Psychiatry, 70(4), 392–400. doi:10.1001/2013.jamapsychiatry.2101
- Fani, N., King, T. Z., Clendinen, C., Hardy, R. A., Surapaneni, S., Blair, J. R., … Bradley, B. (2019). Attentional control abnormalities in posttraumatic stress disorder: Functional, behavioral, and structural correlates. Journal of Affective Disorders, 253, 343–351. doi:10.1016/j.jad.2019.04.098
- Fani, N., Tone, E. B., Phifer, J., Norrholm, S. D., Bradley, B., Ressler, K. J., … Jovanovic, T. (2012). Attention bias toward threat is associated with exaggerated fear expression and impaired extinction in PTSD. Psychological Medicine, 42(3), 533–543. doi:10.1017/S0033291711001565
- Feinstein, A., Pavisian, B., & Storm, H. (2018). Journalists covering the refugee and migration crisis are affected by moral injury not PTSD. JRSM Open, 9(3), 2054270418759010. doi:10.1177/2054270418759010
- Foa, E. B., Riggs, D. S., Dancu, C. V., & Rothbaum, B. O. (1993). Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress, 6, 459–473. doi:10.1002/jts.2490060405
- Gillespie, C. F., Bradley, B., Mercer, K., Smith, A. K., Conneely, K., Gapen, M., … Ressler, K. J. (2009). Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry, 31(6), 505–514. doi:10.1016/j.genhosppsych.2009.05.003
- Griffin, B. J., Purcell, N., Burkman, K., Litz, B. T., Bryan, C. J., Schmitz, M., … Maguen, S. (2019). Moral Injury: An Integrative Review. Journal of Traumatic Stress, 32(3), 350–362. doi:10.1002/jts.22362
- Grothe, K. B., Dutton, G. R., Jones, G. N., Bodenlos, J., Ancona, M., & Brantley, P. J. (2005). Validation of the Beck Depression Inventory-II in a low-income African American sample of medical outpatients. Psychological Assessment, 17(1), 110–114. doi:10.1037/1040-3590.17.1.110
- Hoffman, J., Liddell, B., Bryant, R. A., & Nickerson, A. (2018). The relationship between moral injury appraisals, trauma exposure, and mental health in refugees. Depression and Anxiety, 35(11), 1030–1039. doi:10.1002/da.22787
- Hoffman, J., Liddell, B., Bryant, R. A., & Nickerson, A. (2019). A latent profile analysis of moral injury appraisals in refugees. European Journal of Psychotraumatology, 10(1), 1686805. doi:10.1080/20008198.2019.1686805
- Kelley, M. L., Bravo, A. J., Davies, R. L., Hamrick, H. C., Vinci, C., & Redman, J. C. (2019). Moral injury and suicidality among combat-wounded veterans: The moderating effects of social connectedness and self-compassion. Psychological Trauma : Theory, Research, Practice and Policy, 11(6), 621–629. doi:10.1037/tra0000447
- Levi-Belz, Y., Greene, T., & Zerach, G. (2020). Associations between moral injury, PTSD clusters, and depression among Israeli veterans: A network approach. European Journal of Psychotraumatology, 11(1), 1736411. doi:10.1080/20008198.2020.1736411
- Litz, B. T., Contractor, A. A., Rhodes, C., Dondanville, K. A., Jordan, A. H., Resick, P. A., … Consortium, S. S. (2018). Distinct trauma types in military service members seeking treatment for posttraumatic stress disorder. Journal of Traumatic Stress, 31(2), 286–295. doi:10.1002/jts.22276
- Litz, B. T., Stein, N., Delaney, E., Lebowitz, L., Nash, W. P., Silva, C., & Maguen, S. (2009). Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review, 29(8), 695–706. doi:10.1016/j.cpr.2009.07.003
- Nash, W. P., Marino Carper, T. L., Mills, M. A., Au, T., Goldsmith, A., & Litz, B. T. (2013). Psychometric evaluation of the moral injury events scale. Military Medicine, 178(6), 646–652. doi:10.7205/MILMED-D-13-00017
- Nickerson, A., Hoffman, J., Schick, M., Schnyder, U., Bryant, R. A., & Morina, N. (2018). A longitudinal investigation of moral injury appraisals amongst treatment-seeking refugees. Frontiers in Psychiatry, 9, 667. doi:10.3389/fpsyt.2018.00667
- Nickerson, A., Schnyder, U., Bryant, R. A., Schick, M., Mueller, J., & Morina, N. (2015). Moral injury in traumatized refugees. Psychotherapy and Psychosomatics, 84(2), 122–123. doi:10.1159/000369353
- Powers, A., Fani, N., Murphy, L., Briscione, M., Bradley, B., Tone, E. B., … Jovanovic, T. (2019). Attention bias toward threatening faces in women with PTSD: Eye tracking correlates by symptom cluster. European Journal of Psychotraumatology, 10(1), 1568133. doi:10.1080/20008198.2019.1568133
- Shay, J. (1994). Achilles in Vietnam: Combat trauma and the undoing of character. New York: Scriber.
- Sun, D., Davis, S. L., Haswell, C. C., Swanson, C. A., Mid-Atlantic, M. W., LaBar, K. S., … Morey, R. A. (2018). Brain structural covariance network topology in remitted posttraumatic stress disorder. Frontiers in Psychiatry, 9, 90. doi:10.3389/fpsyt.2018.00090
- Sun, D., Phillips, R. D., Mulready, H. L., Zablonski, S. T., Turner, J. A., Turner, M. D., … Morey, R. A. (2019). Resting-state brain fluctuation and functional connectivity dissociate moral injury from posttraumatic stress disorder. Depression and Anxiety, 36(5), 442–452. doi:10.1002/da.22883
- Wisco, B. E., Marx, B. P., May, C. L., Martini, B., Krystal, J. H., Southwick, S. M., & Pietrzak, R. H. (2017). Moral injury in U.S. combat veterans: Results from the national health and resilience in veterans study. Depression and Anxiety, 34, 340–347. doi:10.1002/da.22614
- Yan, G. W. (2016). The invisible wound: Moral injury and its impact on the health of operation enduring freedom/operation Iraqi freedom veterans. Military Medicine, 181(5), 451–458. doi:10.7205/MILMED-D-15-00103