ABSTRACT
Background
Chinese shidu parents (bereaved parents over the age of 49 who have lost their only child) are potentially at a high risk of prolonged grief disorder (PGD), posttraumatic stress disorder (PTSD) and insomnia.
Objective
The current study aimed to estimate three network models in 310 shidu parents who met the ICD-11 criteria for PGD: (1) a PGD network to identify central symptoms; (2) a comorbidity network to explore bridge symptoms between PGD and PTSD; (3) a comorbidity network to examine the associations between PGD and insomnia symptoms.
Methods
The R-packages bootnet, qgraph and networktools were used to investigate the structure of network models and centrality indices of symptoms. In addition, robustness and significance analyses for the edge weights and the order of centrality were performed.
Results
Emotional pain and numbness emerged as the most central symptoms in the PGD network. In the PGD-PTSD comorbidity network, the highest bridge strength symptoms were inability to trust others (PGD) and feeling upset (PTSD). Inability to trust others (PGD), avoidance (PGD), and impairment of life quality (insomnia) were possible bridge symptoms connecting PGD and insomnia.
Conclusions
Reducing emotional pain and numbness may be a viable target in PGD interventions for shidu parents. Additionally, findings suggest that future studies could examine the role of inability to trust others and avoidance in PGD comorbidities.
HIGHLIGHTS
• Emotional pain and numbness were the most influential symptoms in shidu parents with PGD. The role of PGD symptoms of inability to trust others and avoidance in the comorbidities of PGD with PTSD and insomnia might be worthy of further study
Antecedentes: Los padres chinos shidu (padres en duelo mayores de 49 años que han perdido a su único hijo) tienen un alto riesgo potencial de presentar trastorno de duelo prolongado (TDP), trastorno de estrés postraumático (TEPT) e insomnio.
Objetivo: El presente estudio tuvo como objetivo estimar tres modelos de redes en 310 padres shidu que cumplieron con los criterios CIE-11 para TDP: (1) una red TDP para identificar síntomas centrales; (2) una red de comorbilidad para explorar los síntomas puente entre TDP y TEPT; (3) una red de comorbilidad para examinar las asociaciones entre el TDP y síntomas del insomnio.
Métodos: Se utilizaron los paquetes R bootnet, qgraph y networktools para investigar la estructura de los modelos de redes y los índices de centralidad de los síntomas. Además, se realizaron análisis de robustez y significancia para los pesos de borde y el orden de centralidad.
Resultados: El dolor y el embotamiento emocional surgieron como los síntomas más centrales en la red TDP. En la red de comorbilidad TDP-TEPT, los síntomas fuerza de puente más altos fueron la incapacidad para confiar en los demás (TDP) y sentirse molesto (TEPT). La incapacidad para confiar en los demás (TDP), la evitación (TDP) y el deterioro de la calidad de vida (insomnio) fueron posibles síntomas puente que conectan el TDP y el insomnio.
Conclusiones: Reducir el dolor y el embotamiento emocional puede ser un objetivo viable en las intervenciones de TDP para padres shidu. Además, los hallazgos sugieren que los estudios futuros podrían examinar el papel de la incapacidad para confiar en los demás y la evitación en las comorbilidades del TDP.
背景: 失独父母(49岁以上失去独生子女的父母)患有延长哀伤障碍(PGD)、创伤后应激障碍(PTSD)和失眠的风险较高。
目的: 在310名符合PGD诊断标准的失独父母中探讨三个网络模型:(1)确定PGD网络模型的中心症状;(2)探索PGD与PTSD的共病网络模型的桥症状;(3)探索PGD与失眠共病网络模型的桥症状。
方: 法 采用R程序包bootnet、qgraph和networktools估计网络模型的结构和症状的中心性。此外,还对边缘权重和中心性顺序进行了稳健性和显着性分析。
结果: 情感痛苦和麻木是PGD网络中最中心的症状。在PGD-PTSD共病网络中,中心性程度最高的桥症状是难以信任他人(PGD))和情感痛苦(PTSD)。难以信任他人(PGD)、回避(PGD)和生活质量受损(失眠)可能是连接PGD和失眠的桥症状。
结论: 减轻情感痛苦和麻木可能是对失独父母的哀伤干预的一个可行目标。此外,本研究结果提示,未来的研究可以探讨难以信任他人和回避在PGD共病中的作用。
PALABRAS CLAVE:
1. Introduction
Grief is a natural response to the loss of a loved one. However, prolonged grief disorder (PGD) exists in a significant minority of bereaved people (Cozza et al., Citation2020; Prigerson, Kakarala, Gang, & Maciejewski, Citation2021). PGD, a disorder specifically associated with trauma/stress, has been recently included in the International Classification of Disease (ICD-11) (World Health Organization [WHO], Citation2018), as well as the Diagnostic and Statistical Manual of Mental Disorders, fifth edition, text revision (DSM-5-TR) (Prigerson et al., Citation2021). It is characterized by strong longing for and/or persistent preoccupation with the deceased accompanied by intense emotional pain, such as sadness, guilt, anger, and difficulty accepting the death. The grief reactions last for at least 6 months (WHO, Citation2018) or 12 months (American Psychological Association, Citation2021) and cause significant functional impairment.
Among all kinds of loss, child-death is widely recognized as one of the most painful experiences (Djelantik, Smid, et al., Citation2020; Kersting, Brahler, Glaesmer, & Wagner, Citation2011; Zhou et al., Citation2018). Due to the previous ‘One-Child Policy’, China has the largest population of ‘only-child-death’ parents (Zhang et al., Citation2020). A unique cohort of these parents who have lost their only child and are over 49 years at present and have no living biological or adopted child are referred to as ‘shidu parents (meaning of losing the only child in Mandarin)’ in China (Shi et al., Citation2019; Xu et al., Citation2020; Zhou et al., Citation2020). Alarmingly, the number of shidu parents exceeded 1.5 million in 2015 and is expected to reach around 4.5 million by 2050 in China (Wang, Citation2016). Because the Chinese filial piety culture emphasizes having a child to continue bloodlines, shidu parents might struggle more with bereavement due to being childless (Cao, Yang, & Wang, Citation2018; Zheng & Lawson, Citation2015). Additionally, adult children are the primary caregivers for their parents in old age, which is expected by Chinese culture and law (Zheng, Lawson, & Anderson Head, Citation2017). Therefore, losing the only child may cause shidu parents to suffer intense and persistent grief (Wang & Hu, Citation2020; Yin et al., Citation2018; Zhang & Jia, Citation2019). Results from meta-analyses suggest that in general 9.8% of bereaved adults are at risk for PGD (Lundorff, Holmgren, Zachariae, Farver-Vestergaard, & O'Connor, Citation2017), while losing the only child is related to a higher PGD prevalence (Djelantik, Smid, et al., Citation2020). A recent study found that more than a third of shidu parents suffered from PGD according to ICD-11 criteria, with an average time since loss of 9.41 years (Zhou et al., Citation2020).
From a perspective of the cognitive model, three processes – excessively negative appraisal of the loss and its consequences; poor integration of the loss with existing autobiographical memories; and avoidance of reminders of the loss – are not only crucial in the development and maintenance of PGD (Boelen, van den Hout, & van den Bout, Citation2006), but also are critical for posttraumatic stress disorder (PTSD) (Ehlers & Clark, Citation2000). Bereavement is a significant stressor. Therefore, in addition to PGD, PTSD is also often reported by bereaved people (Boelen & Lenferink, Citation2020), especially those who experienced violent death (Kaltman & Bonanno, Citation2003). A meta-analysis study indicated that the prevalence rate of PTSD was 46.8% in shidu parents (Wang et al., Citation2021), which was much higher than that of non-bereaved parents (Yin et al., Citation2018). A recent study found that 90.9% of shidu parents with PGD also met the criteria for PTSD (Zhang et al., Citation2020).
The attachment-based model postulates that the physical presence of attachment figures is very important for biobehavioural regulation in adults, and biobehavioural dysregulation occurs when we lose a loved one. Therefore, grief is commonly associated with neuroendocrine and sleep disturbance, and this disruption persists in those with PGD (Shear & Shair, Citation2005). Although sleep disturbances constitute one of the diagnostic criteria for PTSD, increasing scholars have suggested that sleep disturbances may not just be a symptom of PTSD, but a correlated independent problem and needs to be addressed directly in treatment (Lommen et al., Citation2016; Spoormaker & Montgomery, Citation2008). Furthermore, treatments focused on PGD or PTSD seem to have limited effectiveness in reducing insomnia (Boelen & Lancee, Citation2013; Nappi, Drummond, & Hall, Citation2012). Therefore, sleep disturbance in bereavement appears to need specific attention (Lancel, Stroebe, & Eisma, Citation2020; Shear, Citation2015; Stroebe, Schut, & Stroebe, Citation2007). A systematic review suggested that about 80% of bereaved people with PGD suffered long-term poor sleep (Lancel et al., Citation2020). A qualitative study found that 35 of 36 shidu parents experienced insomnia and 8 relied on medications for sleep (Wang & Hu, Citation2019). A growing number of empirical studies provide evidence that PGD, PTSD and insomnia symptoms all constitute pathological reactions after a significant loss. To better help the bereaved, knowledge about symptoms of grief and clinically significant symptoms of comorbid disorders are important (Shear & Skritskaya, Citation2012). However, information on how the PGD, PTSD, and insomnia symptoms interact and affect each other in shidu parents is relatively limited.
The network approach offers a new perspective to examine a disorder as a causal system of dynamically and functionally interrelated symptoms (Borsboom & Cramer, Citation2013). A network consists of nodes and edges. Nodes represent symptoms and edges between two nodes represent correlations between two symptoms (Hofmann, Curtiss, & McNally, Citation2016). Therefore, PGD can be conceptualized as a network of mutually reinforcing symptoms rather than an underlying cause of the symptoms. Using network analysis (NA), it is possible to explore interactions between symptoms and identify the most influential symptoms in the network (Borsboom, Citation2017). These symptoms, labelled as central symptoms, have more frequent and stronger associations with other symptoms (Hofmann et al., Citation2016). Choosing such symptoms to design interventions might be a viable heuristic for bereaved people to reduce overall levels of PGD (Fried et al., Citation2018). Moreover, the network approach also offers a new way to understand comorbidity (Jones, Ma, & McNally, Citation2019). Certain symptoms of one disorder might increase risks for another distress. These symptoms that bridge different disorders are called ‘bridge symptoms’ (Cramer, Waldorp, van der Maas, & Borsboom, Citation2010). Previous studies found that meaninglessness, loneliness, emotional pain, and numbness were considered as bridge symptoms between PGD and depression (Robinaugh, LeBlanc, Vuletich, & McNally, Citation2014). Role confusion and difficulty trusting others, and feeling distant from others were bridge symptoms between PGD and PTSD (Djelantik, Robinaugh, et al., Citation2020). Targeting these bridge symptoms might be a good alternative to treat or prevent comorbidity (Jones et al., Citation2019). Therefore, applying NA to explore potential bridge symptoms among disorders in shidu parents may be clinically significant.
Although previous findings bring valuable insights into PGD symptoms and comorbidity networks, grief symptoms and expression may vary across cultures (Stelzer, Zhou, et al., Citation2020). For example, previous studies found that the most central symptom of PGD was emotional pain in American conjugally bereaved people (Robinaugh et al., Citation2014), whereas it was longing in Chinese conjugally bereaved people (Pan, Citation2020). A cross-cultural study found that preoccupation with the deceased or death was the second most central symptom for Chinese bereaved people, while it was the fourth least central for German participants (Stelzer, Holtge, et al., Citation2020). Therefore, it is still uncertain whether previous findings can be generalized to shidu parents, whose bereavement adjustment may be affected by the Chinese filial piety culture (Shi et al., Citation2019). Additionally, a positive association between PGD and insomnia has been confirmed (Lancel et al., Citation2020), whereas interconnections of symptom-level between PGD and insomnia remain unknown. Therefore, the current study aimed to apply a NA approach to identify central PGD symptoms, and explore bridge symptoms between PGD and PTSD, as well as PGD and insomnia in shidu parents. Specifically, we would like to focus on shidu parents with PGD. In this group, it is not the stress of bereavement but rather severe grief symptoms that predict the long-term quality of life and health impairments (Boelen & Prigerson, Citation2007; Prigerson et al., Citation1997). Moreover, interventions seem to be most effective for bereaved people with PGD (Wittouck, Van Autreve, De Jaegere, Portzky, & van Heeringen, Citation2011). Accordingly, the current study aimed to gain a preliminary understanding of the networks of shidu parents with PGD.
2. Methods
2.1. Participants
The data used in this study was a part of a larger project ‘Constructing a psychological help system for Chinese shidu parents, based on a population-based survey’ collected from April 2017 to May 2018 across China. A convenience sample of 885 shidu parents was recruited. Two participants were excluded from the analysis due to missing more than 20% of the data (Enders, Citation2003; Peng, Harwell, Liou, & Ehman, Citation2006). Based on self-report results from the Prolonged Grief Questionnaire (Prigerson et al., Citation2009) and 1 item from the depression subscale of the Symptom Checklist-90 (Tan, Lan, Yu, & Yang, Citation2015), 310 participants in this study were considered to meet ICD-11 criteria for PGD. For a detailed description of recruitment and diagnosis procedures, see Zhou et al. (Citation2020). The sample mainly consisted of females (n = 235, 75.8%). The mean age of the participants was 57.23 years (SD = 7.13), with an average time since child-death of 7.82 years. Descriptive information of the shidu parents is presented in .
Table 1. Demographic characteristics of participants.
The research was approved by the Ethics Committee of Beijing Normal University. Participants took part in the survey voluntarily and received a gift as compensation. Written informed consent was obtained before data collection.
2.2. Measures
2.2.1. Prolonged Grief Questionnaire (PG-13)
The PG-13 is a self-report measure of prolonged grief symptoms (Prigerson et al., Citation2009). The first two items assess separation distress: longing or yearning and emotional pain. Nine items assess cognitive, emotional and behavioural reactions, e.g. anger, numbness, difficulty accepting the loss, avoidance of reminders. The last two items evaluating functional impairment and length of bereavement are answered ‘yes’ or ‘no’. According to previous studies of the PGD network, the item of functional impairment and one item that indexes symptom duration don’t reflect a discrete symptom, so these two items were not included in the network (Maccallum & Bryant, Citation2020; Maccallum, Malgaroli, & Bonanno, Citation2017). The first 11 items scored on a 5-point Likert scale (1 = never, 5 = several times a day) were included in the network analysis. The Chinese version of PG-13 has sound psychometric properties (Yi, Gao, Wu, Tang, & Li, Citation2016), with Cronbach’s α being .72 in the current study.
2.2.2. PTSD checklist-civilian version (PCLC)
The PCLC is a widely used instrument to screen posttraumatic stress symptoms (Weathers, Litz, Herman, Huska, & Keane, Citation1993). It contains 17 items in three subdomains: re-experience, avoidance and numbing, and hyperarousal. Participants respond on a 5-point Likert scale from 1 (not at all) to 5 (extremely) to indicate symptoms’ severity of PTSD during the previous four weeks. Total scores range from 17 to 85, with higher scores representing more severe levels of posttraumatic stress symptoms. This study used a Chinese version of the PCLC, showing good reliability and validity (Yang, Yang, Liu, & Yang, Citation2007). The Cronbach’s alpha of the PCLC was .90 in this study.
2.2.3. Insomnia Severity Index (ISI)
ISI is a brief self-report tool to measure subjective symptoms and consequences of insomnia, as well as worries or distress about those problems (Bastien, Vallieres, & Morin, Citation2001). The Chinese version of ISI is a valid and reliable instrument for Chinese old people (Yu, Citation2010). It comprises seven items, and each item is rated from 0 (none) to 4 (very severe). A higher score indicates more severe insomnia problems. The Cronbach’s alpha of the ISI was .93 in this study.
2.3. Data analysis
2.3.1. Preliminary analyses
The maximum percentage of missing values was 3.5% for the PCLC item 8. Missing values were imputed using the Expectation-Maximization algorithm. Descriptive statistics were calculated to summarize participants’ demographic information, and means and standard deviations for the items. The preliminary analyses were conducted by SPSS 23.0 software.
2.3.2. Network analyses
Three network models were generated: (1) a network including the 11 symptoms presented in the PG-13; (2) a network concerning the co-occurrence of PGD and PTSD symptoms; and (3) a network regarding the co-occurrence of PGD and insomnia symptoms. All analyses related to network analyses were computed by R using RStudio. For analytic code (R-scripts) please see the Supplementary Materials.
2.3.2.1. Notes selection
It has been suggested that if two items are too similar in content, relationships in the network may be obscured (Fried & Cramer, Citation2017). Since PGD, PTSD and insomnia share certain similar symptoms, the goldbricker function in the networktools package was utilized to statistically detect redundant nodes in networks (Jones, Citation2020). Goldbricker function detects pairs of overlapping nodes by examining the correlations between them and comparing their patterns of correlations with other nodes in the network. If the two nodes are similarly correlated with (i.e. statistically different correlation below 25%) all other nodes, they are recognized as the redundant nodes (Hittner, May, & Silver, Citation2003). However, goldbricker function was best implemented with theoretical considerations (Levinson et al., Citation2018). Thus, we evaluated the statistically identified redundant nodes, and determined the final overlapping nodes based on their dimensions in the scale and proximity in meaning. The final overlapping nodes were combined into new nodes by calculating the mean values. In the PGD network, the goldbricker function detected that emotional pain, yearning and avoidance were overlapping. Since they were identified as distinct meaningful symptoms of PGD, they were all retained in the network analysis. Several pairs of statistically redundant nodes were identified in the PGD and PTSD network, as well as the PGD and insomnia network. Based on theoretical consideration, two sets of PTSD nodes were combined: (1) Difficulty concentrating, feeling irritable, feeling easily startled, and being super alert were combined into a ‘high arousal’ node; (2) feeling distant from others and loss of interest were collapsed into a ‘disengagement’ node. Two insomnia symptoms were combined: interference with daily function and worriers about sleep were collapsed into a ‘function-worry’ node.
2.3.2.2. Network estimation techniques
The network analyses were carried out by bootnet and qgraph packages in R. First, a Gaussian graphical model (Costantini et al., Citation2015), which calculates partial correlations between nodes, was used to generate regularized partial networks (Epskamp & Fried, Citation2018). Second, a graphical least absolute shrinkage and selection operator (gLASSO) was employed in combination with Extended Bayesian Information Criterion (EBIC) to shrink weak associations to zero. Then, node placement was determined by the Fruchterman and Reingold (Citation1991) algorithm, which puts nodes with stronger associations with other nodes nearer to the centre. To measure the importance of each symptom in the PGD network, the strength of nodes was calculated as it is considered the most reliable index of centrality (Epskamp, Borsboom, et al., Citation2018). Strength is defined as the sum of absolute edge weights between a given node and all other nodes (McNally, Citation2016). Bridge strength was estimated via the networktools package (Jones et al., Citation2019) in two co-occurrence networks (Network 2 and Network 3) to identify the nodes that share the strongest associations with the nodes belonging to the other community. Bridge strength refers to the sum of the absolute values of all edge weights between a given node and all nodes in different communities (Jones et al., Citation2019). Compared to the strength index, bridge strength takes into account community membership (Jones et al., Citation2019). It is suggested that a restricted range of symptoms variance can distort the estimation of centrality indices (Terluin, de Boer, & de Vet, Citation2016). Following previous publications (Wasil, Venturo-Conerly, Shinde, Patel, & Jones, Citation2020), correlations between strength (bridge strength for Network 2 and Network 3) and variance for each node were tested to address the problem.
2.3.2.3. Network stability and accuracy
The stability and accuracy of networks were estimated using bootnet packages in R. Following the recommendations of Epskamp, Borsboom, et al. (Citation2018), edge stability was estimated using non-parametric bootstrapping procedures. Bootstrapped confidence intervals were employed to gauge the certainty of edge weights and test for the significant differences between edges to check if a given edge is significantly larger than other edges. To measure the stability of centrality indices (strength and bridge strength), we utilized case-dropping bootstrapping method. This method repeatedly resamples subsets retaining 10–75% of the original data to estimate the network and generates a correlation-stability (CS) coefficient for each network. The CS coefficient indicates the maximum proportion of the data that can be dropped while the centrality indices remain highly correlated (>0.70) to the original centrality indices. CS coefficients above 0.25 are acceptable, and above 0.50 are good (Epskamp, Borsboom, et al., Citation2018).
3. Results
3.1. Descriptive statistics
The mean scores, standard deviations and abbreviation of each PGD, PTSD and insomnia symptom included in networks are presented in . For PGD symptoms, yearning is the most frequently endorsed symptom with a mean score of 4.47, while inability to trust others has the lowest mean score of 2.75.
Table 2. Notes included in network analysis.
3.2. Network stability
Three estimated networks were demonstrated to be robust to the stability test. The PGD network demonstrated high stability for strength (CS coefficient = 0.52). Non-parametric bootstrapping showed that edge weights were estimated with moderate confidence intervals. The bootstrap difference test for edges and strength indicated that the strongest edges and the central nodes were significantly different from the other edges and nodes (For figures related to network stability, please see Supplementary Materials).
The PGD and PTSD network as well as PGD and insomnia network showed acceptable to good stability with CS coefficients of bridge strength being 0.44 and 0.59, respectively. For all three networks, the estimated strength (or bridge strength) wasn’t significantly correlated with node variance (Network 1: r = –.15, p = .66; Network 2: r = .32, p = .13; Network 3: r = .28, p = .28). Therefore, the differential variability of symptoms didn’t explain the strength (or bridge strength).
3.3. Network 1: PGD network
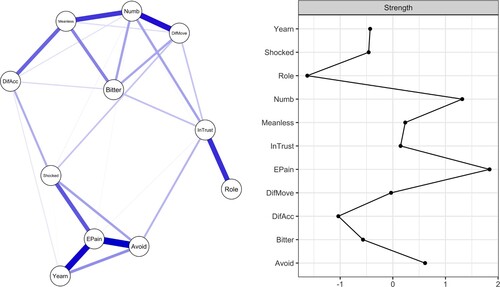
The generated PGD network is shown in . Emotional pain and numbness emerged as the most central symptoms in the network, with their strengths significantly higher than 50% of other nodes. The least central node as indicated by the strength index was role confusion. Several edges that stood out included emotional pain and avoidance, emotional pain and yearning, and difficulty moving on and numbness.
Figure 1. Estimated network model for PGD symptoms with strength. (a) (left) illustrates the network of PGD symptoms. Nodes represent symptoms of PGD and edge thickness indicates the strength of partial correlation between nodes. (b) (right) depicts the strength of each symptom of the PGD network. Strength is shown as standardized z-scores.
Notes: Yearn = Yearning; EPain = Emotional pain; Avoid = Avoidance of reminders; Shocked = Feeling stunned or shocked; Role = Role confusion; DifAcc = Difficulty accepting the loss; InTrust = Inability to trust others; Bitter = Bitterness or anger related to the loss; DifMove = Difficulty moving on; Numb = Numbness; Meanless = Feeling that life is meaningless.
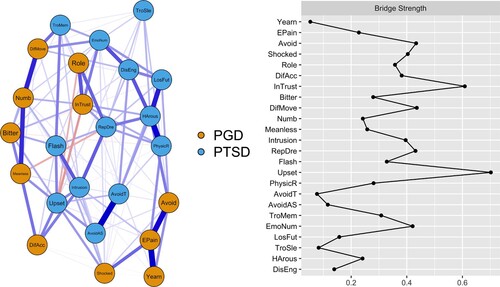
3.4. Network 2: PGD and PTSD network
The estimated network of PGD and PTSD symptoms is provided in . The symptoms with the highest bridge strength were the inability to trust others (PGD) and feeling upset (PTSD). Inability to trust (PGD) was closely related to PTSD symptoms of emotional numbness, high arousal, physical reactions, and repetitive dreams. Stable connections also emerged between feeling upset (PTSD) and PGD symptoms of feeling meaningless, difficulty accepting loss, and feeling shocked.
Figure 2. Network model for PGD and PTSD symptoms with strength. (a) (left) depicts the network of PGD symptoms and PTSD symptoms. (b) (right) depicts the bridge strength of each symptom of the PGD and PTSD network.
Notes: Yearn = Yearning; EPain = Emotional pain; Avoid = Avoidance of reminders; Shocked = Feeling stunned or shocked; Role = Role confusion; DifAcc = Difficulty accepting the loss; InTrust = Inability to trust others; Bitter = Bitterness; DifMove = Difficulty moving on; Numb = Numbness; Meanless = Feeling life is meaningless; Intrusion = Intrusive memories or thoughts; RepDre = Repeated, disturbing dreams; Flash = Feeling as if it were happening again; Upset = Feeling very upset; PhysicR = Having physical reactions; AvoidT = Avoid thinking or talking; AvoidAS = Avoid activities or situations; TroMem = Trouble memories; LosInt = Loss of interest; Distant = Feeling distant; EmoNum = Feeling emotionally numb; LosFut = Feeling future will somehow be cut short; TroSle = Trouble falling asleep; HArous = High arousal.
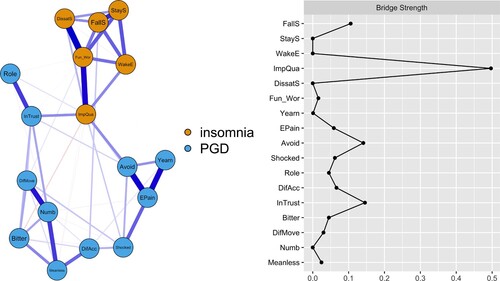
3.5. Network 3: PGD and insomnia network
depicts the network and bridge strength of PGD and insomnia symptoms. The symptoms with the highest bridge strength were inability to trust others (PGD), avoidance of reminders of the loss (PGD) and impairment of life quality (insomnia). Strong associations were shared between the bridge symptoms of PGD and insomnia.
Figure 3. Network model for PGD and insomnia symptoms with strength. (a) (left) shows the network of PGD symptoms and insomnia symptoms. (b) (right) illustrates the bridge strength of each symptom of the PGD and insomnia network.
Notes: Yearn = Yearning; EPain = Emotional pain; Avoid = Avoidance of reminders; Shocked = Feeling stunned or shocked; Role = Role confusion; DifAcc = Difficulty accepting the loss; InTrust = Inability to trust others; Bitter = Bitterness or anger related to the loss; DifMove = Difficulty moving on; Numb = Numbness; Meanless = Feeling life is meaningless; FallS = Difficulty falling asleep; Stay = Difficulty staying asleep; WakeE = Problems waking up too early; DissatS = Dissatisfied with sleep pattern; ImpQua = Impairing the quality of your life; Fun_Wor = Interference with daily function and worriers about sleep.
4. Discussion
To the best of our knowledge, this was the first study to explore the PGD symptoms network, as well as the comorbidity networks of PGD with PTSD and insomnia in a sample of Chinese shidu parents with PGD. Although network analyses based on current data were exploratory, tentative interpretations provide some information for future research and treatment for shidu parents.
Significantly positive correlations between each symptom in the PGD network provided evidence for the syndromic integrity of PGD. In line with previous studies, the emotional pain was the most central symptom in shidu parents with PGD (Maccallum et al., Citation2017; Robinaugh et al., Citation2014; Stelzer, Holtge, et al., Citation2020). The second central symptom was emotional numbness, a prominent node at 11 months post-loss in a spousal bereaved sample (Maccallum, Lundorff, Johannsen, Farver-Vestergaard, & O'Connor, Citation2021). One symptom that exists as central to the network might be because it is a cause of activation, or because it is activated by many other symptoms (Maccallum et al., Citation2017). For most Chinese parents, the only child carries their hope for the future, represents the continuation of their bloodline, and is their primary caregiver when they are old. Losing the only child may mean losing all of these, which may be too difficult for parents to bear (Xu et al., Citation2020). Therefore, emotional pain and numbness may lead to other cognitive or behavioural symptoms, and other symptoms may in turn cause shidu parents’ emotional pain and numbness.
Similar to previous network studies, strong connections were found between emotional pain and yearning, as well as with avoidance among our sample (Maccallum et al., Citation2017; Robinaugh et al., Citation2014; Stelzer, Holtge, et al., Citation2020). Robinaugh et al. (Citation2014) suggested that thoughts about death may cause emotional pain for bereaved individuals, who would thus avoid it. However, avoidance may in turn lead to thoughts related to death, which is highly related to emotional pain and yearning. Therefore, these symptoms may form a potential positive feedback loop contributing to the maintenance of PGD, and emotional pain appears to play a crucial part in it.
Role confusion turned out to be a peripheral symptom of shidu parents with PGD. In a longitudinal study, role confusion was the most central element in the network at 3 and 14 months post-loss, while loneliness displayed the greatest strength centrality at 25 months post-loss (Malgaroli, Maccallum, & Bonanno, Citation2018). Even though role confusion also stayed relatively central, its importance in the network decreased over time. This finding suggested that role confusion may deserve close attention in early bereavement. However, this symptom’s influence on the whole network may be reduced in the long term. There is no doubt that losing an only child would challenge shidu parents’ self-identity as a ‘mother’ or ‘father’ (Zheng & Lawson, Citation2015). However, the bereavement length of our current sample was 7.82 years, which might explain why role confusion was the least connected node in the grief network. Nevertheless, it should be noted that although role confusion was the least central symptom in our sample, the low interconnectedness of other symptoms does not necessarily mean that the role confusion is not theoretically or clinically meaningful.
An interesting finding of the study is that inability to trust others was identified as a bridge symptom for both PGD and PTSD as well as PGD and insomnia networks, while it was the least severe symptom of PGD in the current sample of shidu parents. As McNally (Citation2021) proposed, there is not only one standard for defining important symptoms. Therapists may treat the most severe or dangerous (e.g. suicidal ideation) symptoms as the most clinically significant symptoms. However, network researchers have tried to identify influential symptoms that are most strongly interconnected with other symptoms. Social isolation is common for shidu parents (Xu et al., Citation2020). Inability to trust others may exacerbate shidu parents’ social isolation, which has a significant impact on mental health, sleep disturbance, as well as the quality of life (Choi, Irwin, & Cho, Citation2015; Cornwell & Waite, Citation2009). One previous network study found that difficulty trusting others was related to low social functioning, and social functioning itself may serve as a protective factor (Maccallum & Bryant, Citation2020). Therefore, although difficulty trusting others is the least frequently endorsed symptom of PGD, it might interact with other trauma-related symptoms or insomnia symptoms in multiple pathways, and further deteriorate shidu parents’ mental health. The difficulty trusting others seems to play an essential role as a bridge, consistent with the emphasis on strengthening interpersonal relationships in an efficacious treatment for PGD (Iglewicz et al., Citation2020; Shear & Gribbin Bloom, Citation2017). Our results provided evidence supporting the findings of a recent study that symptoms related to social relationships may not be negligible in PGD comorbidity networks (Djelantik, Robinaugh, et al., Citation2020).
The PTSD symptom of feeling upset was identified as a possible bridging symptom to drive the PGD and PTSD comorbidity. Considering mental disorders are generally accompanied by emotional distress, and emotional pain is a crucial character of PGD, the result is not surprising. The bridging role of feeling upset is in accordance with empirical evidence that comorbidity is a natural consequence of partially overlapping symptoms (Afzali et al., Citation2017; Cramer et al., Citation2010; McNally, Citation2021).
Evidence has demonstrated that PGD has an association with sleep disturbance (Lancel et al., Citation2020). The current study results expanded previous researches by finding that, in addition to the PGD symptom of inability to trust others, avoidance of reminders of the loss was also strongly connected to impairment of quality of life caused by insomnia, which could be theorized to constitute a pathway across PGD and insomnia. Although avoidance may effectively relieve emotional pain in a short time, theoretical models and empirical evidence demonstrate that avoidance can interfere with adapting to the loss in the long run (Boelen et al., Citation2006; Boelen & Eisma, Citation2015; Lechner-Meichsner, Mauro, Skritskaya, & Shear, Citation2021). Meanwhile, impaired quality of life may influence shidu parents’ social activities and lead to shidu parents’ social disconnection. Therefore, the interplay between symptoms of difficulty trusting others, avoidance of reminders and impairment of life quality might constitute a pathway across PGD and insomnia.
4.1. Implications
The current findings based on cross-sectional data provide exploratory insight on relationships between symptoms and might be informative for future research or treatment (Epskamp, Waldorp, et al., Citation2018). First, together with previous network research (Robinaugh, Millner, & McNally, Citation2016), our results suggest that reduction in emotional pain might be promising to reduce overall network activation for shidu parents with PGD. Second, the network analysis results suggest that the role of difficulty trusting others may deserve further study, which has received relatively little attention in PGD research (Maccallum & Bryant, Citation2020). It might be rewarding to keep a close eye on the symptom of difficulty in trusting others. If so, an evidenced-based treatment for PGD that includes a theme of strengthening ongoing relationships could be considered for shidu parents (Shear et al., Citation2016). Furthermore, although it may be common for shidu parents to report insomnia, therapists may need to accurately evaluate the extent to which sleep problems has interfered with their quality of life. The above-cited literature suggested that it is optimal to incorporate sleep-focused treatment into standard treatment for PGD when insomnia causes a significant impairment (Boelen & Lancee, Citation2013).
However, it should be noted that these tentative findings were based on correlational analyses, rather than a causal relationship. Therefore, the results need to be further examined with time series data or pre–post intervention data. Additionally, increasing network researchers highlighted that highly central symptoms are not automatically viable intervention targets (Fried et al., Citation2018; Stelzer, Holtge, et al., Citation2020). Furthermore, it is difficult to target a single symptom without simultaneously affecting other symptoms (McNally, Citation2021). Consequently, a network perspective should not be understood as that only high centrality nodes and bridge symptoms are clinically meaningful.
4.2. Limitations
Some limitations of the current study should be mentioned. First, although we collected our data across China, the sample was recruited by a convenience sampling process. Moreover, our sample only consisted of shidu parents with PGD, which could lead to Berkson’s bias (de Ron, Fried, & Epskamp, Citation2021). Therefore, the analyses of the current study must be considered preliminary and the generalization of our results requires caution. Second, the diagnosis of PGD in the current study was relied on items combined from two self-report measures. Therefore, without a clinical interview, only probable PGD cases were included to analyze. Moreover, we used the PCLC to measure PTSD symptoms according to the DSM-IV, rather than the new diagnostic instrument Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5). Third, this is a cross-sectional study. No causal relationship between symptoms can be concluded based on the current data. Future studies using a clinical interview to confirm PGD cases are encouraged to investigate the relationship between symptoms over time.
5. Conclusion
The current study findings indicated that emotional pain and numbness were the most influential symptoms in the network of shidu parents with PGD. The PGD symptom of inability to trust others may be a symptom worthy of further study, which seems to play a role in the development and maintenance of PGD comorbidity. Meanwhile, when working with shidu parents with PGD, it might be helpful to accurately assess the levels of emotional distress, avoidance of reminders of the death and impairment of life quality caused by insomnia, which are hypothesized to foster diagnostic comorbidity of PGD.
Supplemental Material
Download MS Word (266.1 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
We agree that data sharing will help the advance of research. However, the data published here come from an ongoing project. The data are still accumulating. We would like to make it publicly available after the entire project is over. Therefore, all data used in the current study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Afzali, M. H., Sunderland, M., Teesson, M., Carragher, N., Mills, K., & Slade, T. (2017). A network approach to the comorbidity between posttraumatic stress disorder and major depressive disorder: The role of overlapping symptoms. Journal of Affective Disorders, 208, 490–496. doi:10.1016/j.jad.2016.10.037
- American Psychological Association. (2021). Prolonged grief disorder. Diagnostic and statistical manual of mental disorders, fifth edition, text revision (DSM-5-TR™). Arlington, VA: Author.
- Bastien, C. H., Vallieres, A., & Morin, C. M. (2001). Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine, 2(4), 297–307. Article Pii s1389-9457(00)00065-4. doi:10.1016/s1389-9457(00)00065-4
- Boelen, P. A., & Eisma, M. C. (2015). Anxious and depressive avoidance behavior in post-loss psychopathology: A longitudinal study. Anxiety, Stress, & Coping, 28(5), 587–600. doi:10.1080/10615806.2015.1004054
- Boelen, P. A., & Lancee, J. (2013). Sleep difficulties are correlated with emotional problems following loss and residual symptoms of effective prolonged grief disorder treatment. Depression Research and Treatment, 2013, 739804. doi:10.1155/2013/739804
- Boelen, P. A., & Lenferink, L. I. M. (2020). Symptoms of prolonged grief, posttraumatic stress, and depression in recently bereaved people: Symptom profiles, predictive value, and cognitive behavioural correlates. Social Psychiatry and Psychiatric Epidemiology, 55(6), 765–777. doi:10.1007/s00127-019-01776-w
- Boelen, P. A., & Prigerson, H. G. (2007). The influence of symptoms of prolonged grief disorder, depression, and anxiety on quality of life among bereaved adults: A prospective study. European Archives of Psychiatry and Clinical Neuroscience, 257(8), 444–452. doi:10.1007/s00406-007-0744-0
- Boelen, P. A., van den Hout, M. A., & van den Bout, J. (2006). A cognitive-behavioral conceptualization of complicated grief. Clinical Psychology: Science & Practice, 13(2), 109–128. doi:10.1111/j.1468-2850.2006.00013.x
- Borsboom, D. (2017). A network theory of mental disorders. World Psychiatry, 16(1), 5–13. doi:10.1002/wps.20375
- Borsboom, D., & Cramer, A. O. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121. doi:10.1146/annurev-clinpsy-050212-185608
- Cao, X., Yang, C., & Wang, D. (2018). The impact on mental health of losing an only child and the influence of social support and resilience. Omega. doi:10.1177/0030222818755284
- Choi, H., Irwin, M. R., & Cho, H. J. (2015). Impact of social isolation on behavioral health in elderly: Systematic review. World Journal of Psychiatry, 5(4), 432–438. doi:10.5498/wjp.v5.i4.432
- Cornwell, E. Y., & Waite, L. J. (2009). Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior, 50(1), 31–48. doi:10.1177/002214650905000103
- Costantini, G., Epskamp, S., Borsboom, D., Perugini, M., Mottus, R., Waldorp, L. J., & Cramer, A. O. J. (2015). State of the aRt personality research: A tutorial on network analysis of personality data in R. Journal of Research in Personality, 54, 13–29. doi:10.1016/j.jrp.2014.07.003
- Cozza, S. J., Shear, M. K., Reynolds, C. F., Fisher, J. E., Zhou, J., Maercker, A., … Ursano, R. J. (2020). Optimizing the clinical utility of four proposed criteria for a persistent and impairing grief disorder by emphasizing core, rather than associated symptoms. Psychological Medicine, 50(3), 438–445. doi:10.1017/S0033291719000254
- Cramer, A. O., Waldorp, L. J., van der Maas, H. L., & Borsboom, D. (2010). Comorbidity: A network perspective. Behavioral and Brain Sciences, 33(2–3), 137–150; discussion 150–193. doi:10.1017/S0140525X09991567
- de Ron, J., Fried, E. I., & Epskamp, S. (2021). Psychological networks in clinical populations: Investigating the consequences of Berkson's bias. Psychological Medicine, 51(1), 168–176. doi:10.1017/S0033291719003209
- Djelantik, A., Robinaugh, D. J., Kleber, R. J., Smid, G. E., & Boelen, P. A. (2020). Symptomatology following loss and trauma: Latent class and network analyses of prolonged grief disorder, posttraumatic stress disorder, and depression in a treatment-seeking trauma-exposed sample. Depression and Anxiety, 37(1), 26–34. doi:10.1002/da.22880
- Djelantik, A., Smid, G. E., Mroz, A., Kleber, R. J., & Boelen, P. A. (2020). The prevalence of prolonged grief disorder in bereaved individuals following unnatural losses: Systematic review and meta regression analysis. Journal of Affective Disorders, 265, 146–156. doi:10.1016/j.jad.2020.01.034
- Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. doi:10.1016/s0005-7967(99)00123-0
- Enders, C. K. (2003). Using the expectation maximization algorithm to estimate coefficient alpha for scales with item-level missing data. Psychological Methods, 8(3), 322–337. doi:10.1037/1082-989X.8.3.322
- Epskamp, S., Borsboom, D., & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212. doi:10.3758/s13428-017-0862-1
- Epskamp, S., & Fried, E. I. (2018). A tutorial on regularized partial correlation networks. Psychological Methods, 23(4), 617–634. doi:10.1037/met0000167
- Epskamp, S., Waldorp, L. J., Mottus, R., & Borsboom, D. (2018). The Gaussian graphical model in cross-sectional and time-series data. Multivariate Behavioral Research, 53(4), 453–480. doi:10.1080/00273171.2018.1454823
- Fried, E. I., & Cramer, A. O. J. (2017). Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science, 12(6), 999–1020. doi:10.1177/1745691617705892
- Fried, E. I., Eidhof, M. B., Palic, S., Costantini, G., Huisman-van Dijk, H. M., Bockting, C. L. H., … Karstoft, K. I. (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: A cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science, 6(3), 335–351. doi:10.1177/2167702617745092
- Fruchterman, T. M. J., & Reingold, E. M. (1991). Graph drawing by force-directed placement. Software: Practice and Experience, 21(11), 1129–1164. doi:doi:10.1002/spe.4380211102
- Hittner, J. B., May, K., & Silver, N. C. (2003). A Monte Carlo evaluation of tests for comparing dependent correlations. The Journal of General Psychology, 130(2), 149–168. doi:10.1080/00221300309601282
- Hofmann, S. G., Curtiss, J., & McNally, R. J. (2016). A complex network perspective on clinical science. Perspectives on Psychological Science, 11(5), 597–605. doi:10.1177/1745691616639283
- Iglewicz, A., Shear, M. K., Reynolds, C. F., Simon, N., Lebowitz, B., & Zisook, S. (2020). Complicated grief therapy for clinicians: An evidence-based protocol for mental health practice. Depression and Anxiety, 37(1), 90–98. doi:10.1002/da.22965
- Jones, P. J. (2020). Networktools: Tools for identifying important nodes in networks. R Package, Version 1.2.3. Retrieved from https://CRAN.R-project.org/package=networktools
- Jones, P. J., Ma, R., & McNally, R. J. (2019). Bridge centrality: A network approach to understanding comorbidity. Multivariate Behavioral Research, 1–15. doi:10.1080/00273171.2019.1614898
- Kaltman, S., & Bonanno, G. A. (2003). Trauma and bereavement. Journal of Anxiety Disorders, 17(2), 131–147. doi:10.1016/s0887-6185(02)00184-6
- Kersting, A., Brahler, E., Glaesmer, H., & Wagner, B. (2011). Prevalence of complicated grief in a representative population-based sample. Journal of Affective Disorders, 131(1–3), 339–343. doi:10.1016/j.jad.2010.11.032
- Lancel, M., Stroebe, M., & Eisma, M. C. (2020). Sleep disturbances in bereavement: A systematic review. Sleep Medicine Reviews, 53, 101331. doi:10.1016/j.smrv.2020.101331
- Lechner-Meichsner, F., Mauro, C., Skritskaya, N. A., & Shear, M. K. (2021). Change in avoidance and negative grief-related cognitions mediates treatment outcome in older adults with prolonged grief disorder. Psychotherapy Research, 1–13. doi:10.1080/10503307.2021.1909769
- Levinson, C. A., Brosof, L. C., Vanzhula, I., Christian, C., Jones, P., Rodebaugh, T. L., … Fernandez, K. C. (2018). Social anxiety and eating disorder comorbidity and underlying vulnerabilities: Using network analysis to conceptualize comorbidity. International Journal of Eating Disorders, 51(7), 693–709. doi:10.1002/eat.22890
- Lommen, M. J., Grey, N., Clark, D. M., Wild, J., Stott, R., & Ehlers, A. (2016). Sleep and treatment outcome in posttraumatic stress disorder: Results from an effectiveness study. Depression and Anxiety, 33(7), 575–583. doi:10.1002/da.22420
- Lundorff, M., Holmgren, H., Zachariae, R., Farver-Vestergaard, I., & O'Connor, M. (2017). Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta-analysis. Journal of Affective Disorders, 212, 138–149. doi:10.1016/j.jad.2017.01.030
- Maccallum, F., & Bryant, R. A. (2020). A network approach to understanding quality of life impairments in prolonged grief disorder. Journal of Traumatic Stress, 33(1), 106–115. doi:10.1002/jts.22383
- Maccallum, F., Lundorff, M., Johannsen, M., Farver-Vestergaard, I., & O'Connor, M. (2021). An exploration of gender and prolonged grief symptoms using network analysis. Psychological Medicine, 1–8. doi:10.1017/S0033291721003391
- Maccallum, F., Malgaroli, M., & Bonanno, G. A. (2017). Networks of loss: Relationships among symptoms of prolonged grief following spousal and parental loss. Journal of Abnormal Psychology, 126(5), 652–662. doi:10.1037/abn0000287
- Malgaroli, M., Maccallum, F., & Bonanno, G. A. (2018). Symptoms of persistent complex bereavement disorder, depression, and PTSD in a conjugally bereaved sample: A network analysis. Psychological Medicine, 48(14), 2439–2448. doi:10.1017/S0033291718001769
- McNally, R. J. (2016). Can network analysis transform psychopathology? Behaviour Research and Therapy, 86, 95–104. doi: 10.1016/j.brat.2016.06.006
- McNally, R. J. (2021). Network analysis of psychopathology: Controversies and challenges. Annual Review of Clinical Psychology, 17, 31–53. doi:10.1146/annurev-clinpsy-081219-092850
- Nappi, C. M., Drummond, S. P., & Hall, J. M. (2012). Treating nightmares and insomnia in posttraumatic stress disorder: A review of current evidence. Neuropharmacology, 62(2), 576–585. doi:10.1016/j.neuropharm.2011.02.029
- Pan, H. (2020). Deepening the understanding of complicated grief among Chinese older adults: A network approach. Asian Journal of Psychiatry, 50, 101966. doi:10.1016/j.ajp.2020.101966
- Peng, J., Harwell, M., Liou, S. M., & Ehman, L. H. (2006). Advances in missing data methods and implications for educational research. In S. S. Sawilowsky (Ed.), Real data analysis (pp. 31–78). New York: Elsevier.
- Prigerson, H. G., Bierhals, A. J., Kasl, S. V., Reynolds, C. F., Shear, M. K., Day, N., … Jacobs, S. (1997). Traumatic grief as a risk factor for mental and physical morbidity. American Journal of Psychiatry, 154(5), 616–623. doi:10.1176/ajp.154.5.616
- Prigerson, H. G., Horowitz, M. J., Jacobs, S. C., Parkes, C. M., Aslan, M., Goodkin, K., … Maciejewski, P. K. (2009). Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Medicine, 6(8), e1000121. doi:10.1371/journal.pmed.1000121
- Prigerson, H. G., Kakarala, S., Gang, J., & Maciejewski, P. K. (2021). History and status of prolonged grief disorder as a psychiatric diagnosis. Annual Review of Clinical Psychology. doi:10.1146/annurev-clinpsy-081219-093600
- Robinaugh, D. J., LeBlanc, N. J., Vuletich, H. A., & McNally, R. J. (2014). Network analysis of persistent complex bereavement disorder in conjugally bereaved adults. Journal of Abnormal Psychology, 123(3), 510–522. doi:10.1037/abn0000002
- Robinaugh, D. J., Millner, A. J., & McNally, R. J. (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125(6), 747–757. doi:10.1037/abn0000181
- Shear, K., & Shair, H. (2005). Attachment, loss, and complicated grief. Developmental Psychobiology, 47(3), 253–267. doi:doi:10.1002/dev.20091
- Shear, M. K. (2015). Clinical practice. Complicated grief. The New England Journal of Medicine, 372(2), 153–160. doi:10.1056/NEJMcp1315618
- Shear, M. K., & Gribbin Bloom, C. (2017). Complicated grief treatment: An evidence-based approach to grief therapy. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 35(1), 6–25. doi:10.1007/s10942-016-0242-2
- Shear, M. K., Reynolds, C. F., Simon, N. M., Zisook, S., Wang, Y., Mauro, C., … Skritskaya, N. (2016). Optimizing treatment of complicated grief: A randomized clinical trial. JAMA Psychiatry, 73(7), 685–694. doi:10.1001/jamapsychiatry.2016.0892
- Shear, M. K., & Skritskaya, N. A. (2012). Bereavement and anxiety. Current Psychiatry Reports, 14(3), 169–175. doi:10.1007/s11920-012-0270-2
- Shi, G. Y., Wen, J., Xu, X., Zhou, N. N., Wang, J. N., Shi, Y. Q., … Stelzer, E. M. (2019). Culture-related grief beliefs of Chinese shidu parents: Development and psychometric properties of a new scale. European Journal of Psychotraumatology, 10(1), 1626075. doi:10.1080/20008198.2019.1626075
- Spoormaker, V. I., & Montgomery, P. (2008). Disturbed sleep in post-traumatic stress disorder: Secondary symptom or core feature? Sleep Medicine Reviews, 12(3), 169–184. doi:10.1016/j.smrv.2007.08.008
- Stelzer, E. M., Holtge, J., Zhou, N., Maercker, A., & Killikelly, C. (2020). Cross-cultural generalizability of the ICD-11 PGD symptom network: Identification of central symptoms and culturally specific items across German-speaking and Chinese bereaved. Comprehensive Psychiatry, 103, 152211. doi:10.1016/j.comppsych.2020.152211
- Stelzer, E. M., Zhou, N., Maercker, A., O'Connor, M. F., & Killikelly, C. (2020). Prolonged grief disorder and the cultural crisis. Frontiers in Psychology, 10, 2982. doi:10.3389/fpsyg.2019.02982
- Stroebe, M., Schut, H., & Stroebe, W. (2007). Health outcomes of bereavement. The Lancet, 370(9603), 1960–1973. doi:10.1016/s0140-6736(07)61816-9
- Tan, H., Lan, X. M., Yu, N. L., & Yang, X. C. (2015). Reliability and validity assessment of the revised symptom checklist 90 for alopecia areata patients in China. Journal of Dermatology, 42(10), 975–980. doi:10.1111/1346-8138.12976
- Terluin, B., de Boer, M. R., & de Vet, H. C. (2016). Differences in connection strength between mental symptoms might be explained by differences in variance: Reanalysis of network data did not confirm staging. PLoS One, 11(11), e0155205. doi: 10.1371/journal.pone.0155205
- Wang, G. (2016). Research on the total population, age structure and developing trend of the lost only child women by computer simulation. Population and Economics, 5, 1–11.
- Wang, N., & Hu, Q. (2019). ‘It is not simply the loss of a child’: The challenges facing parents who have lost their only child in post-reproductive age in China. Death Studies. doi:10.1080/07481187.2019.1626941
- Wang, N., & Hu, Q. (2020). Loneliness trajectories: Evidence for staged intervention among Chinese bereaved parents. Journal of Applied Gerontology. doi:10.1177/0733464820978808
- Wang, Q., Zhang, S., Wang, Y., Jing, Z., Zhou, Y., Qi, K., … Zhou, C. (2021). Prevalence and risk factors of posttraumatic stress disorder among Chinese shidu parents: A systemic review and meta-analysis. Journal of Affective Disorders, 282, 1180–1186. doi:10.1016/j.jad.2021.01.017
- Wasil, A. R., Venturo-Conerly, K. E., Shinde, S., Patel, V., & Jones, P. J. (2020). Applying network analysis to understand depression and substance use in Indian adolescents. Journal of Affective Disorders, 265, 278–286. doi:10.1016/j.jad.2020.01.025
- Weathers, F., Litz, B., Herman, D., Huska, J. A., & Keane, T. (1993). PTSD checklist: Reliability, validity, and diagnostic utility.
- Wittouck, C., Van Autreve, S., De Jaegere, E., Portzky, G., & van Heeringen, K. (2011). The prevention and treatment of complicated grief: A meta-analysis. Clinical Psychology Review, 31(1), 69–78. doi:10.1016/j.cpr.2010.09.005
- World Health Organization. (2018). ICD-11 for mortality and morbidity statistics. 6B42 prolonged grief disorder.
- Xu, X., Wen, J., Zhou, N., Shi, G., Tang, R., Wang, J., & Skritskaya, N. A. (2020). Grief and posttraumatic growth among Chinese bereaved parents who lost their only child: The moderating role of interpersonal loss. Frontiers in Psychology, 11, 558313. doi:10.3389/fpsyg.2020.558313
- Yang, X., Yang, H., Liu, Q., & Yang, L. (2007). The research on the reliability and validity of PCL-C and influence factors. China Journal of Health Psychology, 15(1), 6–9.
- Yi, X., Gao, J., Wu, C., Tang, N., & Li, Y. (2016). Reliability and validity of the Chinese version of prolonged grief disorder questionnaire. Chongqing Medicine, 45(7), 943–946.
- Yin, Q., Shang, Z., Zhou, N., Wu, L., Liu, G., Yu, X., … Liu, W. (2018). An investigation of physical and mental health consequences among Chinese parents who lost their only child. BMC Psychiatry, 18(1), 45. doi:10.1186/s12888-018-1621-2
- Yu, D. S. F. (2010). Insomnia Severity Index: Psychometric properties with Chinese community-dwelling older people. Journal of Advanced Nursing, 66(10), 2350–2359. doi:10.1111/j.1365-2648.2010.05394.x
- Zhang, H., Shang, Z., Wu, L., Sun, Z., Zhang, F., Sun, L., … Liu, W. (2020). Prolonged grief disorder in Chinese shidu parents who have lost their only child. European Journal of Psychotraumatology, 11(1), 1726071. doi:10.1080/20008198.2020.1726071
- Zhang, Y., & Jia, X. (2019). The effect of autobiographical memory function on depression and anxiety in Chinese shiduers (parents who have lost their only child): The moderating role of familistic emotion. Death Studies, 1–9. doi:10.1080/07481187.2019.1626948
- Zheng, Y., & Lawson, T. R. (2015). Identity reconstruction asshiduers: Narratives from Chinese older adults who lost their only child. International Journal of Social Welfare, 24(4), 399–406. doi:10.1111/ijsw.12139
- Zheng, Y., Lawson, T. R., & Anderson Head, B. (2017). ‘Our only child has died’ – a study of bereaved older Chinese parents. Omega, 74(4), 410–425. doi:10.1177/0030222815612285
- Zhou, N., Wen, J., Stelzer, E. M., Killikelly, C., Yu, W., Xu, X., … Maercker, A. (2020). Prevalence and associated factors of prolonged grief disorder in Chinese parents bereaved by losing their only child. Psychiatry Research, 284, 112766. doi:10.1016/j.psychres.2020.112766
- Zhou, N., Yu, W., Huang, H., Shi, G., Luo, H., Song, C., … Killikelly, C. (2018). Latent profiles of physical and psychological outcomes of bereaved parents in China who lost their only child. European Journal of Psychotraumatology, 9(1), 1544026. doi:10.1080/20008198.2018.1544026
