ABSTRACT
Background
Complex posttraumatic stress disorder (CPTSD) describes the results of complex, prolonged, and/or inescapable trauma, and is typified by avoidance, re-experiencing, sense of threat, affect dysregulation, negative self-concept, and interpersonal disturbances. Additionally, CPTSD is highly comorbid with other common psychopathologies.
Objectives
A study was conducted in a trauma-exposed UK Armed Forces Veteran population resident in Northern Ireland (N = 638, NI) to determine the prevalence of CPTSD and comorbid associations.
Methods
Data from the Northern Ireland Veterans Health and Wellbeing Study (NIVHWS), including self-report data describing traumatic stress, depression, anxiety, and suicidality, were used in a latent class analysis to identify distinct profiles of symptomology in the sample, and in a multinomial logistic regression to identify comorbidities associated with class membership.
Results
Three distinct classes emerged: a low endorsement ‘baseline’ class (36%), a ‘Moderate Symptomatic’ class (27%), and a high endorsement ‘Probable CPTSD’ class (37%). Both the Moderate Symptomatic and CPTSD classes were predicted by cumulative trauma exposure. Depression was highly comorbid (OR = 23.06 in CPTSD), as was anxiety (OR = 22.05 in CPTSD) and suicidal ideation (OR = 4.32 in CPTSD), with suicidal attempt associated with the CPTSD class (OR = 2.51).
Conclusions
Cases of probable CPTSD were more prevalent than cases of probable posttraumatic stress disorder (PTSD) without Difficulties in Self-Organisation (DSO) symptoms in a UK Armed Forces veteran sample, were associated with repeated/cumulative trauma, and were highly comorbid across a range of psychopathologies. Findings validate previous literature on CPTSD and indicate considerable distress and thus need for support in UK Armed Forces veterans resident in NI.
HIGHLIGHTS
CPTSD was more prevalent than PTSD in a UK Armed Forces veteran sample.
CPTSD was associated with repeated/cumulative trauma, and was highly comorbid across a range of psychopathologies.
These findings validate the previous literature on CPTSD
Antecedentes:El trastorno de estrés postraumático complejo (TEPT-C) describe los resultados de un trauma complejo, prolongado y/o inevitable; y se caracteriza por la presencia de evitación, re-experimentación, sensación de amenaza, desregulación afectiva, un autoconcepto negativo y alteraciones en las relaciones interpersonales. Adicionalmente, el TEPT-C es altamente comórbido con otras psicopatologías frecuentes.
Objetivos: Se realizó un estudio en una población de veteranos de las Fuerzas Armadas del Reino Unido expuestos a trauma residentes en Irlanda del Norte (N=638, NI) para determinar la prevalencia del TEPT-C y las asociaciones comórbidas.
Métodos: Los datos del Estudio de Salud y Bienestar en Veteranos de Irlanda del Norte (NIVHWS, por sus siglas en inglés), incluidos datos de auto-reportes describiendo la presencia de estrés traumático, depresión, ansiedad y suicidalidad, fueron utilizados en un análisis de clases latentes para identificar distintos perfiles de sintomatología en la muestra y en una regresión logística multinomial para identificar las comorbilidades asociadas con la pertenencia a cada clase.
Resultados: Surgieron tres clases distintas: una clase de “línea base” de bajo respaldo (36%), una clase de “sintomático moderado” (27%) y una clase de “TEPT-C probable” de alto respaldo (37%). La exposición acumulativa a trauma predijo tanto las clases de sintomático moderado como la del TEPT-C probable. La depresión fue altamente comórbida (OR=23.06 en TEPT-C), así como la ansiedad (OR=22.05 en TEPT-C) y la ideación suicida (OR=4.32 en TEPT-C), con intento de suicidio asociado a la clase de TEPT-C (OR=2.51).
Conclusiones: Los casos de TEPT-C probable fueron más prevalentes que los casos de trastorno de estrés postraumático (TEPT) sin síntomas de alteraciones en la autoorganización (AAO) en una muestra de veteranos de las Fuerzas Armadas del Reino Unido. Asimismo, los casos de TEPT-C probable se asociaron a la exposición a trauma repetido/acumulativo y fueron altamente comórbidos con una variedad de psicopatologías. Los hallazgos validan la literatura previa concerniente al TEPT-C e indican una angustia considerable y, por lo tanto, demuestran la necesidad de soporte en los veteranos de las Fuerzas Armadas del Reino Unido residentes en Irlanda del Norte.
背景: 复杂性创伤后应激障碍 (CPTSD) 描述了复杂、长期和/或不可避免的创伤的结果, 其典型特征是回避、再体验、威胁感、情感失调、消极的自我概念和人际交往障碍。此外, CPTSD 与其他常见的精神病高度并发。
目的: 在居住在北爱尔兰 (N=638, NI) 创伤暴露英国武装部队退伍军人中进行了一项研究, 以确定 CPTSD 的患病率及其与并发症的关联。
方法: 来自北爱尔兰退伍军人健康和福祉研究 (NIVHWS) 的数据, 包括描述创伤性应激、抑郁、焦虑和自杀的自我报告数据, 被用于潜在类别分析, 以确定样本中不同的症状剖面, 以及在多项逻辑回归中识别与类别成员相关的并发症。
结果: 出现了三个不同的类别: 低发“基线”类别 (36%)、“中度症状”类别 (27%) 和高发“可能 CPTSD”类别 (37%)。中度症状和 CPTSD 类别均可被累积创伤暴露预测。抑郁是高度共病(在 CPTSD 中 OR=23.06), 焦虑(在 CPTSD 中 OR=22.05)和自杀意念(在 CPTSD 中 OR=4.32)也如此, 自杀尝试与 CPTSD 类别相关(OR=2.51)。
结论: 在英国武装部队退伍军人样本中, 可能的 CPTSD 病例比没有自组织困难 (DSO) 症状的可能的创伤后应激障碍 (PTSD) 病例更普遍, 与反复/累积性创伤相关, 并且与一系列精神病理学广泛高度共病。研究结果验证了以往关于 CPTSD 的文献, 并表明在 NI 居住的英国武装部队退伍军人中有相当大的精神痛苦, 因此需要为其提供支持。
1. Introduction
A stressful or traumatic life event is generally accepted as the inceptor for post-traumatic stress disorder (PTSD) while repeated or sustained stress is associated with complex post-traumatic stress disorder (CPTSD), described by PTSD symptomology (re-experiencing, avoidance, and sense of threat) and Difficulties in Self-Organisation (DSO): emotional dysregulation, negative self-concept, and interpersonal disturbances (Cloitre, Citation2020). The International Classification of Diseases 11th Edition (World Health Organization, Citation2019) (ICD-11) recommends a diagnosis of CPTSD when an individual meets criteria for PTSD, has a history of prolonged/repeated stressors, and when DSO symptoms are present (Maercker et al., Citation2013). The 6-factor structural validity of CPTSD has been validated in community (Brewin et al., Citation2017) and trauma exposed populations (Frost, Vang, Karatzias, Hyland, & Shevlin, Citation2019; Hansen, Hyland, Armour, Shevlin, & Elklit, Citation2015), including in military veteran samples (Armour, Robinson, & Ross, Citation2021; Moderno, Nalipay, & Mordeno, Citation2019; Murphy et al., Citation2020), with a recent systematic review confirming both the 6-factor cluster model and a 2-factor (PTSD and DSO) model (Redican et al., Citation2021). While it has been suggested that latent analyses do not guarantee construct validity, as such techniques fit a model to data regardless of the salience of the model (Achterhof, Huntjens, Meewisse, & Kiers, Citation2019; Ford, Citation2020), others have suggested that diagnostic constructs should not rely on a single statistical method for validity and added that multiple methodologies have confirmed and re-confirmed CPTSD as clinically distinct from PTSD (Cloitre et al., Citation2020).
Latent analysis of symptomology in trauma exposed populations has largely shown a distinct difference between PTSD and CPTSD (Elklit, Hyland, & Shevlin, Citation2014; Folke, Nielsen, Andersen, Karatzias, & Karstoft, Citation2019; Karatzias et al., Citation2017; Vang, Nielsen, Auning-Hansen, & Elklit, Citation2020; Zerach, Shevlin, Cloitre, & Solomon, Citation2019) with models describing PTSD, CPTSD, and low symptom/baseline classes. However, the distinction between the two disorders is not always as clear (Folke et al., Citation2019) and ‘moderate symptom’ classes have emerged in study populations which do not exactly match PTSD/CPTSD symptom profiles but are experiencing distress (Böttche et al., Citation2018; Knefel, Garvert, Cloitre, & Lueger-Schuster, Citation2015). Additionally, several studies have found CPTSD to be more prevalent than PTSD in general populations (Cloitre et al., Citation2019; Hyland et al., Citation2021) and in veteran samples (Armour, Robinson, et al., Citation2021; Letica-Crepulja et al., Citation2020; Murphy et al., Citation2020; Zerach et al., Citation2019). Trauma-focused interventions have shown efficacy in reducing CPTSD distress and symptomology (Hébert & Amédée, Citation2020; Voorendonk, De Jongh, Rozendaal, & Van Minnen, Citation2020), including several specialised variants of cognitive behavioural therapy (CBT) (Eilers et al., Citation2021; Karatzias et al., Citation2019), a personalised approach utilising multiple practices to suit the individual is recommended (Cloitre, Citation2021). In veteran treatment-seeking populations, several phase-based interventions have shown positive results (Landes, Garovoy, & Burkman, Citation2013), though it has been noted that CPTSD symptomology may act as an additional barrier to help-seeking (Williamson et al., Citation2021).
PTSD is known to be comorbid with common psychopathologies (Currier, Foster, Karatzias, & Murphy, Citation2021) and the emerging body of literature suggests that CPTSD shares this characteristic, potentially to a greater degree (Armour, Citation2015). Individuals with CPTSD are more likely to report experiencing higher levels of anxiety and depression (Karatzias et al., Citation2019; Letica-Crepulja et al., Citation2020; Murphy, Karatzias, Busuttil, Greenberg, & Shevlin, Citation2021), suicidality (Hyland, Shevlin, Fyvie, & Karatzias, Citation2018; Karatzias et al., Citation2019), moral injury (Letica-Crepulja et al., Citation2020; Murphy et al., Citation2021), substance misuse and psychosis (Facer-Irwin, Karatzias, Bird, Blackwood, & MacManus, Citation2021), and alcohol misuse (Hitch, Toner, & Armour, Citation2020). The DSO elements of CPTSD overlap with symptomology of borderline personality disorder (BPD), which is also associated with trauma (Herman, Perry, & Van der Kolk, Citation1989), though recent studies have shown a clear delineation between the two in trauma exposed populations (Cloitre, Garvert, Weiss, Carlson, & Bryant, Citation2014; Frost et al., Citation2020; Frost, Hyland, Shevlin, & Murphy, Citation2020; Murphy et al., Citation2021), with the association being one of comorbidity.
While CPTSD has been investigated in other veteran populations, the Northern Ireland Veterans Health and Wellbeing Study (NIVHWS) is the first to examine the ethology and aetiology of CPTSD in the unique context of Northern Ireland. Operation Banner, the UK military involvement in Northern Ireland (NI) during a turbulent era commonly known as ‘The Troubles’, ran from 1969 through 2007 and of the estimated 40,500 individuals who participated, roughly 19,500 were native to NI in either the Royal Ulster Constabulary (RUC) or the Ulster Defence Regiment (Armour, Walker, et al., Citation2018) (UDR). Following the signing of the Good Friday Agreement in 1998, which led to the cessation of violence, reduced military operations, and the devolved NI government, being a military veteran has carried a stigma in many parts of NI, leading to much of this population being unwilling to self-disclose their status due to safety issues (Armour, Walker, Waterhouse-Bradley, Hall, & Ross, Citation2017; Armour, Waterhouse-Bradley, Ross, McLafferty, & Hall, Citation2018). The NIVHWS (N = 1,329) made headway into mapping the support needs of this community, including confirming the presence/prevalence of probable CPTSD in the sample (Armour, Robinson, et al., Citation2021) and identifying latent groups of comorbid disorders in those who meet diagnostic screening for CPTSD (Robinson, McGlinchey, & Armour, Citation2021).
It was evident that while the body of literature on CPTSD and associated comorbidities is growing, both in civilian and military contexts, very little formal research had been conducted in a NI veteran population. Previous studies describing CPTSD in this context did not cover the relationship between symptom profile and comorbidities, nor comorbidity likelihood. This study aimed to investigate the prevalence of probable CPTSD and associated comorbidities in UK Armed Forces veterans who are resident in NI. It was hypothesised that (i) probable CPTSD would be more prevalent than probable PTSD, (ii) distinct classes of PTSD symptomology, CPTSD/DSO symptomology, and low symptom/non-clinical would be present, (iii) the probable CPTSD symptom profile would be comorbid with anxiety, depression, and suicidality, and (iv) the likelihood of experiencing these comorbidities would be higher for those with probable CPTSD than probable PTSD.
2. Method
2.1. Sample
A total of N = 1,329 participants provided informed consent as part of the Northern Ireland Veterans Health and Wellbeing Study. For this study, pairwise deletion was used, with N = 307 participants removed as they did not endorse at least one trauma and a further N = 384 removed as they had 20% or more missing data across the key variables of interest (PTSD, CPTSD, suicidality, depression, and anxiety). Participants with less than 20% missing data across these variables were retained, with analyses in this study conducted on a variable-by-variable basis using cases with complete data. The sample size was specified separately for each analysis and the final eligible sample size was N = 638. Ethical approval was originally granted by Ulster University (REC/17/0031) with a confirmational approval granted by the Queen’s University Belfast Research Ethics Committee (EPS 19_156) on relocation on the Chief Investigator. All participants provided written consent.
2.2. Measures
Trauma exposure was measured using 17 items from 2 separate measures: 13 items comprising the Stressful Life Events Screening Questionnaire adapted for the Diagnostic and Statistical Manual 5 (Elhai et al., Citation2012) (SLESQ; DSM-5) and 4 items from the Life Events Checklist for DSM-5 (Weathers et al., Citation2013) (LEC-5). This combination of items was chosen to ensure a fully comprehensive trauma screen within this population, in line with the unique socio-political context of Northern Ireland, as together, the measures covered the spectrum of known trauma experiences specific to the region's conflict history as also utilised in McGlinchey, Ross, Murphy, Shorter, and Armour (Citation2021). These items were presented in binary format, with participants asked to select ‘yes’ if they had experienced any of the 17 specified stressful life events, and ‘no’ if they had not.
The International Trauma Questionnaire (Cloitre et al., Citation2018) (ITQ) was used to examine ICD-11 probable PTSD and CPTSD caseness and symptomatology. The ITQ consists of 6 items measuring PTSD (2 items each allocated to measuring the specific ICD-11 symptom clusters ‘re-experiencing’, ‘avoidance’, and ‘sense of threat’, with 3 items measuring functional impairment) and 6 items measuring DSO symptomology (2 items measuring each of the 3 ICD-11 symptom clusters for CPTSD, ‘affective dysregulation’, ‘negative self-concept’, and ‘interpersonal disturbances’). The scale contains a further 3 items measuring functional impairment in relation to CPTSD symptomology. Participants are asked to answer in relation to their experiences over the past month and rate the degree to which they were affected on a 5-point Likert scale ranging from 0–4 (‘not at all’, ‘a little bit’, ‘moderately’, ‘quite a bit’, and ‘extremely’). Meeting caseness for PTSD requires endorsement of a score of ≥2 for at least 1 of 2 symptoms from each of the 3 PTSD clusters, as well as a score of ≥2 in at least 1 functional impairment item. Similarly, meeting caseness for CPTSD requires meeting the criteria for PTSD, in addition to scoring ≥2 for at least 1 symptom from each of the 3 CPTSD clusters and 1 functional impairment item. As this measure was self-report, caseness for PTSD/CPTSD is considered probabilistic. Previous studies have demonstrated the reliability and validity of the scale (Cloitre et al., Citation2014; Letica-Crepulja et al., Citation2020), with a Cronbach’s alpha of α = 0.96 for the PTSD items, α = 0.96 for the CPTSD items and α = 0.98 for the total scale as used in this study.
Depression and Anxiety were measured using the Patient Health Questionnaire 9 (Kroenke, Spitzer, Williams, Monahan, & Löwe, Citation2007) (PHQ-9) and the Generalised Anxiety Questionnaire 7 (Kroenke, Spitzer, & Williams, Citation2001) (GAD-7) respectively. Regarding both scales, participants are asked to answer in relation to experiences of symptoms over the past 2 weeks using a 4-point Likert scale ranging from 0–4 (‘not at all’, ‘several days’, ‘more than half the days’, and ‘nearly every day’). For both measures, a score of 10 or over is considered to provide adequate sensitivity and specificity to screen for possible caseness of generalised anxiety disorder (GAD) and major depressive disorder (MDD) (Kroenke et al., Citation2001; Kroenke et al., Citation2007; Spitzer, Kroenke, Williams, & Löwe, Citation2006). This criterion was applied in the current study. Both measures are considered valid and reliable self-report tools across both general and clinical populations (Kroenke et al., Citation2001; Spitzer et al., Citation2006), with a Cronbach’s alpha of 0.96 for the GAD-7 and 0.95 for the PHQ-9 in this study.
Suicidality was assessed using 2 items adopted from the Ulster Student Wellbeing Study (Bunting, Murphy, O’Neill, & Ferry, Citation2012). These items specifically assessed lifetime Suicidal Ideation (‘Did you ever in your life have thoughts of killing yourself?’) and lifetime Suicide Attempt (‘Have you ever made a suicide attempt (i.e. purposefully hurt yourself with at least some intent to die)?’), with binary response options (yes/no). Suicidal Ideation and Attempt are considered precursors of completed suicide and robust indicators of suicidality (Klonsky, May, & Saffer, Citation2016).
2.3. Analytic strategy
Data were sourced from the NIVHWS including demographics, trauma exposure, and adverse mental health outcomes. A latent class analysis (LCA) was conducted using the 6 domains of CPTSD symptomology, with potential predictor variables and comorbidities assessed in a multinomial logistic regression.
LCA was used to investigate whether distinct groups of veterans could be identified with distinct symptom profiles in accordance with PTSD and CPTSD diagnostic criteria (as specified by ICD-11). These analyses attempted to identify distinct profiles of CPTSD symptomology in a novel population of military veterans. Findings are expected to contribute to the growing body of evidence related to the latent model of ICD-11 CPTSD (Achterhof et al., Citation2019; Cloitre et al., Citation2020; Elklit et al., Citation2014; Folke et al., Citation2019; Ford, Citation2020; Karatzias et al., Citation2017; Vang et al., Citation2020; Zerach et al., Citation2019). Similarly, these analyses sought to examine salient association with class membership, those identified to be related to PTSD and CPTSD symptomology (Cloitre, Citation2021; Landes et al., Citation2013), to interrogate potential differences between identified classes. Specifically, LCA was conducted using the 6 symptom clusters (‘Re-experiencing’, ‘Avoidance’, ‘Sense of Threat’, Affection Dysregulation’, ‘Negative Self Concept’ and ‘Interpersonal Disturbances’) contained within the ITQ scale to determine the correct number and nature of classes within the sample. LCA is a statistical method used to identify homogeneous groups, or classes, from categorical multivariate data (Muthén & Muthén, Citation1998–Citation2012), therefore it was necessary to create six new binary variables to reflect ‘valid endorsement’ of each of the six ITQ symptoms clusters. Valid endorsement of a symptom cluster is defined as a score of ‘2’ or more on at least one item within each symptom cluster.
The fit of six models was assessed. The models were estimated using robust maximum likelihood (Yuan & Bentler, Citation2000). To avoid solutions based on local maxima, 100 random sets of starting values were used. A number of model fit statistical indices were used to select the optimal number of latent classes. Specifically, the relative fit of the models was compared by using three information theory-based fit statistics: the Akaike information criterion (Akaike, Citation1987) (AIC), the Bayesian information criterion (Schwarz, Citation1978) (BIC) and sample size-adjusted Bayesian information criterion (Sclove, Citation1987) (ssa-BIC). The model that produces the lowest values is judged to be the best fitting model. Entropy scores can range from 0 to 1 with higher scores indicating a better fitting model (Ramaswamy, Desarbo, Reibstein, & Robinson, Citation1993). Additionally, the Lo, Mendell, and Rubin (Citation2001) adjusted likelihood ratio test (LRT) was also used to compare models with increasing numbers of latent classes. When a non-significant value (p > 0.05) occurs, this indicates that the solution with one less class should be accepted.
Two multinomial logistic regressions were then used to determine the extent to which cumulative trauma exposure predicted class membership, and the likelihood of experiencing comorbidities (anxiety, depression, suicidal ideation, and suicide attempt) based on class membership when compared to a normative baseline class. All analyses were conducted in IBM SPSS Statistics (Version 25) and Mplus 7.3.1 (Muthén & Muthén, Citation1998–Citation2012).
3. Results
Most participants were male (90.0%, n = 575), with a mean age of 55.59 years (SD = 10.62, range = 27–99). Most participants (73.4%, n = 468) were married or living with a partner, 16.8% were separated/divorced (n = 107), 5.6% were single/never married (n = 36), 4.1% were widowed (n = 26), with 0.2% responding ‘other’ (n = 1). In specifying military service, 91.4% of participants were Army veterans (n = 583), 10% were Navy veterans (n = 64), 8.3% were Royal Air Force veterans (n = 53), and 1.6% were veterans of the Marines (n = 10). In terms of highest rank served, 17% (n = 121; n = 8 Navy, n = 1 Marines, n = 104 Army, n = 8 Royal Air Force) were commissioned officers, 52.1% (n = 370; n = 30 Navy, n = 6 Marines, n = 305Army, n = 29 Royal Air Force) were non-commissioned officers, and 30.9% (n = 219; n = 26 Navy, n = 6 Marines, n = 174 Army, n = 16 Royal Air Force) served in another rank. It is noted that some participants had served in more than one branch at more than one rank.
Endorsement rates for trauma exposure and mental health outcomes are presented in . Rates for trauma exposure ranged from 6.1% (physical force/threat used by other to attempt sexual assault) to 82% (fire or explosion). Participants were asked to select the ‘worst’ trauma, ranging from 0.2% (unwanted sexual contact when helpless) to 17.6% (fire or explosion). Additionally, 57.7% (n = 367) responded that their worst trauma was related to their military service. Rates for mental health outcomes ranged from 5.8% (PTSD when considered separately from CPTSD) to 56.9% (Affect Dysregulation, suicidal ideation).
Table 1. Endorsement rates for trauma exposure and mental health outcomes.
A latent class analysis (LCA) was performed to test for the presence of latent classes within the study population as defined by endorsement of ITQ subscales. The fit statistics are presented in . The BIC (3696.70) and ssaBIC (3633.20) were lowest for the 3-class solution compared against the other models and the entropy value (0.812) indicated acceptable classification of participants in the 3-class model. While the AIC fit indices were lowest in the 4-class model, the BIC is considered the most reliable of the fit indices (Nylund, Asparouhov, & Muthén, Citation2007). Additionally, the LRT for the 4-class model was not significant, indicating that the model (k-1) should be accepted, leading to the selection of the 3-class model on the basis of best fit and parsimony.
Table 2. Fit statistics for LCA of ITQ Subscales.
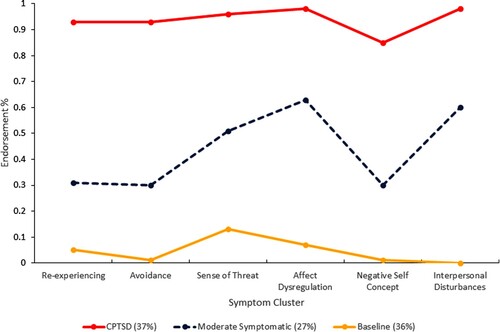
The profile plot for the 3-class model is shown in with endorsement probabilities by class in . Class 1 consisted of 37% (n = 235) of the sample and was observed to have high probability of meeting the diagnostic criteria for all CPTSD symptom clusters. This class was labelled the Probable CPTSD class. Class 2 (27%; n = 175) was characterised by those who met diagnostic criteria for the three PTSD symptom clusters, as well as DSO symptoms clusters, however to a much lower degree than class 1. This class was labelled the Moderate Symptomatic class as this group is described by PTSD and DSO symptomology, though to a lesser degree than the CPTSD class and is not as distinct as those presented in other latent variable models. Finally, class 3 (36%, n = 228) was characterised by those who had the lowest probability of meeting the diagnostic criteria across any of the symptom clusters. This class was labelled the Baseline class.
Table 3. Endorsement probabilities for ITQ symptom cluster by latent class.
Two multinominal regressions were conducted to compare all classes by a predictor variable, cumulative trauma exposure, and by comorbidities: anxiety, depression, suicidal ideation, and suicidal attempt (). The first analysis used the Baseline class (class 3) as a reference category, allowing for comparisons against the Probable CPTSD class (class 1) and Moderate Symptomatic (class 2), and the second used class 2 as the reference category, compared against the CPTSD class.
Table 4. Results of multinomial regressions showing class characteristics.
Cumulative trauma exposure was a significant predictor of Probable CPTSD class membership (when compared to both the Baseline and Moderate Symptomatic classes), and of Moderate Symptomatic class membership when compared to the Baseline class. When compared against the Baseline class, those in the Probable CPTSD class were significantly more likely to experience increased trauma (OR = 1.28, CI = 1.15–1.42), to meet the clinical thresholds for depression (OR = 23.06, CI = 9.69–54.89) and anxiety (OR = 22.05, CI = 8.02–63.19), and to experience both suicidal ideation (OR = 4.32, CI = 2.19–8.48) and suicide attempts (OR = 2.51, CI = 1.04–6.08). Similarly, individuals in the Moderate Symptomatic class were significantly more likely to more to experience increased trauma (OR = 1.14, CI = 1.05–1.23), as well as all other mental health outcomes excluding suicide attempts. When compared against the Moderate Symptomatic class, the Probable CPTSD class were significantly more likely to experience increased trauma (OR = 1.13, CI = 1.03–1.23), and to meet the clinical thresholds for depression (OR = 3.17, CI = 1.73–5.77) and anxiety (OR = 6.01, CI = 3.35–10.78). Additionally, those in the Probable CPTSD class were significantly more likely to experience both suicidal ideation (OR = 1.96, CI = 1.09–3.55) and attempts (OR = 2.60, CI = 1.35–5.03).
4. Discussion
The LCA resulted in a 3-class model: a Probable CPTSD class (37%) described by high levels of PTSD symptomology (re-experiencing, avoidance, and sense of threat) and DSO symptomology (affect dysregulation, negative self-concept, and interpersonal disturbances), a smaller Moderate Symptomatic class (27%) described by moderate levels of all symptomology, and a non-clinical baseline class (36%). While a 3-class model and a larger CPTSD class are largely consistent with previous literature, the number who met criteria for probable PTSD alone when considering probable CPTSD was extremely low, which may account for why a more distinctive ‘PTSD’ class did not emerge. Sub-threshold CPTSD classes have been found in trauma-exposed populations (Böttche et al., Citation2018) with profiles differing in symptom severity (Knefel et al., Citation2015; Wolf et al., Citation2015) and including moderate symptomology with DSO endorsement (Folke et al., Citation2019; Folke, Nielsen, & Karstoft, Citation2021; Liddell et al., Citation2019). It is also possible that highly traumatised samples are more likely to experience DSO symptomology (Shevlin et al., Citation2017; Vang et al., Citation2021), resulting in the absence of a PTSD-only class.
The lack of such a class is likely due to a combination of the sample size and the context of NI rather than a refutation of the construct validity of CPTSD. The sample reported high levels of trauma exposure; overall trauma and ‘worst’ trauma were in categories reflective of both combat exposure and the turbulent climate of NI during Operation Banner. Over half the sample (57.7%) indicated that their ‘worst’ trauma as related to their PTSD was during military service and many serving were targeted during off-duty hours (Armour, Waterhouse-Bradley, et al., Citation2018). Individuals were subject to high levels of cumulative trauma due to decades of political violence and signed on to a career with increased risk of further traumatisation, resulting in a highly traumatised population.
Symptom endorsement probabilities in the Probable CPTSD class ranged from 85% (negative self-concept) to 98% (affect dysregulation, interpersonal disturbances), meeting the diagnostic requirements for CPTSD and describing a group experiencing severe distress. As class membership is probabilistic, the endorsement rates for probable PTSD (n = 37, 5.8%) and probable CPTSD (n = 148, 23.3%) are better indicators of actual caseness. The Moderate Symptomatic class in this sample ranged from 30% (negative self-concept, avoidance) to 63% (affect dysregulation), describing a group above the clinical threshold for PTSD with some aspects of DSO. Negative self-concept was the least endorsed DSO symptom cluster in the clinical classes and a sense of threat was the highest endorsed PTSD symptom cluster in all three classes. This makes sense in the context of NI’s sociopolitical history of guerrilla-style conflict (Frost et al., Citation2020), the objective reality of ongoing threat of violence towards veterans (Armour, McGlinchey, & Ross, Citation2021), and that the perceived, be it objective or subjective, sense of threat reported in this population (Armour, Waterhouse-Bradley, et al., Citation2018).
Cumulative trauma was a significant predictor of membership in both Probable CPTSD (OR = 1.28) and Moderate Symptomatic (OR = 1.14) classes. Experiences of cumulative trauma were also more likely to result in Probable CPTSD class membership, in line with the literature suggesting that CPTSD is a disorder resulting from extreme, repeated, and/or prolonged traumatic experiences (Cloitre et al., Citation2009; Herman, Citation1992; Palic et al., Citation2016). It is well established that a traumatic event can result in the experience of PTSD symptomology (reexperiencing, avoidance, and sense of threat), and that the DSO symptomology is the result of the chronic nature of a prolonged stressor. Military service in an armed conflict is an environment described by a constant threat-to-life with an ambiguous end point and elevated prevalence rates of CPTSD have been previously found in veteran cohorts after service (Letica-Crepulja et al., Citation2020; Murphy et al., Citation2020; Zerach et al., Citation2019). For NI veterans, the repeated trauma did not end with separation, as many remained living ‘in the battlefield’ in the towns in which they had served, and in a region with existing open hostilities towards those who had served.
While all mental health outcomes were highly comorbid, the likelihood of occurrence was higher in the Probable CPTSD class than the Moderate Symptomatic class. This difference was present when the baseline class was used as the reference category and when the Moderate Symptomatic class was the reference, though the likelihood was not as high. These results are consistent with previous findings (Frost et al., Citation2020; Letica-Crepulja et al., Citation2020) and with the suggestion of an increased psychological encumbrance due to CPTSD including high rates of comorbidity with anxiety, depression, and self-injurious/suicidal ideation due to a hypothesised general ‘internalizing’ factor of psychological distress (Hyland et al., Citation2018). Depression was the most comorbid in both classes (OR = 23.06 for Probable CPTSD, OR = 7.28 for Moderate Symptomatic), followed by anxiety (OR = 22.05 for Probable CPTSD, OR = 3.77 for Moderate Symptomatic), and while suicidal ideation was comorbid in both classes, a suicide attempt was only so for the Probable CPTSD class. Both anxiety and depression are comorbid with suicidality (Cougle, Keough, Riccardi, & Sachs-Ericsson, Citation2009; Hawton, Houston, Haw, Townsend, & Harriss, Citation2003), with anxiety highly associated with suicidality in a large veteran cohort (Pfeiffer, Ganoczy, Ilgen, Zivin, & Valenstein, Citation2009), and the findings here support this. It is known that PTSD/CPTSD do not feature a reduced pain threshold characteristic of other disorders with DSO symptoms (Schmahl et al., Citation2010), and that PTSD symptoms are associated with multiple physical conditions including chronic pain (Pacella, Hruska, & Delahanty, Citation2013), which has been associated with suicidality (Ford & Courtois, Citation2014). It is also possible that the increased psychological distress stemming from the additional DSO symptoms contribute to an increased prevalence of suicidal behaviour.
The results here must be viewed in the unique context of NI, taking into account both the complex history of the conflict and the contemporary environment in which the study’s respondents live. As previously discussed, self-disclosure of veteran status carries significant risk (Armour et al., Citation2017; Armour, Waterhouse-Bradley, et al., Citation2018) which can affect help-seeking behaviour, leaving few avenues of support for those experiencing distress. Data from the NIVHWS has shown that veterans resident in NI who served in NI (‘home service’) described more barriers to support service use than those deployed elsewhere (‘general service’) (Armour, McGlinchey, et al., Citation2021). Additionally, the Armed Forces Covenant is not implemented in NI and matters of defence are not devolved issues for the NI Executive, meaning dedicated veteran support is limited to a handful of charitable organisations (Armour et al., Citation2017; Armour, Walker, et al., Citation2018; Armour, Waterhouse-Bradley, et al., Citation2018).
This study has validated previous research of latent analysis of PSTD/CPTSD symptom clusters in a trauma exposed population, replicating previous findings of latent groups espousing low-symptomology, moderate symptomology, and CPTSD/DSO symptomology (Böttche et al., Citation2018; Knefel et al., Citation2015).
4.1. Strengths & limitations
Results must be considered alongside the limitations of this study. Of the overall study population (N = 1,329), 307 were removed for not having endorsed a single trauma and 384 had greater than 20% missing data, meaning data from only 48% of participants (n = 638) were utilised. The sample size was however sufficient for the type of analyses used. The comorbidities used in the analyses do not represent all potential comorbid conditions associated with PTSD and CPTSD, as this study was limited by the available data from the NIVHWS. As the exact size and demographics of the NI veteran population are unknown, these results cannot be generalised to that population. It is possible that the study population was not representative of the NI veteran population due to selection bias, as participants may represent a sub-group typified by willingness to participate and disclose both veteran status and psychological distress. However, the demographic data from the NIVHWS is largely in line with that reported by the Ministry of Defence (Armour, McGlinchey, et al., Citation2021) and can be taken as an approximation of the population in the absence of a complete census of the NI veteran population.
It also must be noted that the prevalence of suicidality is very high in the study population and may also factor into selection bias when considering the prevalence of PTSD and CPTSD in this sample. Due to the political climate, NI population has a high level of cumulative trauma which could make differentiating between ‘on-duty’ and ‘off-duty’ traumatic events difficult for some participants. Finally, the data used was self-report, which carries the potential for social desirability bias and which meant that while a participant may have met criteria for PTSD/CPTSD, a clinical designation could only be probable without a formal assessment.
There are several strengths associated with this study. As above, data were taken from the NIVHWS, which was the first successful large-scale research into the NI veteran community, and subsequent findings utilising the data will build a body of literature on this population, inform further research, contribute to global military veteran research, and influence policy. Understanding the structure, associations, and comorbidities of CPTSD in trauma exposed populations furthers the greater understanding of the new disorder, its distinct difference from PTSD, and can help inform clinical treatment.
4.2. Impact & implications
In this sample, anxiety, depression, and suicidality were significantly associated with the Moderate Symptomatic (excepting suicide attempt) and Probable CPTSD classes, however, the odds of comorbidity for anxiety and depression with CPTSD were quite high. While the study results cannot be generalised to the greater NI veteran population, the results do signal that there is significant need for services addressing not only PTSD and CPTSD relating to military service, but also the high degree of comorbid conditions. These results describe outcomes in a sub-group of the veteran population willing to participate in the study, meaning sub-groups may exist for whom the severity of their distress or concerns surrounding disclosure of their military status made them unwilling/unable to engage, a known issue in NI (Armour et al., Citation2017; Armour, Walker, et al., Citation2018). These groups would need support and reliable access to mental health care.
The findings here, and from other studies utilising NIVHWS data, clearly indicate that the support needs of the NI veteran population remain unmet and barriers to care remain a significant issue (Armour, McGlinchey, et al., Citation2021). These issues are compounded by the relative deprivation of Northern Ireland when compared against the other nations of the United Kingdom in terms of veteran support (Armour et al., Citation2017), access to mental health care/treatment (O’Neill, Heenan, & Betts, Citation2019), and on a socio-economic level (Haase, Citation2018). Specifics of the NI veteran population, including basics such as the estimated size of this group, remain largely unknown. Additional research is recommended but policymakers must consider the findings of this and previous studies when discussing resource allocation and support initiatives.
In conclusion, cases of probable CPTSD have proven to have been more prevalent than probable PTSD without DSO symptoms in this trauma exposed population of UK Armed Forces veterans resident in NI. Additionally in this sample, probable CPTSD has been shown to be highly comorbid in a similar vein to PTSD. Ultimately, this is described as a trifecta of complex and multiple trauma exposures, CPTSD symptomology, and significant comorbid distress. Mental health care and support providers working with veteran populations would be best served evaluating veterans with PTSD for DSO symptomology, especially if exposed to complex trauma in the course of their military service.
Acknowledgements
The authors would like to thank the Forces in Mind Trust for funding the Northern Ireland Veterans’ Health and Well-being Study. The funders had no role in the study design or publication of results.
Data availability statement
Due to the nature of this research the participants in this study did not provide consent for the public sharing of their data, these data are therefore unavailable.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Achterhof, A., Huntjens, R. J. C., Meewisse, M.-L., & Kiers, H. A. L. (2019). Assessing the application of latent class and latent profile analysis for evaluating the construct validity of complex posttraumatic stress disorder: Cautions and limitations. European Journal of Psychotraumatology, 10(1), 1698223. doi:10.1080/20008198.2019.1698223
- Akaike, H. (1987). Factor analysis and AIC. Psychometrika, 52(3), 317–332.
- Armour, C. (2015). The underlying dimensionality of PTSD in the diagnostic and statistical manual of mental disorders: Where are we going? European Journal of Psychotraumatology, 6(1), 28074. doi:10.3402/ejpt.v6.28074
- Armour, C., McGlinchey, E., & Ross, J. (2021). The health and wellbeing of armed forces veterans in Northern Ireland: The results of a cross-sectional psychological wellbeing survey. Retrieved from http://niveteranstudy.org/mentalhealth
- Armour, C., Robinson, M., & Ross, J. (2021). Factor structure of the international trauma questionnaire in UK armed forces veterans residing in Northern Ireland. European Journal of Psychotraumatology, 12(1), 1924954. doi:10.1080/20008198.2021.1924954
- Armour, C., Walker, E., Hall, M., Waterhouse-Bradley, B., Ross, J., & McLafferty, M. (2018). Exploring the need for a veteran’s centre in Northern Ireland. Retrieved October 11, 2021, from https://s31949.pcdn.co/wp-content/uploads/exploring-need-for-veterans-centre-northern-ireland.pdf
- Armour, C., Walker, E., Waterhouse-Bradley, B., Hall, M., & Ross, J. (2017). Current and future needs of veterans in Northern Ireland. Retrieved March 13, 2021, from https://www.fim-trust.org/wp-content/uploads/current-future-needs-veterans-northern-ireland.pdf
- Armour, C., Waterhouse-Bradley, B., Ross, J., McLafferty, M., & Hall, M. (2018). Public attitudes to the UK armed forces in Northern Ireland. Retrieved March 14, 2021, from https://www.fim-trust.org/wp-content/uploads/public-attitudes-uk-armed-forces-northern-ireland.pdf
- Böttche, M., Ehring, T., Krüger-Gottschalk, A., Rau, H., Schäfer, I., Schellong, J., … Knaevelsrud, C. (2018). Testing the ICD-11 proposal for complex PTSD in trauma-exposed adults: Factor structure and symptom profiles. European Journal of Psychotraumatology, 9(1), 1512264. doi:10.1080/20008198.2018.1512264
- Brewin, C. R., Cloitre, M., Hyland, P., Shevlin, M., Maercker, A., Bryant, R. A., … Reed, G. M. (2017). A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clinical Psychology Review, 58, 1–15. doi:10.1016/j.cpr.2017.09.001
- Bunting, B. P., Murphy, S. D., O’Neill, S. M., & Ferry, F. R. (2012). Lifetime prevalence of mental health disorders and delay in treatment following initial onset: Evidence from the Northern Ireland study of health and stress. Psychological Medicine, 42(8), 1727–1739. doi:10.1017/S0033291711002510
- Cloitre, M. (2020). ICD-11 complex post-traumatic stress disorder: Simplifying diagnosis in trauma populations. The British Journal of Psychiatry, 216(3), 129–131. doi:10.1192/bjp.2020.43
- Cloitre, M. (2021). Complex PTSD: Assessment and treatment. European Journal of Psychotraumatology, 12(1), 1866423. doi:10.1080/20008198.2020.1866423
- Cloitre, M., Brewin, C. R., Bisson, J. I., Hyland, P., Karatzias, T., Lueger-Schuster, B., … Shevlin, M. (2020). Evidence for the coherence and integrity of the complex PTSD (CPTSD) diagnosis: Response to Achterhof et al., (2019) and Ford (2020). European Journal of Psychotraumatology, 11(1), 1739873. doi:10.1080/20008198.2020.1739873
- Cloitre, M., Garvert, D. W., Weiss, B., Carlson, E. B., & Bryant, R. A. (2014). Distinguishing PTSD, complex PTSD, and borderline personality disorder: A latent class analysis. European Journal of Psychotraumatology, 5(1), 25097. doi:10.3402/ejpt.v5.25097
- Cloitre, M., Hyland, P., Bisson, J. I., Brewin, C. R., Roberts, N. P., Karatzias, T., & Shevlin, M. (2019). ICD-11 posttraumatic stress disorder and complex posttraumatic stress disorder in the United States: a population-based study. Journal of Traumatic Stress, 32(6), 833–842. doi:10.1002/jts.22454
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The international trauma questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. doi:10.1111/acps.12956
- Cloitre, M., Stolbach, B. C., Herman, J. L., van der Kolk, B., Pynoos, R., Wang, J., & Petkova, E. (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22(5), 399–408.
- Cougle, J. R., Keough, M. E., Riccardi, C. J., & Sachs-Ericsson, N. (2009). Anxiety disorders and suicidality in the national comorbidity survey-replication. Journal of Psychiatric Research, 43(9), 825–829. doi:10.1016/j.jpsychires.2008.12.004
- Currier, J. M., Foster, J. D., Karatzias, T., & Murphy, D. (2021). Moral injury and ICD-11 complex PTSD (CPTSD) symptoms among treatment-seeking veterans in the United Kingdom. Psychological Trauma: Theory, Research, Practice, and Policy, 13(4), 417–421. doi:10.1037/tra0000921
- Eilers, R., Rimane, E., Vogel, A., Renneberg, B., Stein, R., & Rosner, R. (2021). Response of young patients with probable ICD-11 complex PTSD to treatment with developmentally adapted cognitive processing therapy. European Journal of Psychotraumatology, 12(1), 1929024. doi:10.1080/20008198.2021.1929024
- Elhai, J. D., Miller, M. E., Ford, J. D., Biehn, T. L., Palmieri, P. A., & Frueh, B. C. (2012). Posttraumatic stress disorder in DSM–5: Estimates of prevalence and symptom structure in a nonclinical sample of college students. Journal of Anxiety Disorders, 26, 58–64. doi:10.1016/j.janxdis.2011.08.013
- Elklit, A., Hyland, P., & Shevlin, M. (2014). Evidence of symptom profiles consistent with posttraumatic stress disorder and complex posttraumatic stress disorder in different trauma samples. European Journal of Psychotraumatology, 5(1), 24221. doi:10.3402/ejpt.v5.24221
- Facer-Irwin, E., Karatzias, T., Bird, A., Blackwood, N., & MacManus, D. (2021). PTSD and complex PTSD in sentenced male prisoners in the UK: Prevalence, trauma antecedents, and psychiatric comorbidities. Psychological Medicine, 1–11. doi:10.1017/S0033291720004936
- Folke, S., Nielsen, A. B. S., Andersen, S. B., Karatzias, T., & Karstoft, K.-I. (2019). ICD-11 PTSD and complex PTSD in treatment-seeking Danish veterans: A latent profile analysis. European Journal of Psychotraumatology, 10(1686806), doi:10.1080/20008198.2019.168680
- Folke, S., Nielsen, A. B. S., & Karstoft, K.-I. (2021). PTSD and complex PTSD in treatment-seeking Danish soldiers: A replication of Folke et al. (2019) using the international trauma questionnaire. European Journal of Psychotraumatology, 12(1), 1930703. doi:10.1080/20008198.2021.1930703
- Ford, J. D. (2020). New findings questioning the construct validity of complex posttraumatic stress disorder (cPTSD): Let’s take a closer look. European Journal of Psychotraumatology, 11(1), 1708145. doi:10.1080/20008198.2019.1708145
- Ford, J. D., & Courtois, C. A. (2014). Complex PTSD, affect dysregulation, and borderline personality disorder. Borderline Personality Disorder and Emotion Dysregulation, 1, 9. doi:10.1186/2051-6673-1-9
- Frost, R., Hyland, P., Shevlin, M., & Murphy, J. (2020). Distinguishing complex PTSD from borderline personality disorder among individuals with a history of sexual trauma; a latent class analysis. European Journal of Trauma & Dissociation, 4(1), 100080. doi:10.1016/j.ejtd.2018.08.004
- Frost, R., Murphy, J., Hyland, P., Shevlin, M., Ben-Ezra, M., Hansen, M., … McDonagh, T. (2020). Revealing what is distinct by recognising what is common: Distinguishing between complex PTSD and borderline personality disorder symptoms using bifactor modelling. European Journal of Psychotraumatology, 11(1), doi:10.1080/20008198.2020.1836864
- Frost, R., Vang, M. L., Karatzias, T., Hyland, P., & Shevlin, M. (2019). The distribution of psychosis, ICD-11 PTSD and complex PTSD symptoms among a trauma-exposed UK general population sample. Psychosis, 11(3), 187–198. doi:10.1080/17522439.2019.1626472
- Haase, D. (2018). Research for REGI Committee – the economic, social and territorial situation of Northern Ireland, European Parliament, Policy Department for Structural and Cohesion Policies, Brussels. Retrieved from https://www.europarl.europa.eu/RegData/etudes/IDAN/2018/617459/IPOL_IDA(2018)617459_EN.pdf
- Hansen, M., Hyland, P., Armour, C., Shevlin, M., & Elklit, A. (2015). Less is more? Assessing the validity of the ICD-11 model of PTSD across multiple trauma samples. European Journal of Psychotraumatology, 6, 4598338. doi:10.3402/ejpt.v6.28766
- Hawton, K., Houston, K., Haw, C., Townsend, E., & Harriss, L. (2003). Comorbidity of Axis I and Axis II disorders in patients who attempted suicide. American Journal of Psychiatry, 160(8), 1494–1500. doi:10.1176/appi.ajp.160.8.1494
- Hébert, M., & Amédée, L. M. (2020). Latent class analysis of post-traumatic stress symptoms and complex PTSD in child victims of sexual abuse and their response to trauma-focused cognitive behavioural therapy. European Journal of Psychotraumatology, 11(1), 1807171. doi:10.1080/20008198.2020.1807171
- Herman, J. L. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5(3), 377–391.
- Herman, J. L., Perry, J. C., & Van der Kolk, B. A. (1989). Childhood trauma in borderline personality disorder. American Journal of Psychiatry, 146(4), 490–495. doi:10.1176/ajp.146.4.490
- Hitch, C., Toner, P., & Armour, C. (2020). Exploring enablers and barriers to help-seeking for military veterans with mental health and alcohol difficulties: A qualitative systematic review. Poster session presented at PsyPAG virtual conference. https://osf.io/7nwu2/?view_only=3dc6578be53f481d94e11395c4a914e5
- Hyland, P., Shevlin, M., Fyvie, C., & Karatzias, T. (2018). Posttraumatic stress disorder and complex posttraumatic stress disorder in DSM-5 and ICD-11: Clinical and behavioral correlates. Journal of Traumatic Stress, 31(2), 174–180. doi:10.1002/jts.22272
- Hyland, P., Vallières, F., Cloitre, M., Ben-Ezra, M., Karatzias, T., Olff, M., … Shevlin, M. (2021). Trauma, PTSD, and complex PTSD in the republic of Ireland: Prevalence, service use, comorbidity, and risk factors. Social Psychiatry and Psychiatric Epidemiology, 56, 649–658. doi:10.1007/s00127-020-01912-x
- Karatzias, T., Hyland, P., Bradley, A., Cloitre, M., Roberts, N. P., Bisson, J. I., & Shevlin, M. (2019a). Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: Findings from a trauma-exposed population based sample of adults in the United Kingdom. Depression and Anxiety, 36(9), 887–894. doi:10.1002/da.22934
- Karatzias, T., Murphy, P., Cloitre, M., Bisson, J., Roberts, N., Shevlin, M., … Hutton, P. (2019b). Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychological Medicine, 49(11), 1761–1775. doi:10.1017/S0033291719000436
- Karatzias, T., Shevlin, M., Fyvie, C., Hyland, P., Efthymiadou, E., Wilson, D., … Cloitre, M. (2017). Evidence of distinct profiles of posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD) based on the new ICD-11 trauma questionnaire (ICD-TQ). Journal of Affective Disorders, 207, 181–187. doi:10.1016/j.jad.2016.09.032
- Klonsky, E. D., May, A. M., & Saffer, B. Y. (2016). Suicide, suicide attempts, and suicidal ideation. Annual Review of Clinical Psychology, 12, 307–330. doi:10.1146/annurev-clinpsy-021815-093204
- Knefel, M., Garvert, D. W., Cloitre, M., & Lueger-Schuster, B. (2015). Update to an evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse by Knefel & Lueger-Schuster (2013): A latent profile analysis. European Journal of Psychotraumatology, 6(1), 25290. doi:10.3402/ejpt.v6.25290
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi:10.1046/j.1525-1497.2001.016009606.x
- Kroenke, K., Spitzer, R. L., Williams, J. B., Monahan, P. O., & Löwe, B. (2007). Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine, 146(5), 317–325. doi:10.7326/0003-4819-146-5-200703060-00004
- Landes, S. J., Garovoy, N. D., & Burkman, K. M. (2013). Treating complex trauma among veterans: Three stage-based treatment models. Journal of Clinical Psychology, 69(5), 523–533. doi:10.1002/jclp.21988
- Letica-Crepulja, M., Stevanović, A., Protuđer, M., Juretić, T. G., Rebić, J., & Frančišković, T. (2020). Complex PTSD among treatment-seeking veterans with PTSD. European Journal of Psychotraumatology, 11(1), 1716593. doi:10.1080/20008198.2020.1716593
- Liddell, B. J., Nickerson, A., Felmingham, K. L., Malhi, G. S., Cheung, J., Den, M., … Bryant, R. A. (2019). Complex posttraumatic stress disorder symptom profiles in traumatized refugees. Journal of Traumatic Stress, 32(6), 822–832. doi:10.1002/jts.22453
- Lo, Y., Mendel, N. R., & Rubin, D. B. (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. doi:10.1093/biomet/88.3.767
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., Reed, G. M., van Ommeren, M., … Saxena, S. (2013). Proposals for mental disorders specifically associated with stress in the International Classification of diseases-11. The Lancet, 381, 1683–1685. doi:10.1016/S0140-6736(12)62191-6
- McGlinchey, E., Ross, J., Murphy, D., Shorter, G. W., & Armour, C. (2021). Disentangling the symptom-level nuances in comorbid posttraumatic stress disorder and problematic alcohol use in Northern Irish military veterans: A network analysis. Journal of Traumatic Stress, 22666. doi:10.1002/jts.22666
- Moderno, I. G., Nalipay, M. J. N., & Mordeno, E. R. (2019). The factor structure of complex PTSD in combat-exposed Filipino soldiers. Psychiatry Research, 278, 65–69. doi:10.1016/j.psychres.2019.05.035
- Murphy, D., Karatzias, T., Busuttil, W., Greenberg, N., & Shevlin, M. (2021). ICD-11 posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) in treatment seeking veterans: Risk factors and comorbidity. Social Psychiatry and Psychiatric Epidemiology, 56, 1289–1298. doi:10.1007/s00127-021-02028-6
- Murphy, D., Shevlin, M., Pearson, E., Greenberg, N., Wessely, S., Busuttil, W., & Karatzias, T. (2020). A validation study of the International Trauma Questionnaire to assess post-traumatic stress disorder in treatment-seeking veterans. The British Journal of Psychiatry, 216(3), 132–137. doi:10.1192/bjp.2020.9
- Muthén, L. K., & Muthén, B. O. (1998–2012). Mplus user’s guide: Statistical analysis with latent variables (7th ed.). Los Angeles, CA: Muthén & Muthén.
- Nylund, K. L., Asparouhov, T., & Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. doi:10.1080/10705510701575396
- O’Neill, S., Heenan, D., & Betts, J. (2019). Review of mental health policies in Northern Ireland: Making parity a reality. Retrieved October 11, 2021, from https://www.ulster.ac.uk/__data/assets/pdf_file/0004/452155/Final-Draft-Mental-Health-Review-web.pdf
- Pacella, M. L., Hruska, B., & Delahanty, D. L. (2013). The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. Journal of Anxiety Disorders, 27(1), 33–46. doi:10.1016/j.janxdis.2012.08.004
- Palic, S., Zerach, G., Shevlin, M., Zeligman, Z., Elklit, A., & Solomon, Z. (2016). Evidence of complex posttraumatic stress disorder (CPTSD) across populations with prolonged trauma of varying interpersonal intensity and ages of exposure. Psychiatry Research, 246(30), 692–699.
- Pfeiffer, P. N., Ganoczy, D., Ilgen, M., Zivin, K., & Valenstein, M. (2009). Comorbid anxiety as a suicide risk factor among depressed veterans. Depression and Anxiety, 26(8), 752–757. doi:10.1002/da.20583
- Ramaswamy, V., Desarbo, W. S., Reibstein, D. J., & Robinson, W. T. (1993). An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Marketing Science, 12(1), 103–124.
- Redican, E., Nolan, E., Hyland, P., Cloitre, M., McBride, O., Karatzias, T., … Shevlin, M. (2021). A systematic literature review of factor analytic and mixture models of ICD-11 PTSD and CPTSD using the international trauma questionnaire. Journal of Anxiety Disorders, 56, 1289–1298. doi:10.1007/s00127-021-02028-6
- Robinson, M., McGlinchey, E., & Armour, C. (2021, October 18). ICD-11 C-PTSD and psychiatric comorbidity among UK armed forces veterans in Northern Ireland. doi:10.17605/OSF.IO/VEQP5
- Schmahl, C., Meinzer, M., Zeuch, A., Fichter, M., Cebulla, M., Kleindienst, N., … Bohus, M. (2010). Pain sensitivity is reduced in borderline personality disorder, but not in posttraumatic stress disorder and bulimia nervosa. The World Journal of Biological Psychiatry, 11(2), 364–371. doi:10.3109/15622970701849952
- Schwarz, G. (1978). Estimating the dimension of a model. The Annals of Statistics, 6(2), 461–464.
- Sclove, S. L. (1987). Application of model-selection criteria to some problems in multivariate analysis. Psychometrika, 52(3), 333–343.
- Shevlin, M., Hyland, P., Karatzias, T., Fyvie, C., Roberts, N., Bisson, J. I., … Cloitre, M. (2017). Alternative models of disorders of traumatic stress based on the new ICD-11 proposals. Acta Psychiatrica Scandinavica, 135(5), 419–428. doi:10.1111/acps.12695
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(1), 1092–1097. doi:10.1001/archinte.166.10.1092
- Vang, M. L., Dokkedalh, S. B., Løkkegaard, S. S., Jakobsen, A. V., Møller, L., Auning-Hansen, M. A., & Ask, E. (2021). Validation of ICD-11 PTSD and DSO using the International Trauma Questionnaire in five clinical samples recruited in Denmark. European Journal of Psychotraumatology, 12(1), 1984806. doi:10.1080/20008198.2021.1894806
- Vang, M. L., Nielsen, S. B., Auning-Hansen, M., & Elklit, A. (2020). Testing the validity of ICD-11 PTSD and CPTSD among refugees in treatment using latent class analysis. Torture Journal, 29(3), 27–45. doi:10.7146/torture.v29i3.115367
- Voorendonk, E. M., De Jongh, A., Rozendaal, L., & Van Minnen, A. (2020). Trauma-focused treatment outcome for complex PTSD patients: Results of an intensive treatment programme. European Journal of Psychotraumatology, 11(1), 1783955. doi:10.1080/20008198.2020.1783955
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The life events checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov.
- Williamson, V., Pearson, E. J., Shevlin, M., Karatzias, T., Macmanus, D., & Murphy, D. (2021). Experiences of veterans with ICD-11 complex PTSD in engaging with services. Journal of Loss and Trauma, 26(2), 166–178. doi:10.1080/15325024.2020.1749784
- Wolf, E. J., Miller, M. W., Kilpatrick, D., Resnick, H. S., Badour, C. L., Marx, B. P., … Friedman, M. J. (2015). ICD-11 Complex PTSD in U.S. national and veteran samples: Prevalence and structural associations with PTSD. Clinical Psychological Science, 3(2), 215–229. doi:10.1177/2167702614545480
- World Health Organization. (2019). International Statistical Classification of Diseases and Related Health Problems (11th ed.). Geneva. https://icd.who.int/
- Yuan, K.-H., & Bentler, P. M. (2000). Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology, 30(1), 165–200. doi:10.1111/0081-1750.00078
- Zerach, G., Shevlin, M., Cloitre, M., & Solomon, Z. (2019). Complex posttraumatic stress disorder (CPTSD) following captivity: A 24-year longitudinal study. European Journal of Psychotraumatology, 10(1), 1616488. doi:10.1080/20008198.2019.1616488