ABSTRACT
Background: With few RCTs having compared active treatments for paediatric PTSD, little is known about whether or which baseline (i.e. pre-randomization) variables predict or moderate outcomes in the evaluated treatments.
Objective: To identify predictors and moderators of paediatric PTSD outcomes for Eye Movement Desensitization and Reprocessing Therapy (EMDR) and Cognitive Behavioural Writing Therapy (CBWT).
Method: Data were obtained as part of a multi-centre, randomized controlled trial of up to six sessions (up to 45 minutes each) of either EMDR therapy, CBWT, or wait-list, involving 101 youth (aged 8–18 years) with a PTSD diagnosis (full/subthreshold) tied to a single event. The predictive and moderating effects of the child’s baseline sociodemographic and clinical characteristics, and parent’s psychopathology were evaluated using linear mixed models (LMM) from pre- to post-treatment and from pre- to 3- and 12-month follow-ups.
Results: At post-treatment and 3-month follow-up, youth with an index trauma of sexual abuse, severe symptoms of PTSD, anxiety, depression, more comorbid disorders, negative posttraumatic beliefs, and with a parent with more severe psychopathology fared worse in both treatments. For children with more severe self-reported PTSD symptoms at baseline, the (exploratory) moderator analysis showed that the EMDR group improved more than the CBWT group, with the opposite being true for children and parents with a less severe clinical profile.
Conclusions: The most consistent finding from the predictor analyses was that parental symptomatology predicted poorer outcomes, suggesting that parents should be assessed, supported and referred for their own treatment where indicated. The effect of the significant moderator variables was time-limited, and given the large response rate (>90%) and brevity (<4 hours) of both treatments, the present findings suggest a focus on implementation and dissemination, rather than tailoring, of evidence-based trauma-focused treatments for paediatric PTSD tied to a single event.
HIGHLIGHTS
Given the time-limited significance of differential treatment effects on outcome, brevity and large effect size for EMDR and cognitive-behavioural writing therapy for paediatric PTSD, future focus should be on enhancing delivery of these treatments, rather than tailoring them.
Antecedentes: Dado que pocos ECA (ensayos controlados aleatorizados) han comparado tratamientos activos para el TEPT pediátrico, se sabe poco acerca de si las variables basales (es decir, pre-aleatorización) predicen o moderan los resultados en los tratamientos evaluados.
Objetivo: Identificar predictores y moderadores de los resultados del TEPT pediátrico para la Terapia de Reprocesamiento y Desensibilización por Movimientos Oculares (EMDR) y la Terapia de Escritura Cognitiva Conductual (CBWT en sus siglas en ingles).
Método: Los datos se obtuvieron como parte de un ensayo controlado aleatorizado multicéntrico de hasta seis sesiones (de hasta 45 minutos cada una) de terapia EMDR, CBWT o lista de espera, que incluyó a 101 jóvenes (de 8 a 18 años de edad) con un diagnóstico de TEPT (total/subumbral) vinculado a un solo evento. Los efectos predictivos y moderadores de las características sociodemográficas y clínicas basales del niño y la psicopatología de los padres se evaluaron mediante modelos lineales mixtos (MLM) desde antes y después del tratamiento y desde antes hasta los 3 y 12 meses de seguimiento.
Resultados: En el post-tratamiento y en el seguimiento a los 3 meses, los jóvenes con un trauma índice de abuso sexual, síntomas severos de TEPT, ansiedad, depresión, más trastornos comórbidos, creencias postraumáticas negativas y con un padre con psicopatología más severa obtuvieron los peores resultados en ambos tratamientos. Para los niños con síntomas de TEPT auto-informados más graves al inicio del estudio, el análisis del moderador (exploratorio) mostró que el grupo EMDR mejoró más que el grupo CBWT, siendo lo opuesto para los niños y los padres con un perfil clínico menos grave.
Conclusiones: El hallazgo más consistente de los análisis de predictores fue que la sintomatología de los padres predijo peores resultados, lo que sugiere que los padres deben ser evaluados, apoyados y referidos para su propio tratamiento cuando esté indicado. El efecto de las variables moderadoras significativas fue limitado en el tiempo, y dada la gran tasa de respuesta (> 90%) y la brevedad (<4 horas) de ambos tratamientos, los presentes hallazgos sugieren un enfoque en la implementación y diseminación, en lugar de la adaptación, de tratamientos centrados en el trauma basados en la evidencia para el TEPT pediátrico vinculados a un solo evento.
背景: 由于很少有 RCT 比较儿科 PTSD 的积极治疗, 因此对基线 (即随机分组前) 变量是否或者哪些可以预测或调节评估治疗的结果知之甚少。;
目的: 确定眼动脱敏与再加工疗法 (EMDR) 和认知行为写作疗法 (CBWT) 的儿科 PTSD 结果的预测因素和调节因素。;
方法: 数据获取于一项多中心, 随机对照试验的一部分, 该试验涉及 101 名有单次事件PTSD 诊断 (完全/亚阈值) 青年 (8-18 岁) 参加了最多 6 次 (每次最多 45 分钟) 的 EMDR 治疗, CBWT 或候补名单。;从治疗前到治疗后以及从治疗前到 3个月和 12个月的随访, 使用线性混合模型 (LMM) 评估儿童基线社会人口学和临床特征以及父母精神病的预测和调节作用。;
结果: 在治疗后和 3 个月的随访中, 有性虐待相关创伤, PTSD 严重症状, 焦虑, 抑郁, 更多共病障碍, 消极的创伤后信念以及父母有更严重精神病的青少年的情况在这两种治疗中都更糟。;对于基线自我报告的 PTSD 症状更严重的儿童, (探索性) 调节分析表明 EMDR 组比 CBWT 组改善更多, 而对于临床特征较轻的儿童和父母则相反。;
结论: 预测分析中最一致的发现是父母的症状预测了较差的结果, 这表明父母应该在有需要的情况下接受评估, 支持和转诊以进行自己的治疗。;显著调节变量的效应是有时间限制的, 并且鉴于两种治疗的大反应率 (>90%) 和简短性(<4 小时), 目前的研究结果建议关注实施和传播, 而不是针对单个事件相关的儿科 PTSD 量身定制的循证创伤治疗
1. Introduction
Practice guidelines for paediatric posttraumatic stress disorder (PTSD) recommend trauma-focused psychological therapies as the first-line treatment approach, i.e. various forms of cognitive-behavioural therapy (CBT) including trauma-focused CBT (TF-CBT; Cohen, Mannarino, & Deblinger, Citation2006) prolonged exposure (Foa, Chrestman, & Gilboa-Schechtman, Citation2008) cognitive therapy for PTSD (Smith, Perrin, & Yule, Citation2010), (KiD)NET (Schauer, Neuner, & Elbert, Citation2017) as well as eye movement desensitization and reprocessing (EMDR) therapy (International Society of Traumatic Stress Studies (ISTSS), Citation2019; National Institute for Health and Clinical Excellence (NICE), Citation2018; Shapiro, Citation2018; WHO, Citation2013). These recommendations are supported by a number of meta-analyses that found both trauma-focused CBT and EMDR therapy superior to controls, usually wait-list or treatment as usual (Bastien, Jongsma, Kabadayi, & Billings, Citation2020; Brown et al., Citation2017; Gutermann et al., Citation2016; Mavranezouli et al., Citation2020; Morina, Koerssen, & Pollet, Citation2016). Of all therapies, TF-CBT has received the strongest empirical support to date. Until now, five randomized controlled trials (RCTs) have compared trauma-focused CBT to EMDR therapy for paediatric PTSD, with no differences observed for diagnostic remission or symptom reduction (Jaberghaderi, Greenwald, Rubin, Zand, & Dolatabadi, Citation2004; Jaberghaderi, Rezaei, Kolivand, & Shokoohi, Citation2019; Diehle et al., Citation2015; De Roos et al., Citation2011, Citation2017).
With few RCTs having compared active treatments for paediatric PTSD, little is known about whether or which baseline (i.e. pre-randomization) variables predict or moderate outcomes in the evaluated treatments (i.e. which treatment works best for whom; Kraemer, Citation2016). RCTs reporting upon predictors have almost exclusively involved evaluations of trauma-focused CBT (e.g. Kane et al., Citation2016; Nixon, Sterk, & Pearce, Citation2012; Nixon, Sterk, Pearce, & Weber, Citation2017; Qouta, Palosaari, Diab, & Punamaki, Citation2012; Weems & Scheeringa, Citation2013). Across these studies, the presence of parental psychopathology (specifically maternal depression) has consistently been found to predict poorer child’s PTSD treatment response in trauma-focused CBT (Alisic, Jongmans, van Wesel, & Kleber, Citation2011; Dorsey et al., Citation2017; Trickey, Siddaway, Meiser-Stedman, Serpell, & Field, Citation2012). With respect to the child’s pretreatment levels of psychopathology, gender, age, type of trauma exposure, level of comorbid symptoms as predictors of child PTSD outcomes, the findings in the literature are mixed and inconclusive. Some studies found evidence that youth with high pretreatment levels of PTSS (e.g. Lindebø Knutsen, Sachser, Holt, Goldbeck, & Jensen, Citation2020; Wamser-Nanney, Scheeringa, & Weems, Citation2016), high initial level of anxiety and depression (Wamser-Nanney et al., Citation2016), girls (e.g. Lindebø Knutsen et al., Citation2020), and older children (e.g. Goldbeck, Muche, Sachser, Tutus, & Rosner, Citation2016) may be at risk of poorer treatment outcomes. However, findings of other studies showed that the aforementioned factors were not related to the effectiveness of treatment (for pretreatment levels of comorbid symptoms, e.g. Lindebø Knutsen et al., Citation2020; for gender, e.g. Kane et al., Citation2016; for age, e.g. Kane et al., Citation2016; Lindebø Knutsen et al., Citation2020; for type of trauma exposure, e.g. Goldbeck et al., Citation2016). Regarding posttraumatic cognitions as predictor, it is well known that this variable and the severity of posttraumatic stress symptoms (PTSS) are strongly associated, and that pre-treatment level in posttraumatic cognitions mediates outcome in TF-CBT (Jensen, Holt, Mørup Ormhaug, Fjermestad, & Wentzel-Larsen, Citation2018; Pfeiffer, Sachser, de Haan, Tutus, & Goldbeck, Citation2017). However, much less is known about the association between pre-treatment level in posttraumatic cognitions and the trajectory of PTSD treatment outcome in youth. Results of the only study that explored the latter association showed no evidence to support that having many maladaptive posttraumatic cognitions was related to treatment non response (Lindebø Knutsen et al., Citation2020). With respect to EMDR therapy for paediatric PTSD, only one meta-analysis (Moreno-Alcázar et al., Citation2017 explored if baseline variables were related to treatment response. The authors identified eight RCTs that compared this treatment to either wait-list, standard care, placebo or trauma-focused CBT. Across EMDR studies, gender (male) was the only variable that was related to poorer treatment outcomes.
Regarding moderators of treatment response in paediatric PTSD, the evidence-base is even more sparse (Taylor et al., Citation2015) and only explored in trauma-focused CBT with no moderators being evaluated for EMDR therapy. A recent review examined moderators in the areas of child characteristics (age, gender, ethnicity, domicile), parent/caregiver variables (involvement, functioning), trauma type and treatment factors (i.e. dose, individual/group; Danzi & La Greca, Citation2020). Age is the most frequently studied moderator variable with several studies showing age to be a significant moderator of treatment response suggesting that older youth receiving TF-CBT may have improved treatment outcomes (Danzi & La Greca, Citation2020; Gutermann et al., Citation2016; Morina et al., Citation2016). Reason might be that older youth have developed more cognitive capabilities affecting positively their responsiveness to a CBT approach. For gender, domicile, ethnicity, trauma type, parent involvement, treatment dose, individual/group and sudden gains in treatment response, results were inconsistent and support for these factors being a moderator variable was absent or limited. Regarding future studies, specifically the inclusion of comorbidity as a potential moderator variable is recommended as comorbidity may hinder recovery (Danzi & La Greca, Citation2020).
In conclusion, the inferences that can be drawn from the treatment literature involving predictors and moderators of outcome in trauma-focused CBT and EMDR therapy are limited due to the high level of heterogeneity in respect of inclusion criteria and treatments evaluated, small sample sizes, and no or brief follow-ups, with further studies needed before tailoring of treatment can be an empirically based process (Danzi & La Greca, Citation2020; Taylor, Graham, & Weems, Citation2015).
The purpose of the present paper was to identify potential predictors and moderators of outcome in a previously published, multi-centre, three-armed, rater-blinded RCT comparing EMDR therapy to Cognitive Behavioural Writing Therapy (CBWT), and delayed treatment (wait-list), for children and adolescents (aged 8–18 years) with a current diagnosis of PTSD or subthreshold PTSD tied to a single traumatic event (De Roos et al., Citation2017). Given that this trial was not designed to test for predictor and moderator effects, the selection of potential predictor and moderator variables was based on relevant variables identified in the paediatric PTSD literature that were also measured in the abovementioned trial. The influence of the following pre-treatment variables on outcome were evaluated: age, gender, trauma type, severity of the child’s symptoms (PTSD, anxiety, and depression), the number of comorbid psychiatric diagnoses, the child’s trauma-related beliefs, and parental psychopathology (overall, PTSD, anxiety, and depression). As parental psychopathology has been the most consistent outcome predictor in RCTs of trauma-focused CBT, we hypothesized that participants with parents suffering from more severe psychopathology would have poorer PTSD outcomes, irrespective of treatment assignment. Furthermore, given research findings that change of posttraumatic cognitions is crucial for treatment outcome and cognitive restructuring is a core component of CBWT, but not of EMDR therapy, we also hypothesized that children with higher levels of child’s trauma-related beliefs would profit more from CBWT than from EMDR therapy.
2. Method
2.1. Ethics statement
The study was approved by the Ethics Committee of the University of Amsterdam and registered in the Dutch Trial Register (www.trialregister.nl, 3870 or NTR3870).
All participants provided informed written consent.
2.1.1. Participants
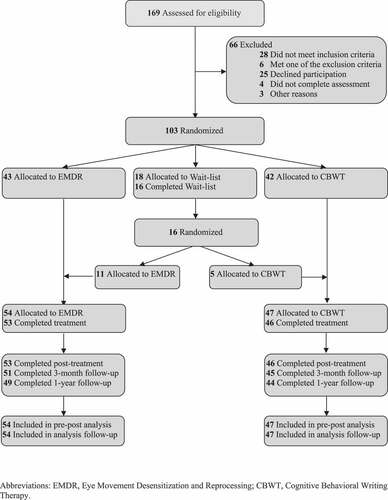
Participants were 103 treatment-seeking youth with a primary diagnosis of DSM-IV PTSD (full or subthreshold) tied to a single traumatic event that occurred at least 1 month prior to inclusion (for full details, see De Roos et al., Citation2017). All children underwent structured diagnostic interviews employing the Anxiety Disorders Interview Schedule (child and parent version; Silverman & Albano, Citation1996) and were assessed (blindly) at baseline, post-treatment/post-waitlist (WL), and at 3- and 12-month follow-ups. Participants were randomly assigned to one of the three conditions and those who still met inclusion criteria at the end of the 6-week WL were re-randomized to EMDR or CBWT. Mean age of the sample was 13.6 years (SD 2.92), 57.3% of the participants was female, 28.2% were immigrants. Regarding trauma type, 23.3% experienced physical abuse, 26.2% sexual abuse, 19.4% accident or injury of a loved one, 18.4% traumatic loss and 12.6% disaster/and other. The present study used all available treatment outcome data (N = 101) from this trial, inclusive the participants that were first randomized into wait-list. Two participants dropped out immediately after randomization (one from EMDR, one from CBWT) and were excluded because they did not receive any treatment. provides the CONSORT flow chart for the trial.
2.2. Measures
2.2.1. Outcome
Child’s PTSD symptom severity, assessed using the total score on the Revised Children’s Responses to Trauma Inventory – Child Version (CRTI-C; Alisic & Kleber, Citation2010) served as the primary outcome variable. The CRTI-C is a 34-item self-report measure of DSM-IV PTSD symptoms (1 = never; 5 = always) over the past 7 days. A total score is computed along with four subscales: intrusion (7 items), avoidance (11 items), arousal (6 items), and other child-specific responses to the trauma that are not mentioned in the DSM-IV PTSD criteria (10 items). The CTRI-C has excellent psychometric properties (e.g. Cronbach’s α = 0.92; Alisic & Kleber, Citation2010).
2.2.2. Baseline predictors and moderators
For all candidate predictor/moderator variables based on the child’s characteristics, we used information obtained from both the child and the parent (included separately in the analyses), except for trauma-related beliefs (based only on child report). The severity of the child’s PTSD symptoms was assessed using the Revised Children’s Responses to Trauma Inventory – Child Version (CRTI-C; Alisic & Kleber, Citation2010). The child’s anxiety and depression were assessed via total scores on the 47-item Revised Child Anxiety and Depression Scale, Child and Parent Versions (RCADS-C/P; Chorpita, Yim, Moffitt, Umemoto, & Francis, Citation2000). The number of comorbid diagnoses was assessed via separate child and parent interviews using the Anxiety Disorders Interview Schedule for DSM-IV, Child and Parent Versions (ADIS-C/P; Silverman & Albano, Citation1996). The child’s trauma-related beliefs were assessed via the total score on the 25-item Children’s Post Traumatic Cognitions Inventory (CPTCI; Meiser-Stedman et al., Citation2009; Diehle et al., Citation2015). Parental PTSD symptoms, only in relation to their child’s index trauma, were assessed via the total score on the 22-item Impact of Event Scale-Revised (IES-R; Weiss & Marmar, Citation1997). Finally, overall parental psychopathology, anxiety and depression were assessed via total scores (and respective subscales) of the 53-item, Brief Symptom Inventory (BSI; Derogatis, Citation1992). For parent-report measures of the child’s functioning, primarily mothers (88%) completed the measures, followed by fathers (11%) and other caretakers (1%).
2.3. Interventions
For a full description of the two treatments, see De Roos et al (Citation2017). Briefly, CBWT and EMDR are manual-based, trauma-focused treatments that were delivered in up to six, weekly individual sessions lasting up to 45 minutes each. There were no homework assignments, no separate sessions for parents, and no instructions given to parents to encourage their child to discuss the trauma or to confront reminders in either treatment. EMDR followed the standard 8-phase protocol developed by Shapiro (Citation2018) with age-appropriate modifications suggested by Tinker and Wilson (Citation1999) and Greenwald (Citation1999), using the Dutch translation of the EMDR protocol for children and adolescents. It consists of history taking, treatment planning, preparation, reprocessing, installation of a positive cognition, checking for and then reprocessing any residual disturbing body sensations, positive closure and evaluation. During all reprocessing phases, the participant tracked the movement of therapist’s index finger with their eyes as the therapist moved their hand back and forth horizontally across the participant’s field of vision (saccades). CBWT (included: psychoeducation, imaginal exposure via the construction of a written narrative of the index trauma), cognitive restructuring, promoting healthy coping strategies, and enlisting support from loved ones or friends (social sharing; Van der Oord, Lucassen, Van Emmerik, & Emmelkamp, Citation2010). Both treatments were delivered by fully trained clinical psychologists, experienced in the treatment of paediatric PTSD, trained to administer either CBWT or EMDR before commencing the trial, and who received supervision from an expert in either CBWT or EMDR on a monthly basis during the trial. Session duration was timed with a stopwatch, so that the exact mean number of minutes per treatment (up to six sessions lasting up to 45 minutes) could be calculated. Mean contact time for EMDR and CBWT was, respectively, 4.1 sessions/140 minutes versus 5.4 sessions/227 minutes.
3. Statistical analyses
All analyses were conducted using version 23 of SPSS (IBM Corp, Armonk, NY).
For the predictor/moderator analyses, we carried out linear mixed modelling (LMM) using all available measurement occasions for the outcome variable (child-reported PTSD symptoms as assessed by the CRTI-C). For all analyses, we used the baseline (pre-treatment) values for the candidate predictor/moderators. Variables lacking an observed value of zero with substantial interpretation were (grand) mean centred. In the first series of analyses, candidate predictors of change in child-reported PTSD symptoms were evaluated for all participants (i.e. across EMDR and CBWT conditions) from pre-treatment to post-treatment, pre-treatment to 3-month follow-up, and pre-treatment to 12-month follow-up. For the moderator analyses (cross-level) interaction terms were added to the model to assess whether the moderator influenced changes in child-reported PTSD symptoms for the three time episodes described above. An additional interaction term was added to assess whether the moderator effects were different between the EMDR and CBWT groups. For all analyses, a random intercept was introduced into the models to account for baseline differences between participants, with alpha set to .05 for both main and interaction effects.
4. Results
4.1. Baseline differences
presents descriptive data for the candidate predictor and moderator variables at baseline separately for participants randomized to EMDR or CBWT, as well as comparisons between the two groups. Overall, the two groups were similar except that: 1) the CBWT group scored higher than EMDR on the child-report measures of PTSD (CRTI-C), depression and anxiety (RCADS-C), and negative trauma-related beliefs (CPTCI), and 2) the two groups differed in the distribution of trauma types. Baseline differences between the two treatment groups do not create a problem for the analyses as individual differences are utilized by LMM to detect whether there is a predictor or moderator effect.
Table 1. Descriptive statistics for the outcome and predictor/moderator variables at baseline by treatment group and between group comparisons (N = 101)
4.2. Predictor analyses
presents the results of the LMM analyses for the effects (irrespective of treatment condition) of the candidate predictors on child-reported PTSD symptoms from pre- to post-treatment, pre-treatment to 3-month follow-up, and pre-treatment to 12-month follow-up. As can be seen in , age and gender did not significantly predict outcomes but trauma type did. For all types of traumatic events, PTSD symptoms significantly improved after trauma treatment (see , change per week). However, children exposed to physical abuse or assault showed a significantly greater decline in PTSD symptoms than children exposed to one of the other types of traumatic events (, estimate −1.303). On the contrary, sexually abused children showed a significantly smaller decline in PTSD symptoms than children exposed to one of the other traumatic events (, estimate .982). Only the predictive effect for sexual abuse remained from pre-treatment to 3-month follow-up.
Table 2. Results of linear mixed models testing predictor by time interaction on change per week in child-reported PTSD symptoms from pre-treatment to post-treatment and follow-up (N = 101)
With regards to child psychopathology, children who had more severe symptoms of PTSD, depression, and anxiety, more comorbid diagnoses, and more negative trauma-related beliefs, experienced a significantly smaller decline in PTSD symptoms (child reported) as measured from pre- to post-treatment. These predictive effects were maintained from pre-treatment to the 3-month follow-up assessment, but only when based on information obtained from the parent and not the child. The exception was that severity of the (child-reported) trauma-related beliefs still predicted poorer outcome from pre-treatment to the 3-month-follow-up. None of the child psychopathology variables predicted outcomes from pre-treatment to 12-month follow-up.
In respect of parental psychopathology, children whose parent reported higher levels of PTSD (tied to their child’s index trauma), depression and anxiety, and overall psychopathology, experienced a significantly smaller decline in PTSD symptoms (child-reported) as measured from pre- to post-treatment and from pre-treatment to the 3-month follow-up. Parental psychopathology did not predict outcomes from pre-treatment to the 12-month follow-up.
4.3. Moderator analyses
provides the results of the LMM analyses testing the effects upon outcome (change in child-reported PTSD symptoms from baseline) of the interaction between time, the candidate moderator, and treatment assignment (EMDR vs CBWT), from pre- to post-treatment, pre-treatment to 3-month follow-up, and pre-treatment to 12-month follow-up. Given the fact that the randomization procedure did not involve stratification by trauma type and a rather skewed distribution of trauma types between conditions, we excluded this variable from the moderator analyses. Results of the moderator analyses showed a significant effect for several indices of child and parental psychopathology, indicating a differential effect of these variables on outcomes in EMDR and CBWT. Specifically, outcome from pre- to post-treatment was significantly moderated by the baseline severity of the child’s PTSD (child- and parent-report), anxiety and depressive symptoms (parent-report only), and by the severity of the parent’s psychopathology (PTSD, depression, anxiety, and overall psychopathology). Parental depression and anxiety continued to moderate outcomes from pre-treatment to the 3-month follow-up, and parental anxiety from pre-treatment to the 12-month follow-up. A significant effect was observed for age, in that older children experienced a smaller reduction in PTSD symptoms in CBWT than EMDR therapy, but only from pre-treatment to the 3-month follow-up.
Table 3. Results of linear mixed models testing for effect between time, moderator and treatment condition, with estimates of change per week and the difference in change estimates between CBWT and EMDR for child-reported PTSD symptoms from pre-treatment to post-treatment and follow-up (N = 101)
To further explore the direction and strength of the moderating effects of child and parent psychopathology on outcomes (rates of decrease in child-reported PTSD symptoms in EMDR and CBWT), the effects on outcome of the moderator measured at the low (total score < 40th percentile) and high (total score > 60th percentile) ends of severity at baseline, were calculated as an illustration (cf., Hayes, Citation2013). By taking these percentiles as a reference point, the results refer to a large part of the sample. As the RCT from which these data were drawn was not designed as a moderator study, we did not test for differential outcomes between EMDR and CBWT to reduce the risk of false positive/negative findings.
provides the estimated mean of child-reported PTSD symptoms from pre- to post-treatment for high- and low-scoring groups of EMDR therapy and CBWT participants, and the difference in estimates (within groups), for the significant moderator variables (see Appendix S1 for the pre-treatment to follow-up results). At higher severity levels of the child (PTSD, anxiety and depression) and parental psychopathology moderators (PTSD, overall psychopathology, depression, and anxiety), CBWT and EMDR therapy appeared equally effective. At the lower severity level of these moderators (< 40th percentile), participants in CBWT experienced a greater decrease in PTSD symptoms than those in EMDR therapy (CRTI-C, range of 7 to 14 points). The one exception to this pattern of results was that children with more severe PTSD symptoms at baseline (child-reported) experienced a greater decrease in PTSD symptoms (child-reported) in EMDR therapy than CBWT (5 points on the CRTI-C scale).
Table 4. Estimated means for child-reported PTSD symptoms at pre- and post-treatment, and difference (Δ) between these means, separately for participants scoring at the high- and low-end of the significant moderator variables in EMDR and CBWT groups
5. Discussion
To our knowledge, the current study is one of the few RCTs (see also Jensen et al., Citation2014; Kane et al., Citation2016) that has evaluated candidate moderators for two active psychological treatments or treatment as usual (TAU) for children and adolescents (aged 8–18 years) meeting full or subthreshold diagnostic criteria for PTSD, and the first to include CBWT and EMDR therapy. The results add to the literature in that the present study is the first to investigate the role of differential treatment moderators at a long-term follow-up (i.e. 12 months). The main results of the predictor analyses showed that a more severe clinical profile at the child and parental level predicted a smaller reduction in child-reported PTSD symptoms from pre- to post-treatment in both CBWT and EMDR therapy. The same pattern held true from pre-treatment to the 3-month follow-up, with the exception that mainly parental reports of the child’s symptoms and parental psychopathology continued to predict poorer outcomes. Interestingly, the results of the (exploratory) moderator analyses showed differential responses in outcome, mainly from pre- to post-treatment, albeit there were high rates of improvement for both methods at post-treatment (> 90% achieved diagnostic remission) in less than 4 hours of therapy (De Roos et al., Citation2017).
As hypothesized, an important finding from the predictor analyses was that parental psychopathology (i.e. PTSD, anxiety, depression, and overall psychopathology) predicted poorer outcomes for the child in both treatments, which is largely consistent with an extensive body of literature (Alisic et al., Citation2011; Trickey et al., Citation2012). At the very least, this finding emphasizes the importance of assessing parental psychopathology at intake or during the diagnostic phase, and where necessary, adding extra sessions of parent guidance or referring the parent for their own treatment. With respect to the child’s levels of psychopathology as predictors of child PTSD outcomes, the results of the present study are consistent with earlier CBT studies (Lindebø Knutsen et al., Citation2020; Wamser-Nanney et al., Citation2016) in that children with more severe PTSD at baseline fared worse in both EMDR therapy and CBWT. It is conceivable that clinicians could add extra child sessions to either of these treatments to enhance outcomes for more affected children. Moreover, a noteworthy finding is that children with more trauma-related beliefs fared less well in both treatments. This finding is consistent with cognitive models of PTSD as applied to both adults and children (Ehlers & Clark, Citation2000; Meiser-Stedman et al., Citation2019) that emphasize the central role of such beliefs in the development, maintenance and severity of PTSD, and as such are important targets for treatment. In this regard, the present study extends findings for the relevance of trauma-related beliefs to outcomes in EMDR therapy and CBWT. Finally, those with sexual abuse as their index trauma fared worse in both treatments whereas gender and age did not predicted outcome either. The latter is contrary to the results of Danzi and La Greca (Citation2020), suggesting that trauma-focused treatment seemed to be more effective in older youth. Apparently, both EMDR therapy and CBWT used adequate age-appropriate modifications to the whole age-group (8–18 years), so that both treatments could easily be applied.
As to the moderator analyses, contrary to our hypothesis, dysfunctional posttraumatic cognitions did not moderate treatment response. The level of these cognitions did equally decrease for CBWT and EMDR therapy. This is remarkable because EMDR therapy is not targeting dysfunctional cognitions, while CBWT is focused on changing dysfunctional cognitions by restructuring. Maybe, this finding suggest that the level of dysfunctional posttraumatic cognitions can better be seen as a manifestation of PTSD, that improves when PTSD symptoms decreases (Cuijpers, Citation2019). The overall results of the moderator analyses suggest that children with high scores on the significant moderator variables, especially child and parental psychopathology, experienced similar levels of improvement in both treatments. There were two exceptions to this pattern. First, children reporting higher levels of PTSD at baseline experienced a greater reduction in PTSD symptoms in EMDR therapy at post-treatment than those who received CBWT. Second, children with lower levels of psychopathology, and children whose parent had lower levels of psychopathology, appeared to fare better in CBWT than EMDR therapy. These results are in line with experimental research in the area of EMDR therapy showing that increased level of arousal (as when individuals have a high level of PTSD symptoms (Kim, Bae, & Park, Citation2008), both in relation to the memory (Van den Hout, Eidhof, Verboom, Littel, & Engelhard, Citation2014) and in general (Littel, Remijn, Tinga, Engelhard, & van den Hout, Citation2017), is likely to lead to stronger desensitizing effects and thus better treatment outcomes. Clearly, results should be interpreted with caution as the child’s baseline levels of PTSD were higher in the CBWT than EMDR therapy group (), and both treatments yielded high rates of diagnostic remission and symptom change in the original trial. While not measured in this study, it is possible that the findings for the moderating role of child psychopathology partly reflects an interaction between the child’s level of distress measured at the symptom level and the levels of emotional arousal they experienced during subsequent treatment sessions. In EMDR therapy, the child is asked to recall the most disturbing images from their traumatic memory, which is usually accompanied by an immediate increase in emotional arousal, and this may benefit those with more severe PTSD symptoms. In CBWT, the child builds an increasingly detailed, written trauma narrative over successive sessions, alongside cognitive restructuring, identifying positive coping responses, and sharing the narrative with loved ones, all of which may elicit emotional arousal in a more gradual fashion and benefit children with less severe PTSD. As emotional arousal is argued to be necessary to the activation and reconsolidation of the trauma memory, and thus an essential change mechanism in all trauma-focused therapies (Layne et al., Citation2015), future comparative studies should measure in-session arousal as part of a process of identifying possible outcome moderators and mediators. In addition, we did not measure parenting style/skills or change in the parent’s symptoms during the course of the child’s treatment, both of which may be important to interpreting the current findings. Overall, it should be noted that both for the predictor and moderator analyses, the significant effect of variables on outcome were time-limited and primarily found for the pre- to post-treatment interval (a short time span of up to 6 weekly treatment sessions) and to a lesser extent from pre-treatment to the 3-month follow-up, with one exception for pre-treatment to 1-year follow-up.
As with any study, several strengths and limitations need to be noted. The present study benefits from the data being collected as part of a large RCT comparing two active, evidence-based treatments for paediatric PTSD, and involving a blinded diagnostic interview, a wide range of standardized child- and parent-report symptom measures, low attrition rates (2%), and 3- and 12-month follow-ups (De Roos et al., Citation2017). This study shows a high degree of external validity. However, an important limitation is that this trial was not designed to test for predictor and moderator effects. The choice of candidate predictors and moderators for the present study was pragmatic, reflecting the measures that were used to assess clinical outcomes in the earlier RCT. To restrict the risk of obtaining chance findings, we did not test for interactions between predictors or moderators. Secondly, this study was carried out in the Netherlands, with clinically referred children (aged 8–18 years) who had a current DSM-IV diagnosis of either full or subthreshold PTSD tied to a single traumatic event, and thus the current findings may not generalize to other populations, trauma types or clinical settings.
Future studies should include measures related to hypotheses about candidate predictors, mediators and moderators of treatment outcome and test for interactions between predictors or moderators. Moreover, new statistical approaches need to be considered, because individual RCTs often lack the power to examine the contribution of specific factors to clinical outcomes and have produced inconsistent results across studies. Individual participant data meta-analysis (IPD-MA) may provide a more reliable means to address the question ‘what works for whom’, due to combined data sets and sufficient statistical power (De Haan et al., Citation2021). Future studies may also consider combining baseline patient characteristics to create a single strong moderator as a more powerful and precise measure to detect differential treatment responses (Wallace, Frank, & Kraemer, Citation2013) or consider the use of the Personalized Advantage Index approach (PAI; DeRubeis et al., Citation2014), which is a treatment selection algorithm, that predicts the optimal treatment option for an individual patient.
In conclusion, the present study aimed to address important gaps in the paediatric PTSD treatment literature about predictors and moderators of outcome in two forms of evidence-based, trauma-focused treatments for paediatric PTSD. Given the limited duration of the significant differential treatment (moderator) effects on PTSD outcomes, and the brevity and large, equal effects of both EMDR therapy and CBWT for paediatric PTSD tied to a single event, the future challenge appears to be on enhancing delivery and dissemination of trauma-focused treatments rather than tailoring them. For future trials investigating moderators it should be considered to include patient subgroups for whom matching of treatment to presentation may be particularly relevant, such as children with PTSD tied to multiple traumas or complex PTSD.
Financial disclosures
Ms de Roos receives income from a published book about EMDR therapy and for training postdoctoral professionals in EMDR. Ms Lucassen and professor van der Oord have received royalties for a published book/book chapters (CBWT) and Ms Lucassen receives income for training postdoctoral professionals in CBWT. Dr Perrin receives income from books/book chapters and workshops on CBT for paediatric PTSD. Professor Emmelkamp and Dr Zijlstra have no conflict of interest. Professor de Jongh receives income from published books/book chapters about EMDR therapy and training postdoctoral professionals in EMDR.
Supplemental Material
Download ()Acknowledgments
The authors thank all the participants and their parents/caretakers, therapists, research assistants, involved mental health departments and all others who contributed to this study.
Supporting information
Additional Supporting Information may be found in the online version of this article:Appendix S1. Table with estimated means in child reported PTSD symptoms pre- and follow-ups for low- and high scoring groups (EMDR therapy and CBWT).
Data availability statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data are not available.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed here.
References
- Alisic, E., Jongmans, M. J., van Wesel, F., & Kleber, R. J. (2011). Building child trauma theory from longitudinal studies: A meta-analysis. Clinical Psychological Review, 31(5), 736–14. doi:10.1016/j.cpr.2011.03.001.
- Alisic, E., & Kleber, R. J. (2010). Measuring posttraumatic stress reactions in children: A preliminary validation of the Children’s Responses to Trauma Inventory. Journal of Child & Adolescent Trauma, 3(3), 192–204. doi:10.1080/19361521.2010.500979.
- Bastien, R. J. B., Jongsma, H. E., Kabadayi, M., & Billings, J. (2020). The effectiveness of psychological interventions for post-traumatic stress disorder in children, adolescents and young adults: A systematic review and meta-analysis. Psychological Medicine, 50(10), 1598–1612. doi:10.1017/S0033291720002007.
- Brown, R. C., Witt, A., Fegert, J. M., Keller, F., Rassenhofer, M., & Plener, P. L. (2017). Psychosocial interventions for children and adolescents after man-made and natural disasters: A meta-analysis and systematic review. Psychological Medicine, 47(11), 1893–1905. doi:10.1017/S0033291717000496.
- Chorpita, B. F., Yim, L., Moffitt, C., Umemoto, L. A., & Francis, S. E. (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research & Therapy, 38(8), 835–855. doi:10.1016/S0005-7967(99)00130-8.
- Cohen, J. A., Mannarino, A. P., & Deblinger, E. (2006). Treating trauma and traumatic grief in children and adolescents. New York, NY: Guilford Press.
- Cuijpers, P. (2019). Targets and outcomes of psychotherapies for mental disorders: An overview. World Psychiatry, 18(3), 276–285. doi:10.1002/wps.20661.
- Danzi, B. A., & La Greca, A. M. (2020). Treating children and adolescents with posttraumatic stress disorder: Moderators of treatment response. Journal of Clinical Child & Adolescent Psychology, 1–7. doi:10.1080/15374416.2020.1823849.
- De Haan, A., Hitchcock, C., Meiser-Stedman, R., Landolt, M. A., Kuhn, I., Black, M. J., … Dalgleish, T. (2021). Efficacy and moderators of efficacy of trauma-focused cognitive behavioural therapies in children and adolescents: Protocol for an individual participant data meta-analysis from randomised trials. BMJ Open, 11(2), e047212. doi:10.1136/bmjopen-2020-047212.
- De Roos, C., Greenwald, R., Den Hollander-Gijsman, M., Noorthoorn, E., Van Buuren, S., & De Jongh, A. (2011). A randomised comparison of cognitive behavioural therapy (CBT) and eye movement desensitisation and reprocessing (EMDR) in disaster-exposed children. European Journal of Psychotraumatology, 2(1), 5694. doi:10.3402/ejpt.v2i0.5694.
- De Roos, C., Van der Oord, S., Zijlstra, B., Lucassen, S., Perrin, S., Emmelkamp, P., & De Jongh, A. (2017). Comparison of eye movement desensitization and reprocessing therapy, cognitive behavioral writing therapy, and wait‐list in pediatric posttraumatic stress disorder following single‐incident trauma: A multicenter randomized clinical trial. Journal of Child Psychology & Psychiatry, 58(11), 1219–1228. doi:10.1111/jcpp.12768.
- Derogatis, L. R. (1992). B51: Administration, scoring and procedures manual-II. Towson, MD: Clinical Psychometric Research.
- DeRubeis, R. J., Cohen, Z. D., Forand, N. R., Fournier, J. C., Gelfand, L. A., & Lorenzo-Luaces, L. (2014). The Personalized Advantage Index: Translating research on prediction into individualized treatment recommendations. A demonstration. PloS One, 9(1), e83875. doi:10.1371/journal.pone.0083875.
- Diehle, J., De Roos, C., Meiser-Stedman, R., Boer, F., & Lindauer, R. J. (2015). The Dutch version of the Child Posttraumatic Cognitions Inventory: Validation in a clinical sample and a school sample. European Journal of Psychotraumatology, 6(1), 26362. doi:10.3402/ejpt.v6.26362.
- Diehle, J., Opmeer, B. C., Boer, F., Mannarino, A. P., & Lindauer, R. J. (2015). Trauma-focused cognitive behavioral therapy or eye movement desensitization and reprocessing: What works in children with posttraumatic stress symptoms? A randomized controlled trial. European Child & Adolescent Psychiatry, 24(2), 227–236. doi:10.1007/s00787-014-0572-5.
- Dorsey, S., McLaughlin, K. A., Kerns, S. E., Harrison, J. P., Lambert, H. K., Briggs, E. C., … Amaya-Jackson, L. (2017). Evidence base update for psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child & Adolescent Psychology, 46(3), 303–330. doi:10.1080/15374416.2016.1220309.
- Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research & Therapy, 38(4), 319–345. doi:10.1016/S0005-7967(99)00123-0.
- Foa, E. B., Chrestman, K., & Gilboa-Schechtman, E. (2008). Prolonged exposure manual for children and adolescents suffering from PTSD. Oxford: Oxford University Press.
- Goldbeck, L., Muche, R., Sachser, C., Tutus, D., & Rosner, R. (2016). Effectiveness of trauma-focused cognitive behavioral therapy for children and adolescents: A randomized controlled trial in eight German mental health clinics. Psychotherapy and Psychosomatics, 85(3), 159–170. doi:10.1159/000442824.
- Greenwald, R. (1999). Eye movement desensitization and reprocessing (EMDR) in child and adolescent psychotherapy. New York, NY: Aronson.
- Gutermann, J., Schreiber, F., Matulis, S., Schwartzkopff, L., Deppe, J., & Steil, R. (2016). Psychological treatments for symptoms of posttraumatic stress disorder in children, adolescents, and young adults: A meta-analysis. Clinical Child & Family Psychology Review, 19(2), 77–93. doi:10.1007/s10567-016-0202-5.
- Hayes, A. F. (2013). Introduction to mediation, moderation and conditional process analysis: A regression-based approach. New York, NY: Guilford Press.
- International Society of Traumatic Stress Studies (ISTSS), (2019). Posttraumatic stress disorder, prevention and treatment guidelines. Retrieved from www.istss.org/clinical-resources/treatingtrauma/new-istss-prevention-and-treatment-guidelines.
- Jaberghaderi, N., Greenwald, R., Rubin, A., Zand, S. O., & Dolatabadi, S. (2004). A comparison of CBT and EMDR for sexually-abused Iranian girls. Clinical Psychology & Psychotherapy, 11(5), 358–368. doi:10.1002/cpp.395.
- Jaberghaderi, N., Rezaei, M., Kolivand, M., & Shokoohi, A. (2019). Effectiveness of cognitive behavioral therapy and eye movement desensitization and reprocessing in child victims of domestic violence. Iranian Journal of Psychiatry, 14(1), 67–75. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6505052/
- Jensen, T. K., Holt, T., Mørup Ormhaug, S., Fjermestad, K. W., & Wentzel-Larsen, T. (2018). Change in post-traumatic cognitions mediates treatment effects for traumatized youth—A randomized controlled trial. Journal of Counseling Psychology, 65(2), 166. doi:10.1037/cou0000258.
- Jensen, T. K., Holt, T., Ormhaug, S. M., Egeland, K., Granly, L., Hoaas, L. C., … Wentzel-Larsen, T. (2014). A randomized effectiveness study comparing trauma-focused cognitive behavioral therapy with therapy as usual for youth. Journal of Clinical Child & Adolescent Psychology, 43(3), 356–369. doi:10.1080/15374416.2013.822307.
- Kane, J. C., Murray, L. K., Cohen, J., Dorsey, S., Skavenski van Wyk, S., Galloway Henderson, J., … Bolton., P. (2016). Moderators of treatment response to trauma‐focused cognitive behavioral therapy among youth in Zambia. Journal of Child Psychology & Psychiatry, 57(10), 1194–1202. doi:10.1111/jcpp.12623.
- Kim, D., Bae, H., & Park, Y. C. (2008). Validity of the subjective units of disturbance scale in EMDR. Journal of EMDR Practice and Research, 2(1), 57–62. doi:10.1891/1933-3196.2.1.57
- Kraemer, H. C. (2016). Messages for clinicians: Moderators and mediators of treatment outcome in randomized clinical trials. American Journal of Psychiatry, 173(7), 672–679. doi:10.1176/appi.ajp.2016.15101333.
- Lane, R. D., Ryan, L., Nadel, L., & Greenberg, L. (2015). Memory consolidation, emotional arousal, and the process of change in psychotherapy: New insights from brain science. Behavioral & Brain Sciences, 38, E1. doi:10.1017/S0140525X14000041.
- Lindebø Knutsen, M., Sachser, C., Holt, T., Goldbeck, L., & Jensen, T. K. (2020). Trajectories and possible predictors of treatment outcome for youth receiving trauma-focused cognitive behavioral therapy. Psychological Trama: Theory, Research, Practice, and Policy, 12(4), 336. doi:10.1037/tra0000482.
- Littel, M., Remijn, M., Tinga, A. M., Engelhard, I. M., & van den Hout, M. A. (2017). Stress enhances the memory-degrading effects of eye movements on emotionally neutral memories. Clinical Psychological Science, 5(2), 316–324. doi:10.1177/2167702616687292.
- Mavranezouli, I., Megnin-Viggars, O., Daly, C., Dias, S., Stockton, S., Meiser-Stedman, R., … Pilling, S. (2020). Psychological and psychosocial treatments for children and young people with post-traumatic stress disorder: A network meta-analysis. Journal of Child Psychology & Psychiatry, 61(1), 18–29. doi:10.1111/jcpp.13094.
- Meiser-Stedman, R., McKinnon, A., Dixon, C., Boyle, A., Smith, P., & Dalgleish, T. (2019). A core role for cognitive processes in the acute onset and maintenance of post-traumatic stress in children and adolescents. Journal of Child Psychology & Psychiatry, 60(8), 875–884. doi:10.1111/jcpp.13054.
- Meiser-Stedman, R., Smith, P., Bryant, R., Salmon, K., Yule, W., Dalgleish, T., & Nixon, R. D. (2009). Development and validation of the Child Post-Traumatic Cognitions Inventory (CPTCI). Journal of Child Psychology & Psychiatry, 50(4), 432–440. doi:10.1111/j.1469-7610.2008.01995.x.
- Moreno-Alcázar, A., Treen, D., Valiente-Gómez, A., Sio-Eroles, A., Pérez, V., Amann, B. L., & Radua, J. (2017). Efficacy of eye movement desensitization and reprocessing in children and adolescent with post-traumatic stress disorder: A meta-analysis of randomized controlled trials. Frontiers in Psychology, 8(1), 1750. doi:10.3389/fpsyg.2017.01750.
- Morina, N., Koerssen, R., & Pollet, T. V. (2016). Interventions for children and adolescents with posttraumatic stress disorder: A meta-analysis of comparative outcome studies. Clinical Psychology Review, 47(7), 41–54. doi:10.1016/j.cpr.2016.05.006.
- National Institute for Health and Clinical Excellence (NICE), (2018). Post-traumatic stress disorder. NG116. Management of PTSD in children, young people and adults (1.6.13). Retrieved from https://www.nice.org.uk/guidance/ng116/chapter/Recommendations
- Nixon, R. D., Sterk, J., & Pearce, A. (2012). A randomized trial of cognitive behaviour therapy and cognitive therapy for children with posttraumatic stress disorder following single-incident trauma. Journal of Abnormal Child Psychology, 40(3), 327–337. doi:10.1007/s10802-011-9566-7.
- Nixon, R. D., Sterk, J., Pearce, A., & Weber, N. (2017). A randomized trial of cognitive behaviour therapy and cognitive therapy for children with posttraumatic stress disorder following single-incident trauma: Predictors and outcome at 1-year follow-up. Psychological Trauma: Theory, Research, Practice & Policy, 9(4), 471–478. doi:10.1037/tra0000190.
- Pfeiffer, E., Sachser, C., de Haan, A., Tutus, D., & Goldbeck, L. (2017). Dysfunctional posttraumatic cognitions as a mediator of symptom reduction in Trauma-Focused Cognitive Behavioral Therapy with children and adolescents: Results of a randomized controlled trial. Behaviour Research and Therapy, 97, 178–182. doi:10.1016/j.brat.2017.08.001.
- Qouta, S. R., Palosaari, E., Diab, M., & Punamaki, R. L. (2012). Intervention effectiveness among war affected children: A cluster randomised controlled trial on improving mental health. Journal of Traumatic Stress, 25(3), 288–298. doi:10.1002/jts.21707.
- Schauer, M., Neuner, F., & Elbert, T. (2017). Narrative exposure therapy for children and adolescents (KIDNET). In M. A. Landolt, M. Cloitre, & U. Schnyder (Eds.), Evidence-based treatments for trauma related disorders in children and adolescents (pp. 227–250). Cham, Switzerland: Springer International Publishing.
- Shapiro, F. (2018). Eye movement desensitization and reprocessing: Basic principles, protocols, and procedures (3rd ed.). New York, NY: Guilford Press.
- Silverman, W. K., & Albano, A. M. (1996). The anxiety disorders interview schedule for children for DSM-IV: Child and parent version. Psychological Corporation.
- Smith, P., Perrin, S., & Yule, W. (2010). Post traumatic stress disorder: Cognitive therapy with children and young people. Abingdon, Oxfordshire, UK: Routledge.
- Taylor, J. E., Graham, R. A., & Weems, C. F. (2015). Moderators and mediators of treatments for youth with traumatic stress. In M. Maric, P. J. M. Prins, & T. H. Ollendick (Eds.), Moderators and mediators of youth treatment outcomes (pp. 41–65). Oxford, UK: Oxford University Press.
- Tinker, R. H., & Wilson., S. A. (1999). Through the eyes of a child: EMDR with children. New York, NY: Norton.
- Trickey, D., Siddaway, A. P., Meiser-Stedman, R., Serpell, L., & Field, A. P. (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review, 32(2), 122–138. doi:10.1016/j.cpr.2011.12.001.
- Van den Hout, M. A., Eidhof, M. B., Verboom, J., Littel, M., & Engelhard, I. M. (2014). Blurring of emotional and non-emotional memories by taxing working memory during recall. Cognition & Emotion, 28(4), 717–727. doi:10.1080/02699931.2013.848785.
- Van der Oord, S., Lucassen, S., Van Emmerik, A. A., & Emmelkamp, P. M. (2010). Treatment of post-traumatic stress disorder in children using cognitive behavioural writing therapy. Clinical Psychology & Psychotherapy, 17(3), 240–249. doi:10.1002/cpp.670.
- Wallace, M. L., Frank, E., & Kraemer, H. C. (2013). A novel approach for developing and interpreting treatment moderator profiles in randomized clinical trials. JAMA Psychiatry, 70(11), 1241–1247. doi:10.1001/jamapsychiatry.2013.1960.
- Wamser-Nanney, R., Scheeringa, M. S., & Weems, C. F. (2016). Early treatment response in children and adolescents receiving CBT for trauma. Journal of Pediatric Psychology, 41(1), 128–137. doi:10.1093/jpepsy/jsu096.
- Weems, C. F., & Scheeringa, M. S. (2013). Maternal depression and treatment gains following a cognitive behavioral intervention for posttraumatic stress in preschool children. Journal of Anxiety Disorders, 27(1), 140–146. doi:10.1016/j.janxdis.2012.11.003.
- Weiss, D. S., & Marmar, C. R. (1997). The impact of event scale-revised. In J. P. Wilson & T. M. Keane (Eds.), Assessing psychological trauma and PTSD: A practitioner’s handbook (pp. 399–411). New York, NY: Guilford Press.
- WHO (2013). Guidelines for the management of conditions that are specifically related to stress. World Health Organization. Retrieved from http://apps.who.int/iris/bitstream/handle/10665/85119/9789241505406_eng.pdf;jsessionid=A87FC4134F1F50FE3F66C587868D2F32?sequence=1