ABSTRACT
Background: Individuals with dissociative identity disorder (DID) have complex symptoms consistent with severe traumatic reactions. Clinicians and forensic assessors are challenged by distinguishing symptom exaggeration and feigning from genuine symptoms among these individuals. This task may be aided by administering validity measures.
Objective: This study aimed to document how individuals with DID score on the Structured Inventory of Malingered Symptomatology (SIMS). The second objective was to compare coached DID simulators and healthy controls to DID patients on the SIMS’s total score and subscales. The third objective was to examine the utility rates of the SIMS in distinguishing simulated DID from clinically diagnosed DID.
Method: We compared SIMS data gathered from participants from two Dutch sites, one Swiss site and one U.S. site. Sixty-three DID patients were compared to 77 coached DID simulators and 64 healthy controls on the SIMS. A multivariate analysis compared the groups on the SIMS total scores and subscales, and post-hoc Games Howell tests and univariate ANOVAs examined differences between the groups. Utility statistics assessed the accuracy of the SIMS in distinguishing clinical from simulated DID.
Results: DID simulators scored significantly higher than DID individuals and healthy controls on every SIMS subscale as well as the total score. The majority (85.7%) of the individuals with DID scored above the cut-off, which is typically interpreted as indicative of possible symptom exaggeration. DID individuals scored higher than the healthy controls on every subscale except Low Intelligence, even after controlling for dissociation. The subscales and items most frequently endorsed by the DID group are consistent with symptoms associated with complex trauma exposure and dissociative reactions. The SIMS total score had a sensitivity of 96% but an unacceptably low specificity of 14%.
Conclusions: The findings indicate that the instrument is not accurate in assessing potential symptom exaggeration or feigning in DID.
HIGHLIGHTS
The malingering screen, Structured Inventory of Malingered Symptomatology (SIMS), cannot accurately distinguish SIMS data collected from DID patients compared to DID feigners.
The items endorsed by the DIDs are consistent with symptoms associated with complex trauma exposure.
Antecedentes: Los individuos con trastorno de identidad disociativo (TID) tienen síntomas complejos consistentes con reacciones traumáticas severas. Los clínicos y evaluadores forenses se enfrentan al reto de distinguir la exageración de los síntomas y la simulación de los síntomas genuinos entre estos individuos. Esta tarea puede verse facilitada por la administración de medidas de validez.
Objetivo: Este estudio tuvo como objetivo documentar la puntuación de los individuos con TID en el Inventario Estructurado de Sintomatología Simulada (SIMS). El segundo objetivo era comparar los simuladores de TID entrenados y los controles sanos con los pacientes de TID en la puntuación total y las subescalas del SIMS. El tercer objetivo fue examinar los índices de utilidad del SIMS para distinguir el TID simulado del TID diagnosticado clínicamente.
Método: Se compararon los datos de la SIMS obtenidos de participantes de dos centros holandeses, un centro suizo y un centro estadounidense. Se compararon 63 pacientes de TID con 77 simuladores de TID entrenados y 64 controles sanos en el SIMS. Un análisis multivariante comparó los grupos en las puntuaciones totales y subescalas de la SIMS, y las pruebas post-hoc de Games Howell y los ANOVAs univariantes examinaron las diferencias entre los grupos. Las estadísticas de utilidad evaluaron la precisión de la SIMS para distinguir el TID clínico del simulado.
Resultados: Los simuladores de TID obtuvieron puntuaciones significativamente más altas que los individuos con TID y los controles sanos en cada subescala del SIMS, así como en la puntuación total. La mayoría (85,7%) de los individuos con TID puntuaron por encima del punto de corte, que suele interpretarse como indicativo de una posible exageración de los síntomas. Los individuos con TID puntuaron más alto que los controles sanos en todas las subescalas excepto en Inteligencia baja, incluso después de controlar la disociación. Las subescalas y los ítems más frecuentemente respaldados por el grupo de TID son consistentes con los síntomas asociados con la exposición al trauma complejo y las reacciones disociativas. La puntuación total del SIMS tuvo una sensibilidad del 96% pero una especificidad inaceptablemente baja del 14%.
Conclusiones: Los resultados indican que el instrumento no es preciso para evaluar la potencial exageración o simulación de los síntomas en el TID.
背景: 患有分离性身份障碍 (DID) 的个体具有与严重创伤反应一致的复杂症状。临床医生和法医评估员面临着区分这些人症状夸大和装病与真实症状的挑战。这项任务可以通过实施有效测量来帮助。
目的: 本研究旨在记录 DID 患者如何在诈病症状学结构化问卷 (SIMS) 上评分。第二个目的是在 SIMS 的总分和分量表上比较训练过的 DID 模拟器和健康对照与 DID 患者。第三个目的是考查 SIMS 在区分模拟 DID 和临床诊断 DID 方面的有效性。
方法: 我们比较了从两个荷兰站点, 一个瑞士站点和一个美国站点参与者中收集的 SIMS 数据。对 63 名 DID 患者与 77 名训练过的 DID 模拟器和 64 名 SIMS 方面的健康对照进行了比较。多变量分析比较了各组的 SIMS 总分和分量表, 事后Games Howell 检验和单变量方差分析考查了各组间差异。有效性统计评估了 SIMS 在区分临床和模拟 DID 方面的准确性。
结果: 在每个 SIMS 分量表以及总分上, DID 模拟器的得分显著高于 DID 个体和健康对照。大多数 (85.7%) DID 个体得分高于临界值, 这通常被解释为可能的症状夸大的迹象。 DID 个体在除低智力外的每个子量表的得分都高于健康对照, 即使在控制了分离之后也如此。 DID 组最常患的分量表和条目x与复杂创伤暴露和分离反应相关症状一致。 SIMS 总分具有 96% 的敏感性, 但令人无法接受的 14% 低特异性。
结论: 结果表明, 此工具在评估 DID 潜在症状夸大或装病方面并不准确。
1. Introduction
Dissociative Identity Disorder (DID) is a disorder characterized by two or more distinct personality states or identities that influence behaviour, accompanied by recurrent amnestic gaps in memory (American Psychiatric Association, Citation2000Footnote1) . Over 95% of these individuals report exposure to early, chronic child maltreatment and adverse early life events, as well as attachment difficulties which has been found to contribute to the development of DID and other trauma-related disorders (Dalenberg et al., Citation2012; Brand et al., Citation2009; Dimitrova et al., Citation2020). Individuals with DID tend to have high scores on many psychological measures’ clinical and validity scales, making it challenging to distinguish genuine versus exaggerated and feigned presentations of DID. Therefore, it is critical that clinicians and forensic assessors have research that guides them in making this distinction.
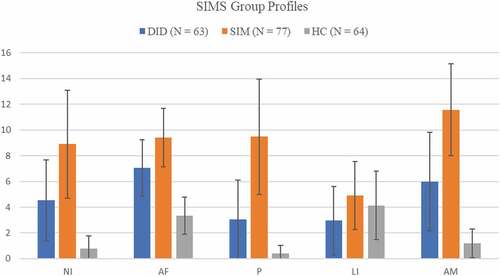
Figure 1. DID = dissociative identity disorder; SIM = simulators; HC = healthy controls; SIMS = Structured Inventory of Malingered Symptoms; NI = neurological impairment; AF = affective disorders; P = psychosis; LI = low intelligence; AM = Amnesia
Unfortunately, few clinicians receive systematic education about developmental trauma, much less dissociation and dissociative disorders (DDs), as part of their training (Henning, Courtois, & Brand, Citation2021; Kumar, Brand, & Courtois, Citation2019; Reinders & Veltman, Citation2020). The lack of training is exacerbated by information about trauma and dissociation in undergraduate and graduate textbooks that is often inadequate, inaccurate, sensationalized, or fails to present a balanced review of research (Brand, Kumar, & McEwen, Citation2019; Reinders & Veltman, Citation2020; Wilgus, Packer, Lile-King, Miller-Perrin, & Brand, Citation2016). Even seasoned clinicians may believe they understand and know how to identify the impacts of trauma, including dissociation, yet many clinicians cannot accurately diagnose DDs when presented with vignettes that describe cases with clear dissociative symptoms (Dorahy et al., Citation2016). Indeed, clinicians may feel quite confident they are correctly diagnosing a traumatized individual, when in fact, they are incorrect (Perniciaro, Citation2015).
2. Symptom exaggeration, feigning, and trauma’s impact
Symptom exaggeration and feigning is a significant concern, particularly in forensic contexts. Due to the high stakes in forensic settings, testing for symptom exaggeration and feigning are a standard part of forensic assessments, although detection is particularly difficult with traumatized individuals because their presentation may appear to be exaggerated due to the complexity and severity of their symptoms (Demakis & Elhai, Citation2011). Some symptoms, including seemingly neurological ones, may be thought to be rare even though they are common among traumatized individuals (Schiavone, McKinnon, & Lanius, Citation2018).
Many tests designed to detect symptom exaggeration and feigning rely on detecting the endorsement of what is deemed to be too many, too unusual, or too severe symptoms (Rogers & Bender, Citation2018). Misclassifying a traumatized person as exaggerating or malingering could cause substantial clinical, psychological, economic, social, vocational, and legal consequences. For example, misclassifying a dissociative person as feigning in a criminal case when they accurately reported their trauma-related symptoms could contribute to more severe sentences. In contrast, if trauma-related symptoms are understood and explained as such they might assist the court in considering the mitigating impact of trauma and result in a less severe sentence or placement where they can receive trauma-informed treatment. [Note that indeed, the United States Supreme Court recently remanded to the Texas Court of Criminal Appeals the case of Terence Tramaine Andrus because his attorneys had not adequately presented the devastating impact of child abuse and neglect on him. The Supreme Court concluded that Andrus had demonstrated the original ‘counsel’s deficient performance’ despite a ‘tidal wave’ of mitigating evidence about the defendant’s abusive childhood (Terence Tramaine Andrus v. Texas, 202, p.18).]
Many people, including possibly judges and juries, may have preconceived ideas about individuals with DID due to stigmatizing stereotypes reinforced by movies such as Split that portray them as aggressive and threatening (Brand & Pasko, Citation2017). Individuals attempting to feign DID on psychological testing may endorse stereotypes about these individuals that are not supported by science. A study comparing the items endorsed by 67 DID simulators to those of 53 DID patients on the Minnesota Multiphasic Personality Inventory-2 (MMPI-2) found that simulators endorsed sociopathic, sadistic, and paranoid items, suggesting this is how they perceive people with DID (Brand et al., Citation2016). Feigners were 50 times more likely than DID individuals to say it would be helpful to discard almost all laws and 46 times more likely to indicate they enjoyed hurting people they love. This level of misunderstanding of DID individuals indicates that they may face prejudicial and unfounded bias in assessment, treatment, and legal proceedings. It would rightfully be considered racist if such stereotypes were drawn on the basis of skin colour. On the other hand, not detecting malingered DID could result in unwarranted use of treatment resources and/or disability payments or escaping just legal consequences. Errors in either direction have serious ramifications and need to be avoided. Therefore, research that illuminates how to distinguish exaggerated and feigned from clinical DID is critical.
Tests of symptom exaggeration have generally not been created with sensitivity to the impact of trauma. Many tests include symptoms that are supposedly rare yet are common among traumatized and/or dissociative groups. For example, DID individuals endorse items that are supposedly infrequent on the MMPI-2, yet the endorsed items describe symptoms or problems that are common among traumatized and/or dissociative individuals (see Brand et al., Citation2016). Similarly, other measures have unacceptably low specificity (i.e. the proportion of genuine individuals a test accurately identifies as not feigning) with DID, including the Trauma Symptom Inventory-2 (Palermo & Brand, Citation2018), and the Structured Interview of Reported Symptoms (SIRS) although the SIRS-based Trauma Index and the SIRS-2 show adequate specificity (SIRS/SIRS-2; Brand, McNary, Loewenstein, Kolos, & Barr, Citation2006; Brand, Tursich, Tzall, & Loewenstein, Citation2014; Rogers, Payne, Correa, Gillard, & Ross, Citation2009) as does the Test of Memory Malingering (Brand, Webermann, Snyder, & Kaliush, Citation2019), and the SCID-D-R (Mychailyszyn, Brand, Webermann, Şar, & Draijer, Citation2020) with this group.
The Structured Inventory of Malingered Symptomatology (SIMS, Widows & Smith, Citation2005) is a screen for malingering that has not yet had its specificity examined in DID individuals. The SIMS has five subscales including Amnesia (AM), Affective Disorders (AF), Psychosis (P), Neurological Impairment (NI), and Low Intelligence (LI). People with DID often struggle with experiences that may be misinterpreted as exaggerated yet are consistently documented including amnesia, hearing voices, neurological-sounding symptoms such as unexplained shifts in body sensation and temperature, and psychoform inability to move, as well as mood disturbances (Loewenstein, Frewen, & Lewis-Fernández, Citation2017). Items related to these experiences are included in the SIMS, making it likely that individuals with DID may endorse so many items that they score higher than the cut-off of 14 points that indicates possible malingering (Widows & Smith, Citation2005).
One study compared individuals with DID (n = 17) to patients with PTSD and healthy controls on the SIMS (Vissia et al., Citation2016). The DID group scored higher than the PTSD and controls on total score as well as all subscales except Low Intelligence. Affective Disorders was the highest score, followed by Amnesia and Neurological Impairment subscales in the DID group. The DID group did not differ significantly from the PTSD group on Affective Disorders, suggesting that endorsement of affective items could be related to trauma exposure rather than exaggeration. The study was limited by small groups and the authors did not calculate the SIMS’ utility statistics.
Another important reason to study the SIMS in DID is that some authors claim that DID patients’ high SIMS scores indicate that they are prone to symptom exaggeration and fantasy proneness (Merckelbach et al., Citation2015). However, individuals with diagnosed DID have been shown to not be more suggestible, fantasy prone or vulnerable to creating false memories than are healthy controls or individuals with PTSD (Vissia et al., Citation2016). Interestingly, it was found that, “Dissociativity correlated with symptom over-reporting in the student samples, but not in the clinical sample (emphasis added, p. 165, Merckelbach et al., Citation2015). Merckelbach, Boskovic, Pesy, Dalsklev, and Lynn (Citation2017) subsequently suggested that the correlation between SIMS scores and dissociation could be due to many SIMS items overlapping with trauma-related symptoms although this conclusion is often overlooked by those who argue that those high dissociation over-report their symptoms (see discussion of these omissions in Dalenberg, Brand, Loewenstein, Frewen, & Spiegel, Citation2020).
Some individuals with genuine, severe psychopathology score high on the SIMS (Peters, Jelicic, Moritz, Hauschildt, & Jelinek, Citation2013). Thirty percent of patients diagnosed with schizophrenia scored above a cut-off of 16; the SIMS scores correlated with symptoms of schizophrenia including hallucination and distress, even when controlling for demographic variables (all rs > .44; Peters et al., Citation2013). This raises the question of how individuals with DID, who have a wide range of serious trauma-related psychopathology (e.g. Rodewald, Wilhelm-Gößling, Emrich, Reddemann, & Gast, Citation2011), will perform on the SIMS. But researchers have yet to compare the SIMS total and subscale scores of DID individuals to DID simulators.
The current study does just that and compares the SIMS scores of diagnosed DID to those of simulating DID and healthy controls. The first objective of this study was to document the SIMS total score, subscales and items endorsed by a large, international group of individuals with DID and investigate how many participants score above the SIMS’ total score cut-off. It was hypothesized that the most frequently endorsed subscales and items would be related to symptoms associated with DDs, specifically subscales related to amnesia, mood, psychosis, and neurological symptoms; furthermore, we hypothesized that these subscales would correlate with dissociation for the DID group but not the other groups. The second objective was to compare coached DID simulators and healthy controls to DID individuals on the SIMS’s total score and subscales. It was hypothesized that DID individuals would score higher than the controls but lower than the simulators on the total score and subscales. The third objective was to examine the SIMS’ utility rates for distinguishing simulated from clinical DID. It was hypothesized that the SIMS would have a low specificity rate.
3. Methods
3.1. Participants
3.1.1. DID participants
A total of 63 DID participants were gathered from four sites: Baltimore, Maryland, USA, Amsterdam and Groningen in the Netherlands, and Zurich, Switzerland. The thirty-one participants from Maryland were recruited from a psychiatric hospital unit specializing in treating trauma and outpatient private practices with therapists who have expertise in treating trauma patients (see for details: Palermo & Brand, Citation2018). Therapists were notified of the study through listservs and email announcements; in turn, they notified patients with DID about the possibility of participating in the study. Fifteen Swiss DID individuals were recruited from outpatient practices of clinicians who are trained in treating trauma and dissociative patients (see for details: Schlumpf et al., Citation2013, Citation2014). Seventeen DID individuals were recruited from mental health care institutions and via advertisements on Internet forums in the Netherlands (see for details:; Vissia et al., Citation2016).
Inclusion criteria included: having a diagnosis of DID given by the inpatient team or outpatient therapist, being 18 or older, having at least an eighth-grade reading level, and being able to engage in the study without becoming distressed (as determined by the clinicians). Each potential participant was given the Structured Clinical Interview for DSM-IV Dissociative Disorders-Revised (SCID-D-R; Steinberg, Citation1994) by the first author, or either a postdoctoral fellow or research assistant trained in conducting the SCID-D-R, and supervised by the first author, to ensure that they met criteria for DID. No patients were excluded due to any comorbid psychiatric disorder. All of the Dutch and Swiss patients had current (90.6%) or remitted (9.4%) PTSD; PTSD was not assessed in the U.S. sample. Patients with a traumatic brain injury were excluded.
DID participants ranged from 19–63 years old (M = 42.89, SD = 11.05) and almost all (n = 60, 95.2%) were female. The sample was primarily White (93.7%, n = 59), while 4.8% (n = 3) were African American, 1.6% (n = 1) were Hispanic/Latinx, and none were Asian, biracial or ‘other’. The sample varied in terms of education, with just over half (50.8%) having completed college. Relationship status varied: 39.7% (n = 25) were single, 38.1% (n = 24) were married, and 19.0% (n = 12) were divorced.
3.1.2. Simulated DID participants
Ninety college students were recruited from a research pool at a university in Maryland, USA. They were informed they were to simulate having DID while taking a variety of psychological tests, and that they did not need to behaviourally act as if they had the disorder. Inclusion criteria included being at least 18 years of age and scoring below 30 on the Dissociative Experiences Scale (DES, Bernstein & Putnam, Citation1986). Scores of 30 or higher on the DES may indicate a DD (Bernstein & Putnam, Citation1986); 13 participants (14.4%) were removed due to their high DES score, leaving 77 DID simulators. Ages ranged from 18–58 (M = 21.40, SD = 5.28), with 61 (79.2%) identifying as female and 16 (20.8%) as male. The majority were White (n = 52, 67.5%), 11 (14.3%) were of African American, 4 (5.2.%) were Asian American, 4 (5.2%) were Hispanic/Latinx, 5 (6.5%) were biracial, and 1 (1.3%) was ‘other’. Simulated DID participants were primarily single (93.5%, n = 72).
3.1.3. Healthy controls
Sixty-four healthy individuals from three sites (Amsterdam and Groningen, the Netherlands, and Zurich, Switzerland) participated. Some of the healthy participants from both countries were recruited via acting schools and platforms for actors because, after the data used in this study was collected, they were instructed to simulate DID. However, in the present study, all actors reported data about themselves prior to engaging in simulation; thus, they are included in the healthy control group. Healthy Swiss participants (n = 37) were recruited through advertisements posted at a university, on internet platforms where actors seek performance opportunities, and through word of mouth. They were informed they would participate in a project investigating neural reactions to a variety of cognitive tasks. The 27 Dutch controls were recruited from acting schools, through the internet, magazines, and newspapers whereas others were recruited from the general population and informed they would participate in a study investigating autobiographical memory processing in the brain. The healthy control’s mean age was 39.64 years (SD = 11.50) and varied from 21–62 years-old; all were female andWhite. The majority of controls had some college (n = 49, 76.6%) and almost evenly split between being single (48%) and being married or living with a partner.
3.2. Measures
3.2.1. Dissociative experiences scale
The Dissociative Experiences Scale (DES; Bernstein & Putnam, Citation1986) was used to screen simulated DID participants for a possible DD. At the Swiss site, the German version of the DES was used (Spitzer et al., Citation1998), while the Dutch version (Boon & Draijer, Citation1995) was used in the Netherlands. At the U.S. site, participants with an average score above 30 were removed to safeguard against the possibility that the simulator had a DD, while the Netherlands site used a cut-off of 25 and Swiss site used a cut-off of 15. The Netherlands excluded controls who scored high on somatoform dissociation, traumatic experiences, alcohol or drug abuse, neurological, or mental illness in the past or present. The Swiss controls were excluded if they had PTSD and/or major depression.
3.2.2. Structured inventory of malingered symptoms
The Structured Inventory of Malingered Symptoms (SIMS; Smith & Burger, Citation1997) is a 75-item self-report measure designed to screen for symptom feigning in five categories: Neurological Impairment (NI), Psychosis (P), Low Intelligence (LI), Affective Disorders (AF), and Amnesia (AM). Individuals respond with ‘yes’ or ‘no’ to the items, which are then added to create an sum ranging from 0 to 75. Scores exceeding 14 are interpreted as indicative of overreporting. The Swiss site used the German version of the SIMS (Cima et al., Citation2003) and the Dutch site used the Dutch version (Merckelbach & Smith, Citation2003).
3.3. Procedure
The data used in this study was collected as part of larger studies which explored the detection of genuine versus simulated DID. The study was approved by institutional review boards at the collection sites. Participants signed informed consent forms before participating.
Participants with DID completed a variety of tests and interviews, which took between three to five hours. The American DID sample was given a $20 gift card when they began the study and received another $20 gift card at the conclusion. The Swiss participants were compensated with 80 Swiss Francs upon completion. The compensation of the Dutch participants varied depending on the time involved in their participation; the maximum was 100 Euros.
DID simulators received extra credit in a psychology course. They were informed that the best simulator each semester would win $50 (see Palermo & Brand, Citation2018 for details).
3.4. Statistical analyses
We first investigated the percentage of participants per group that scored higher than a cut-off of 14. Correlations between the SIMS total scores and subscales and the DES were conducted within each group. The total SIMS scores for the groups were compared with a between-subjects one-way ANOVA followed by post hoc Games Howell tests. A Kruskal Wallis H test was performed to account for skewed data. A MANOVA compared groups’ subscale scores, followed by univariate ANOVAs and post hoc Games Howell tests. An ANOVA compared groups’ DES scores. Because dissociation may influence subscale scores, an ANCOVA and a MANCOVA controlled for DES mean when examining the SIMS subscales. Utility statistics were calculated to determine how well the SIMS can distinguish diagnosed from simulated DID. All analyses were conducted using Statistical Package for the Social Sciences (SPSS), version 27.
4. Results
Our first finding is that 85.7% of the individuals with DID scored higher than the cut-off of 14, while 96.1% of simulators and 12.5% of the healthy control group exceeded the cut-off. Groups’ SIMS total score differed, F(2,201) = 191.22, p = < .001, η2 = .66. Post hoc Games Howell comparisons revealed that simulators (M = 44.38, SD = 13.37) scored higher than DID participants (M = 23.59, SD = 11.03, p < .001), and healthy controls (M = 9.89, SD = 4.58, p < .001). The latter two groups also differed significantly, p < .001. Mean and standard deviation were similar in all groups as indicated by a Kruskal-Wallis H test.
A main effect of group on the SIMS subscales was found, Wilks’ λ = .21, F(10,394) = 46.46, p < .001, η2p = .54. Follow-up analyses showed that simulators scored higher than individuals with genuine DID on every subscale (p < .001 on all subscales) and higher than healthy controls on all subscales (p < .001) except Low Intelligence (See ). Significant differences were found between the DID group and healthy controls, in which DID patients scored higher than controls on all subscales (p < .001) except the Low Intelligence subscale (p = .034). shows the means and standard deviations for subscales.
Table 1. DES and SIMS descriptives for total score and subscales
A main effect of group for DES was found, F(2,200) = 231.74 p < .001, η2 = .70. The DID group reported higher DES (M = 43.76, SD = 17.92) than simulators (M = 15.63, SD = 15.09), p < .001, and healthy controls (M = 4.61, SD = 3.67), p < .001. The simulators’ DES score also differed from healthy controls (p < .001).
Correlations between the SIMS total scores and subscales and the DES were significant for the DID group. Specifically, there were significant associations between the DES and SIMS total score (r = .35, p = .006), Amnesia (r = .295, p = .02), Psychosis (r = .297, p = 019), and Neurological Impairment (r = .49, p < .001). DES and SIMS correlations were not significant for the controls and simulators.
When controlling for dissociative symptoms using the DES scores and comparing the groups’ SIMS subscale scores, significant differences on every subscale were found (p < .001), except for the LI subscale. When examining the groups’ total SIMS score using the DES scores as a covariate no relationship was found, F(1,199) = 3.29, p = .071. However, after controlling for DES score, SIMS scores were predicted by group status, F(2,199) = 193.68, p < .001.
Utility statistics based on the SIMS total score predictions are in and indicate that 59% of the participants were correctly classified. The SIMS had a sensitivity of 96%, but a very low specificity of 14%.
Table 2. Utility statistics for SIMS total score based on DID status
5. Discussion
In the current study we sought to: characterize the Structured Inventory of Malingered Symptomatology (SIMS) profiles of individuals with DID using a large, international sample; to learn which subscales and items would be most frequently endorsed; and to determine if the DID group’s SIMS scores could be distinguished from those of coached DID simulators and healthy controls. Our first finding is that 85.7% of the individuals with DID scored higher than the cut-off of 15 that has been suggested to indicate potential malingering. As predicted, dissociation was significantly related to the DID group’s SIMS total score, as well as to their scores on the Amnesia, Psychosis and Neurological Impairment subscales, yet these relationships were insignificant for the other groups. Our second finding was, as predicted, that the DID group scored significantly lower than coached simulators (M = 44.38, SD = 13.37), and significantly higher (M = 23.59, SD = 11.03) than healthy controls (M = 9.89, SD = 4.58) on the total scores as well as every subscale except Low Intelligence, even when controlling for the relationships between dissociation and the subscales. Last, we found that the SIMS had an extremely low specificity rate of 14%. That is, the test overclassifies individuals with DID as exaggerating. It therefore does not prove to be a valid screening measure for symptom exaggeration in this disorder.
The inability of the SIMS to discriminate simulated from clinical DID, and the likely dissociative and trauma-related nature of the endorsements by individuals with DID, as supported by the significant correlations between the SIMS total scores and subscales and the DES for the DID group only, call into question the conclusions of the theorists who argue that, on the basis of SIMS data, individuals with DID exaggerate their symptoms (e.g. Merckelbach et al., Citation2017). Our study is part of a growing literature that links elevations in measures designed to assess symptom exaggeration and dissociation, childhood abuse, and, especially with PTSD comorbidity. This research indicates that great caution should be used in interpreting validity scales as indicative of exaggeration or feigning among traumatized individuals, particularly in the context of reported childhood trauma and/or high dissociative symptoms, unless the measures have been validated with these groups (Elhai, Gold, Mateus, & Astaphan, Citation2001; Klotz Flitter, Elhai, & Gold, Citation2003).
Examining the SIMS’ individual items endorsed helps clarify if the endorsements could be exaggerations or related to dissociative reactions and/or trauma exposure. The items most frequently endorsed by the DID group (see Supplemental Online Table 3) occurred on the four subscales, that is, Affective Disorders, Amnesia, Neurological Impairment, and Psychosis, that are consistent with decades of research about the diagnostic criteria and associated features of DID. The DID group scored the highest on AF subscale with high endorsements of items relating to sleeping difficulty (endorsed by 82% of the patients). Sleep disruptions could be related to either depression and/or PTSD, both of which are ubiquitous in DID (Boon & Draijer, Citation1993; Brand et al., Citation2009; Putnam, Guroff, Silberman, Barban, & Post, Citation1986; Dimitrova et al., Citation2020). DID individuals also frequently endorsed having low energy (84%) and going to bed to avoid feeling depressed (57%). The DID group’s second highest subscale score was directly related to the diagnostic criteria for DID, that is, amnesia: 67% endorsed having difficulty remembering the date; 60% endorsed sometimes forgetting how to drive to their home and forgetting more than three times a day what they were in the process of doing; and 41% endorsed having major problems with memory and having entire days they could not recall. These are classic symptoms associated with DID that have been documented for decades (e.g. Putnam et al., Citation1986). The third highest subscale among the DID group was Neurological Impairment, that is, neurological-like symptoms, followed by psychotic-like symptoms. Notably, research shows that symptoms similar to temporal lobe epilepsy and psychotic-like symptoms are common among individuals with trauma-related disorders (e.g. Schiavone et al., Citation2018). Many seemingly neurological symptoms are conceptualized as somatoform dissociative symptoms and are associated with PTSD symptoms and with cumulative traumatization, particularly bodily threat (Nijenhuis, Spinhoven, van Dyck, Van Der Hart, & Vanderlinden, Citation1998; Nijenhuis, Van Der Hart, Kruger, & Steele, Citation2004). Some of these symptoms were endorsed by the majority of the DID individuals including 59% reported their sense of smell had changed and 51% reported that on a weekly basis they suddenly feel cold even though the temperature was warm. Similarly, they endorsed items on the Psychosis subscale quite frequently. For example, 49% reported they began to hear voices suddenly and 44% reported the voices they hear have not stopped since they began. Up to 90% of people diagnosed with DID report hearing voices, almost always beginning before age 18 and continuing throughout adulthood (Dorahy et al., Citation2009). Thus, endorsing these items is consistent with this disorder. Furthermore, voice hearing is strongly associated with trauma and stress (e.g. Dorahy et al., Citation2009). Many of the most frequently endorsed SIMS items are most likely related to phenomena associated with having a DD and/or exposure to trauma, rather than exaggeration or feigning. In support of this conclusion, all the European DID participants were diagnosed with comorbid PTSD; unfortunately, comorbidity was not assessed in the U.S. sample.
The pattern of subscale elevations among the DID group replicates prior research (Vissia et al., Citation2016). Although affective, amnesia, neurological, and psychotic symptoms may be rare in some psychiatric groups, this wide range of symptoms is well-documented and common among individuals with DID (Boon & Draijer, Citation1993; Brand & Chasson, Citation2015; Putnam et al., Citation1986). The DID group’s lack of elevation on Low Intelligence is consistent with research showing that DID patients have average intelligence (Armstrong, Citation1994).
This is the first study to assess the SIMS utility statistics in DID individuals. A strength of the study is that it used data gathered from three international sites to discern if simulated DID and controls could be distinguished from DID patients. This strength was balanced by using a simulation design that relied on students from one study centre rather than people known to be feigning DID at each participating centre. Another limitation is that the DID patients were predominantly middle-aged, well educated, and almost entirely White women. Future research should recruit a more diverse sample of DID patients, and, if possible, a group of known DID feigners.
In conclusion, this study found that the majority of DID patients scored sufficiently high on the SIMS to be categorized as possibly exaggerating symptoms. However, the DID group’s highest scores were on the Affective Disorders, Amnesia, Neurological Impairment, and Psychosis subscales; their most frequently endorsed items were consistent with the broad range of symptoms found in individuals who have experienced chronic trauma, particularly those with DDs. These findings suggest that the SIMS is not a valid instrument for assessing symptom exaggeration in individuals that meet criteria for DID. Considerable caution should therefore be used in interpreting the SIMS as indicative of exaggeration among traumatized individuals, particularly those with dissociative reactions. Additional trauma-informed guidance about measures that are valid for distinguishing malingering from clinical DID is needed. Thus far, the Test of Memory Malingering (Brand et al., Citation2019), the Dissociative Experiences Scale-Revised (Katz et al., Citation2020), and the SCID-D-R (Mychailyszyn et al., Citation2020) have shown utility in differentiating simulated from clinical DID.
Data availability
Due to the sensitive nature of the data, the ethics review committee did not approve sharing the data online. Requests for data can be sent to the first author.
Supplemental Material
Download ()Acknowledgments
This report represents independent research part funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. A.A.T.S. Reinders was supported by the Netherlands Organization for Scientific Research (www.nwo.nl), NWO-VENI grant no. 451-07-009. The authors would like to thank all the participants and their therapists.
Disclosure statement
The authors have no conflicts of interest.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
Notes
1. Diagnostic criteria for the DDs were updated in the DSM-5. Because data collection began prior to the introduction of the DSM-5, DSM-IV criteria and diagnoses are utilized in this study.
References
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (Text Revision) (4 ed.). Washington , DC: American Psychiatric Press.
- Armstrong, J. G. (1994). Reflections on multiple personality disorder as a developmentally complex adaptation. Psychoanalytic Study of the Child, 49(1), 349–10. doi:10.1080/00797308.1994.11823068
- Bernstein, E. M., & Putnam, F. W. (1986). Development, reliability, and validity of a dissociation scale. Journal of Nervous and Mental Disease, 174(12), 727–735. doi:10.1097/00005053-198612000-00004
- Boon, S., & Draijer, N. (1993). Multiple personality disorder in the Netherlands: A clinical investigation of 71 patients. American Journal of Psychiatry, 150, 489–494.
- Boon, S., & Draijer, N. (1995). Screening en diagnostiek van dissociatieve stoornissen. Lisse: Swets & Zeitlinger.
- Brand, B. L., Chasson, G. S., Palermo, C. A., Donato, F. M., Rhodes, K. P., & Voorhees, E. F. (2016). MMPI-2 item endorsements in dissociative identity disorder vs. simulators. The Journal of the American Academy of Psychiatry and the Law, 44(1), 63–72 https://pubmed.ncbi.nlm.nih.gov/26944745/.
- Brand, B. L., & Chasson, G. S. (2015). Distinguishing simulated from genuine dissociative identity disorder on the MMPI-2. Psychological Trauma: Theory, Research, Practice, and Policy, 7(1), 93–101. doi:10.1037/a0035181
- Brand, B. L., Kumar, S. A., & McEwen, L. E. (2019). Coverage of child maltreatment and adult trauma in graduate psychopathology textbooks. Psychological Trauma: Theory, Research, Practice, and Policy. doi:10.1037/tra0000454.supp. (Supplemental)
- Brand, B. L., McNary, S. W., Loewenstein, R. J., Kolos, A. C., & Barr, S. R. (2006). Assessment of genuine and simulated dissociative identity disorder on the structured interview of reported symptoms. Journal of Trauma & Dissociation, 7(1), 63–85. doi:10.1300/J229v07n01_06
- Brand, B. L., Tursich, M., Tzall, D., & Loewenstein, R. J. (2014). Utility of the SIRS-2 in distinguishing genuine from simulated dissociative identity disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 6(4), 308–317. doi:10.1037/a0036064
- Brand, B. L., Webermann, A. R., Snyder, B. L., & Kaliush, P. R. (2019). Detecting genuine and simulated dissociative identity disorder with the test of memory malingering. Psychological Trauma: Theory, Research, Practice & Policy, 11(5), 513–520. doi:10.1037/tra0000405
- Brand, B., Classen, C., Lanius, R., Loewenstein, R., McNary, S., Pain, C., & Putnam, F. (2009). A naturalistic study of dissociative identity disorder and dissociative disorder not otherwise specified patients treated by community clinicians. Psychological Trauma: Theory, Research, Practice, and Policy, 1(2), 153–171. doi:10.1037/a0016210
- Brand, B., & Pasko, D. (2017). Split is based on myths about dissociative identity disorder. PsycCRITIQUES, 62(18). doi:10.1037/a0040801
- Cima, M., Hollnack, S., Kremer, K., Knauer, E., Schellbach-Matties, R., Klein, B., & Merckelbach, H. (2003). “Strukturierter Fragebogen Simulierter Symptome “Die deutsche Version des Structured Inventory of Malingered Symptomatology: SIMS. Nervenarzt, 74(11), 977–986. doi:10.1007/s00115-002-1438-5
- Dalenberg, C. J., Brand, B. L., Gleaves, D. H., Dorahy, M. J., Loewenstein, R. J., Cardena, E., … Spiegel, D. (2012). Evaluation of the evidence for the trauma and fantasy models of dissociation. Psychological Bulletin, 138(3), 550–588. doi:10.1037/a0027447
- Dalenberg, C. J., Brand, B. L., Loewenstein, R. J., Frewen, P. A., & Spiegel, D. (2020). Inviting scientific discourse on traumatic dissociation: Progress made and obstacles to further resolution. Psychological Injury and Law, 13(2), 135–154. doi:10.1007/s12207-020-09376-9
- Demakis, G. J., & Elhai, J. D. (2011). Neuropsychological and psychological aspects of malingered posttraumatic stress disorder. Psychological Injury and Law, 4(1), 24–31. doi:10.1007/s12207-011-9099-y
- Dimitrova, L., Fernando, V., Vissia, E. M., Nijenhuis, E. R. S., Draijer, N., & Reinders, A. A. T. S. (2020). Sleep, trauma, fantasy and cognition in dissociative identity disorder, post-traumatic stress disorder and healthy controls: A replication and extension study. European Journal of Psychotraumatology, 11(1), 1. doi:10.1080/20008198.2019.1705599
- Dorahy, M. J., Lewis-Fernández, R., Krüger, C., Brand, B. L., Şar, V., Ewing, J., … Middleton, M. (2016). The role of clinical experience, diagnosis, and theoretical orientation in the treatment of posttraumatic and dissociative disorders: A vignette and survey investigation. Journal of Trauma & Dissociation. doi:10.1080/15299732.2016.1225626
- Dorahy, M. J., Shannon, C., Seagar, L., Corr, M., Stewart, K., Hanna, D., … Middleton, W. (2009). Auditory hallucinations in dissociative identity disorder and schizophrenia with and without a childhood trauma history: Similarities and differences. Journal of Nervous and Mental Disease, 197(12), 892–898. doi:10.1097/NMD.0b013e3181c299ea
- Elhai, J. D., Gold, S. N., Mateus, L. F., & Astaphan, T. A. (2001). Scale 8 elevations on the MMPI-2 among women survivors of childhood sexual abuse: Evaluating posttraumatic stress, depression, and dissociation as predictors. Journal of Family Violence, 16(1), 47–57. doi:10.1023/A:1026576425986
- Henning, J. A., Courtois, C. A., & Brand, B. L. (2021). Graduate training and certification in trauma treatment for clinical practitioners. Advance online publication. Training and Education in Professional Psychology. doi:10.1037/tep0000326
- Katz, R. R., Thompson, K. J., Ortiz, M., Duncan, N., Abu-Rus, A., & Dalenberg, C. J. (2020, August 6- 9). Replication and improvement of the validity scale for the dissociative experiences scale-revised. Poster presentation APA 2020 Convention, Washington DC.
- Klotz Flitter, J. M., Elhai, J. D., & Gold, S. N. (2003). MMPI-2 F scale elevations in adult victims of child sexual abuse. Journal of Traumatic Stress, 16(3), 269–274. doi:10.1023/A:1023700208696
- Kumar, S., Brand, B. L., & Courtois, C. A. (2019). The need for trauma training: Clinicians’ reactions to training on complex trauma. Psychological Trauma: Theory, Research, Practice, and Policy. doi:10.1037/tra0000515
- Loewenstein, R. J., Frewen, P. A., & Lewis-Fernández, R. (2017). Dissociative disorders. In B. J. Sadock, V. A. Sadock, & P. Ruiz (Eds.), Kaplan & Sadock’s comprehensive textbook of psychiatry (Vol. 1, 10th ed., pp. 1866–1952). Philadelphia, PA: Wolters Kluwer/ Lippincott Williams & Wilkens.
- Merckelbach, H., Boskovic, I., Pesy, D., Dalsklev, M., & Lynn, S. J. (2017). Symptom overreporting and dissociative experiences: A qualitative review. Consciousness and Cognition: An International Journal, 49, 132–144. doi:10.1016/j.concog.2017.01.007
- Merckelbach, H., Giesbrecht, T., van Heugten-van der Kloet, D., de Jong, J., Meyer, T., & Rietman, K. (2015). The overlap between dissociative symptoms and symptom over-reporting. The European Journal of Psychiatry, 29(3), 165–172. doi:10.4321/S0213-61632015000300001
- Merckelbach, H., & Smith, G. P. (2003). Diagnostic accuracy of the Structured Inventory of Malingered Symptomatology (SIMS) in detecting instructed malingering. Archives of Clinical Neuropsychology, 18(2), 145–152. doi:10.1093/arclin/18.2.145
- Mychailyszyn, M. P., Brand, B. L., Webermann, A. R., Şar, V., & Draijer, N. (2020). Differentiating dissociative from non-dissociative disorders: A meta-analysis of the structured clinical interview for DSM dissociative disorders (SCID-D). Journal of Trauma & Dissociation. doi:10.1080/15299732.2020.1760169
- Nijenhuis, E. R. S., Spinhoven, P., van Dyck, R., Van Der Hart, O., & Vanderlinden, J. (1998). Degree of somatoform and psychological dissociation in dissociative disorder is correlated with reported trauma. Journal of Traumatic Stress, 11(4), 711–730. doi:10.1023/A:1024493332751
- Nijenhuis, E. R. S., Van Der Hart, O., Kruger, K., & Steele, K. (2004). Somatoform dissociation, reported abuse and animal defence-like reactions. Australian and New Zealand Journal of Psychiatry, 38(9), 678–686. doi:10.1111/j.1440-1614.2004.01441.x
- Palermo, C. A., & Brand, B. L. (2018). Can the trauma symptom inventory-2 distinguish coached simulators from dissociative disorder patients? Psychological Trauma: Theory, Research, Practice, and Policy. doi:10.1037/tra0000382
- Perniciaro, L. A. (2015). The influence of skepticism and clinical experience on the detection of dissociative identity disorder by mental health clinicians. p. 75. ProQuest Information & Learning, US.
- Peters, M. J. V., Jelicic, M., Moritz, S., Hauschildt, M., & Jelinek, L. (2013). Assessing the boundaries of symptom over-reporting using the Structured Inventory of Malingered Symptomatology in a clinical schizophrenia sample: Its relation to symptomatology and neurocognitive dysfunctions. Journal of Experimental Psychopathology, 4(1), 64–77. doi:10.5127/jep.023811
- Putnam, F. W., Guroff, J. J., Silberman, E. K., Barban, L., & Post, R. M. (1986). The clinical phenomenology of multiple personality disorder: A review of 100 recent cases. Journal of Clinical Psychiatry, 47, 285–293 https://pubmed.ncbi.nlm.nih.gov/3711025/.
- Reinders, A. A. T. S., & Veltman, D. J. (2020). Dissociative identity disorder: Out of the shadows at last? British Journal of Psychiatry, 1–2. doi:10.1192/bjp.2020.168
- Rodewald, F., Wilhelm-Gößling, C., Emrich, H. M., Reddemann, L., & Gast, U. (2011). Axis-I comorbidity in female patients with dissociative identity disorder and dissociative identity disorder not otherwise specified. Journal of Nervous and Mental Disease, 199(2), 122–131. doi:10.1097/NMD.0b013e318208314e
- Rogers, R., & Bender, S. D. (2018). Clinical assessment of malingering and deception (4th ed.). New York, NY: The Guilford Press.
- Rogers, R., Payne, J. W., Correa, A. A., Gillard, N. D., & Ross, C. A. (2009). A study of the SIRS with severely traumatized patients. Journal Of Personality Assessment, 91(5), 429–438. doi:10.1080/00223890903087745
- Schiavone, F. L., McKinnon, M. C., & Lanius, R. A. (2018). Psychotic-like symptoms and the temporal lobe in trauma-related disorders: Diagnosis, treatment, and assessment of potential malingering. Chronic Stress, 2, 247054701879704. doi:10.1177/2470547018797046
- Schlumpf, Y. R., Nijenhuis, E. R. S., Chalavi, S., Weder, E. V., Zimmermann, E., et al. (2013). Dissociative part-dependent biopsychosocial reactions to backward masked angry and neutral faces: An fMRI study of dissociative identity disorder. Neuroimage: Clinical, 3, 54–64.
- Schlumpf, Y. R., Reinders, A. A. T. S., Nijenhuis, E. R. S., Luechinger, R., Van Osch, M. J. P., Jäncke, L., & Chao, L. (2014). Dissociative part-dependent resting-state activity in dissociative identity disorder: A controlled fMRI perfusion study. PLoS One, 9(6), 1–15. doi:10.1371/journal.pone.0098795
- Smith, G. P., & Burger, G. K. (1997). Detection of malingering: Validation of the Structured Inventory of Malingered Symptomatology (SIMS). Journal of the American Academy of Psychiatry and the Law, 25(2), 183–189 https://pubmed.ncbi.nlm.nih.gov/9213290/.
- Spitzer, C., Freyberger, H. J., Stieglitz, R. D., Carlson, E. B., Kuhn, G., Magdeburg, N., & Kessler, C. (1998). Adaptation and psychometric properties of the German version of the dissociative experience scale. Journal of Traumatic Stress, 11(4), 799–809. doi:10.1023/A:1024457819547
- Steinberg, M. (1994). The Structured Clinical Interview for DSM-IV dissociative disorders-revised (SCID-D-R). Washington, D.C.: American Psychiatric Press.
- Vissia, E. M., Giesen, M. E., Chalavi, S., Nijenhuis, E. R. S., Draijer, N., Brand, B. L., & Reinders, A. A. T. S. (2016). Is it trauma- or fantasy-based? Comparing dissociative identity disorder, post-traumatic stress disorder, simulators, and controls. Acta Psychiatrica Scandinavica, 134(2), 111–128. doi:10.1111/acps.12590
- Widows, M. R., & Smith, G. P. (2005). Structured Inventory of Malingered Symptomatology. Lutz, Florida: PAR.
- Wilgus, S. J., Packer, M. M., Lile-King, R., Miller-Perrin, C. L., & Brand, B. L. (2016). Coverage of child maltreatment in abnormal psychology textbooks: Reviewing the adequacy of the content. Psychological Trauma: Theory, Research, Practice, & Policy, 8(2), 188–197. doi:10.1037/tra0000049
