ABSTRACT
Background: Complex Trauma (CT) is a term used to refer to multiple or prolonged traumatic experiences. Such experiences are often first encountered during childhood and may impact key developmental periods. CT is a risk for a broad range of deleterious physical, psychological, social, and occupational outcomes. The diagnosis of Complex Posttraumatic Stress Disorder (C-PTSD) has been proposed to capture the symptomatology resulting from CT exposure.
In Australia, there are few publicly funded services that target, and are purposely designed to support, the mental health needs of young people with symptoms of complex post-traumatic stress (C-PTSD). The Tern Programme has been designed as a purpose-built model of care for providing mental health support to young people with C-PTSD.
Methods: This implementation trial will involve a longitudinal examination of Tern participants for a fixed 24-month period. Participants will be recruited from the young people referred to Tern at headspace centres in regional Australia where Tern operates. Eligible participants will have reported a history of complex trauma, and present with symptoms of C-PTSD. All participants will be invited to complete a series of surveys during their participation in the programme. Survey items will assess C-PTSD symptom change, quality of life and occupational functioning.
The Tern model of care is delivered in a semi-structured format to accommodate a person-centred flexible approach. Fidelity will be monitored through the completion of a clinician post-session checklist and through group supervision.
Discussion: This study will provide the first quantitative data on the new Tern model of care and evaluate mental health and functional outcomes of its participants. If effective, Tern may be suitable for replication in other Australian or international youth mental health services where complex post-traumatic stress is prevalent.
Trial Registration: Australia and New Zealand Clinical Trials Registry (ANZCTR): ACTRN12621000079842p. Prospectively registered on 29 January 2021.
Abbreviations: CT = Complex Trauma; C-PTSD = Complex Posttraumatic Stress Disorder
HIGHLIGHTS
Tern represents a new model of care incorporating a flexible, person-centred approach to C-PTSD treatment whilst providing for the complex needs of young people as well as the wellbeing of the staff delivering the intervention.
Antecedentes: El trauma complejo (TC) es un término que se utiliza para referirse a experiencias traumáticas múltiples o prolongadas. A menudo, estas experiencias se encuentran por primera vez durante la infancia y pueden afectar períodos clave del desarrollo. El TC es un riesgo para una amplia gama de secuelas perjudiciales físicas, psicológicas, sociales y ocupacionales. Se ha propuesto el diagnóstico de trastorno de estrés postraumático complejo (TEPT-C) para capturar la sintomatología resultante de la exposición al TC. En Australia existen pocos servicios financiados con fondos públicos dirigidos a las necesidades de salud mental de los jóvenes con síntomas de estrés postraumático complejo (TEPT-C) y que estén específicamente diseñados para respaldarlos. El Programa Tern ha sido diseñado como un modelo de atención especialmente orientado para brindar apoyo de salud mental a los jóvenes con TEPT-C.
Métodos: Esta implementación implicará un examen longitudinal de los participantes del programa Tern durante un período fijo de 24 meses. Los participantes serán reclutados entre los jóvenes derivados al programa Tern en los centros de referencia en la región de Australia donde opera Tern. Los participantes elegibles informarán un historial de trauma complejo y presentarán síntomas de TEPT-C. Se invitará a todos los participantes a completar una serie de encuestas durante su participación en el programa. Los ítemes de la encuesta evaluarán el cambio en los síntomas de TEPT-C, la calidad de vida y el funcionamiento ocupacional. El modelo de atención Tern se ofrece en un formato semiestructurado para adaptarse a un enfoque flexible centrado en la persona. La fidelidad se controlará mediante la realización de una lista de verificación posterior a la sesión por parte del clínico y mediante supervisión grupal.
Discusión: Este estudio proporcionará los primeros datos cuantitativos sobre el nuevo modelo de atención Tern, y evaluará la salud mental y resultados funcionales de sus participantes. Si es eficaz, el programa Tern puede ser adecuado para su reproducción en otros servicios de salud mental para jóvenes australianos o internacionales donde prevalece el estrés postraumático complejo.
Registro de Ensayo Clínico: Australia and New Zealand Clinical Trials Registry (ANZCTR): ACTRN12621000079842p. Registrado prospectivamente el 29 de enero del 2021.
背景: 复杂性创伤 (CT) 是一个用于指代多次或长期创伤经历的术语。这些经历通常是在童年期首次遭遇, 可能影响关键的发展时期。 CT 会导致多种有害的身体, 心理, 社会和职业后果。已提出复杂性创伤后应激障碍 (C-PTSD) 的诊断来刻画 CT 暴露引起的症状。
在澳大利亚, 很少有公共资助针对且为有复杂性创伤后应激 (C-PTSD) 症状年轻人心理健康需求设计的服务。 Tern 计划旨在为患有 C-PTSD 的年轻人提供量身打造的心理健康支持护理模式。
方法: 该试行实验将包含一项对固定 24 个月期间 Tern 参与者的纵向考查。参与者将从施行Tern 的澳大利亚偏远地区顶空中心的年轻人中招募。符合条件的参与者将报告复杂性创伤史及C-PTSD 症状表现。将邀请所有参与者在参与该计划期间完成一系列调查。调查条目将评估 C-PTSD 症状变化, 生活质量和职业功能。
Tern 护理模式以半结构化形式提供, 以适应以人为本的灵活方法。精确性将通过完成临床医生会后检查表和小组监督来监控。
讨论: 本研究将提供首个有关新 Tern 护理模式并评估参与者心理健康和功能结果的定量数据。如果有效, Tern 可能适合在其他普遍存在复杂性创伤后应激的澳大利亚或国际青年心理健康服务中复制。
实验注册: 澳大利亚和新西兰临床试验注册中心 (ANZCTR):ACTRN12621000079842p。预计于 2021 年 1 月 29 日注册。
1. Background
Complex Trauma (CT), when used as a clinical formulation term, refers to both the nature of traumatic experiences, as well as the myriad of mental and physical effects that may result from traumatic experiences (Cook, Blaustein, Spinazola, & van der Kolk, Citation2003; John et al., Citation2019). When referring to traumatic history, CT typically refers to experiences of trauma that have been multiple or prolonged, where escape may have been prohibited and/or the trauma was perpetrated by persons supposed to provide safety such as parents (Lawson, Citation2017). Examples of CT include physical or sexual abuse, neglect, torture, and domestic, intimate or community violence. CT experiences in young people may increase the risk for developing difficulties in one or several domains of functioning including attachment, physical health, affect regulation, dissociation, behavioural control, cognition, and self-concept (Beal et al., Citation2019; Berto et al., Citation2017; Cook et al., Citation2005). These seven domains attest to a further feature in CT presentations; that young people may present with widely differing needs and meet diagnostic criteria for various conditions beyond post-traumatic stress disorder (Cook et al., Citation2005; John et al., Citation2019; Spinazzola et al., Citation2005; van der Kolk, Citation2005).
While adulthood is traditionally defined as being 18 years or older in many countries, the definition of ‘youth’ tends to vary. The World Health Organization (WHO) defines adolescence (10–19 years), youth (15–24 years) and young people (10–24 years) separately (World Health Organisation, Citation2021). In Australia, the term ‘young people’ is used to refer to those aged 12–24 years, slightly shorter in range that used by the WHO (Australian Institute of Health and Welfare, Citation2021). Traditionally, Australian state mental health services have operated with a clear distinction between child (17 years or younger) and adult (18 years and older) and implemented services in this dichotomous fashion. As emerging adulthood (18–25 years) has become recognized as a distinct developmental period (Arnett, Citation2000), Australian youth services have begun to reorient and broaden in scope (McGorry et al., Citation2007). The extension to an upper limit of 25 years follows evidence suggesting that brain development is not concluded until this age, and that a vast majority of mental health conditions first emerge by the 25th year of life (Arain et al., Citation2013; Solmi, Radua, Olivola, Croce, & Soardo, Citation2021). In the context of this study, the terms youth and young person (young people) are used to refer to individuals aged 12–25.
It has been estimated that between 56% and 75% of adult Australians have been exposed to at least one potentially traumatic event during their lifetime (Mills et al., Citation2011). International estimates indicate that as many as 61% of young people have experienced at least one potentially traumatic event by the age of 16, and the likelihood of exposure is significantly higher for young females (McLaughlin et al., Citation2013). One Australian study interviewed 162 families presenting to a state-funded child and youth mental health service and observed that 69% of clients had experienced at least one potentially traumatic event; however, it was noted that experiences of at least three or more Adverse Childhood Experiences (ACE) were commonly reported (Reay et al., Citation2015). Through efforts to more broadly define differing traumatic experiences, ACEs refer not only to traditionally traumatic events (such as exposure to violence or sexual assault) but also to experiences such as living in poverty, being neglected, bullied, or losing a primary caregiver (Felitti et al., Citation1998).
While ACEs do not always satisfy traditional definitions of ‘trauma’, their presence have yet been linked to the development and severity of psychopathology, including post-traumatic stress amongst youth (Goldenson, Kitollari, & Lehman, Citation2021). Recent research has posed a complex relationship between ACEs and post-traumatic stress. Findings suggest that protective environmental factors (such as positive peer relationships and secure attachment) and that individual factors (such as emotion regulation skills) may mediate the relationship between the experience of ACEs and the development of posttraumatic stress (Cloitre et al., Citation2019; Karatzias et al., Citation2020). In summary, evidence is mounting to indicate that a larger number of situations and events than previously considered may ultimately be experienced as traumatic.
Whilst researchers have endeavoured to continue expanding trauma typology, efforts have also been directed to define the resultant mental health sequelae. In recent years there have been several attempts to standardize CT diagnostic nosology, with the expressed purpose of reaching expert agreement on matters of definition, best-practice treatment, and research. The diagnosis of Complex Posttraumatic Stress Disorder (C-PTSD) has been proposed and subsequently adopted by the International Classification of Diseases (ICD-11) (World Health Organisation, Citation2018). This diagnosis of C-PTSD requires the presence of post-traumatic stress symptoms (re-experiencing, hypervigilance, and avoidance) and three domains adopted from the CT literature; affect dysregulation, difficulties in close relationships and negative self-concept (Maercker et al., Citation2013). As the diagnosis of C-PTSD is relatively new, research is continuing to assess the validity of the construct in youth populations (Perkonigg et al., Citation2016; Sachser et al., Citation2017). What has been learned from adult prevalence studies is that CPTSD is observed in relatively higher frequency than its sister diagnosis of PTSD (up to 61% for CPTSD and 25% for PTSD) in clinical populations (Cloitre et al., Citation2018; Vallières et al., Citation2018). As interpersonal adversity is commonly experienced amongst those with mental health issues, it has been suggested that rates of CPTSD may be high amongst psychiatric populations generally (Møller, Augsburger, Elklit, Søgaard, & Simonsen, Citation2020).
Several treatment guidelines have been published to guide the delivery and implementation of interventions for CT in adults (Internation Society for Traumatic Stress Studies (Citationn.d.); Kezelman & Stavropoulos, Citation2012, Citation2019a, Citation2019b). Research specific to the young person population is developing and informing adaptation of treatment guidelines; however, these remain less comprehensive than current treatment guidelines for adults (International Society for Traumatic Stress Studies (Citationn.d.); National Child Traumatic Stress Network, Citationn.d., Orygen, Citation2018). Nonetheless, there is a clear consensus across adult and young person treatment guidelines that treatments must be multidimensional, tailored to the individual, and address key symptom areas of post-traumatic stress, affect regulation and relational functioning. These recommendations differ to those of traditional PTSD treatments. In cases of single trauma exposure (PTSD), emphasis is placed on early, direct memory exposure as the primary ingredient for change (American Psychological Association, Citation2017; Phoenix Australia, Citation2021). Alternatively, as CPTSD has been defined to reflect additional symptoms of affect regulation, difficulties in interpersonal relationship and negative self-concept, more research is needed to determine whether simply applying existing PTSD treatments to CPTSD is sufficient, or if new methods of intervention are necessary to achieve change in these additional areas of concern.
Expert consensus has recommended that CT interventions follow a ‘phased’ structure with client safety and self-regulation skills prioritized before the use of exposure-based techniques for addressing traumatic memory (Cloitre et al., Citation2011). However, this recommendation has been criticized due to lack of evidence, which has led to a new area of investigation regarding the true benefits of delaying exposure methods in the treatment of CT (Cloitre, Citation2015; de Jongh et al., Citation2016; van Vliet, Huntjens, van Dijk, & de Jongh, Citation2018). Further studies are required to clarify the circumstances in which phased interventions are/are not of benefit – particularly for young people. In saying this, the phased vs. not phased contention promotes a simplified dichotomy of intervention. Followed too resolutely this may jeopardize the individuality of CT patients and their experiences. It is intended that the current project will make an important contribution to this area of research through examining outcomes of a treatment model that offers and accommodates both phased and exposure-first methods, dependent on the symptom profile and goals of the individual.
1.1. Mental health access for young people in regional areas
Access to specialist mental healthcare in regional and rural areas is an internationally recognized problem (Caxaj, Citation2016; Cyr, Etchin, Guthrie, & Benneyan, Citation2019; Morales, Barksdale, & Beckel-Mitchener, Citation2020). Common factors contributing to this issue include lack of funding, appropriate staffing, stigma towards mental health disorders and limits to adapting urban treatment approaches to the regional setting (Wainberg et al., Citation2017). In Australia, regional and rural districts employ significantly lower rates of mental health professionals per capita compared to metropolitan areas (National Rural Health Alliance Inc, Citation2017; Rural Doctors Association, Citation2018). The issue of access is further compounded when matters of demand are considered. Recent data from the United States shows that youth in rural locations are 1.29 times greater risk of exposure to four or more ACE experiences compared to urban youth (Calthorpe & Pantell, Citation2021). Australian police and health data has indicated that individuals who live outside major cities are 1.4 times more likely to report having experienced any form of partner violence, and domestic violence-related hospitalizations are 24 times more likely in remote and very remote areas (Australian Institue of Health and Welfare, Citation2019). In combination, this information suggests that regional Australians are both a) at increased risk to experience interpersonal trauma and b) less able to access-appropriate support services.
Young people in Australia have limited options for accessing publicly funded CT intervention programs. Access to mental healthcare in Australia is provided predominantly through primary healthcare as part of the Medicare Benefits Scheme (MBS). This system allows young people to access 10–20 psychotherapy sessions with a suitably qualified health professional following referral from a general practitioner (Department of Health, Citation2019). Alternatively, young people may access mental healthcare through state-funded hospital services; however, these services typically have high-threshold entry criteria that excludes many young people from receiving adequate support Orygen (Citationn.d.). Further, services that are provided either by MBS primary healthcare or state-funded hospitals are not specific to CT. This means that access to latest best-practice care may not be equitably available across districts. A single, transferable model of care designed for the Australian context is therefore indicated as a gap in service provision.
1.2. Aims
As Tern is a new model of care, best-practice dictates that formal feasibility and implementation studies are precursors to a randomized controlled clinical trial. The aim of this study is to provide a quantitative, evidence-based evaluation of Tern as a real-world clinical model of care. It is hypothesized that young people who receive Tern will report reductions in symptoms of complex post-traumatic stress whilst reporting increased levels of occupational activity and improved quality of life.
Recruitment for this study commenced in June 2021. This study is funded by the CQUniversity Elevate Scholarship which is co-contributed to by Northern Australia Primary Health Limited (NAPHL) and CQUniversity under an industry partnership agreement. The CQUniversity Human Research Ethics Committee has approved this research (CQU HREC 0000022729), which has been registered with the Australia and New Zealand Clinical Trials Registry (ACTRN12621000079842p).
2. Methods/design
2.1. Tern Programme
Tern is a long-term, semi-structured and multi-component psychosocial model of care for youth aged 12–25 years with histories of complex trauma. This intervention programme is primarily designed to provide treatment for Complex Posttraumatic Stress Disorder (C-PTSD); however, it has a deliberately broad scope to facilitate provision of care for other CT sequelae such as dissociative disorders and borderline personality disorder. Tern is long-term to accommodate anticipated issues of engagement, re-traumatization, and lapses in recovery.
Development of the model followed an inductive process. Initial inspection of youth access data from headspace centres (community mental health outpatient clinics for Australian youth; (McGorry et al., Citation2007)) in regional Australia (Townsville and Mackay), together with anecdotal reporting from staff and young people about strengths and barriers in accessing mental health in these regions, provided preliminary insight into service problems. Simultaneous to this investigation, a comprehensive review of research regarding best-practice was conducted and recommendations were used to inform the development of Tern (Chanen et al., Citation2008; Cohen, Mannarino, Kliethermes, & Murray, Citation2012; Cook et al., Citation2003; Fraser, MacKenzie, & Versnel, Citation2017; International Society for Traumatic Stress Studies (Citationn.d.); Orygen, Citation2018; Siehl, Robjant, & Crombach, Citation2020). The Blue Knot Foundation, Australia’s national centre for excellence for CT, provided the foundational structures and core guiding treatment principles upon which Tern. was designed (Briere & Scott, Citation2014; Courtois & Ford, Citation2009; Fisher, Citation2018; Ford, BAvd, Herman, & Courtois, Citation2020; Kezelman & Stavropoulos, Citation2012, Citation2019a, Citation2019b; Porges & Dana, Citation2018; Rothschild, Citation2011; Schwarz, Corrigan, Hull, & Raju, Citation2016; Van der Kolk, Citation2014). Psychotherapy components were chosen for inclusion based on their consistency with C-PTSD symptom areas of 1) post-traumatic stress, 2) affect dysregulation, 3) negative self-concept, and 4) interpersonal difficulties (Maercker et al., Citation2013).
Tern has been designed to represent a model of best practice mental healthcare young people with complex trauma histories, and so incorporates various components in addition to psychotherapeutic treatment. There are four key components of Tern:
2.1.1. Psychotherapy
This is an evidence-based psychotherapeutic model drawing from the current treatment guidelines for interventions for complex trauma (Cook et al., Citation2003; International Society for Traumatic Stress Studies (Citationn.d.); Internation Society for Traumatic Stress Studies (Citationn.d.); Kezelman & Stavropoulos, Citation2012, Citation2019a, Citation2019b; Orygen, Citation2018). Intervention components include psychoeducation, cognitive therapy, somatic and affect regulation skills, behavioural activation, narrative and imaginal exposure, psychodynamic techniques, and supportive techniques, such as problem-solving and coaching (Chanen et al., Citation2008; Cohen et al., Citation2012; Fraser et al., Citation2017; Siehl et al., Citation2020). The Tern intervention model is semi-structured and is broadly defined as including four distinct phases of care, with differing treatment components within each phase. An abridged description of each phase is described in . It is important to note that that duration of phases is not prescribed, and only proposed to maximize the individualized nature of each intervention under Tern.
Table 1. Phases of Tern model of care
Intervention components will be delivered to greater or lesser extent as required by the young person. Length of individual psychotherapy sessions may range from 50 to 90 minutes. Session length is determined on a case-by-case basis according to individual need and is moderated around engagement and the safe provision of exposure and grounding techniques (Kezelman & Stavropoulos, Citation2019a). Psychotherapy will be delivered in weekly, one-on-one sessions. The government funding granted for Tern affords young people a 24-month window to access and engage as needed (from the time of their initial appointment). The benefit of this timeframe will allow for young people to engage flexibly, where matters of attendance and living circumstances (such as transport) can be accommodated.
The treatment programme will be tailored to each young person and will be required to be reviewed after every 10 sessions of intervention. Twice weekly sessions are provided where issues of disengagement or risk warrants more intensive support. It is anticipated that participants with PTSD or overall subthreshold symptoms will receive a significantly shorter intervention, and indeed may skip entire phases, compared to young people with all CPTSD symptom domains.
2.1.2. Tern skills group (Psychoeducation group)
Young people aged 16–25 years will be eligible to participate in a structured, five-week psychoeducational group programme at any point during their engagement in Tern. The decision to provide the group only for those aged 16–25 years was made due to 1) the need to develop a set of materials deliverable to a minimum level of cognitive development, 2) prioritization of safety by not exposing the youngest clients to the trauma narratives of older clients, and 3) the availability of appropriately skilled staff. Participants aged 12–15 who would potentially benefit from a group programme are referred to external group programs designed for their age and developmental stage.
Group sessions are 60 minutes in duration. Group programme content includes trauma psychoeducation, somatic regulation skills, sleep hygiene, mindfulness, healthy eating, and physical activity scheduling. These topics are consistent with traditional ‘Phase 1’ interventions for CT where psychoeducation and basic emotional regulation skills are recommended as early treatment targets (Cook et al., Citation2003; International Society for Traumatic Stress Studies (Citationn.d.); International Society for Traumatic Stress Studies (Citationn.d.); Kezelman & Stavropoulos, Citation2012, Citation2019a, Citation2019b; Orygen, Citation2018).
2.1.3. Limited case management
This component refers to non-traditional psychotherapy tasks aimed at improving the young person’s broader health and environmental circumstances. Staff are afforded additional time to undertake necessary treatment planning, referral writing, and advocacy tasks with (or on behalf of) the young person. For example, arranging and attending a meeting with school staff to implement a return-to-school programme.
2.1.4. Therapist supports
Staff in the programme are provided with fortnightly, two-hour group supervision while they are providing Tern intervention services. Clinical review is a rolling element of each session, with additional optional components including programme development, reflective supervision and continuing professional development opportunities. Numerous past researchers have examined the negative relationship between providing mental health support to individuals with CT histories and practitioner wellbeing factors, such as vicarious trauma and compassion fatigue (Ben-Porat & Itzhaky, Citation2009; Craig & Sprang, Citation2010; Newell, Nelson-Gardell, & MacNeil, Citation2016; VanDeusen & Way, Citation2006; Way, VanDeusen, MartIn, Applegate, & Jandle, Citation2004). This data serves as the justification to assertively provide for practitioner supervision and support in the Tern model of care. describes the components of the group supervision process.
Table 2. Group supervision components
2.2. Study setting
Tern will be conducted at two regional youth community mental health centres in Queensland, Australia: headspace Townsville and headspace Mackay. The ‘headspace Centre’ model of youth mental healthcare has been adopted nationally and is funded by the Australian Federal Government Department of Health (McGorry et al., Citation2007). Core objectives of the headspace model are to overcome issues of access for young people, and to provide a youth-friendly, no- or low-cost integrated mental health service within the space of primary healthcare. Interested readers are directed to Rickwood et al. (Rickwood et al., Citation2019) for a full discussion of the headspace model and history.
Headspace centres were originally designed as providers of early intervention for mild-to-moderate mental health presentations; however, in recognition of the increased needs for intervention services for moderate-to-severe youth mental health presentations (sometimes referred to as the ‘missing middle’), additional government funding has been granted to select centres to implement enhanced intervention programmes. Observational data from the two headspace centres in Townsville and Mackay indicated that histories of complex trauma were frequently observed in the highest-needs youth. Further, in both locations there were no alternative specialized intervention programmes that could accommodate the complex mental health needs of these young people (Northern Australia Primary Health Limited, Citation2017).
Headspace centres were identified as suitable locations to operate Tern as they possessed the existing youth-friendly infrastructure, referral base, and inter-agency connections desired for this programme. Within each of these centres, Tern operates as a co-located mental health service that integrates directly across existing headspace programs, as well as with local state mental health services. Staff who deliver Tern participate in shared clinic reviews with other headspace programme staff and receive the same clinical governance and oversight as other programmes within the centres.
2.3. Participants
Tern was deliberately developed to complement existing mental health service infrastructure in Australia. As headspace was the chosen setting, Tern was designed to service the same cohort already managed by the headspace centre programme. Participants in Tern will be young people aged 12–25 years who present at either headspace Townsville or Mackay for services. As Tern is already operational at both sites, young people currently receiving services under Tern as well as newly referred Tern clients will all be invited to participate in the research project. G*Power was used to conduct a power analysis which indicated that between 29 and 84 participants would be required to detect a medium-to-large effect size for correlation between variables such as treatment dosage and primary outcomes (Faul, Erdfelder, Albert-Georg, & Buchner, Citation2007). Based on previous referral data, it is anticipated that between 50 and 70 young people will participate in the study during the data collection period.
2.4. Inclusion and exclusion criteria
All young people referred to headspace Townsville and Mackay are screened for Tern eligibility criteria and, if meeting criteria, subsequently offered this intervention model. In addition, each referred young person is then invited to participate in the study, unless exclusion criteria have been met. Should a young person decline to participate in the study, they are still eligible to receive Tern.
Eligibility for services in Tern is defined by evidence of CT and endorsement of post-traumatic stress symptoms. Interpersonal traumatic history and associated adversity will be assessed using the Revised ACE Questionnaire (Finkelhor, Shattuck, Turner, & Hamby, Citation2015) in conjunction with a semi-structured clinical interview that is part of routine assessment in headspace Centres. Triage staff at both Townsville and Mackay received additional training in screening for CT and C-PTSD by the principal author. In addition to a trauma history, young people must also present with features of C-PTSD. Screening of post-traumatic symptoms will be assessed using age-appropriate administration of either the Child Adolescent Trauma Screen (Sachser et al., Citation2017) or the Posttraumatic Stress Disorder Checklist (Blevins, Weathers, Davis, Witte, & Domino, Citation2015) in conjunction with the clinical interview. Participants who have endorsed one or more interpersonal traumatic event/s (e.g. physical or sexual abuse) and met the clinical cut-off on the age-appropriate measure (21 or higher for CATS/33 or higher for PCL-5) and subjectively described these traumas during their triage interview will be referred to Tern. Further clinical assessments will be conducted at commencement of intervention in Tern (see ‘Outcome Measures’ section).
Tern situates within the headspace model of care, which adopts the principal of early intervention. For this reason, participants are not required to have an existing diagnosis or meet full-threshold for C-PTSD. Where presentation is sub-clinical, referral into the programme is conditional upon 1) impact on functioning, where impaired functioning is determined by degree of reduction in occupational activity and/or frequency of self-harm or suicidal behaviour, and 2) limited availability of alternative mental health programs to adequately support the young person.
To best represent real-world clinical practice, exclusion criteria have been limited to factors that may impact research participation, specifically – completion of the required surveys and/or participation in the informed consent process (e.g. individuals with reduced capacity as a result of intellectual or language impairment). Young people who present with symptoms of psychosis are not excluded from Tern; however, individuals who present with active psychosis or who satisfy criteria for At Risk Mental State are priority referred to an appropriate state-health service for treatment. These individuals may be re-assessed for Tern once their psychotic illness has been appropriately managed. Determination of the presence of psychotic features will be undertaken by headspace triage staff prior to referral to Tern. However, given the potential duration of the Tern intervention, it is possible that a young person may develop psychosis during their care. In these instances, the responsible Tern practitioner would be responsible for referring the participant to an appropriate specialist service and discharging them from Tern.
Participants undergoing concurrent pharmacotherapy are permitted entry regardless of whether this has been stabilized prior to enrolment. As part of their general mental healthcare it is anticipated that Tern participants may commence or discontinue psychiatric medicines during this trial, as indicated by clinical decision-making and referral to appropriate medical practitioners. Participants will not be permitted to undertake concurrent psychotherapeutic treatment whilst engaging in Tern.
2.5. Suicide risk management
It is anticipated that participants in this programme will present with varying degrees of suicidal ideation and/or behaviour. Management of suicidal crises will be in accordance with existing practice guidelines and clinical escalation policies in place at headspace Townsville and Mackay. Participants experiencing suicidal ideation are typically supported to create safety plans, engage with and inform trusted caregivers or friends and may receive a temporary increase in face-to-face therapeutic contact. Where risk is acute, participants will be referred and transported to a local hospital for review and consideration for admission. Should a participant be hospitalized during their treatment under Tern, the participant is not automatically discharged. Their Tern practitioner will work in partnership with acute services during the crisis, continuing to provide therapy or advocacy services as required.
2.6. Staffing
Tern will be delivered by mental health professionals with i) a minimum undergraduate degree in psychology, social work, or occupational therapy, and ii) a minimum of two years of mental health intervention experience. Operational funding for the programme, provided by the North Queensland Primary Health Network, is limited to 2.0 FTE employees for Townsville and Mackay, respectively. All staff will be provided with a minimum of three days training in foundational skills for the assessment and treatment of C-PTSD, followed by an additional training session in the Tern model of care. Training and assessment of intervention competencies will be overseen by the principal investigator (BJD).
2.7. Treatment fidelity
Staff will be invited to complete a purpose-built fidelity checklist at the end of every session delivered. This checklist will be used promote fidelity to the Tern intervention components and provide overall summary data of type and frequency of intervention components delivered over the span of the study. Fidelity will also be monitored through the fortnightly group supervision process, overseen by the principal investigator (BJD). In the event a fidelity breach is observed, the practitioner involved will be provided with individual supervision to support them to continue delivering the Tern model of care.
2.8. Participant dropout
Observations from adult-focused literature indicate that dropout amongst patients with post-traumatic stress is common and is highest amongst those who received trauma-focused treatments (Imel, Laska, Jakupcak, & Simpson, Citation2013; Lewis, Roberts, Gibson, & Bisson, Citation2020). Equivalent research is less exhaustive for youth; however, there is some evidence indicating that retaining youth in treatment is also challenging (de Haan, Boon, de Jong, Hoeve, & Vermeiren, Citation2013; Wamser-Nanney, Citation2019). Tern has been explicitly designed to anticipate and accommodate engagement issues for CT youth with flexibility around attendance times and missed appointments. Young people are exited from the programme if they make no contact over a three month period, or if they fail to attend three consecutive appointments and do not respond to a letter requesting they re-engage. Prior to being exited from Tern, each young person’s case is presented at supervision for review and confirmation that it is appropriate to make no further attempts at engagement.
2.9. Outcome measures
As the symptoms of C-PTSD have only been recently defined, to our knowledge no single outcome tool for assessing complex post-traumatic symptoms in teenagers and young adults has yet been designed and tested. For this reason, existing measures of posttraumatic stress, affect dysregulation, and interpersonal and identity issues, have been selected based upon published precedence to support their use. The primary outcomes for this trial will be measured as change in the four symptoms of CPTSD: 1) post-traumatic stress, 2) affect regulation, 3) interpersonal difficulties, and 4) disturbance in self-concept. The secondary outcomes of this project will include quality of life, time spent in occupational activity and use of psychiatric emergency services.
Given the broad age range of participants (12–25 years), the Child and Adolescent Trauma Screen (CATS; (Sachser et al., Citation2017)) and the Post-traumatic Stress Disorder Checklist (PCL-5; (Blevins et al., Citation2015)) have been chosen to monitor core PTSD symptomatology of re-experiencing, hypervigilance and avoidance for 12–17 and 18–25 year old participants, respectively. The Borderline Personality Disorder Checklist (BPD-47; (Bloo, Arntz, & Schouten, Citation2017)) has been chosen to monitor C-PTSD symptoms of affect dysregulation, interpersonal issues, and negative self-concept for all participants. The BPD-47 has previously been used for this purpose with a cohort of young people (Hendriks et al., Citation2017). Trauma history type and number of experiences will be recorded through the Revised Adverse Childhood Experiences Scale (Finkelhor et al., Citation2015), which has been selected in recognition of the potential for events beyond actual or threatened death or sexual assault to contribute to the development of posttraumatic stress (Pai, Suris, & North, Citation2017).
In addition to C-PTSD symptom outcome measures, data about living circumstances, occupational functioning, quality of life and use of psychiatric emergency services, will be collected. According to accepted definitions of mental illness, impact on occupational, social, or other major activity must be present (American Psychiatric Association, Citation2013). Further, previous research has observed that histories of CT may be associated with poorer occupational or educational outcomes (Currie & Spatz Widom, Citation2010). The decision to evaluate quality of life was made to include a strengths-based perspective of recovery and allow for analysis of relationships between functioning, quality of life and symptom severity. The Youth Quality of Life Short Form (YQOL-SF; (Patrick, Edwards, & Topolski, Citation2002)) and the World Health Organization Quality of Life Short Form (WHOQOL-BREF; (The WHOQOL Group, Citation1998)) were chosen to evaluate quality of life for participants aged 12–17 years and 18–25 years, respectively. Extent of occupational activity and frequency of use of psychiatric emergency services will be recorded through a demographic questionnaire.
2.10. Data collection processes
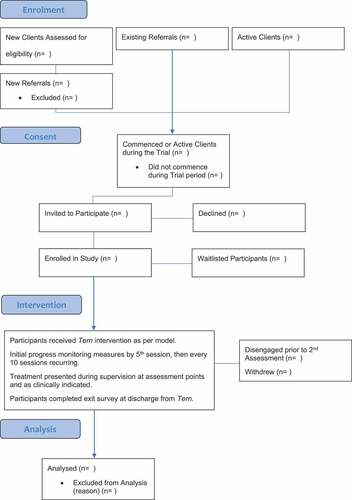
Data will be collected over a fixed 24-month period between June 2021–2023. As Tern is an active programme, both existing clients (those who have already received one or more sessions of support under Tern) and clients who have not yet commenced the programme will be invited to participate. Clients who have already commenced their intervention will be invited to complete the first progress monitoring survey within their next scheduled assessment point. Total number of sessions to date will also be recorded at that point. Tern practitioners will be responsible for conducting the informed consent for their clients as well as facilitating the completion of study surveys. displays the intended participant flow.
Following the initial screening process (see section on ‘Inclusion and Exclusion Criteria’ above), prospective participants are referred to Tern and invited to participate in the study. For young people aged 12–15 consent will be sought by parents/legal guardians and assent will be sought from the young person. For young people aged 14–15, and where no suitable/safe parent/legal guardian is available, these young people will be assessed for mature minor status and permitted to self-consent if satisfied. Mature minor status, sometimes termed as Gillick Competence, is granted to a person under the age of 18 where they can demonstrate sufficient insight and understanding of major decisions, such as healthcare and research participation (Hunter & Pierscionek, Citation2007). Participants aged 16–25 will be assumed competent and permitted to consent for themselves (see Supplementary Materials for full procedural details).
All data will be collected through online survey format and will be completed during a clinical consult where both the young person and their Tern practitioner are present. All surveys will be hosted within the Qualtrics online survey software. Young people will complete surveys on supplied laptop computers at their respective headspace centre.
Once consent has been given, a one-off entry survey will be completed with the participant. This survey will record demographic information, psychiatric and trauma history. Within the first five sessions post-consent, the young person will be invited to complete their first progress monitoring survey (or at next due date if intervention has already commenced), which will then be repeated after every 10 sessions of Tern received until service exit/end of data collection. The initial progress monitoring survey will be used as the baseline measure. This progress monitoring survey will record limited functional data regarding living situation, occupational activity, psychiatric emergencies, C-PTSD symptomatology, and Tern engagement. When a young person has been discharged from Tern, they will be invited to complete a final exit survey to record their main reason for leaving the service. illustrates all variables and their collection timing.
Table 3. Assessments and outcomes
2.11. Control group
To complement this evaluation a waitlist control will be included as comparator. Pending an initial six months of data collection regarding Tern implementation and client outcomes, young people referred to Tern at the Townsville site but who are 1) not able to commence the programme immediately and 2) not eligible for any other treatment service will be invited to be waitlist participants until they can commence Tern treatment. Waitlisted individuals will be contacted by the principal author by telephone and invited to attend a face-to-face appointment to complete informed consent. This will be followed by completion of their initial demographic survey and progress monitoring surveys. Consent processes and measures will be identical to those completed by active treatment recipients. Repeat measures will be completed at 10-weekly intervals to mimic the time required for 10 sessions of Tern. Once the young person is offered a place in Tern, their practitioner will assume ongoing data collection in place of the principal author.
2.12. Data analysis
Data will be screened and tested for missingness prior to analysis. In the cases of data Missing Completely At Random (MCAR) or Missing At Random (MAR) multiple imputation is the preferred method of resolution (Rubin, Citation1987). Should a significant proportion of dropout be observed, a chi-square test will be conducted to examine for any profile differences between those who completed treatment and those who withdrew. Descriptive statistics will be calculated to answer preliminary questions about the nature of functioning and the mental health experiences of the cohort. To answer the primary aims of this project, mixed effect modelling using multiple timepoints will be used to determine the relationship between number of sessions in Tern to primary clinical outcomes. Time series and survival analyses will be employed to examine secondary outcomes such as engagement in work or study, and frequency of hospitalization as a function of duration in the intervention (Flynn, Citation2012). These tests will be contingent upon a minimum of two time points per participant (Wei, Citation2019). Both recruitment of the desired participant sample size as well as retention of these participants for at least an initial and subsequent progress monitoring survey will be required. However, we do anticipate each participant will provide multiple timepoints given the Tern window of intervention. Dependent on the final sample, sub-groupings may be divided and analysed to determine whether age (adolescence or young adulthood), sex, gender, income, living circumstances, substance use or number and type of interpersonal traumatic events are predictive of outcomes.
3. Discussion
Experiences of traumatic events are common amongst Australian youth presenting to mental health services (Reay et al., Citation2015). Previous research has identified that serious childhood trauma may disrupt a young person’s biological, psychological, and social development (Beal et al., Citation2019; Berto et al., Citation2017; Cook et al., Citation2005). Long-term outcome studies have observed that economic achievement and health outcomes are lower in traumatized individuals compared to non-traumatized individuals (Currie & Spatz Widom, Citation2010; Norman et al., Citation2012).
Within Australia, there are limited options for youth to access publicly funded intervention programs for CT or C-PTSD, and this appears to worsen with degree of rurality (Australian Institue of Health and Welfare, Citation2019). Several proposed guidelines and potential interventions for CT have been evaluated and published in recent years (Cook et al., Citation2003; Society for Traumatic Stress Studies (n.d.); Society for Traumatic Stress Studies (n.d.); Kezelman & Stavropoulos, Citation2012, Citation2019a, Citation2019b; Orygen, Citation2018). However, with the formal inclusion of diagnostic criteria for C-PTSD in the ICD-11, intervention programs have only now been able to be designed and evaluated against these new criteria. There is both opportunity and need for the development and evaluation of new models of care for traumatized youth that draw from established guidelines and pre-existing data. Tern has been designed to address the clinical needs of youth with complex post-traumatic stress, and to also promote functional recovery where occupational and educational attainment are frequently identified as areas of vulnerability for these youth (Currie & Spatz Widom, Citation2010; Norman et al., Citation2012).
3.1. Strengths and limitations
This study is being conducted at two headspace centres in regional North Queensland. Consequently, this project carries the strength of clinically applied ‘real world’ research and has greater generalizability to equivalent youth mental health services in Australia and abroad. Evaluation of the Tern model of care is essential to ensure a true measure of feasibility and implementation. The outcomes from this important preliminary evidence-building phase will support implementation of a randomized controlled trial, which will measure the efficacy of Tern compared to other first-line interventions for this unique cohort.
A further strength of this study is that it will be one of the first to evaluate a purpose-built, Australian model of care for CT. As interventional research into CT has developed, projects have commenced with adapting or applying existing psychosocial interventions to this cohort (Murray, Cohen, & Mannarino, Citation2013). By contrast, Tern has been developed for the specific purpose of treating CT as manifested in C-PTSD and will be among the few, newer interventions designed for this purpose alone. As investigations are ongoing to determine the relative need for phased vs direct processing treatments, this study will expand the current dichotomy through evaluating and reporting outcomes of this individualized model with capacity to offer both phased-based and/or exposure-first methods.
In addition to reducing post-traumatic stress symptoms, Tern seeks to also provide a wrap-around, intensive support for young people to achieve functional outcomes, such as improved work, education, and social function. We propose that including a functional focus in Tern may ameliorate/prevent long-term psychopathology by building young people’s resilience through the fostering of protective factors (e.g. work, education) and minimizing of maintaining factors (e.g. substance use, interpersonal conflict, and re-traumatization).
The young people in the programme are expected to present with complex mental health needs. We anticipate that these young people may present with features of one or more diagnosis, may engage in risky substance use or self-harming behaviour, and will likely fluctuate between regular attendance and irregular or sporadic attendance. We anticipate that intervention in Tern may be interrupted or augmented by psychiatric admission or temporary care by state health services as needed. These factors suggest relative heterogeneity amongst participants as well as in the services they will receive by their Tern practitioner. While these factors pose a challenge in making comparative statements about outcomes, it may be argued that this study is more representative of real-world mental healthcare to much of the similarly focused clinical trial research. Consideration for extraneous variables mediating client outcomes has been considered. Major non-Tern variables that have been hypothesized to have this effect will be measured alongside core clinical outcomes. These are: past psychosocial treatments, current and past psychopharmacological treatment, illicit substance use and change in living circumstances. Functional change as both a variable and outcome is expected to mediate client progress. One specific example is in the observation of living circumstance, where leaving the family may impact the clinical picture when caregivers may be/have been the perpetrators of the traumatic experiences.
The objective of creating a sound evaluative process to nestle within an already operating intervention is not without its challenges. This has necessitated certain sacrifices to the overall design of the project. Firstly, data collected will not be free from demand bias (McCambridge, de Bruin, Witton, & Baradaran, Citation2012). As part of the consenting procedures participants will be informed that the purpose of the study is to evaluate the outcomes of Tern. Further, Tern practitioners will facilitate the completion of monitoring surveys. It will be possible that participants in the programme may unconsciously over or underreport on their surveys based on their relationship with their practitioner. Whilst this may introduce bias into the overall findings, it does represent the real-world nature of this study where in everyday practice it may be such that the treating practitioner conducts assessments of progress themselves (Hatfield & Ogles, Citation2004). Secondly, due to the resource intensity of direct fidelity monitoring, this study will evaluate fidelity through the indirect methods of fidelity checklists and through the structured group supervision process. Monitoring through direct methods such as audio or video recording are beyond the scope of this project; however, there is explicit intention to follow this in a follow-up RCT (Walton, Spector, Tombor, & Michie, Citation2017).
4. Conclusion
This study represents the first major evaluation of the Tern Programme, a new psychosocial intervention model of care for youth with histories of CT. Tern has been developed in response to a gap in Australian mental health services where young people with CT histories have not been adequately managed by existing primary and tertiary services. This implementation trial will examine participants in the programme for a 24-month period and assess mental health, quality of life, and occupational outcomes. It is anticipated that results from this study will contribute to the continuation of research and development of youth mental health services for CT and C-PTSD in Australia.
Author’s Contributions
All authors have made an intellectual contribution to this research project. BJD has developed the model of care. BJD, JP and CK collaborated on the research design and determination of proposed statistical analyses. Manuscript prepared by BJD and reviewed by JP and CK for final approval.
Author’s Information
BJD is completing this research project as part of his Doctor of Philosophy qualification with CQUniversity. This study represents the first in a series of studies being conducted by BJD to evaluate the feasibility of the Tern programme from client and practitioner perspectives.
Ethics Approval and Consent to Participate
Ethical approval was received by the Central Queensland University Human Research Ethics Committee on 14/06/2021, reference number 0000022729. Written consent will be obtained from all participants in this study.
Acknowledgments
We gratefully acknowledge and thank Northern Australia Primary Health Limited for commissioning and funding this research project alongside CQUniversity. Without your support the realisation of Tern would not be possible. We would like to thank Phil Ihme and Kirsten Seymour for the original concept and in securing this research partnership. We would like to thank Barbara Anderson for her contribution to the design of the Tern intervention and teaching us trauma-informed care. We would like to thank Gillian Lunn, Ashlea Sutton and Sandy Revel for the design and implementation of the Tern Skills Group. We would like to thank Rachel Taylor for her contribution and feedback to research ethics and the Tern triage system. Lastly, we would like to thank all other past and future practitioners of Tern, and of course, all the young people who have participated on this journey with us.
Disclosure statement
Northern Australia Primary Health Limited, a not-for-profit organisation, employs BJD and has contributed funding to this project.
Additional information
Funding
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
- American Psychological Association. (2017). Clinical practice guidelines for the treatment of PTSD [Internet]. Retrieved from https://www.apa.org/ptsd-guideline/ptsd.pdf
- Arain, M., Haque, M., Johal, L., Mathur, P., Nel, W., Rais, A., … & Sharma, S. (2013). Maturation of the adolescent brain. Neuropsych Dis Treat, 9 (2013), 449–16 doi:10.2147/NDT.S39776.
- Arnett, J. J. (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. doi:10.1037/0003-066X.55.5.469
- Australian Institue of Health and Welfare. (2019). Family, domestic and sexual violence in Australia: Continuing the national story [Internet]. Retrieved from https://www.aihw.gov.au/getmedia/b0037b2d-a651-4abf-9f7b-00a85e3de528/aihw-fdv3-FDSV-in-Australia-2019.pdf.aspx?inline=true
- Australian Institute of Health and Welfare. (2021). Australia’s youth [Internet]. Retrieved from https://www.aihw.gov.au/reports/children-youth/australias-youth/contents/about
- Balint, M. (2000). The doctor, his patient, and the illness (2th ed.). London: Churchill Livingstone.
- Beal, S., Wingrove, T., Mara, C., Lutz, N., Noll, J., & Greiner, M. (2019). Childhood adversity and associated psychosocial function in adolescents with complex trauma. Child Youth Care Forum, 48(3), 305–322 doi:10.1007/s10566-018-9479-5.
- Ben-Porat, A., & Itzhaky, H. (2009). Implications of treating family violence for the therapist: Secondary traumatization, vicarious traumatization, and growth. Journal of Family Violence, 24(7), 507–515. doi:10.1007/s10896-009-9249-0
- Berto, C., Ferrin, M., Barbera, M., Livianos, L., Rojo, L., & Garcia-Blanco, A. (2017). Abnormal emotional processing in maltreated children diagnosed of complex posttraumatic stress disorder. Child Abuse & Neglect, 73, 42–50. doi:10.1016/j.chiabu.2017.09.020
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. doi:10.1002/jts.22059
- Bloo, J., Arntz, A., & Schouten, E. (2017). The borderline personality disorder checklist: Psychometric evaluation and factorial structure in clinical and nonclinical samples. Roczniki Psychologiczne, 20(2), 311–336. doi:10.18290/rpsych.2017.20.2-3en
- Briere, J. N., & Scott, C. (2014). Principles of trauma therapy: A guide to symptoms, evaluation, and treatment (DSM-5 update). Thousand Oaks: Sage Publications.
- Calthorpe, L. M., & Pantell, M. S. (2021). Differences in the prevalence of childhood adversity by geography in the 2017-18 national survey of children’s health. Child Abuse & Neglect, 111, 104804. doi:10.1016/j.chiabu.2020.104804
- Caxaj, C. S. (2016). A review of mental health approaches for rural communities: Complexities and opportunities in the Canadian context. Canadian Journal of Community Mental Health, 35(1), 29–45. doi:10.7870/cjcmh-2015-023
- Chanen, A. M., Jackson, H. J., McCutcheon, L. K., Jovev, M., Dudgeon, P., Yuen, H. P., & McGorry, P. D. (2008). Early intervention for adolescents with borderline personality disorder using cognitive analytic therapy: Randomised controlled trial. British Journal of Psychiatry, 193(6), 477–484. doi:10.1192/bjp.bp.107.048934
- Cloitre, M., Courtois, C. A., Charuvastra, A., Carapezza, R., Stolbach, B. C., & Green, B. L. (2011). Treatment of complex PTSD: Results of the ISTSS expert clinician survey on best practices. Journal of Traumatic Stress, 24(6), 615–627. doi:10.1002/jts.20697
- Cloitre, M., Khan, C., Mackintosh, M.-A., Garvert, D. W., Henn-Haase, C. M., Falvey, E. C., & Saito, J. (2019). Emotion regulation mediates the relationship between ACES and physical and mental health. Psychological Trauma: Theory, Research, Practice, and Policy, 11(1), 82–89. doi:10.1037/tra0000374
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The international trauma questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. doi:10.1111/acps.12956
- Cloitre, M. (2015). The “one size fits all” approach to trauma treatment: Should we be satisfied? European Journal of Psychotraumatology, 6(1), 27344. doi:10.3402/ejpt.v6.27344
- Cohen, J. A., Mannarino, A. P., Kliethermes, M., & Murray, L. A. (2012). Trauma-focused CBT for youth with complex trauma. Child Abuse & Neglect, 36(6), 528–541. doi:10.1016/j.chiabu.2012.03.007
- Cook, A., Blaustein, M., Spinazola, J., & van der Kolk, B. A. (2003). Complex trauma in children and adolescents. Retrieved from http://www.NCTSNet.org
- Cook, A., Spinazzola, J., Ford, J., Lanktree, C., Blaustein, M., Cloitre, M., & van der Kolk, B. (2005). Complex trauma in children and adolescents. Psychiatric Annals, 35(5), 390–398. doi:10.3928/00485713-20050501-05
- Courtois, C. A., & Ford, J. D. (2009). Treating complex traumatic stress disorders: An evidence-based guide. New York: Guilford Press.
- Craig, C. D., & Sprang, G. (2010). Compassion satisfaction, compassion fatigue, and burnout in a national sample of trauma treatment therapists. Anxiety, Stress & Coping, 23(3), 319–339. doi:10.1080/10615800903085818
- Currie, J., & Spatz Widom, C. (2010). Long-term consequences of child abuse and neglect on adult economic well-being. Child Maltreatment, 15(2), 111–120. doi:10.1177/1077559509355316
- Cyr, M. E., Etchin, A. G., Guthrie, B. J., & Benneyan, J. C. (2019). Access to specialty healthcare in urban versus rural US populations: A systematic literature review. BMC Health Services Research, 19(1), 974. doi:10.1186/s12913-019-4815-5
- de Haan, A. M., Boon, A. E., de Jong, J. T. V. M., Hoeve, M., & Vermeiren, R. R. J. M. (2013). A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clinical Psychology Review, 33(5), 698–711. doi:10.1016/j.cpr.2013.04.005
- de Jongh, A., Resick, P. A., Zoellner, L. A., van Minnen, A., Lee, C. W., Monson, C. M., … Bicanic, I. A. E. (2016). Critical analysis of the current treatment guidelines for complex PTSD in adults. Depression and Anxiety, 33(5), 359–369. doi:10.1002/da.22469
- Department of Health. (2019). Better access to mental healthcare: Fact sheet for professionals [Internet]. Retrieved from https://www1.health.gov.au/internet/main/punlishing.nsf/Content/mental-ba-fact-prof
- Faul, F., Erdfelder, E., Albert-Georg, L., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. doi:10.3758/BF03193146
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. doi:10.1016/S0749-3797(98)00017-8
- Finkelhor, D., Shattuck, A., Turner, H., & Hamby, S. (2015). A revised inventory of adverse childhood experiences. Child Abuse Neglect, 48, 13–21. doi:10.1016/j.chiabu.2015.07.011
- Fisher, J. (2018). Healing the fragmented selves of trauma survivors: Overcoming internal self alientation. Abingdon: Routledge.
- Flynn, R. (2012). Survival analysis. Journal of Clinical Nursing, 21(19pt20), 2789–2797. doi:10.1111/j.1365-2702.2011.04023.x
- Ford, J. D., Van der Kolk, B., Herman, J. L., & Courtois, C. A. (2020). Treating complex traumatic stress disorders in adults: Scientific foundations and therapeutic models (2nd ed.). New York: Guilford Press.
- Fraser, K., MacKenzie, D., & Versnel, J. (2017). Complex trauma in children and youth: A scoping review of sensory-based interventions. Occupational Therapy in Mental Health, 33(3), 199–216. doi:10.1080/0164212X.2016.1265475
- Goldenson, J., Kitollari, I., & Lehman, F. (2021). The relationship between ACEs, trauma-related psychopathology and resilience in vulnerable youth: Implications for screening and treatment. Journal of Child & Adolescent Trauma, 14(1), 151–160. doi:10.1007/s40653-020-00308-y
- Hatfield, D. R., & Ogles, B. M. (2004). The use of outcome measures by psychologists in clinical practice. Professional Psychology: Research and Practice, 35(5), 485–491. doi:10.1037/0735-7028.35.5.485
- Hendriks, L., Kleine, R. A., Heyvaert, M., Becker, E. S., Hendriks, G. J., & Minnen, A. (2017). Intensive prolonged exposure treatment for adolescent complex posttraumatic stress disorder: A single‐trial design. Journal of Child Psychology and Psychiatry, 58(11), 1229–1238. doi:10.1111/jcpp.12756
- Hunter, D., & Pierscionek, B. K. (2007). Children, Gillick competency and consent for involvement in research. Journal of Medical Ethics, 33(11), 659. doi:10.1136/jme.2006.018853
- Imel, Z. E., Laska, K., Jakupcak, M., & Simpson, T. L. (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81(3), 394–404. doi:10.1037/a0031474
- Internation Society for Traumatic Stress Studies. (n.d.). ISTSS position paper on complex PTSD in adults [Internet]. Retrieved from http://istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-Treatment-Guidelines/ISTSS_CPTSD-Position-Paper-(Adults)_FNL.pdf.aspx
- International Society for Traumatic Stress Studies. (n.d.). ISTSS position paper on complex PTSD in children and adolescents [Internet]. Retrieved from https://istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-Treatment-Guidelines/ISTSS_CPTSD-Position-Paper-(Child_Adol)_FNL.pdf.aspx
- John, S. G., Brandt, T. W., Secrist, M. E., Mesman, G. R., Sigel, B. A., & Kramer, T. L. (2019). Empirically-guided assessment of complex trauma for children in foster care A focus on appropriate diagnosis of attachment concerns. Psychological Services, 16(1), 120–133. doi:10.1037/ser0000263
- Karatzias, T., Shevlin, M., Fyvie, C., Grandison, G., Garozi, M., Latham, E., … Hyland, P. (2020). Adverse and benevolent childhood experiences in Posttraumatic Stress Disorder (PTSD) and Complex PTSD (CPTSD): Implications for trauma-focused therapies. European Journal of Psychotraumatology, 11(1), 1793599. doi:10.1080/20008198.2020.1793599
- Kezelman, C. A., & Stavropoulos, P. A. (2012). Practice guidelines for treatment of complex trauma and trauma informed care and service delivery [Internet]. Retrieved from https://www.blueknot.org.au/
- Kezelman, C. A., & Stavropoulos, P. A. (2019a). Practice guidelines for clinical treatment of complex trauma [Internet]. Retrieved from https://www.blueknot.org.au/
- Kezelman, C. A., & Stavropoulos, P. A. (2019b). Complementary guidelines to practice guidelines for clinical treatment of complex trauma [Internet]. Retrieved from https://www.blueknot.org.au/
- Lawson, D. M. (2017). Treating adults with complex trauma: An evidence-based case study. Journal of Counseling & Development, 95(3), 288–298. doi:10.1002/jcad.12143
- Lewis, C., Roberts, N. P., Gibson, S., & Bisson, J. I. (2020). Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1709709. doi:10.1080/20008198.2019.1709709
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., Ommeren, M., Jones, L. M., & Reed, G. M. (2013). Diagnosis and classification of disorders specifically associated with stress: Proposals for ICD‐11. World Psychiatry, 12(3), 198–206. doi:10.1002/wps.20057
- McCambridge, J., De Bruin, M., Witton, J., & Baradaran, H. R. (2012). The effects of demand characteristics on research participant behaviours in non-laboratory settings: A systematic review. PLoS ONE, 7(6), e39116. doi:10.1371/journal.pone.0039116
- McGorry, P. D., Tanti, C., Stokes, R., Hickie, I. B., Carnell, K., Littlefield, L. K., & Moran, J. (2007). headspace: Australia’s national youth mental health foundation — Where young minds come first. Medical Journal of Australia, 187(S7), S68–S70. doi:10.5694/j.1326-5377.2007.tb01342.x
- McLaughlin, K. A., Koenen, K. C., Hill, E. D., Petukhova, M., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2013). Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 52(8), 815–30.e14. doi:10.1016/j.jaac.2013.05.011
- Mills, K. L., McFarlane, A. C., Slade, T., Creamer, M., Silove, D., Teesson, M., & Bryant, R. (2011). Assessing the prevalence of trauma exposure in epidemiological surveys. Australian & New Zealand Journal of Psychiatry, 45(5), 407–415. doi:10.3109/00048674.2010.543654
- Møller, L., Augsburger, M., Elklit, A., Søgaard, U., & Simonsen, E. (2020). Traumatic experiences, ICD-11 PTSD, ICD-11 complex PTSD, and the overlap with ICD-10 diagnoses. Acta Psychiatrica Scandinavica, 141(5), 421–431. doi:10.1111/acps.13161
- Morales, D. A., Barksdale, C. L., & Beckel-Mitchener, A. C. (2020). A call to action to address rural mental health disparities. Journal of Clinical and Translational Science, 4(5), 463–467. doi:10.1017/cts.2020.42
- Murray, L. K., Cohen, J. A., & Mannarino, A. P. (2013). Trauma-focused cognitive behavioral therapy for youth who experience continuous traumatic exposure. Peace and Conflict: Journal of Peace Psychology, 19(2), 180. doi:10.1037/a0032533
- National Child Traumatic Stress Network. (n.d.). Trauma treatments: Overview [Internet]. Retrieved from https://www.nctsn.org/treatments-and-practices/trauma-treatments/overview
- National Rural Health Alliance Inc. (2017). Mental health in rural and remote Australia: Factsheet December 2017 [Internet]. Retrieved from https://www.ruralhealth.org.au/sites/default/files/publications/nrha-mental-health-factsheet-dec-2017.pdf
- Newell, J. M., Nelson-Gardell, D., & MacNeil, G. (2016). Clinician responses to client traumas: A chronological review of constructs and terminology. Trauma, Violence, & Abuse, 17(3), 306–313. doi:10.1177/1524838015584365
- Norman, R. E., Byambaa, M., De, R., Butchart, A., Scott, J., Vos, T., & Tomlinson, M. (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLoS Medicine, 9(11), 11. doi:10.1371/journal.pmed.1001349
- Northern Australia Primary Health Limited. (2017). Youth Trauma Informed Services. [Internal Document].
- Orygen. (2018). Trauma and young people: Moving toward trauma informed services and systems [Internet]. Retrieved from https://www.orygen.org.au/Policy/Policy-Reports/Trauma-and-young-people-Moving-toward-trauma-info/Orygen_trauma_and_young_people_policy_report
- Orygen. (n.d.). Defining the missing middle [Internet]. Retrieved from https://www.orygen.org.au/Policy/Policy-Areas/Government-policy-service-delivery-and-workforce/Service-delivery/Defining-the-missing-middle/orygen-defining-the-missing-middle-pdf.aspx?ext=
- Pai, A., Suris, A. M., & North, C. S. (2017). Posttraumatic stress disorder in the DSM-5: Controversy, change, and conceptual considerations. Behavioral Sciences, 7(1), 7. doi:10.3390/bs7010007
- Patrick, D. L., Edwards, T. C., & Topolski, T. D. (2002). Adolescent quality of life, Part II: Initial validation of a new instrument. Journal of Adolescence, 25(3), 287–300. doi:10.1006/jado.2002.0471
- Perkonigg, A., Höfler, M., Cloitre, M., Wittchen, H., Trautmann, S., & Maercker, A. (2016). Evidence for two different ICD-11 posttraumatic stress disorders in a community sample of adolescents and young adults. European Archives of Psychiatry and Clinical Neuroscience, 266(4), 317–328 doi:10.1007/s00406-015-0639-4.
- Phoenix Australia. (2021). Australian guidelines for the prevention and treatment of acute stress disorder, posttraumatic stress disorder and complex PTSD [Internet]. Retrieved from https://www.phoenixaustralia.org/australian-guidelines-for-ptsd/
- Porges, S. W., & Dana, D. (2018). Clinical applications of the polyvagal theory: The emergence of polyvagal-informed therapies. New York: WW Norton & Company.
- Reay, R. E., Raphael, B., Aplin, V., McAndrew, V., Cubis, J. C., Riordan, D. M., & Preston, W. (2015). Trauma and adversity in the lives of children and adolescents attending a mental health service. Children Australia, 40(3), 167–179. doi:10.1017/cha.2015.20
- Rickwood, D., Paraskakis, M., Quin, D., Hobbs, N., Ryall, V., Trethowan, J., & McGorry, P. (2019). Australia’s innovation in youth mental health care: The headspace centre model. Early Intervention in Psychiatry, 13(1), 159–166. doi:10.1111/eip.12740
- Rothschild, B. (2011). Trauma essentials: The go-to guide. New York: WW Norton & Company.
- Rubin, D. B. (1987). Multiple imputation for nonresponse in surveys. Hoboken, NJ: John Wiley & Sons.
- Rural Doctors Association. (2018). Submission to the senate community affairs committee inquiry into the accessibility and quality of mental health services in rural and remote Australia [Internet]. Retrieved from https://www.aph.gov.au/DocumentStore.ashx?id=3e1d8adf-61a3-44ab-a41c-ad4d08d9daff&subId=612895
- Sachser, C., Berliner, L., Holt, T., Jensen, T. K., Jungbluth, N., Risch, E., … Goldbeck, L. (2017). International development and psychometric properties of the Child and Adolescent Trauma Screen (CATS). Journal of Affective Disorders, 210, 189–195. doi:10.1016/j.jad.2016.12.040
- Schwarz, L., Corrigan, F., Hull, A., & Raju, R. (2016). The comprehensive resource model: Effective therapeutic techniques for the healing of complex trauma. Abingdon: Routledge.
- Siehl, S., Robjant, K., & Crombach, A. (2020). Systematic review and meta-analyses of the long-term efficacy of narrative exposure therapy for adults, children and perpetrators. Psychotherapy Research, 31(6), 695–710 doi:10.1080/10503307.2020.1847345.
- Solmi, M., Radua, J., Olivola, M., Croce, E., Soardo, L., Salazar de Pablo, G., Il Shin, J., Kirkbride, J. B., Jones, P., Kim, J. H., Kim, J. Y., Carvalho, A. F., Seeman, M. V., Correll, C. U., & Fusar-Poli, P (2021). Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Molecular Psychiatry, 10.1038/s41380-021-01161-7. Advance online publication. https://doi.org/10.1038/s41380-021-01161-7
- Spinazzola, J., Ford, J. D., Zucker, M., van der Kolk, B. A., Silva, S., Smith, S. F., & Blaustein, M. (2005). Survey evaluates: Complex trauma exposure, outcome, and intervention among children and adolescents. Psychiatric Annals, 35(5), 433–439. doi:10.3928/00485713-20050501-09
- The WHOQOL Group. (1998). Development of the World Health Organization WHOQOL-BREF Quality of life assessment. Psychological Medicine, 28(3), 551–558. doi:10.1017/S0033291798006667
- Vallières, F., Ceannt, R., Daccache, F., Abou Daher, R., Sleiman, J., Gilmore, B., & Hyland, P. (2018). ICD-11 PTSD and complex PTSD amongst Syrian refugees in Lebanon: The factor structure and the clinical utility of the International Trauma Questionnaire. Acta Psychiatrica Scandinavica, 138(6), 547–557. doi:10.1111/acps.12973
- van der Kolk, B. A. (2005). Developmental trauma disorder: Toward a rational diagnosis for children with complex trauma histories. Psychiatric Annals, 35(5), 401–408. doi:10.3928/00485713-20050501-06
- Van der Kolk, B. (2014). The body keeps the score: Mind, brain and body in the transformation of trauma. London: Penguin.
- van Vliet, N. I., Huntjens, R. J. C., van Dijk, M. K., & de Jongh, A. (2018). Phase-based treatment versus immediate trauma-focused treatment in patients with childhood trauma-related posttraumatic stress disorder: Study protocol for a randomized controlled trial. Trials, 19(1), 138. doi:10.1186/s13063-018-2508-8
- VanDeusen, K. M., & Way, I. (2006). Vicarious trauma: An exploratory study of the impact of providing sexual abuse treatment on clinicians’ trust and intimacy. Journal of Child Sexual Abuse, 15(1), 69–85. doi:10.1300/J070v15n01_04
- Wainberg, M. L., Scorza, P., Shultz, J. M., Helpman, L., Mootz, J. J., Johnson, K. A., & Arbuckle, M. R. (2017). Challenges and opportunities in global mental health: A research-to-practice perspective. Current Psychiatry Reports, 19(5), 28. doi:10.1007/s11920-017-0780-z
- Walton, H., Spector, A., Tombor, I., & Michie, S. (2017). Measures of fidelity of delivery of, and engagement with, complex, face-to-face health behaviour change interventions: A systematic review of measure quality. British Journal of Health Psychology, 22(4), 872–903. doi:10.1111/bjhp.12260
- Wamser-Nanney, R. (2019). risk factors for attrition from pediatric trauma-focused treatment. Child Maltreatment, 25(2), 172–181. doi:10.1177/1077559519874406
- Way, I., VanDeusen, K. M., MartIn, G., Applegate, B., & Jandle, D. (2004). Vicarious trauma: A comparison of clinicians who treat survivors of sexual abuse and sexual offenders. Journal of Interpersonal Violence, 19(1), 49–71. doi:10.1177/0886260503259050
- Wei, W. (2019). Multivariate time series analysis and applications (1st ed.). Hoboken, NJ: John Wiley & Sons Inc.
- World Health Organisation. (2018). International classification of diseases for mortality and morbidity statistics [Internet]. Retrieved from https://icd.who.int/browse11/l-m/en
- World Health Organisation. (2021). Adolescent health [Internet]. Retrieved from https://www.who.int/southeastasia/health-topics/adolescent-health