ABSTRACT
Background
Early Psychological First Aid (PFA) has been widely recommended for preventing posttraumatic stress disorder (PTSD). However, its lack of empirical evidence of safety and effectiveness has been criticized.
Objectives
To assess the effectiveness of PFA-ABCDE, an original PFA protocol, for preventing PTSD one month after the intervention and decreasing PTSD symptoms at one and six months of follow up.
Methods
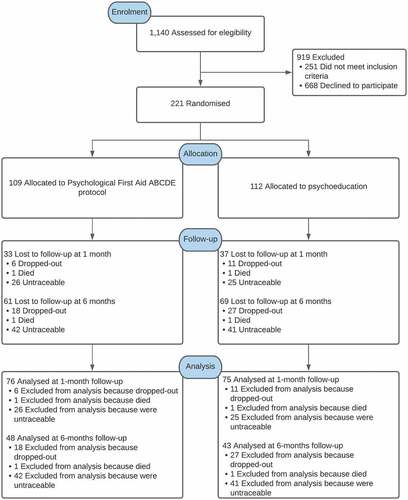
We assessed the eligibility of 1,140 adult survivors of recent trauma (≤ 72 hours) consulting five emergency departments in Chile. Two hundred twenty-one were randomized to receive either PFA-ABCDE (active listening, breathing retraining, categorization of needs, referral to ancillary services, and psychoeducation) or only psychoeducation. We used the Composite International Diagnostic Interview (CIDI) to assess PTSD diagnosis. The Posttraumatic Checklist (PCL), the Beck Depression Inventory-II (BDI-II), and a 0–10 points analogue visual scale were used to assess PTSD symptoms, depressive symptoms, and immediate distress relief after the intervention.
Results
We found no difference between the experimental and control groups in the frequency of PTSD one month after the intervention (PFA-ABCDE = 23/76 [30.3%], psychoeducation = 18/75 [24.0%], adjusted odds ratio = 1.39, 95% confidence interval = 0.63–3.07, p = .408). Immediately after the intervention, participants who received PFA-ABCDE reported greater distress relief (PFA-ABCDE mean = 9.06, psychoeducation mean = 8.55, Cohen’s d = 0.30, p = .038). Fewer PTSD symptoms were reported by those who received PFA-ABCDE one month after the intervention (PFA-ABCDE mean = 36.26, psychoeducation mean = 43.62, Cohen’s d = 0.42, p = .033). We found no difference in depressive symptoms at one-month follow up (p = .713) nor in PTSD symptoms six months after the intervention (p = .986).
Conclusions
PFA-ABCDE does not prevent PTSD diagnosis, but it provides immediate distress relief and decreases PTSD symptoms in the short term.
HIGHLIGHTS
Experts recommend Psychological First Aid (PFA) to prevent PTSD.
Evidence of its effectiveness is lacking.
We set up a Randomized-Controlled Trial in 221 adults to assess if PFA-ABCDE, an original PFA protocol, prevents PTSD.
PFA-ABCDE decreased PTSD symptoms, but it did not prevent PTSD.
Antecedentes: Los Primeros Auxilios Psicológicos (PAP) han sido recomendados para prevenir el Trastorno de Estrés Postraumático (TEPT) en supervivientes de trauma. A pesar de su popularidad, la escasez de evidencia empírica sobre su seguridad y efectividad ha sido criticada.
Objetivos: Evaluar la efectividad de los PAP-ABCDE, un protocolo original de PAP, para prevenir el TEPT al mes de seguimiento y disminuir los síntomas de TEPT luego de uno y seis meses de seguimiento.
Métodos: Evaluamos elegibilidad de 1.140 adultos supervivientes de trauma reciente (≤ 72 horas) que consultaron cinco servicios de urgencia en Chile. Doscientos veintiún fueron aleatorizados a recibir PAP-ABCDE (escucha activa, reentrenamiento de la respiración, categorización de necesidades, derivación a redes de apoyo, y psicoeducación) o sólo psicoeducación. Utilizamos la Composite International Diagnostic Interview (CIDI) para evaluar el diagnóstico de TEPT. La Posttraumatic Checklist (PCL), la Beck Depression Inventory-II (BDI-II), y una escala visual análoga de 0-10 puntos fueron utilizadas para evaluar síntomas de TEPT, síntomas depresivos, y alivio inmediato de distrés luego de la intervención.
Resultados: No encontramos diferencia entre el grupo experimental y el grupo control en la frecuencia de TEPT un mes después de la intervención (PAP-ABCDE = 23/76 [30,3%], psicoeducación = 18/75 [24,0%], odds ratio ajustado = 1,39, intervalo de confianza 95% = 0,63-3,07, p = ,408). Inmediatamente después de la intervención los participantes que recibieron PAP-ABCDE reportaron un mayor alivio de distrés (media en PAP = 9,06, media en psicoeducación = 8,55, d de Cohen = 0,30, p = ,038). Menos síntomas de TEPT fueron reportados un mes después de la intervención por aquellos que recibieron PAP-ABCDE (media de PAP-ABCDE = 36,26, media de psicoeducación = 43,62, d de Cohen = 0,42, p = ,033). No encontramos diferencias en síntomas depresivos al mes de seguimiento (p = ,713) ni en síntomas de TEPT seis meses después de la intervención (p = ,986).
Conclusiones: Los PAP-ABCDE no previenen el diagnóstico de TEPT, pero brindan alivio inmediato del distrés y disminuyen la severidad de los síntomas del TEPT en el corto plazo.
背景: 早期心理急救 (PFA) 已被广泛推荐用于预防创伤后应激障碍 (PTSD)。然而, 其安全性和有效性的缺乏实证证据受到批评。
目的: 评估 PFA-ABCDE (原始 PFA 方案) 在干预后 1 个月预防 PTSD 并在随访 1 个月和 6 个月时减少 PTSD 症状的有效性。
方法: 我们评估了 1140 名咨询了智利五个急诊科的近期创伤 (≤ 72 小时) 成年幸存者的资格。 221 人随机接受 PFA-ABCDE (积极倾听, 呼吸再训练, 需求分类, 转介辅助服务和心理教育) 或仅接受心理教育。我们使用复合国际诊断访谈 (CIDI) 来评估 PTSD 诊断。创伤后检查表 (PCL), 贝克抑郁量表-II (BDI-II) 和 0-10 分模拟视觉量表用于评估干预后的 PTSD 症状, 抑郁症状和即时痛苦缓解。
结果: 我们发现干预后 1 个月的 PTSD 发生率在实验组和对照组之间没有差异 (PFA-ABCDE = 23/76 [30.3%], 心理教育 = 18/75 [24.0%], 调整优势比 = 1.39, 95% 置信区间 = 0.63-3.07, p= .408)。干预一结束, 接受 PFA-ABCDE 的参与者报告了更大的痛苦缓解 (PFA-ABCDE 平均值 = 9.06, 心理教育平均值 = 8.55, Cohen’s d= 0.30, p= .038) 。干预后一个月接受 PFA-ABCDE 的患者报告的 PTSD 症状较少 (PFA-ABCDE 平均值 = 36.26, 心理教育平均值 = 43.62, Cohen’s d= 0.42, p= .033) 。我们发现在 1 个月的随访中抑郁症状 (p= .713) 和干预后 6 个月的 PTSD 症状 (p= .986) 没有差异。
结论: PFA-ABCDE 不能预防 PTSD 诊断, 但它可以立即缓解痛苦并在短期内减轻 PTSD 症状。
1. Introduction
More than 70% of the world’s population have experienced a traumatic event in their life, such as an accident, a sudden death, a loved one being harmed, or sexual assault. Almost one-third have undergone four or more of these incidents (Benjet et al., Citation2016). Trauma survivors have an increased risk of developing mental disorders such as posttraumatic stress disorder (PTSD), anxiety disorders, depression, or psychosis (Auxéméry, Citation2018). For example, in a sample of 1,084 patients hospitalized for traffic accidents in Australia, 22% developed a new psychiatric disorder after one year of follow-up (Bryant et al., Citation2010).
PTSD can be particularly pernicious. In the US National Comorbidity Survey, PTSD increased the odds of teenage childbearing, high school or college failure, marital instability, and unemployment by 30%, 40%, 60%, and 150%. Moreover, prior PTSD raised the odds of a subsequent first onset suicide attempt by 600% (Kessler, Citation2000). PTSD symptoms tend to follow a chronic course. In a follow-up of participants from the National Comorbidity Survey, only one-third of those who develop PTSD recovered after one year. Ten years after the exposure, one-third were still symptomatic (Kessler, Sonnega, Bromet, Hughes, & Nelson, Citation1995).
Multiple experts and institutions have recommended Psychological First Aid (PFA) early after trauma for preventing PTSD (Bisson & Lewis, Citation2009; Guidelines for the management of conditions specifically related to stress; Hobfoll et al., Citation2007; Psychological First Aid (PFA) Field Operations Guide: 2nd Edition, Citation2021; Psychological First Aid: A guide to supporting people affected by disaster, Citation2021). Although there is no single definition and protocol for PFA (Bisson & Lewis, Citation2009; Shultz & Forbes, Citation2014), it has been conceptualized as the provision of ‘information, comfort, emotional care, and instrumental support to those exposed to an extreme event, with assistance provided in a stepwise fashion tailored to the person’s needs (Forbes et al., Citation2011). It has also been regarded as ‘documenting and operationalizing good common sense – those activities that sensible, caring human beings would do for each other anyway’ (during traumatic events), ‘avoiding those elements (notably expectations for a detailed incident review) that may be iatrogenic’ (Forbes et al., Citation2011). Importantly, besides preventing mental disorders, PFA seeks to contact survivors compassionately, promote their safety and calmness, assess their basic needs, offer them practical assistance and information, connect them with their support networks, support their adaptive coping, and link them with ancillary services (Brymer et al., Citation2006).
PFA is regarded as ‘evidence-informed’ (Bisson & Lewis, Citation2009). It is underpinned by ‘five essential elements’ of early interventions after trauma, proposed by Hobfoll and 19 mental health experts during a consensus conference convened in 2004. These five elements are 1) a sense of safety; 2) calming; 3) a of self and community efficacy; 4) connectedness; and 5) hope (Hobfoll et al., Citation2007). PFA does not promote early emotional ventilation, a mechanism that could exacerbate people’s stress reaction after trauma (Hobfoll et al., Citation2007). It does not need to be delivered by mental health specialists (Shultz & Forbes, Citation2014), making it attractive and affordable. Importantly, it is not considered a stand-alone intervention. Contrarily, it is considered an early, simple intervention to be articulated with other interventions in a continuum of care for people affected by traumatic events, including traumatic grief (Brymer et al., Citation2006; World Health Organization, World Trauma Foundation, World Vision International, Citation2011). PFA aims to reduce distress, foster short- and long-term adaptive functioning, and prevent long-term problems such as PTSD (Psychological First Aid (PFA) Field Operations Guide: 2nd Edition, Citation2021, Brymer et al., Citation2006). Through limiting further harm, meeting basic needs, adjusting risk appraisal, enhancing adaptive coping skills, facilitating emotional regulation, and increasing the perception of social support, PFA may regulate the stress response, mitigating its deleterious effect.
As stated in the Prevention and Treatment Guidelines of the International Society for Traumatic Stress Studies (ISTSS), there are only four interventions with emerging evidence of efficacy for preventing PTSD symptoms in adults: Group 512 Psychological Intervention Model (PIM), Single-Session EMDR, Brief Dyadic Therapy, and Self-Guided Internet-Based Intervention (International Society for Traumatic Stress Studies, Citation2019). PFA is not among them. Moreover, despite its popularity, there is a lack of controlled trials in ecologically valid settings assessing the effectiveness and safety of PFA for preventing PTSD (Bisson & Lewis, Citation2009; Dieltjens et al., Citation2014; Fox et al., Citation2012; Gartlehner et al., Citation2013; Roberts, Kitchiner, Kenardy, Lewis, & Bisson, Citation2019). Some experts have criticized the ease with which it has been adopted by the international community (Shultz & Forbes, Citation2014). Besides two RCTs that assessed the effect of PFA in a laboratory (Despeaux, Lating, Everly, Sherman, & Kirkhart, Citation2019; Everly, Lating, Sherman, & Goncher, Citation2016), the only controlled trial in an ecologically valid setting we are aware of is a study by McCart and colleagues (McCart, Chapman, Zajac, & Rheingold, Citation2020). In a sample of 172 crime survivors, they assessed the effect of PFA offered up to three weeks following a traumatic event. They did not find that PFA outperformed usual services regarding self-reported psychiatric symptoms during four months of follow-ups. In a post hoc analysis, the authors reported that survivors who received PFA showed significantly higher global functioning improvements. Unfortunately, PTSD symptoms were only assessed by a self-reported instrument not intended to diagnose PTSD. Therefore, evaluating the effect of PFA in preventing PTSD was not feasible.
Among other goals, PFA has been widely recommended for preventing PTSD. However, convincing evidence supporting this recommendation is lacking. In this study, we aim to assess the safety and effectiveness of PFA-ABCDE, an original PFA protocol, in preventing PTSD diagnosis. As such, we set up an RCT with people who experienced a recent unintentional traumatic event in an emergency room. We expected that PFA-ABCDE would reduce the frequency of PTSD one month after the intervention compared to the control group. We also anticipated that PFA-ABCDE would reduce immediate self-reported distress and decrease PTSD and depression symptoms up to six months after the traumatic event.
2. Methods
2.1. Design
This study was an RCT with two parallel intervention arms, designed to evaluate if PFA-ABCDE prevented PTSD one month after the intervention, compared to a control group. The study was carried out between November 2015 and August 2016 in Santiago, the capital city of Chile, a high-income country in South America with a population of 18,952,038 individuals (The World Bank, Citation2021). The protocol was registered in ClinicalTrials.gov, with the number 02608086, and was approved by the Pontificia Universidad Católica de Chile School of Medicine Ethics Committee, under the approval number 15–196.
We calculated the sample size to detect a PTSD diagnosis relative risk reduction of 50% one month after the intervention, with a statistical power of 80% and alpha 5%. We assumed a PTSD frequency of 34.4% in the control group, following Fullerton et al. (Fullerton et al., Citation2001). We calculated a sample size of 200 individuals with these parameters, which we increased by 10% (N = 220), assuming sample loss at follow up.
The primary outcome was the proportion of adults diagnosed with PTSD one month after the intervention. Secondary outcomes were the severity of PTSD symptoms one and six months after the intervention, depressive symptoms one month after the intervention, and the immediate distress change post-intervention.
2.2. Participants
Participants were 18 years old or older individuals exposed to a recent event (≤ 72 hours) that imposed an actual or threatened death or serious injury directly, as a witness, or as a close relative/friend who suddenly learned about a mishap that affected a loved one (DSM-5 A criterion) (American Psychiatric Association, Citation2013). Index events could include medical conditions if they were unexpected and severe according to the attending physician’s opinion (e.g. heart attacks, massive gastrointestinal bleedings, seizures, strokes). They could also include notifications of a loved one’s mishap if the accident or medical condition was recent (≤ 72 hours), unexpected, and imposed an actual or threatened death or serious injury, according to the attending physician’s opinion. We excluded survivors of intentional trauma (e.g. assault, rape, terrorist attacks) to increase the sample’s homogeneity, considering that intentional trauma has been associated with different conditional risks of PTSD than unintentional traumas (Santiago et al., Citation2013). Other exclusion criteria were non-Spanish language fluency, illiteracy, disruptive, agitated, or violent behaviour, lack of a personal telephone number, being under current resuscitation manoeuvres at the time of the intervention, having a close relative in imminent agony in the resuscitation room, not having memories about the traumatic event, loss of consciousness ≥ 5 min during the traumatic event, psychosis, suicide attempt, or having reported an active psychiatric disorder. Grieving was not an exclusion criterion, but we did not assess its presence. Inclusion and exclusion criteria were systematically assessed by providers with a checklist through direct questions to the participants, the technical opinion of the attending physician, and a review of medical records when available.
2.3. Providers
Providers were ten fourth or fifth-year undergraduate psychology students who voluntarily participated in the study. They received a monthly payment for their participation.
All providers underwent eight hours of PFA-ABCDE training and eight hours of instruction about the enrolment process (adding 16 hours), including role-playing about correctly approaching potential participants, the enrolment process, and the interventions themselves for the experimental and control conditions. The course included general topics of traumatic stress, foundations of psychological first aid, the rationale behind each step of the intervention protocol, warning signs, public social support programmes available at each hospital, details about every instrument’s use, and self-care. Its length and content are equivalent to other courses that have shown mixed results on the effectiveness of promoting the acquisition and retention of knowledge and skills to work in the aftermath of adversity (Horn et al., Citation2019; Kılıç & Şimşek, Citation2019; Sijbrandij et al., Citation2020). Only 70% of the students approved the course.
Each provider had a toolkit with printed versions of the intervention’s manual, psychoeducation handouts, and the instruments for data collection.
Providers received daily supervision from the research team members through regular face-to-face visits at the enrolling hospitals and via telephone.
2.4. Setting
The enrolment and interventions took place in the emergency department of five teaching hospitals. The interventions were implemented at the bedside for patients under medical assessment/procedures and in a quiet room for patients’ companions.
2.5. Enrolment
Each emergency room triage nurse was asked to notify the providers whenever they knew about a patient or companion experiencing significant psychological distress due to a life-threatening event (i.e. crying, screaming, yelling, whining). Then, providers carefully approached the candidates to offer them support and invited them to participate in the study, using a brief brochure explaining the intervention characteristics, benefits, and potential risks. Then inclusion and exclusion criteria were assessed. Those willing to be enrolled were asked to sign an informed consent document approved by each hospital’s ethics committee. Participants were then asked to complete a set of questionnaires on baseline demographic data, details about their recent traumatic event, and self-reported symptoms of depression after giving their consent.
2.6. Randomization
After completing the baseline questionnaires, participants were remotely assigned to one of the two interventions by a person outside the hospital, blind to any information about them. The allocation was made through a hidden randomization sequence of 400 digits, 0 or 1, equal proportion.
2.7. Intervention
We used an original PFA protocol designed by authors RF and PC in 2015 named ‘PAP-ABCDE’. It was inspired by the World Health Organization (WHO)’s definition of PFA (i.e. a ‘humane, supportive response to a fellow human being who is suffering and who may need support. It entails basic, non-intrusive pragmatic care with a focus on listening but not forcing talk, assessing needs and concerns, ensuring that basic needs are met, encouraging social support from significant others and protecting from further harm’) (Guidelines for the management of conditions specifically related to stress,). This definition is comparable to other widely accepted definitions (Bisson & Lewis, Citation2009; Shultz & Forbes, Citation2014).
Although the WHO definition of PFA inspired PAP-ABCDE, the three core actions of the WHO protocol (i.e. look, listen and link) (World Health Organization, World Trauma Foundation, World Vision International, Citation2011) were replaced by five steps recalled by the mnemonic ‘ABCDE’ to enhance its learning. Each letter represents a component of the intervention. Given that there is no single definition of PFA and that the PFA-ABCDE protocol satisfies all the components of widely accepted PFA definitions (Bisson & Lewis, Citation2009; Shultz & Forbes, Citation2014), including the one by the WHO, we consider it a comprehensive model of PFA.
The PFA-ABCDE protocol has been taught regularly as a continuing education programme in the Pontificia Universidad Católica de Chile School of Medicine (UC | Chile) since 2015. Its manual, handouts and a complete set of learning resources can be found free of charge in https://medicina.uc.cl/educacion-continua/pap-abcde/. It has been uptaken by several public and private institutions in Chile, Argentina, Peru, Colombia, Guatemala, Spain, and Brazil. Its manual has been translated into English and Portuguese and is available in preventionweb.net, the global knowledge-sharing platform for disaster risk reduction and resilience by the United Nations Disaster Risk Reduction programme (ABCDE psychological first aid application handbook: For individual and collective crises, Citation2021).
The PFA-ABCDE protocol is as follows:
A. Active listening (10–20 min). An uninterrupted listening period, withholding judgements, expressing interest, compassion, and empathy through open questioning, paraphrasing, and reflecting but not forcing the participant to talk.
B. Breathing retraining (5–10 min). A breathing technique that uses prolonged exhalation is offered to enhance calm for survivors in extreme distress. It is also used to model adaptive coping skills. The breathing technique is a component of Prolonged Exposure Therapy (Foa, Hembree, & Rothbaum, Citation2007). Additional calming skills such as ‘grounding’ or Jacobson’s progressive muscle relaxation are also considered and taught upon participant’s request or preference.
C. Categorization of needs (5–10 min). Assistance is given to promote awareness, identification, and prioritization of the survivor’s most immediate needs and concerns (e.g. communication with relatives, food, concerns about physical/mental/ethical topics, legal issues, orientation about health insurances and financial assistance, transportation, accessing social services). The provider supports the survivor in systematically assessing and prioritizing her needs and concerns, modelling a goal-oriented thinking style, and comforting by helping him recover control over the situation.
D. From the Spanish word ‘Derivación’ (referral) (5–10 min). It consists of referring survivors to those social support networks that best meet the needs identified in step C (e.g. contact with relatives, access to a telephone, referral to the hospital’s social worker, legal advocacy, police, ambulances, or patient’s transportation). A leaflet with information about the different public health and social protection services available, including a 24/7 telephone service for health-related issues, is used to complement this step. Regular social support benefits are highlighted, and the importance of engaging in close contact with relatives and friends is discussed and encouraged. Those in need of further mental health clinical support are triaged and referred.
E. PsychoEducation (5–10 min). Delivery of information about the normal reactions to trauma (reassurance through normalization), adaptive coping skills for survivors and their families, including children and special groups (physical activity, sleep hygiene, substances avoidance, social engagement and experience sharing, relaxation techniques), self-monitoring of alert signs, myths, and misconceptions about traumatic stress, and where/how/when to ask for further assistance, all backed by brochures.
Providers were instructed to offer all the protocol’s steps to participants in one session. To meet the principles of flexibility and a client-centred approach endorsed by PFA, they were allowed to skip some steps or change their sequence according to the participants’ preferences or situational circumstances (e.g. rapid physical deterioration that granted an urgent intervention). We did not record sessions or assess adherence to the protocol.
The control group only received psychoeducation (step E of the ABCDE protocol). Therefore, the control intervention is an incomplete, shorter (5–10 minutes) fraction of the complete protocol (30–60 minutes) delivered face-to-face by the same psychology students, in the same emergency rooms, and with the same brochures, maximizing participants’ blinding to the intervention. Notably, two previous studies failed to find any effect of psychoeducation on preventing PTSD (Rose, Brewin, Andrews, & Kirk, Citation1999; Wong E, Marshall G, & Miles J, Citation2013). Hence, psychoeducation can be considered an active placebo, similar to the reduced drug dose placebo used in some pharmacological trials (Laursen, Hansen, Paludan-Müller, & Hróbjartsson, Citation2020).
The participants’ credibility on the active and control interventions was not assessed.
2.8. Data collection
After the intervention, participants were immediately asked to register on a visual analogue scale the change in their level of distress. They were later dismissed, and contact information was provided for follow up.
One month after the intervention, PTSD and depressive symptoms were assessed by a clinical psychologist through a face-to-face interview in an outpatient mental health clinic. Participants who repeatedly did not attend the face-to-face follow-up or were unable to commute were offered a telephone evaluation in which only the diagnosis of PTSD was assessed. Participants received monetary compensation ($14 US dollars) for their participation, aimed to cover the transportation expenses.
After six months, symptoms of PTSD were evaluated through self-report by trained telephone operators.
2.9. Blinding
The study’s hypothesis and interventions technical details were not disclosed to participants. As aforementioned, the same psychology students applied both the active and control interventions in the same emergency rooms through face-to-face meetings and using the same brochures. The clinical psychologist who assessed the participants one month after the intervention and the trained telephone operators who evaluated the participants were blind to the intervention assignment.
2.10. Instruments
2.10.1. Demographics
The demographic data was collected using items A1 to A11 of the WHO World Mental Health Composite International Diagnostic Interview 12-month, Spanish version 2.1 (CIDI) (World Health Organization, Citation1997), which obtains self-reported data regarding sex, age, marital status, number of children, and educational level.
2.10.2. PTSD diagnosis
To diagnose PTSD, we used section K, items K23 to K45 of the CIDI. The incident that led the participant to the emergency room was the index trauma. The CIDI is a structured clinical interview that has been widely used around the world. In a sample of 53 participants of the 1996 US Detroit Area Survey of Trauma, the CIDI demonstrated a sensitivity of 0.76, a specificity of 0.97, a positive predictive value of 0.75, a negative predictive value of 0.97, when using the Clinician-Administered PTSD Scale for DSM-IV (CAPS-DX) as the gold standard (Breslau, Kessler, & Peterson, Citation1998).
2.10.3. PTSD symptoms
The Spanish version of the Posttraumatic Stress Disorder Checklist specific version (PCL-S) was used to measure symptoms of PTSD in the last month, referring to the index trauma. The PCL-S is a 17-item self-report measure aimed to assess PTSD symptoms according to the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), through Likert questions with scores 1 (not at all) to 5 (extremely). The Chilean validation was carried out in a sample of adults from the Metropolitan Region affected by the 27 F 2010 earthquake, showing excellent internal consistency (0.89) (Vera-Villarroel, Zych, Celis-Atenas, Córdova-Rubio, & Buela-Casal, Citation2011).
2.10.4. Depression symptoms
We used the Spanish version of the Beck Depression Inventory-II (BDI-II) to assess symptoms of depression. The BDI-II is a self-report instrument with 21 items containing four options scoring 0 to 3 points. This instrument was validated in Chile in a sample of adolescents, obtaining a Cronbach’s alpha coefficient of 0.89–0.91 and a high correlation with the Millon Adolescent Clinical Inventory (Melipillán Araneda, Cova Solar, Rincón González, & Valdivia Peralta, Citation2008).
2.10.5. Self-reported distress change
To evaluate immediate distress change after the intervention, participants used a visual analogue scale with the question ‘In general terms, how do you feel right now after the intervention?’. Responses ranged from 0 (much worse) to 10 (much better).
2.11. Data and statistical analysis
We used Chi-square tests and Student’s t-test for independent samples to compare the experimental and control groups. The effect size for the difference of mean was calculated with Cohen’s d. A p-value < 0.05 (two-tails) was used as a criterion of statistical significance for all analyses. We used SPSS version 24 for Chi-square, Student’s t-test, and Cohen’s d calculations.
All analyses were carried out according to the allocated intervention, excluding missing data. We imputed missing data of PTSD symptoms one month after the intervention to test if the loss-to-follow-up results changed after imputations. Auxiliary variables were identified using a) mean differences between respondents and non-respondents, b) correlations between observed values between variables, and c) correlations between observed values and missingness. Imputation calculations were done in R 3.5.3. We used the mice package to generate 500 imputed datasets under a wholly conditional approach with predictive mean matching as the imputation method (Van Buuren, Citation2012). Visual inspection of trace plots and evaluation of the potential scale reduction factor indicate convergence with 70 burn-in iterations for each imputation.
As we found a significant correlation between baseline depression and PTSD symptoms at follow-up (at one-month r = 0.547, p < .001; at six-months r = 0.419, p < .001), coherent with previous reports (Sayed, Iacoviello, & Charney, Citation2015), baseline depression was included as a covariate for all the calculations. The intervention’s effect on the frequency of PTSD one month after trauma was also adjusted for the method of application of the CIDI (face-to-face interview or telephone) and baseline age. Age was included as a covariate since there was selective attrition of older participants in the control group at one-month follow-up (see supplementary material, Table 1). Because selective attrition of older and less educated participants was observed in the control group six months after the intervention (see supplementary material, Table 2), the intervention’s effect on PTSD symptoms was also adjusted for baseline age and education at this endpoint. We did not find significant differences between the experimental and the control groups regarding age, education, depressive symptoms, sex, civil status, or type of trauma in those who were followed-up to assess their PTSD symptoms one month after the intervention (see supplementary material, ), suggesting an absence of selective attrition. We did not include trauma type as a covariate because, besides intentional traumas (e.g. intimate partner or sexual violence, kidnapping), excluded in this study, other types of unintentional traumas do not show a significantly different conditional risk of PTSD (Kessler et al., Citation2017).
Table 1. Participant characteristics
Table 2. Proportion of participants with PTSD secondary to the index trauma one month after the intervention
Table 3. Distress relief, PTSD self-reported symptoms, and depressive self-reported symptoms after the intervention
3. Results
We assessed for eligibility a total of 1,140 individuals. Of them, 251 (22.0%) did not meet the enrolment criteria, and 668 (58.6%) declined to participate. Finally, 221 individuals were enrolled and randomized (19.4% of those screened) (). Almost all of them received their allocated intervention (n = 217, 98.2%), the same proportion in the experimental and control groups. One individual in each intervention arm dropped out immediately after randomization and before the intervention was implemented.
Randomized individuals had an average age of 48.6 years (SD = 16.4) and 11.1 years of formal education (SD = 4.3). More than half were female (n = 130, 58.8%). Most participants were married (n = 100, 46.9%) or single (n = 65, 29.4%). The most common traumatic event was a severe and sudden medical condition (n = 77, 34.8%) or suddenly learning about an imminent life-risk condition of a close relative (n = 49, 22.2%). Participants reported mild depressive symptoms at the baseline (average BDI-II score = 17.4, SD = 11.9). The baseline characteristics of the PFA-ABCDE and control groups were equivalent (see ).
One month after the intervention, we could only assess 151 individuals (68.3% of those enrolled; 65 [43.0%] face-to-face, and 86 [57%] by telephone). The main reason they declined the face-to-face interview was that they were out of town on vacations (most of the one-month follow-ups took place in January and February, midsummer in Chile). Almost a quarter of all participants were untraceable (n = 51, 23.1%). Two individuals died during the first month of follow-up (0.9%), and 17 (7.7%) voluntarily withdrew from the study. We did not find differences between groups in the proportion of participants that were evaluated face to face (28.4% versus 30.4%, χ2 = 0.098, df = 1, p = .755), through telephone (41.4% versus 36.6%; χ2 = 0.508; df = 1; p = .476), who died (0.9% versus 0.9%; χ2 = 0.000; df = 1; p = .985), who were untraceable (23.9% versus 22.3%; χ2 = 0.073; df = 1; p = .787), or who resigned the study (5.5% versus 9.8%; χ2 = 1.450; df = 1; p = .229), suggesting that attrition was similar between groups.
Six months after the intervention it was possible to assess only 91 participants (41.2% of those who were randomized). More than one third of the participants were untraceable (n = 83, 37.6%). In addition, 45 individuals (20.4%) resigned from the study. We did not find significant differences between groups in the proportion of individuals who resigned (16.5% versus 24.1%; χ2 = 1.964; df = 1; p = .161), who were untraceable (38.5% versus 36.6%; χ2 = 0.087; df = 1; p = .768), or who died (0.9% versus 0.9%; χ2 = 0.000; df = 1; p = .985), suggesting a similar attrition between groups.
3.1. Intervention effect
No significant effect was found in the frequency of PTSD diagnosis one month after the intervention (30.3% in the experimental group, 24.0% in the control group, adjusted odds ratio = 1.39, 95% confidence interval = 0.63–3.07, p = .408) (see ). Participants in the experimental group reported a higher immediate distress relief after the intervention (PFA mean = 9.06, psychoeducation mean = 8.55, mean difference = 0.51, adjusted mean difference = 0.51, Cohen’s d = 0.30, p = .038). They also presented fewer PTSD symptoms at one-month follow-up (PFA-ABCDE mean = 36.26, psychoeducation mean = 43.62, adjusted mean difference = 7.23, Cohen’s d = 0.42, p = .033) (see ). The difference of PTSD symptoms one month after the intervention remained significant after multiple imputations of missing data (p = .044) (see Supplementary material, Table 4). We did not find a significant difference of depressive symptoms at one-month follow-up (p = .713), nor PTSD symptoms at six-months follow-up (p = .986).
4. Discussion
PFA has emerged as the mainstay for early psychological intervention after extreme events (Shultz & Forbes, Citation2014). In the present study, we predicted that PFA-ABCDE, an original protocol of PFA, would prevent the emergence of PTSD one month after a traumatic event compared to a control group; however, we did not find evidence for its effectiveness. Nevertheless, PFA-ABCDE was associated with higher emotional distress relief immediately after the intervention and lower self-reported PTSD symptoms one-month post-trauma. No effects were found on PTSD symptoms six months post-trauma, although the very high attrition rate at this endpoint precludes any inference. We discuss these findings regarding the study’s methodological characteristics and putative mechanisms of PTSD prevention.
PFA-ABCDE was designed to satisfy the most accepted PFA definitions (Bisson & Lewis, Citation2009; Guidelines for the management of conditions specifically related to stress; Shultz & Forbes, Citation2014). Its steps were deliberately formulated to operationalize all the components of valid PFA definitions (i.e. ‘basic, non-intrusive pragmatic care’; ‘a focus on listening but not forcing talk’; ‘assessing needs and concerns’; ‘ensuring that basic needs are met’; ‘encouraging social support from significant others’; ‘protecting from further harm’ (Guidelines for the management of conditions specifically related to stress); ‘information, comfort, emotional care’; and ‘assistance provided in a stepwise fashion tailored to the person’s needs’ (Shultz & Forbes, Citation2014)). PFA-ABCDE has been taught regularly in UC | Chile since 2015, and several public and private institutions in Chile and abroad have uptaken it. Hence, we believe that PFA-ABCDE can be considered a comprehensive model of PFA, and that the knowledge obtained through its study can be arguably extended to the PFA field in general.
Among the methodological aspects, our study excluded survivors of intentional trauma, who have a higher risk of developing PTSD than unintentional trauma survivors (Santiago et al., Citation2013). Hence, individuals in our study could have lower PTSD risk overall and higher natural recovery rates, making detecting a significant effect of PFA-ABCDE more difficult. For example, in a recent study with survivors of recent trauma, researchers failed to replicate a previous RCT that showed that three 60-min sessions of prolonged exposure outperformed an assessment-only control on preventing PTSD symptoms (Maples‐Keller et al., Citation2020). One explanation was a lower proportion of survivors of sexual assault, a population with a significant incidence of PTSD, in the second study. Consequently, some authors have asserted that selecting individuals with a higher risk of PTSD will be crucial in future studies (Maples‐Keller et al., Citation2020). On the other hand, even in a sample of intentional trauma survivors, McCart et al. (McCart et al., Citation2020) did not find that PFA decreases PTSD symptoms. Therefore, it is questionable if sampling only high-risk survivors necessarily would have allowed us to find a significant effect.
Another factor that could explain why we failed to prove that PFA-ABCDE prevents PTSD is insufficient intervention dosing. We provided a single session of PFA-ABCDE, while PFA guidelines do not preclude more sessions when needed. However, there is emerging evidence showing that single session immediate interventions such as EMDR (Chiorino et al., Citation2020), Group 512 PIM (Wu et al., Citation2012), or Tetris (Iyadurai et al., Citation2018) could effectively reduce PTSD symptoms. Moreover, in the McCart et al. (McCart et al., Citation2020) study, two to three PFA sessions did not reduce PTSD symptoms. A recent study failed to find a meaningful difference between one or three immediate, prolonged exposure sessions (Maples‐Keller et al., Citation2020). Thus, it is uncertain if more sessions would necessarily increase the effectiveness of PFA-ABCDE or any early intervention for preventing PTSD. Moreover, including additional PFA-ABCDE sessions would have undermined the ecological validity of the study because PFA is usually implemented in one helping contact. Future studies assessing the dose-response effect of PFA could clarify this issue.
There are a few aspects to consider regarding the putative mechanisms of PTSD prevention. It has been postulated that traumatic memories consolidate during the first hours after trauma. This period offers a unique window of opportunity to disrupt traumatic memories’ consolidation (the ‘Golden Hours’) (Zohar, Sonnino, Juven-Wetzler, & Cohen, Citation2009). Some neuroscience studies show that memories would be malleable for approximately six hours from their acquisition (Nader, Schafe, & LeDoux, Citation2000). Other studies show that disrupting the first sleep after aversive stimulation can disrupt intrusive memories (Porcheret, Holmes, Goodwin, Foster, & Wulff, Citation2015). Our study enrolled patients with traumatic experiences that occurred up to 72 hours earlier. Hence, it is probable that in a significant proportion of our sample, the intervention was administered long after the presumed window of opportunity was closed. Unfortunately, we did not measure the precise amount of time between the traumatic event and the intervention. Consequently, assessing this effect was not feasible. Nonetheless, several promising early interventions, such as Brief dyadic cognitive-behavioural therapy (Brunet, Des Groseilliers, Cordova, & Ruzek, Citation2013), Internet guided self-help (Mouthaan et al., Citation2013), Intensive care diaries (Jones et al., Citation2010), Group 512 PIM (Wu et al., Citation2012), and EMDR-PRECI (Jarero, Artigas, & Luber, Citation2011), started a few days and even weeks after trauma. Furthermore, some evidence shows that long-term memories can be modified by disrupting their reconsolidation or enhancing extinction (Careaga, Girardi, & Suchecki, Citation2016). Consequently, whether waiting for more than 24 hours to use PFA moderates its effect is still an open question requiring further investigation.
It is questionable if PFA-ABCDE’s lack of PTSD evidence-based psychotherapies’ common factors components, such as imaginal exposure, cognitive processing, targeting of emotions, or memory processing (Schnyder et al., Citation2015), may have affected its effectiveness in preventing PTSD. Immediate interventions occur when PTSD has not yet been established, and the neurobiological underpinnings of PTSD prevention and treatment seem to be different (Careaga et al., Citation2016). For example, a promising early intervention such as Tetris (Iyadurai et al., Citation2018) does not include any of the aforementioned common factors, suggesting that these components could be dispensable in early interventions. On the other hand, debriefing, an intervention including several components of the evidence-based therapies for PTSD, has failed to prove its effectiveness in preventing PTSD (Roberts et al., Citation2019). Consequently, it remains unclear whether the absence of common factors of evidence-based PTSD therapies could negatively impact the effectiveness of PFA-ABCDE.
Visual elements occupy a significant part of the intrusions in PTSD (Brewin, Citation2014). Experiments in cognitive neuroscience show that visuospatial tasks can interfere with encoding visual elements of traumatic experiences, decreasing intrusion (Kavanagh, Freese, Andrade, & May, Citation2001). It has been hypothesized that the divided attention between a recent traumatic memory and another simultaneous task, especially visuospatial, would ‘tax’ the working memory, interfering with memory consolidation (van den Hout, Eidhof, Verboom, Littel, & Engelhard, Citation2014). This hypothesis is consistent with clinical findings, which show that immediate interventions with visuospatial components, such as EMDR or Tetris, could reduce PTSD symptoms up to three months after trauma (Gil-Jardiné et al., Citation2018; Iyadurai et al., Citation2018). However, other early interventions with emerging evidence, such as Group 512 PIM (Wu et al., Citation2012), Brief dyadic cognitive-behavioural therapy (Brunet et al., Citation2013), or Internet guided self-help (Mouthaan et al., Citation2013), do not include visual elements, so they do not appear to be indispensable. The contribution of adding visuospatial tasks to PFA-ABCDE is a potential area of exploration.
Our results must be interpreted considering our study’s methodological limitations, mostly high attrition, limited external validity due to excluding survivors of intentional trauma, and lack of control of experimental conditions. Selective attrition cannot be ruled out. However, most of our analyses suggest that this did not occur. All the analyses were adjusted for variables with evidence of selective attrition to minimize bias. Furthermore, the statistical analysis of PTSD symptoms one month after the intervention was complemented with imputed missing data, confirming the results. As the conditional risk of PTSD has shown to be higher in victims of intentional trauma, we excluded them, limiting the generalizability of our findings in that group (Santiago et al., Citation2013). Lacking control of the time elapsed between the index trauma and the intervention, the type of trauma, and the presence of grief, missing information about additional interventions during follow-up, absence of an assessment of the perceived credibility of the two interventions, and missing session records to evaluate adherence to the protocol, protocol modifications, and the duration of the intervention are significant limitations that also need to be considered.
Strengths of this study include a randomized-controlled trial design, use of an active control intervention, good sample size, use of validated instruments and interviews to assess PTSD symptoms and diagnosis, a 6-month follow-up assessment, assessors blind to the intervention condition, balanced participation of males and females, ongoing supervision of PFA providers, recruitment in hospital emergency rooms where many trauma survivors present for assistance, and delivery of both the active and control interventions by the same providers, who received an ecologically-valid training. Moreover, this study demonstrates the feasibility of conducting RCTs of PFA in emergency room settings. According to our knowledge, this is the first RCT investigating the effectiveness of PFA for preventing PTSD diagnosis, extending the findings of a previous controlled trial that tested its effect on PTSD symptoms (McCart et al., Citation2020). We found that PFA-ABCDE reduced immediate distress after the intervention and lowered self-reported PTSD symptoms one-month post-trauma. This finding is remarkable considering that we used an active control (i.e. psychoeducation), a design that can make it more difficult to find a significant effect. It remains crucial to assess whether fewer PTSD symptoms can help survivors be more amenable to additional treatments, including seeking ancillary services.
The theoretical underpinnings of the controversy between categorical and dimensional assessment of mental illnesses (i.e. ‘the relationships between predictors and syndromes of psychological distress are more accurately captured in statistical models that specify dimensional rather than categorical representations of distress’) (Kessler, Citation2002) may have accounted for the different results that we obtained assessing PTSD with the CIDI (categorical) and the PCL (dimensional).
The simplicity of PFA-ABCDE and its lack of adverse events suggest it may be safe and suitable for wide dissemination. Assessing an optimal training schema remains crucial to guarantee proper implementation, considering that one-day training has received criticism on its capacity to promote the acquisition of goal PFA competencies (Horn et al., Citation2019).
Given the paucity of evidence on PFA and the current trial’s limited scope, it is imperative to replicate our study across several settings and to include intentional trauma survivors. It will also be crucial to adopt adequate procedures to avoid attrition. Future studies should assess if PFA in general, and PFA-ABCDE in particular, facilitates access to ancillary services, promotes appropriate mental health self-seeking, enhances social connection, meets basic needs, and limits unadaptive coping behaviours (e.g. self-medication, alcohol consumption, or poor sleep hygiene). These are essential objectives of PFA besides PTSD prevention that were not assessed in this study. Furthermore, assessing PFA’s effect on these and other phenomena such as the perception of social support, risk appraisal, emotional regulation and harm prevention could clarify its putative mechanisms of action. Controlling experimental variables such as time elapsed between trauma and intervention and adherence to the intervention protocol will be critical. The presence of grief should also be controlled, considering that it could elicit distinct cognitive correlations than traumatic events without a loss (Smith, Ehlers, & Sar, Citation2021), moderating PFA’s effect. Furthermore, it may be worth investigating if combining PFA with other promising interventions such as Tetris or corticosteroids enhances its effect.
Although PFA-ABCDE does not prevent PTSD, it decreases PTSD symptoms in the short term and elicits immediate distress relief after the interventions. Furthermore, it seems to be a safe intervention for survivors of unintentional trauma, as they did not exhibit a worsening of symptoms. Consequently, we still recommend PFA-ABCDE for people affected by recent traumatic events. Caution should be taken to avoid unrealistic expectations about PFA as an effective intervention for preventing PTSD diagnosis.
Supplemental Material
Download MS Word (35.2 KB)Acknowledgments
To Hospital del Trabajador de Santiago, Hospital Dr. Sótero del Río, Hospital Padre Hurtado, Hospital Barros Luco Trudeau, and Hospital Clínico UC, for hosting this study. To Nicolás Crossley, MD, PhD, FRCPych; Constanza Caneo, MD, MSc; Luis Flores, MD, PhD; and Juan Ignacio Reculé, MD, for their thoughtful suggestions during the reviewing of this manuscript. To Miss. Eleanore Henderson, for her native-English edition of this paper.
Supplemental data
Supplemental data for this article can be accessed here.
Disclosure statement
Dr. Rodrigo Figueroa and Dr. Humberto Marín reports that they earn professional fees for their directive and teaching work in the “Psychological First Aid ABCDE course” at the Pontificia Universidad Católica de Chile School of Medicine. No potential conflict of interest was reported by authors Paula F. Cortés, Alvaro Vergés, Rodrigo Gillibrand, and Paula Repetto.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to information that could compromise the privacy of research participants.
Additional information
Funding
References
- ABCDE psychological first aid application handbook: For individual and collective crises. (2021, December 9). PreventionWeb [Internet]. Retrieved from https://www.preventionweb.net/publication/abcde-psychological-first-aid-application-handbook-individual-and-collective-crises
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
- Auxéméry, Y. (2018, May). Post-traumatic psychiatric disorders: PTSD is not the only diagnosis. La Presse Médicale, 47(5), 423–14. doi:10.1016/j.lpm.2017.12.006
- Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., & Koenen, K. C. (2016, Jan). The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327–343. doi:10.1017/S0033291715001981
- Bisson, J. I., & Lewis, C. (2009). Systematic review of psychological first aid. Commissioned by World Health Organization. Geneva, Switzerland; Cardiff, Wales: Cardiff University; and World Health Organization.
- Breslau, N., Kessler, R., & Peterson, E. L. (1998, August). Post-traumatic stress disorder assessment with a structured interview: Reliability and concordance with a standardized clinical interview. International Journal of Methods in Psychiatric Research, 7(3), 121–127. doi:10.1002/mpr.41
- Brewin, C. R. (2014, January). Episodic memory, perceptual memory, and their interaction: Foundations for a theory of posttraumatic stress disorder. Psychological Bulletin, 140(1), 69–97. doi:10.1037/a0033722
- Brunet, A., Des Groseilliers, I. B., Cordova, M. J., & Ruzek, J. I. (2013, December). Randomized controlled trial of a brief dyadic cognitive-behavioral intervention designed to prevent PTSD. European Journal of Psychotraumatology, 4(1), 21572. doi:10.3402/ejpt.v4i0.21572
- Bryant, R. A., O’Donnell, M. L., Creamer, M., McFarlane, A. C., Clark, C. R., & Silove, D. (2010, March). The psychiatric sequelae of traumatic injury. American Journal of Psychiatry, 167(3), 312–320. doi:10.1176/appi.ajp.2009.09050617
- Brymer, M., Jacobs, A., Layne, C., Pynoos, R., Ruzek, J., Steinberg, A. Vernberg, E., Watson, P . (2006). Psychological first aid field operations guide. Washington, DC: National Child Traumatic Stress Network and National Center for PTSD.
- Careaga, M. B. L., Girardi, C. E. N., & Suchecki, D. (2016, December). Understanding posttraumatic stress disorder through fear conditioning, extinction and reconsolidation. Neuroscience & Biobehavioral Reviews, 71, 48–57. doi:10.1016/j.neubiorev.2016.08.023
- Chiorino, V., Cattaneo, M. C., Macchi, E. A., Salerno, R., Roveraro, S., Bertolucci, G. G., … Fernandez, I. (2020, July). The EMDR recent birth trauma protocol: A pilot randomised clinical trial after traumatic childbirth. Psychology & Health, 35(7), 795–810. doi:10.1080/08870446.2019.1699088
- Despeaux, K. E., Lating, J. M., Everly, G. S., Sherman, M. F., & Kirkhart, M. W. (2019, August). A randomized controlled trial assessing the efficacy of group psychological first aid. Journal of Nervous & Mental Disease, 207(8), 626–632. doi:10.1097/NMD.0000000000001029
- Dieltjens, T., Moonens, I., Van Praet, K., De Buck, E., Vandekerckhove, P., & Matsuoka, Y. (2014, December). A systematic literature search on psychological first aid: Lack of evidence to develop guidelines. PLoS ONE, 9(12), e114714. doi:10.1371/journal.pone.0114714
- Everly, G. S., Lating, J. M., Sherman, M. F., & Goncher, I. (2016, March). The potential efficacy of psychological first aid on self-reported anxiety and mood: A pilot study. Journal of Nervous & Mental Disease, 204(3), 233–235. doi:10.1097/NMD.0000000000000429
- Foa, E., Hembree, E., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences therapist guide. New York: Oxford University Press.
- Forbes, D., Lewis, V., Varker, T., Phelps, A., O’Donnell, M., Wade, D. J., … Creamer, M. (2011). Psychological first aid following trauma: Implementation and evaluation framework for high-risk organizations. Psychiatry, 74(3), 224–239. doi:10.1521/psyc.2011.74.3.224
- Fox, J. H., Burkle, F. M., Bass, J., Pia, F. A., Epstein, J. L., & Markenson, D. (2012, Oct). The effectiveness of psychological first aid as a disaster intervention tool: Research analysis of peer-reviewed literature from 1990-2010. Disaster Medicine and Public Health Preparedness, 6(3), 247–252. doi:10.1001/dmp.2012.39
- Fullerton, C. S., Ursano, R. J., Epstein, R. S., Crowley, B., Vance, K., Kao, T. C., … Baum, A. (2001, September). Gender differences in posttraumatic stress disorder after motor vehicle accidents. American Journal of Psychiatry, 158(9), 1486–1491. doi:10.1176/appi.ajp.158.9.1486
- Gartlehner, G., Forneris, C. A., Brownley, K. A., Gaynes, B. N., Sonis, J., and Coker-Schwimmer, E. Jonas, D. E., Greenblatt, A., Wilkins, T. M., Woodell, C. L., & Lohr, K. N . (2013). Interventions for the Prevention of Posttraumatic Stress Disorder (PTSD) in adults after exposure to psychological trauma. Rockville (MD): Agency for Healthcare Research and Quality (US).
- Gil-Jardiné, C., Evrard, G., Al Joboory, S., Tortes Saint Jammes, J., Masson, F., Ribéreau-Gayon, R., … Lagarde, E. (2018, May 26). Emergency room intervention to prevent post concussion-like symptoms and post-traumatic stress disorder. A pilot randomized controlled study of a brief eye movement desensitization and reprocessing intervention versus reassurance or usual care. Journal of Psychiatric Research, 103, 229–236. doi:10.1016/j.jpsychires.2018.05.024
- Hobfoll, S. E., Watson, P., Bell, C. C., Bryant, R. A., Brymer, M. J., Friedman, M. J., & Ursano, R. J. (2007). Five essential elements of immediate and mid-term mass trauma intervention: Empirical evidence. Psychiatry: Interpersonal and Biological Processes, 70(4), 283–315. doi:10.1521/psyc.2007.70.4.283; discussion 316
- Horn, R., O’May, F., Esliker, R., Gwaikolo, W., Woensdregt, L., Ruttenberg, L., & Ager, A. (2019, May 7). The myth of the 1-day training: The effectiveness of psychosocial support capacity-building during the Ebola outbreak in West Africa. Global Mental Health, 6, e5. doi:10.1017/gmh.2019.2
- International Society for Traumatic Stress Studies. (2019). ISTSS PTSD prevention and treatment guidelines [Internet]. Available from https://istss.org/clinical-resources/treating-trauma/new-istss-prevention-and-treatment-guidelines
- Iyadurai, L., Blackwell, S. E., Meiser-Stedman, R., Watson, P. C., Bonsall, M. B., Geddes, J. R., & Holmes, E. A. (2018, Mar). Preventing intrusive memories after trauma via a brief intervention involving Tetris computer game play in the emergency department: A proof-of-concept randomized controlled trial. Molecular Psychiatry, 23(3), 674–682. doi:10.1038/mp.2017.23
- Jarero, I., Artigas, L., & Luber, M. (2011). The EMDR protocol for recent critical incidents: Application in a disaster mental health continuum of care context. Journal of EMDR Practice And, 9(4), 166–173. doi:10.1891/1933-3196.9.4.166
- Jones, C., Bäckman, C., Capuzzo, M., Egerod, I., Flaatten, H., Granja, C., … Rachel Group, T. (2010, September). Intensive care diaries reduce new onset post traumatic stress disorder following critical illness: A randomised, controlled trial. Critical Care, 14(5), R168. doi:10.1186/cc9260
- Kavanagh, D. J., Freese, S., Andrade, J., & May, J. (2001). Effects of visuospatial tasks on desensitization to emotive memories. British Journal of Clinical Psychology, 40(3), 267–280. doi:10.1348/014466501163689
- Kessler, R. C. (2000). Posttraumatic stress disorder: The burden to the individual and to society. The Journal of Clinical Psychiatry, 61(Suppl 5), 4–12; discussion 13. https://pubmed.ncbi.nlm.nih.gov/10761674/
- Kessler, R. C. (2002, Jun). The categorical versus dimensional assessment controversy in the sociology of mental illness. Journal of Health and Social Behavior, 43(2), 171. doi:10.2307/3090195
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., & Koenen, K. C. (2017, October). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. doi:10.1080/20008198.2017.1353383
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995, December). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060. doi:10.1001/archpsyc.1995.03950240066012
- Kılıç, N., & Şimşek, N. (2019, September 6). The effects of psychological first aid training on disaster preparedness perception and self-efficacy. Nurse Education Today, 83, 104203. doi:10.1016/j.nedt.2019.104203
- Laursen, D. R., Hansen, C., Paludan-Müller, A. S., & Hróbjartsson, A. (2020, July 28). Active placebo versus standard placebo control interventions in pharmacological randomised trials. Cochrane Database Syst Rev, 7. doi:10.1002/14651858.MR000055
- Maples‐Keller, J. L., Post, L. M., Price, M., Goodnight, J. M., Burton, M. S., Yasinski, C. W., & Rothbaum, B. O. (2020, May). Investigation of optimal dose of early intervention to prevent posttraumatic stress disorder: A multiarm randomized trial of one and three sessions of modified prolonged exposure. Depression and Anxiety, 37(5), 429–437. doi:10.1002/da.23015
- McCart, M. R., Chapman, J. E., Zajac, K., & Rheingold, A. A. (2020, August). Community-based randomized controlled trial of psychological first aid with crime victims. Journal of Consulting and Clinical Psychology, 88(8), 681–695. doi:10.1037/ccp0000588
- Melipillán Araneda, R., Cova Solar, F., Rincón González, P., & Valdivia Peralta, M. (2008, July). Propiedades Psicométricas del Inventario de Depresión de Beck-II en Adolescentes Chilenos. Terapia Psicológica, 26(1), doi:10.4067/S0718-48082008000100005
- Mouthaan, J., Sijbrandij, M., de Vries, G.-J., Reitsma, J. B., van de Schoot, R., Goslings, J. C., … Olff, M. (2013, August). Internet-based early intervention to prevent posttraumatic stress disorder in injury patients: Randomized controlled trial. Journal of Medical Internet Research, 15(8), e165. doi:10.2196/jmir.2460
- Nader, K., Schafe, G. E., & LeDoux, J. E. (2000, December). The labile nature of consolidation theory. Nature Reviews Neuroscience, 1(3), 216–219. doi:10.1038/35044580
- Porcheret, K., Holmes, E. A., Goodwin, G. M., Foster, R. G., & Wulff, K. (2015, July). Psychological effect of an analogue traumatic event reduced by sleep deprivation. Sleep, 38(7), 1017–1025. doi:10.5665/sleep.4802
- Psychological First Aid (PFA) Field Operations Guide: 2nd Edition. (2021, February 23). The national child traumatic stress network [Internet]. Retrieved from https://www.nctsn.org/resources/psychological-first-aid-pfa-field-operations-guide-2nd-edition
- Psychological First Aid: A guide to supporting people affected by disaster. (2021, February 23). APS [Internet]. Retrieved from https://www.psychology.org.au/for-the-public/Psychology-topics/Disasters/Recovering-from-disasters/Psychological-first-aid-supporting-people-disaster
- Roberts, N. P., Kitchiner, N. J., Kenardy, J., Lewis, C. E., & Bisson, J. I. (2019, December). Early psychological intervention following recent trauma: A systematic review and meta-analysis. European Journal of Psychotraumatology, 10(1), 1695486. doi:10.1080/20008198.2019.1695486
- Rose, S., Brewin, C. R., Andrews, B., & Kirk, M. (1999, July). A randomized controlled trial of individual psychological debriefing for victims of violent crime. Psychological Medicine, 29(4), 793–799. doi:10.1017/S0033291799008624
- Santiago, P. N., Ursano, R. J., Gray, C. L., Pynoos, R. S., Spiegel, D., Lewis-Fernandez, R., … Coyne, J. (2013, April). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLoS ONE, 8(4), e59236. doi:10.1371/journal.pone.0059236
- Sayed, S., Iacoviello, B. M., & Charney, D. S. (2015, Aug). Risk factors for the development of psychopathology following trauma. Current Psychiatry Reports, 17(8), 612. doi:10.1007/s11920-015-0612-y
- Schnyder, U., Ehlers, A., Elbert, T., Foa, E. B., Gersons, B. P. R., Resick, P. A., … Cloitre, M. (2015, August). Psychotherapies for PTSD: What do they have in common? European Journal of Psychotraumatology, 6(1), 28186. doi:10.3402/ejpt.v6.28186
- Shultz, J. M., & Forbes, D. (2014, March). Psychological first aid: Rapid proliferation and the search for evidence. Disaster Health, 2(1), 3–12. doi:10.4161/dish.26006
- Sijbrandij, M., Horn, R., Esliker, R., O’May, F., Reiffers, R., Ruttenberg, L., & Ager, A. (2020, January). The effect of psychological first aid training on knowledge and understanding about psychosocial support principles: A cluster-randomized controlled trial. International Journal of Environmental Research and Public Health, 17(2), 484. doi:10.3390/ijerph17020484
- Smith, K. V., Ehlers, A., & Sar, V. (2021, Apr). Prolonged grief and posttraumatic stress disorder following the loss of a significant other: An investigation of cognitive and behavioural differences. PLoS ONE, 16(4), e0248852. doi:10.1371/journal.pone.0248852
- Van Buuren, S. (2012). Flexible imputation of missing data (chapman & hall/CRC interdisciplinary statistics) (1st ed.). Boca Raton, FL: Chapman And Hall/CRC.
- van den Hout, M. A., Eidhof, M. B., Verboom, J., Littel, M., & Engelhard, I. M. (2014). Blurring of emotional and non-emotional memories by taxing working memory during recall. Cognition and Emotion, 28(4), 717–727. doi:10.1080/02699931.2013.848785
- Vera-Villarroel, P., Zych, I., Celis-Atenas, K., Córdova-Rubio, N., & Buela-Casal, G. (2011, August). Chilean validation of the Posttraumatic Stress Disorder Checklist-Civilian version (PCL-C) after the earthquake on February 27, 2010. Psychological Reports, 109(1), 47–58. doi:10.2466/02.13.15.17.PR0.109.4.47-58
- Wong E, C., Marshall G, N., & Miles J, N. V. (2013). Randomized controlled trial of a psychoeducational video intervention for traumatic injury survivors. Journal of Traumatic Stress Disorders & Treatment, 2(2). doi:10.4172/2324-8947.1000104
- The World Bank. (2021, March 10). Chile [Internet]. Available from https://data.worldbank.org/country/chile
- World Health Organization. (1997). The world mental health composite international diagnostic interview 12-months version 2.1. Washington DC: American Psychiatric Press.
- World Health Organization. (2013). Guidelines for the management of conditions specifically related to stress. Geneva: World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/85119/9789241505406_eng.pdf
- World Health Organization, World Trauma Foundation, World Vision International. (2011). Psychological first aid: Guide for field workers. WHO: Geneva. https://www.who.int/publications/i/item/9789241548205
- Wu, S., Zhu, X., Zhang, Y., Liang, J., Liu, X., Yang, Y., … Miao, D. (2012, Jul). A new psychological intervention: “512 Psychological Intervention Model” used for military rescuers in Wenchuan Earthquake in China. Social Psychiatry and Psychiatric Epidemiology, 47(7), 1111–1119. doi:10.1007/s00127-011-0416-2
- Zohar, J., Sonnino, R., Juven-Wetzler, A., & Cohen, H. (2009, January). Can posttraumatic stress disorder be prevented? CNS Spectrums, 14(1 Suppl 1), 44–51. https://pubmed.ncbi.nlm.nih.gov/19169193/