ABSTRACT
Background
New intensive trauma-focused treatment (TFT) programmes that incorporate physical activity have been developed for people with post-traumatic stress disorder (PTSD). However, the unique contribution of physical activity within these intensive TFT programmes has never been investigated in a controlled manner.
Objectives
This randomized controlled trial will investigate the effectiveness of physical activity added to an intensive TFT programme. In addition, the study aims to investigate the underlying mechanisms of the effects of physical activity on the change in PTSD symptoms.
Methods
Individuals with PTSD (N = 120) will be randomly allocated to two conditions: a physical activity or a non-physical active control condition. All participants will receive the same intensive TFT lasting eight days within two consecutive weeks, in which daily prolonged exposure and EMDR therapy sessions, and psycho-education are combined. The amount of physical activity will differ per condition. While the physical activity condition induces daily physical activities with moderate intensity, in the non-physical active control condition no physical activity is prescribed; but instead, a controlled mixture of guided (creative) tasks is performed. The two primary outcome measures are change in PTSD symptoms from pre- to post-treatment and at six months follow-up, measured with the Clinician-Administered PTSD Scale (CAPS-5), and the PTSD Checklist for DSM-5 (PCL-5). Additionally, self-reported sleep problems, depressive symptoms, emotion regulation, dissociation symptoms and anxiety sensitivity will be measured as potential underlying mechanisms.
Conclusions
This study will contribute to the research field of augmentation strategies for PTSD treatment by investigating the effectiveness of physical activity added to intensive TFT.
Trial registration
This trial is registered in the Netherlands Trial Register (Trial NL9120).
HIGHLIGHTS
This study will be the first to determine the effectiveness of physical activity as add-on to an intensive TFT programme, and to investigate the underlying mechanisms of the effects of physical activity on the treatment-related change in PTSD symptoms.
Antecedentes: Se han desarrollado para personas con TEPT nuevos programas de tratamiento intensivos centrados en trauma (TFT por sus siglas en inglés) que incorporan actividad física. Sin embargo, la contribución única de la actividad física dentro de estos programas de TFT intensivos nunca se ha investigado de manera controlada.
Objetivos: Este ensayo controlado aleatorizado investigará la efectividad de la actividad física agregada a un programa intensivo de TFT. Además, el estudio tiene como objetivo investigar los mecanismos subyacentes de los efectos de la actividad física sobre el cambio en los síntomas de TEPT.
Métodos: Las personas con TEPT serán asignadas en forma aleatoria a dos condiciones: una actividad física o una condición de control activo no físico. Todos los participantes recibirán la misma TFT intensiva que durará 8 días dentro de dos semanas consecutivas, en las que se combinarán diariamente la exposición prolongada y las sesiones de terapia EMDR y psicoeducación. La cantidad de actividad física diferirá según la condición. Mientras que la condición de actividad física induce actividades físicas diarias de moderada intensidad, en la condición de control activo no físico no se prescribe actividad física, sino que se realiza una mezcla controlada de tareas guiadas (creativa). Las dos medidas de resultado primarias son el cambio en los síntomas de TEPT antes y después del tratamiento y a los seis meses de seguimiento, medidos con la Escala de TEPT administrada por el clínico (CAPS-5) y la Lista de verificación de TEPT del DSM-5 (PCL-5). Adicionalmente, los problemas del sueño autoinformados, los síntomas depresivos, la regulación de emociones, los síntomas disociativos y la sensibilidad a la ansiedad se medirán como potenciales mecanismos subyacentes.
Conclusiones: Este estudio contribuirá al campo de la investigación de las estrategias de potenciación para el tratamiento del TEPT al investigar la efectividad de la actividad física agregada a la TFT intensiva.
Registro de ensayo: este ensayo esta registrado en el Registro de ensayos de los Países Bajos (ensayo NL 9120).
背景: 已经为 PTSD 患者开发了包含身体活动的全新聚焦创伤强化治疗 (TFT) 计划。然而, 体育活动在这些强化TFT 计划中的独特贡献从未被以受控的方式研究过。
目的: 本随机对照试验将考查添加到强化 TFT 计划中的身体活动的有效性。此外, 本研究旨在考查体育活动对 PTSD 症状变化影响的潜在机制。
方法: 患有 PTSD 的个体 (N = 120) 将被随机分配到两个条件:身体活动或非身体活动控制条件。所有参与者将在连续两周内接受持续八天的相同强化 TFT, 结合了日常延长暴露和 EMDR 治疗以及心理教育。身体活动量会因情况而异。虽然身体活动条件诱发中等强度的日常体力活动, 在非体力活动控制条件下, 不指定体力活动, 而是执行指导性 (创造性) 任务的受控混合。两个主要结果指标是从治疗前到治疗后以及六个月随访时用临床用PTSD 量表 (CAPS-5) 和 DSM-5 PTSD 检查表 (PCL-5) 测量的 PTSD 症状改变。此外, 自我报告的睡眠问题, 抑郁症状, 情绪调节, 分离症状和焦虑敏感性将作为可能的潜在机制进行测量。
结论: 本研究将通过考查添加到强化 TFT 的身体活动的有效性, 为 PTSD 治疗增强策略的研究领域做出贡献。试验注册:该试验已在荷兰试验注册中心 (Trial NL9120) 登记。
1. Background
Several empirical studies yielded a positive effect of supplemental physical activity on the treatment outcome of individuals with post-traumatic stress disorder (PTSD). For instance, the first meta-analysis on this topic showed that physical activity (e.g. active yoga, aerobic resistance based- or stationary cycling interventions) in addition to usual care was associated with a stronger decrease in PTSD symptoms compared to usual care, or a wait-list control condition alone (Rosenbaum, Vancampfort, et al., Citation2015). These physical activity interventions ranged from one to two supervised sessions per week within a time frame of six to 12 weeks. Additionally, more recent meta-analyses supported these findings and showed that physical activity interventions as an add-on to psychological treatments, are promising treatment options for individuals with PTSD (Davis, Zachry, & Berke, Citation2021; Ramos-Sanchez et al., Citation2021). However, many previous (pilot) studies lacked a non-physical active control condition (Goldstein et al., Citation2018; Hall et al., Citation2020; Nordbrandt, Sonne, Mortensen, & Carlsson, Citation2020; Powers et al., Citation2015; Rosenbaum, Sherrington, et al., Citation2015). Therefore, non-specific effects of the physical activity sessions, such as receiving attention and social support, might have been responsible for the stronger decrease in PTSD symptoms. Besides, most studies investigated a homogeneous group of patients (e.g. veterans, refugees; Goldstein et al., Citation2018; Hall et al., Citation2020; Nordbrandt et al., Citation2020), and lacked long-term follow-up measurements (Goldstein et al., Citation2018; Nordbrandt et al., Citation2020; Powers et al., Citation2015; Rosenbaum, Sherrington, et al., Citation2015; Whitworth, Nosrat, SantaBarbara, & Ciccolo, Citation2019a, Citation2019b).
In compliance with the promising findings for supplemental physical activity, new intensive trauma-focused treatment (TFT) programmes, including prolonged exposure (PE) and eye movement desensitization and reprocessing (EMDR) therapy, have been invented for people with PTSD that integrate physical activity. These intensive TFT treatments have shown strong declines in PTSD symptoms within five to eight treatment days (Brynhildsvoll Auren, Gjerde Jensen, Rendum Klæth, Maksic, & Solem, Citation2021; Van Woudenberg et al., Citation2018; Voorendonk, De Jongh, Rozendaal, & Van Minnen, Citation2020; Zalta et al., Citation2018; Zepeda Méndez, Nijdam, Ter Heide, Van Der, & Olff, Citation2018). Yet, as these studies were not controlled or randomized, the unique contribution of physical activity remains unknown (Voorendonk, Sanches, De Jongh, & Van Minnen, Citation2019). Therefore, the first aim of our proposed study is to determine the possible enhancing effect of physical activity to TFT on PTSD treatment outcome using a randomized controlled trial. In this study we include a non-physical active control condition to control for the effects of physical activity above attention and any other non-specific effects. Additionally, we will include a follow-up assessment six months after treatment to investigate whether these effects are sustained.
In addition, as a second aim, we are interested in the underlying mechanisms of these physical activity effects, since studies designed to investigate mediators of PTSD symptom change after physical activity are lacking (Davis et al., Citation2021). One possible mechanism of the effect of physical activity on the mental health of individuals with PTSD could be the positive effect that physical activity exerts on (self-reported indices of) sleep (Babson et al., Citation2015; Reid et al., Citation2010; Whitworth, Craft, Dunsiger, & Ciccolo, Citation2017; Whitworth et al., Citation2019b). Other mechanisms that may underlie the beneficial effects of physical activity on PTSD symptoms is through the improvement of depressive symptoms (Gordon et al., Citation2018; Schuch et al., Citation2016), and emotion regulation (Jacquart et al., Citation2018; Oaten & Cheng, Citation2006; Voorendonk, Sanches, Mojet, De Jongh, & Van Minnen, Citation2021; Warner, Spinazzola, Westcott, Gunn, & Hodgdon, Citation2014). Furthermore, mediators of the relation between physical activity and PTSD symptoms might be through the reductions in dissociative symptoms (Voorendonk et al., Citation2021; Zoet, Wagenmans, Van Minnen, & De Jongh, Citation2018) or anxiety sensitivity (Broman-fulks, Berman, Rabian, & Webster, Citation2004; Jacquart et al., Citation2018; Smits et al., Citation2008). Additionally, the effects of physical activity on other secondary (health) variables between the conditions will be explored (quality of life, daily physical activities, general somatic complaints, physical health, and complex PTSD symptoms).
In sum, the objectives of the current study are 1) to determine the effectiveness of physical activity added to an intensive TFT programme and 2) to investigate the underlying mechanisms of the effects of physical activity on the treatment-related change in PTSD symptoms from pre- to posttreatment. It is hypothesized that patients receiving the physical activity condition will show a significantly greater decrease in PTSD symptoms between pre- and post-treatment than patients in the non-physical active control condition. This difference between the conditions will persist at six months follow-up. Furthermore, we hypothesize that the effects of physical activity on the treatment-related change in PTSD symptoms will be mediated by stronger improvements over time in sleep problems, depressive symptoms, emotion regulation, dissociation, and anxiety sensitivity in the physical activity condition compared to the non-physical active control condition.
2. Methods
2.1. Study design
The design of the study will be a randomized controlled trial in which participants will be randomly assigned to two conditions; a physical activity or a non-physical active control condition, in addition to an intensive TFT treatment programme. Symptom and mediator assessments will take place at pre-treatment (T0intake), during the eight days of treatment (Tday1-day8), at mid-treatment (Tmid), post-treatment (T1post), and at six months (T2follow-up) follow-up. The first four days of treatment are delivered face-to-face (inpatient) and the last four days of the programme will be delivered fully remotely.
2.2. Participants
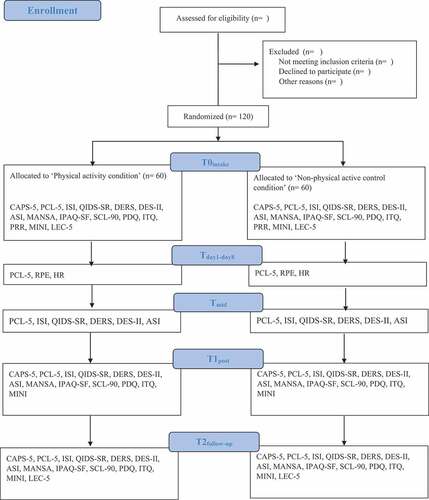
The research will be carried out with a group of 120 patients with PTSD who are treated at the Psychotrauma Expertise Centre (PSYTREC Bilthoven; the Netherlands). All patients will be referred by their general practitioner, psychologist, or psychiatrist. In order to be eligible to participate in this study, subjects must meet all of the following inclusion criteria: (1) a diagnosis of PTSD based on the Clinician-Administered PTSD Scale (CAPS-5), (2) being at least 18 years old, and (3) sufficient knowledge of the Dutch language to undergo treatment. Potential subjects who meet any of the following criteria will be excluded from participation in this study: (1) a suicide attempt less than three months prior to treatment, (2) being medically unfit to participate in the physical activity condition, i.e. not being able to walk for at least 30 minutes (e.g. physical impairments that necessitate the use of wheelchair). We will not exclude patients in this study based on suicidal ideation, type of trauma or comorbidity (e.g. personality disorders, psychosis). The CONSORT flow diagram is shown in .Footnote1
2.3. Interventions
In both conditions, the intervention will consist of the same intensive TFT programme of eight days within two consecutive weeks combining daily prolonged exposure (PE; 90 minutes), eye movement desensitization and reprocessing (EMDR) therapy (90 minutes), and psycho-education (see for more treatment information Van Woudenberg et al., Citation2018; Voorendonk et al., Citation2020). Every treatment day, besides the PE in the morning and EMDR therapy in the afternoon, participants take part in four timeslots (of 90 minutes each) of physical activity or non-physical active control activities (see ). These four timeslots are in a group format and follow a protocol. The psycho-education sessions for the non-physical active control condition will not include information on physical activity, but will be slightly modified in a way that highlights the benefits of creative tasks instead.
Figure 2. Overview of (A) the treatment schedule and (B) the daily schedule (an example). PE = Prolonged exposure; EMDR = eye movement desensitization and reprocessing.
2.3.1. Physical activity condition
The physical activity condition induces daily physical activities of moderate intensity, with 60–70% of a person’s maximum heart rate, which has been found to enhance TFT effects in previous research (e.g. Powers et al., Citation2015). Additionally, since resistance training has also been found to improve anxiety symptoms (Gordon, McDowell, Lyons, & Herring, Citation2017), the physical activity intervention will consist of combined exercise forms (aerobic and resistance training). Every on-site treatment day will start and end with an outside walk. The other two timeslots per day will differ, based on the protocol; basketball, ultimate frisbee, mountain biking, boxing, soccer, softball, ergometer and resistance training. In the protocol for online treatment days, every timeslot the participants will start and end in a group format through Zoom Meetings. Daily live-lessons (aerobic and resistance) will be delivered digitally through Zoom, alternated with timeslots of individual walking or other activities. Of importance, no therapeutic interventions such as body awareness, exposure, relaxation, and mindfulness will be delivered during the physical activities.
2.3.2. Non-physical active control condition
In the non-physical active control condition, no additional physical activity is performed, but the condition consists of a controlled mixture of guided tasks based on a protocol. Participants in the non-physical active control condition will be instructed to move as little as possible and remain largely sedentary as indicated by a low heart rate. Examples of activities that will be used in the non-physical active control condition are: board games, reading, and creative activities, such as drawing, painting, crochet, and clay modelling. The tasks will be accompanied with assignments and themes (e.g. painting a flower vase). In the protocol for online treatment days, every timeslot the participants will start and end in a group format through Zoom Meetings. Of importance, no therapeutic interventions will be delivered during the (creative) tasks.
2.3.3. Manipulation check
Physical activity intensity will be individually monitored and checked in both conditions at every timeslot with heart rate monitors (Fitbit Charge 4) and a subjective perception rating scale (Borg’s Rating of Perceived Exertion; RPE; Borg, Citation1998). The RPE is a widely used, easy and valid measure to describe physical activity intensity as it strongly correlates with heart rate and blood lactate (Scherr et al., Citation2013). The RPE is already used in PTSD samples (Rosenbaum, Sherrington, et al., Citation2015) and the moderate intensity of 60–70% of someone’s maximal heart rate is comparable to a RPE score between 12 and 15 (Crombie, Brellenthin, Hillard, & Koltyn, Citation2018). The heart rate and RPE scales will be used to control for the intensity during the first and second week of treatment at home (online). All physical activity sessions and non-physical active control activities will be provided by instructors with a degree in human movement sciences, who are specifically trained for the activity programme and have experience in working with patients with PTSD. High attendance rates and the quality of the conditions are assured since these trained instructors will supervise all participants, alternating physical activity and non-physical active control conditions.
2.4. Procedures
In total, eight treatment groups of 15 participants will be included in the randomized controlled trial. A treatment group will start every two weeks (120 participants in total). To prevent contamination effects between conditions, there will be no participants from different conditions in the same treatment group. The intake procedure consists of two intake sessions with one week in between. During the first day of the intake procedure, patients who meet the inclusion criteria will be informed about the study by a trained clinical psychologist. They receive written and verbal explanation about the aims of the research and what participation entails. Furthermore, the CAPS-5, LEC-5, and MINI will be measured during the first intake. In between the two intake sessions, participants will be asked to fill in digital self-report questionnaires (T0intake: PCL-5, ISI, QIDS-SR, DERS, DES-II, ASI, MANSA, IPAQ-SF, SCL-90, PDQ, ITQ, and PRR). During the second intake, after at least a week of consideration time, the participants will give written informed consent for participation in the trial. Allocation to the physical activity or the non-physical active control condition will take place immediately after the second intake session and participants will receive information about their starting date. To ensure allocation concealment, the coordinator of the research, who is not involved in recruitment during intake, will perform the randomization. Block randomization, without stratification factors, will be performed with a scientific randomization programme on the Internet (www.randomizer.org). There will be 20 blocks of six participants, so each block has three assignments for the two conditions. Participants will be allocated to one of the two conditions, which will be delivered every two weeks in one treatment group. Patients that do not want to participate in the study will be offered the regular PSYTREC treatment every two weeks in between the study treatment groups. Participant flow is presented in .
When participants start treatment at Sunday evening, heart rate monitors will be handed out. Afterwards, during all eight treatment days, the PCL-5 will be administered in the morning to assess PTSD symptoms during treatment (Tday1-day8), and the RPE scale plus heart rate recordings will be assessed after all four timeslots of physical or non-physical active control activities. After the first four days of treatment, participants will return home and mid-treatment assessment of the possible mediating variables will be measured digitally, in between treatment week one and two (Tmid: ISI, QIDS-SR, DERS, DES-II, ASI). Participants will take the heart rate monitors and additional materials (e.g. creative equipment for the non-physical active control condition) home with them. They return the heart rate monitor and materials directly after the eight treatment days. Eight days after the last day of treatment the post-treatment measurements will be administered (T1post; CAPS-5, MINI, PCL-5, ISI, QIDS-SR, DERS, DES-II, ASI, MANSA, IPAQ-SF, SCL-90, PDQ, and ITQ). These measurements will be repeated at six months follow-up through telephone and online (T2follow-up; additional LEC-5). An overview of the assessments is presented in and .
Table 1. Overview of assessments
2.5. Ethics
Ethical approval for this study was granted by the Medical Ethics Review Committee of the VU university Medical Center (VUmc: IRB00002991, FWA00017598) on 15 May 2020 (reference number: 2019.574 – NL70812.029.19). The study is also registered in the Netherlands Trial Register (Trial NL9120).
2.6. Assessments
2.6.1. Primary outcomes
The primary outcome will be the change in PTSD symptoms measured using the Dutch version of the Clinician-Administered PTSD Scale (CAPS-5; Boeschoten et al., Citation2018) and the PTSD Checklist for DSM-5 (PCL-5; Boeschoten, Bakker, Jongedijk, & Olff, Citation2014).
The CAPS-5 will be administered at baseline, post-treatment and at six months follow-up and is a clinical interview used to assess PTSD symptom severity and diagnosis. The CAPS-5 consists of 20 items on frequency and intensity of PTSD symptoms, scored on a 5-point Likert scale from 0 (absent) to 4 (extreme/incapacitating), with a maximum score of 80. The PTSD diagnosis will be established with the SEV2 rule and DSM-5 algorithm (Boeschoten et al., Citation2018; Weathers et al., Citation2017). At baseline and six months follow-up, the CAPS-5 month-version will be used, whereas at post-measurement the week-version will be used. The CAPS-5 is the widely used ‘gold standard’ to assess PTSD severity and diagnosis and is a reliable and internally consistent measure (α = .90; Boeschoten et al., Citation2018).
The PCL-5 is a self-report measure to assess PTSD symptom severity and will be measured at baseline, during the eight days of treatment, mid-treatment, post-treatment and at six months follow-up. The PCL-5 is a validated and widely used scale that consists of 20 items, scored on a 5-point Likert scale from 0 (not at all) to 4 (extremely), with a total score ranging between 0 and 80 (α = .94; Blevins, Weathers, Davis, Witte, & Domino, Citation2015; Boeschoten et al., Citation2014).
2.6.2. Possible mediators
The following secondary outcome measures (possible mediators) will be measured at baseline, mid- and post-treatment and at six months follow-up:
(1) Insomnia, measured with the valid brief self-report instrument Insomnia Severity Index (ISI; α = .91; Morin, Belleville, Bélanger, & Ivers, Citation2011). The ISI consists of seven items scored on a scale ranging from 0 (not at all) to 4 (extremely hindering) with a maximum score of 28. An additional self-constructed item, concerning whether sleep medication has been used (yes/no), will be added to the questionnaire.
(2) Depressive symptoms, measured with the validated 16-item Quick Inventory of Depressive Symptomatology Self-Report (QIDS-SR; α = .89; Reilly, MacGillivray, Reid, & Cameron, Citation2015; Surís, Holder, Holliday, & Clem, Citation2016). The QIDS-SR consists of 16 items on depressive symptoms over 9 symptom domains with a score ranging between 0 and 3 per item. For each symptom domain one score is used resulting in a maximum total score of 27.
(3) Emotion regulation problems, measured with the validated Difficulties in Emotion Regulation Scale (DERS; α = .93; Gratz & Roemer, Citation2004; Neumann, Lier, Van, Gratz, & Koot, Citation2010). The DERS is a self-report measure that consist of 36 items with a scoring range from 1 (almost never) to 5 (almost always). The total score ranges between 36 and 180.
(4) Dissociative symptoms, measured with the valid Dissociative Experiences Scale-II (DES-II; α = .92; Zingrone & Alvarado, Citation2002). The DES-II consists of 28 items on which each participant will indicate the percentage of time they experience a symptom (between 0 and 100%). The total score is calculated by averaging these percentage scores, with total scores ranging between 0 and 100.
(5) Anxiety sensitivity, measured with the validated self-report Anxiety Sensitivity Index (ASI; α = .83; Vujanovic, Arrindell, Bernstein, Norton, & Zvolensky, Citation2007). The ASI measures the distress of anxiety-related symptoms with 16 items on a 5-point Likert scale ranging from 0 (very little) to 4 (very much). The total score ranges between 0 and 64.
2.6.3. Secondary (health) outcomes
(1) Changes in quality of life will be indexed using the validated Manchester Short Assessment of quality of life (MANSA; α = .81; Björkman & Svensson, Citation2009; Van Nieuwenhuizen, Schene, & Koeter, Citation2000).
(2) To assess the subjective health-related physical activity the International Physical Activity Questionnaire Short Form will be used (IPAQ-SF; Craig et al., Citation2003). The physical activity level (low, moderate and vigorous) will be indexed with the IPAQ scoring protocol to assess its influence on the treatment effect (possible moderator; IPAQ Research Committee, 2005).
(3) The somatization subscale from the Symptom Check List-90 (SCL-90; Arrindell & Ettema, Citation2003) will be used to measure general somatic complaints.
(4) A self-constructed self-report questionnaire to assess physical health in general will be administered (e.g. diabetes and cardiovascular problems; Physical Disorders Questionnaire; PDQ).
(5) The International Trauma Questionnaire (ITQ; α = .89-.94; Cloitre, Hyland, Prins, & Shevlin, Citation2021; Eidhof, Ter Heide, Boeschoten, & Olff, Citation2018) will be used to establish PTSD and Complex PTSD (CPTSD) diagnoses and (C)PTSD symptom severity.
2.6.4. Other measures
(1) A modified version of the Personal Reactions to Rationales (PRR; Zoellner, Feeny, & Bittinger, Citation2009) questionnaire will be used to assess treatment preferences (physical activity or creative tasks) at baseline to assess its influence on the treatment effect (possible moderator). An additional question about subjective physical fitness level will be added because current subjective fitness level may differ between subjects and may influence preferences.
(2) The Mini International Neuropsychiatric Interview Dutch version (MINI; Overbeek, Schruers, & Griez, Citation1999) will be used to diagnose comorbid disorders. It is a detailed, structured and well-validated questionnaire administered in an interview format (Lecrubier et al., Citation1997).
(3) The life events checklist for DSM-5 (LEC-5; Weathers et al., Citation2013) will be used to assess trauma characteristics at baseline, and to establish possible revictimization, this will be repeated at six months follow-up.
2.7. Power and sample size calculation
An a priori power calculation programme showed that the proposed randomized controlled trial sample need to consists of 86 participants (G*Power 3.1.9.2; F-test over two groups with a moderate effect size, α = .05, f = .25, power = .80). This moderate effect size is based on multiple previous research showing bordering-medium to large effect sizes (Goldstein et al., Citation2018; Hall et al., Citation2020; Powers et al., Citation2015; Ramos-Sanchez et al., Citation2021; Rosenbaum, Sherrington, et al., Citation2015; Rosenbaum et al., Citation2015; Whitworth et al., Citation2019a). Besides this, our study most resembles the study of Rosenbaum, Sherrington, and colleagues (Citation2015), who reported a moderate effect size. Therefore, we chose to perform a power analysis with a moderate effect size as well. To take into account the possibility of drop out, technical measurement failure and missing data, an additional 20% (Rosenbaum, Sherrington, et al., Citation2015; Rosenbaum, Tiedemann, Sherrington, & van der Ploeg, Citation2014) of the study participants will be added (N = 103). Based on the current treatment group sizes at PSYTREC (n= 15), we have decided to include eight treatment groups to assure equal distribution over both conditions (N = 120). Thus, both conditions in the trial will include 60 participants.
2.8. Data analysis
To test whether the decrease in PTSD symptoms over time will be significantly stronger in the physical activity condition compared to the non-physical active control condition, two Linear Mixed Models (LMM) will be used on the primary outcome variables (CAPS-5 and PCL-5). The fixed part will consist of time, condition, and its interaction. A random intercept and random time slope will be added so that the possible higher correlation between the measurements points within one participant could be taken into account, and this dependence cannot influence the fixed part of the model. The intention-to-treat and completers sample will both be analysed.
To test the possible underlying mechanisms (ISI, QIDS-SR, DERS, DES-II, and ASI), mediation analyses will be carried out with the bootstrap method tests, from Hayes’s PROCESS tool in SPSS (Field, Citation2013). Besides testing the regression models of path c, a and b, it eventually tests the indirect effect (path axb; the effect of mediation) and its confidence interval (CI) (Hayes, Citation2018).
The same LMM analyses will be used to explore the changes in the other secondary (health) outcome measures over time between the two conditions (MANSA, IPAQ-SF, SCL-90, PDQ, and ITQ), as well as to investigate the possible moderators for the effect on PTSD symptom progression over time (for PRR and IPAQ-SF levels).
3. Discussion
The current study will be the first to determine the effectiveness of physical activity as add-on to an intensive TFT programme in a controlled manner, and to investigate the underlying mechanisms of the effects of physical activity on the treatment-related change in PTSD symptoms. If we can find support for the addition of physical activity to a TFT programme as an enhancing strategy for PTSD treatment outcome in intensive TFT, over and above its non-specific effects, this may be a meaningful contribution to the research field on physical activity and PTSD treatment outcomes. What makes this research goal especially relevant is that several PTSD treatments worldwide incorporate forms of physical activity in (intensive) PTSD treatment formats (Brynhildsvoll Auren et al., Citation2021; Van Woudenberg et al., Citation2018; Voorendonk et al., Citation2020; Zalta et al., Citation2018; Zepeda Méndez et al., Citation2018) without knowing its exact effects.
Strengths of the design are the randomization and incorporation of a non-physical active control condition. Additionally, underlying mechanisms will be investigated (sleep problems, depressive symptoms, emotion regulation, dissociation and anxiety sensitivity). This is needed since research on mediators of the effect of physical activity on treatment-related change in PTSD symptoms are limited (Davis et al., Citation2021). Moreover, the study includes a comprehensive manipulation check to verify the internal validity of our physical activity intervention using the monitoring of heart rate and self-reported perceived exertion. The intensive format and supervision during the programme may also help in achieving high attendance rates in both conditions. Furthermore, we will follow participants for a period of six months after treatment, to establish whether effects are sustained after treatment, plus clinician-administered interviews and self-report questionnaires will be used together with a broad variety of secondary (health) outcome measures (quality of life, daily physical activities, general somatic complaints, physical health, complex PTSD symptoms). At last, a heterogeneous and large (N = 120) group of individuals with PTSD will be included, who might have been exposed to a wide variety of traumatic events and suffer from a wide array of comorbid mental health conditions, since very few exclusion criteria are adopted. At the same time, some limitations should be mentioned. Firstly, we will not include a control condition in which the PE, EMDR therapy, and psycho-education will be combined with no additional intervention at all. Therefore, we cannot conclude that adding physical activity in the context of an intensive TFT format is better than doing nothing. However, the added value of physical activity in comparison to wait-list control conditions, or nothing (stand-alone form), has already shown to be effective in reducing PTSD symptoms (Davis et al., Citation2021; Ramos-Sanchez et al., Citation2021; Rosenbaum et al., Citation2015). Therefore, our comparison with a non-physical active control condition seems a logical next step. Secondly, although we will continuously monitor the heart rates and perceived exertions during the intervention time slots, it is impossible to keep track of all activities, especially during the six months after treatment when participants will not be monitored with heart rate monitors. Moreover, the heart rate monitor in itself could already elicit a treatment effect in both conditions through having knowledge of their own heart rates being a form of interoceptive exposure to feared somatic sensations (Asmundson et al., Citation2013; Hegberg, Hayes, & Hayes, Citation2019). Furthermore, it could be that the brief duration of the physical activities (two weeks) might be too short to already enhance the PTSD treatment outcome, and that longer physical interventions (e.g. six weeks) are needed, or that differences will only become visible at follow-up. Likewise, the intensive schedule of the physical activity condition could also be too exhaustive for individuals with a low physical activity level at baseline, which may negatively influence the PTSD treatment outcome and might result in higher drop-out rates.
In conclusion, it is expected that the current study will contribute to the research field of augmentation strategies for PTSD treatment by investigating the effectiveness of physical activity added to intensive TFT. Besides the well-known physical health benefits of physical activity, we will determine whether it contributes to the enhancement of PTSD treatment outcome over and above non-specific effects. Since a physical activity intervention is an easy to administer strategy for the enhancement of intensive TFT for PTSD, results from the current study could justify and facilitate its use in clinical practice.
Supplemental Material
Download MS Word (124.5 KB)Acknowledgments
We would like to thank Ella Hoogendoorn and Georgy Gomon for their assistance in the data analysis plan.
Disclosure statement
Agnes Van Minnen receives income for published book chapters on PTSD and for the training of postdoctoral professionals in prolonged exposure. Ad De Jongh receives income from published books on EMDR therapy and for the training of postdoctoral professionals in this method. Eline Voorendonk, Sarita Sanches and Marieke Tollenaar have no competing interests.
Data availability statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
Notes
1 The SPIRIT 2013 checklist can be found in the supplementary file.
References
- Arrindell, W. A., & Ettema, J. H. M. (2003). SCL-90 — Handleiding bij een multidimensionele psychopathologie indicator [SCL-90 — Manual for a multidimensional psychopathology indicator]. Lisse, the Netherlands: Swets & Zeitlinger.
- Asmundson, G. J. G., Fetzner, M. G., Deboer, L. B., Powers, M. B., Otto, M. W., & Smits, J. A. J. (2013). Let’s get physical: A contemporary review of the anxiolytic effects of exercise for anxiety and its disorders. Depression and Anxiety, 30(4), 362–11. doi:10.1002/da.22043
- Babson, K. A., Heinz, A. J., Ramirez, G., Puckett, M., Irons, J. G., Bonn-Miller, M. O., & Woodward, S. H. (2015). The interactive role of exercise and sleep on veteran recovery from symptoms of PTSD. Mental Health and Physical Activity, 8, 15–20. doi:10.1016/j.mhpa.2014.12.002
- Björkman, T., & Svensson, B. (2009). Quality of life in people with severe mental illness. Reliability and validity of the Manchester Short Assessment of Quality of Life (MANSA). Nordic Journal of Psychiatry, 59(4), 302–306. doi:10.1080/08039480500213733
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. doi:10.1002/jts
- Boeschoten, M. A., Bakker, A., Jongedijk, R. A., & Olff, M. (2014). PTSD checklist for the DSM-5 (PCL-5) – Nederlandstalige versie. Diemen: Arq Psychotrauma Expert Groep.
- Boeschoten, M. A., Van der Aa, N., Bakker, A., Ter Heide, F. J. J., Hoofwijk, M. C., Jongedijk, R. A., Olff, M. (2018). Development and Evaluation of the Dutch Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). European Journal of Psychotraumatology, 9(1), 1. doi:10.1080/20008198.2018.1546085
- Borg, G. (1998). Borg’s perceived exertion and pain scales. Champaign, IL: Human Kinetics.
- Broman-fulks, J. J., Berman, M. E., Rabian, B. A., & Webster, M. J. (2004). Effects of aerobic exercise on anxiety sensitivity. Behaviour Research and Therapy, 42(2), 125–136. doi:10.1016/S0005-7967(03)00103-7
- Brynhildsvoll Auren, T. J., Gjerde Jensen, A., Rendum Klæth, J., Maksic, E., & Solem, S. (2021). Intensive outpatient treatment for PTSD: A pilot feasibility study combining prolonged exposure therapy, EMDR, physical activity, and psychoeducation. European Journal of Psychotraumatology, 12(1), 1. doi:10.1080/20008198.2021.1917878
- Cloitre, M., Hyland, P., Prins, A., & Shevlin, M. (2021). The international trauma questionnaire (ITQ) measures reliable and clinically significant treatment-related change in PTSD and complex PTSD. European Journal of Psychotraumatology, 12(1), 1. doi:10.1080/20008198.2021.1930961
- Craig, C. L., Marshall, A. L., Sjöström, M., Bauman, A. E., Booth, M. L., Ainsworth, B. E., … Oja, P. (2003). International physical activity questionnaire: 12-Country reliability and validity. Medicine and Science in Sports and Exercise, 35(8), 1381–1395. doi:10.1249/01.MSS.0000078924.61453.FB
- Crombie, K. M., Brellenthin, A. G., Hillard, C. J., & Koltyn, K. F. (2018). Psychobiological responses to Aerobic exercise in individuals with posttraumatic stress disorder. Journal of Traumatic Stress, 31(1), 134–145. doi:10.1002/jts.22253
- Davis, A. A., Zachry, C. E., & Berke, D. S. (2021). Physical interventions for the treatment of trauma and stressor-related disorders: A comprehensive systematic review. Mental Health and Physical Activity, 20(December2020), 100401. doi:10.1016/j.mhpa.2021.100401
- Eidhof, M., Ter Heide, F., Boeschoten, M., & Olff, M. (2018). Internationale Trauma Vragenlijst: Zelfrapportage vragenlijst voor ICD-11 PTSS en CPTSS. Nederlandstalige versie. Uitgave Arq Psychotrauma Expert Groep, Diemen. Retrieved from http://www.psychotraumadiagnostics.centrum45.nl/
- Field, A. (2013). Discovering Statistics Using IBM SPSS Statistics (4th ed.). London, England: SAGE.
- Goldstein, L. A., Mehling, W. E., Metzler, T. J., Cohen, B. E., Barnes, D. E., Choucroun, G. J., Neylan, T. C. (2018). Veterans group exercise: A randomized pilot trial of an integrative exercise program for veterans with posttraumatic stress. Journal of Affective Disorders, 227(August 2017), 345–352. doi:10.1016/j.jad.2017.11.002
- Gordon, B. R., McDowell, C. P., Hallgren, M., Meyer, J. D., Lyons, M., & Herring, M. P. (2018). Association of efficacy of resistance exercise training with depressive symptoms meta-analysis and meta-regression: Analysis of randomized clinical trials. JAMA Psychiatry, 75(6), 566–576. doi:10.1001/jamapsychiatry.2018.0572
- Gordon, B. R., McDowell, C. P., Lyons, M., & Herring, M. P. (2017). The effects of resistance exercise training on anxiety: A meta-analysis and meta-regression analysis of randomized controlled trials. Sports Medicine, 47(12), 2521–2532. doi:10.1007/s40279-017-0769-0
- Gratz, K. L., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. doi:10.1023/B:JOBA.0000007455.08539.94
- Hall, K. S., Morey, M. C., Bosworth, H. B., Beckham, J. C., Pebole, M. M., Sloane, R., & Pieper, C. F. (2020). Pilot randomized controlled trial of exercise training for older veterans with PTSD. Journal of Behavioral Medicine, 43(4), 648–659. doi:10.1007/s10865-019-00073-w
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: The guilford press.
- Hegberg, N. J., Hayes, J. P., & Hayes, S. M. (2019). Exercise intervention in PTSD: A narrative review and rationale for implementation. Frontiers in Psychiatry, 10(March). doi:10.3389/fpsyt.2019.00133
- Jacquart, J., Dutcher, C. D., Freeman, S. Z., Stein, A. T., Dinh, M., Carl, E., & Smits, J. A. J. (2018). The effects of exercise on transdiagnostic treatment targets: A meta-analytic review. Behaviour Research and Therapy, November. doi:10.1016/j.brat.2018.11.007
- Lecrubier, Y., Sheehan, D. V., Weiller, E., Amorim, P., Bonora, I., Sheehan, K. H., Dunbar, G. C. (1997). The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry, 12(5), 224–231. doi:10.1016/S0924-9338(97)83296-8
- Morin, C. M., Belleville, G., Bélanger, L., & Ivers, H. (2011). The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep, 34(5), 601–608. doi:10.1093/sleep/34.5.601
- Neumann, A., Van Lier, P. A. C., Gratz, K. L., & Koot, H. M. (2010). Multidimensional assessment of emotion regulation difficulties in adolescents using the difficulties in emotion regulation scale. doi:10.1177/1073191109349579
- Nordbrandt, M. S., Sonne, C., Mortensen, E. L., & Carlsson, J. (2020). Trauma-affected refugees treated with basic body awareness therapy or mixed physical activity as augmentation to treatment as usual - A pragmatic randomised controlled trial. PLoS ONE, 15(3), 1–16. doi:10.1371/journal.pone.0230300
- Oaten, M., & Cheng, K. (2006). Longitudinal gains in self-regulation from regular physical exercise. British Journal of Health Psychology, 11(4), 717–733. doi:10.1348/135910706X96481
- Overbeek, T., Schruers, K., & Griez, E. (1999). MINI: Mini International Neuropsychiatric Interview, Dutch version 5.0. 0 (DSM-IV). Maastricht: Internal Publication University of Maastricht.
- Powers, M. B., Medina, J. L., Burns, S., Kauffman, B. Y., Monfils, M., Asmundson, G. J. G., … Smits, J. A. J. (2015). Exercise augmentation of exposure therapy for PTSD: Rationale and pilot efficacy data. Cognitive Behaviour Therapy, 44(4), 314–327. doi:10.1080/16506073.2015.1012740
- Ramos-Sanchez, C. P., Schuch, F. B., Seedat, S., Louw, Q. A., Stubbs, B., Rosenbaum, S., Vancampfort, D. (2021). The anxiolytic effects of exercise for people with anxiety and related disorders: An update of the available meta-analytic evidence. Psychiatry Research, 302, 114046. doi:10.1016/j.psychres.2021.114046
- Reid, K. J., Baron, K. G., Lu, B., Naylor, E., Wolfe, L., & Zee, P. C. (2010). Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Medicine, 11(9), 934–940. doi:10.1016/j.sleep.2010.04.014
- Reilly, T. J., MacGillivray, S. A., Reid, I. C., & Cameron, I. M. (2015). Psychometric properties of the 16-item quick inventory of depressive symptomatology: A systematic review and meta-analysis. Journal of Psychiatric Research, 60, 132–140. doi:10.1016/j.jpsychires.2014.09.008
- Rosenbaum, S., Sherrington, C., & Tiedemann, A. (2015). Exercise augmentation compared with usual care for post-traumatic stress disorder: A randomized controlled trial. Acta Psychiatrica Scandinavica, 131(5), 350–359. doi:10.1111/acps.12371
- Rosenbaum, S., Tiedemann, A., Sherrington, C., & van der Ploeg, H. P. (2014). Assessing physical activity in people with posttraumatic stress disorder: Feasibility and concurrent validity of the international physical activity questionnaire–short form and actigraph accelerometers. BMC Research Notes, 7(1), 576. doi:10.1186/1756-0500-7-576
- Rosenbaum, S., Vancampfort, D., Steel, Z., Newby, J., Ward, P. B., & Stubbs, B. (2015). Physical activity in the treatment of post-traumatic stress disorder: A systematic review and meta-analysis. Psychiatry Research, 230(2), 130–136. doi:10.1016/j.psychres.2015.10.017
- Scherr, J., Wolfarth, B., Christle, J. W., Pressler, A., Wagenpfeil, S., & Halle, M. (2013). Associations between Borg’s rating of perceived exertion and physiological measures of exercise intensity. European Journal of Applied Physiology, 113(1), 147–155. doi:10.1007/s00421-012-2421-x
- Schuch, F. B., Vancampfort, D., Richards, J., Rosenbaum, S., Ward, P. B., & Stubbs, B. (2016). Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. Journal of Psychiatric Research, 77, 42–51. doi:10.1016/j.jpsychires.2016.02.023
- Smits, J. A. J., Berry, A. C., Rosenfield, D., Powers, M. B., Behar, E., & Otto, M. W. (2008). Reducing anxiety sensitivity with exercise. Depression and Anxiety, 25(8), 689–699. doi:10.1002/da.20411
- Surís, A., Holder, N., Holliday, R., & Clem, M. (2016). Psychometric validation of the 16 Item Quick Inventory of Depressive Symptomatology Self-Report Version (QIDS-SR 16) in military veterans with PTSD. Journal of Affective Disorders, 202, 16–22. doi:10.1016/j.jad.2016.05.029
- Van Nieuwenhuizen, C., Schene, A. H., & Koeter, M. (2000). Manchester-verkorte Kwaliteit van Leven meting. (The Manchester-short assessment of quality of life). Eindhoven, the Netherlands, Institute of Mental Health Care Eindhoven.
- Van Woudenberg, C., Voorendonk, E. M., Bongaerts, H., Zoet, H. A., Verhagen, M., Lee, C. W., De Jongh, A. (2018). Effectiveness of an intensive treatment programme combining prolonged exposure and eye movement desensitization and reprocessing for severe post-traumatic stress disorder. European Journal of Psychotraumatology, 9(1), 1–10. doi:10.1080/20008198.2018.1487225
- Voorendonk, E. M., De Jongh, A., Rozendaal, L., & Van Minnen, A. (2020). Trauma-focused treatment outcome for complex PTSD patients: Results of an intensive treatment programme intensive treatment programme. European Journal of Psychotraumatology, 11(1), 1783955. doi:10.1080/20008198.2020.1783955
- Voorendonk, E. M., Sanches, S. A., De Jongh, A., & Van Minnen, A. (2019). Improvements in cardiorespiratory fitness are not significantly associated with post-traumatic stress disorder symptom reduction in intensive treatment. European Journal of Psychotraumatology, 10(1), 1. doi:10.1080/20008198.2019.1654783
- Voorendonk, E. M., Sanches, S. A., Mojet, M., De Jongh, A., & Van Minnen, A. (2021). Combining a single session of prolonged exposure with physical activity in patients with PTSD: The effect of sequence. Mental Health and Physical Activity, 21 (December 2020), 100417. doi:10.1016/j.mhpa.2021.100417
- Vujanovic, A. A., Arrindell, W. A., Bernstein, A., Norton, P. J., & Zvolensky, M. J. (2007). Sixteen-item anxiety sensitivity index confirmatory factor analytic evidence, internal consistency, and construct validity in a young adult sample from the Netherlands. Assessment, 14(2), 129–143. doi:10.1177/1073191106295053
- Warner, E., Spinazzola, J., Westcott, A., Gunn, C., & Hodgdon, H. (2014). The body can change the score: Empirical support for somatic regulation in the treatment of traumatized adolescents. Journal of Child & Adolescent Trauma, 237–246. doi:10.1007/s40653-014-0030-z
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The life events checklist for DSM-5 (LEC-5). In Instrument Available from the National Center for PTSD http://www.ptsd.va.gov.
- Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., … Marx, B. P. (2017). The clinician-administered PTSD scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395. doi:10.1037/pas0000486
- Whitworth, J. W., Craft, L. L., Dunsiger, S. I., & Ciccolo, J. T. (2017). Direct and indirect effects of exercise on posttraumatic stress disorder symptoms: A longitudinal study. General Hospital Psychiatry, 49(March), 56–62. doi:10.1016/j.genhosppsych.2017.06.012
- Whitworth, J. W., Nosrat, S., SantaBarbara, N. J., & Ciccolo, J. T. (2019a). Feasibility of resistance exercise for posttraumatic stress and anxiety symptoms: A randomized controlled pilot study. Journal of Traumatic Stress, 32(6), 977–984. doi:10.1002/jts.22464
- Whitworth, J. W., Nosrat, S., SantaBarbara, N. J., & Ciccolo, J. T. (2019b). High intensity resistance training improves sleep quality and anxiety in individuals who screen positive for posttraumatic stress disorder: A randomized controlled feasibility trial. Mental Health and Physical Activity, 16(April), 43–49. doi:10.1016/j.mhpa.2019.04.001
- Zalta, A. K., Held, P., Smith, D. L., Klassen, B. J., Lofgreen, A. M., Normand, P. S., … Karnik, N. S. (2018). Evaluating patterns and predictors of symptom change during a three-week intensive outpatient treatment for veterans with PTSD. BMC Psychiatry, 18(1), 1–15. doi:10.1186/s12888-018-1816-6
- Zepeda Méndez, M., Nijdam, M. J., Ter Heide, J. J. F., Van Der, A. N., & Olff, M. (2018). A five-day inpatient EMDR treatment programme for PTSD: Pilot study. European Journal of Psychotraumatology, 9(1), 1–10. doi:10.1080/20008198.2018.1425575
- Zingrone, N. L., & Alvarado, C. S. (2002). The Dissociative Experiences Scale-II: Descriptive statistics, factor analysis, and frequency of experiences. Imagination, Cognition and Personality, 21(2), 145–157.
- Zoellner, L. A., Feeny, N. C., & Bittinger, J. N. (2009). What you believe is what you want: Modeling PTSD-related treatment preferences for sertraline or prolonged exposure. Journal of Behavior Therapy and Experimental Psychiatry, 40(3), 455–467. doi:10.1016/j.jbtep.2009.06.001.What
- Zoet, H. A., Wagenmans, A., Van Minnen, A., & De Jongh, A. (2018). Presence of the dissociative subtype of PTSD does not moderate the outcome of intensive trauma- focused treatment for PTSD. European Journal of Psychotraumatology, 9(1), 1468707. doi:10.1080/20008198.2018.1468707