ABSTRACT
Background
Historically, resilience has often been conceptualized as the sustained lack of symptoms following trauma exposure. In line with a novel conceptualization of resilience as being dynamic over lifespan, determined by interacting biological and environmental factors, we examined the VA Mid-Atlantic Post Deployment Mental Health Repository (PDMH) comprised of 3876 US Military Veterans with and without PTSD diagnoses.
Methods
We performed regression modelling to study the relationship between resilience (measured with Connor Davidson Resilience Scale; CD-RISC), posttraumatic stress disorder (PTSD) severity (Davidson Trauma Scale; DTS), social support (Medical Outcome Study Social Support Survey; MOSSS), combat exposure (Combat Exposure Scale; CES), childhood trauma (Trauma Life Events Questionnaire; TLEQ), and demographic factors. CD-RISC was positively correlated with years of education and negatively correlated with DTS, CES and TLEQ scores.
Results
We found an interaction between CD-RISC and CES in predicting PTSD severity (Davidson Trauma Scale). Specifically, high resilience predicted lower PTSD symptom severity than low resilience, this relationship was amplified with increasing levels of combat exposure. Structural equation modelling (SEM) identified an optimal latent variable that represents resilience and relationships between latent variables for resilience, trauma, and illness. We derived a resilience latent variable composed of age, education level, MOSSS and race.
Conclusions
Our results support a conceptualization of resilience as a multifactorial determinant that coexists with PTSD, a state rather than trait variable, and can be quantified by biological and behavioural metrics.
HIGHLIGHTS
• Historically, resilience has often been conceptualized as the sustained lack of symptoms following trauma exposure.
• We examined the VA Mid-Atlantic Post Deployment Mental Health Repository (PDMH) comprised of 3876 US Military Veterans.
• We found an interaction effect between CD-RISC and CES in predicting PTSD severity (Davidson Trauma Scale)
Antecedentes: Históricamente, la resiliencia a menudo se ha conceptualizado como la ausencia sostenida de síntomas después de la exposición al trauma. En línea con una novedosa conceptualización de la resiliencia como un fenómeno dinámico a lo largo de la vida, determinada por la interacción de factores biológicos y ambientales, examinamos el Repositorio de salud mental post-despliegue VA Mid-Atlantic (PDMH por sus siglas en ingles) compuesto por 3.876 veteranos militares de EE.UU. con y sin diagnósticos de TEPT.
Métodos: Realizamos modelos de regresión para estudiar la relación entre resiliencia (medida con la Escala de resiliencia de Connor Davidson; CD-RISC por sus siglas en ingles), gravedad del trastorno de estrés postraumático (TEPT) (con Escala de Trauma de Davidson; DTS por sus siglas en ingles), apoyo social (Encuesta de Estudio de Resultados Médicos - Apoyo Social; MOSSS por sus siglas en ingles), exposición al combate (Escala de exposición al combate; CES por sus siglas en ingles), trauma infantil (Cuestionario de Eventos de vida traumáticos; TLEQ por sus siglas en ingles), y factores demográficos. CD-RISC se correlacionó positivamente con años de educación y se correlacionó negativamente con los puntajes de DTS, CES y TLEQ.
Resultados: Encontramos una interacción entre CD-RISC y CES en la predicción de la gravedad del TEPT (Escala de trauma de Davidson). Específicamente, una alta resiliencia predijo menor gravedad de los síntomas de TEPT que una baja resiliencia, esta relación fue amplificada con niveles crecientes de exposición al combate. El modelo de ecuaciones estructurales (SEM por sus siglas en ingles) identificó una variable latente óptima que representa la resiliencia y las relaciones entre las variables latentes de resiliencia, trauma y enfermedad. Derivamos una variable latente de resiliencia compuesta por edad, nivel educativo, MOSSS y raza.
Conclusiones: Nuestros resultados apoyan una conceptualización de la resiliencia como un determinante multifactorial que coexiste con el TEPT, una variable de estado más que de rasgo, y puede ser cuantificada con mediciones biológicas y conductuales.
背景:从历史上看,心理韧性经常被概念化为创伤暴露后持续缺乏症状。根据由相互作用的生物和环境因素确定的心理韧性在整个生命周期内动态变化的新概念,我们考查了由 3876 名具有和不具有 PTSD 诊断的美国退伍军人组成的 VA 中大西洋部署后心理健康资料库 (PDMH)。
方法:我们进行回归建模以研究心理韧性(使用康纳戴维森心理韧性量表;CD-RISC)、创伤后应激障碍 (PTSD) 严重程度(戴维森创伤量表;DTS)、社会支持(医疗结果研究社会支持调查; MOSSS)、战斗暴露 (战斗暴露量表; CES)、童年创伤 (创伤生活事件问卷;TLEQ) 和人口统计学因素。 CD-RISC与受教育年限呈正相关,与DTS、CES和TLEQ分数呈负相关。
结果:我们发现了 CD-RISC 和 CES 在预测 PTSD 严重程度(戴维森创伤量表)方面存在相互作用。具体而言,高心理韧性比低心理韧性预测的 PTSD 症状严重程度更低,这种关系随着战斗暴露水平增加而放大。结构方程模型 (SEM) 确定了一个代表心理韧性以及心理韧性、创伤和疾病的潜在变量之间关系的最佳潜在变量。我们推导出了一个由年龄、教育水平、MOSSS 和种族组成的心理韧性潜变量。
结论:我们的结果支持将心理韧性概念化为与 PTSD 共存的多因素决定因素,这是一种状态而非特质变量,并且可以通过生物学和行为指标进行量化。
1. Introduction
Trauma exposure is a significant risk factor for developing psychiatric disorders including posttraumatic stress disorder (PTSD), depression, anxiety, and sleep-related disorders (Baker et al., Citation2009). Between 2002 and 2015, 1,965,534 Veterans deployed as part of Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) were deemed eligible for VA healthcare services (Epidemiology Program P-DHG, Office of Patient Care Services, Veterans Health Administration, Department of Veterans Affairs). Rates of PTSD among Veterans exposed to combat vary from 10% to 25% (Fulton et al., Citation2015; Hoge, Auchterlonie, & Milliken, Citation2006). Combat Veterans also endorse a significantly higher rates of substance use, effective, and anxiety disorders than non-combat Veterans (Thomas, Harpaz-Rotem, Tsai, Southwick, & Pietrzak, Citation2017).
While rates of psychiatric disorders, particularly PTSD, are significantly higher in military and veteran populations than in civilians, 75–90% of individuals deployed do not develop a chronic psychiatric disorder (Hoge et al., Citation2004; Hoge et al., Citation2006). These prevalence rates underscore the importance of identifying risk and resilience factors associated with the trauma exposure. Historically, resilience has been regarded as the lack of psychopathology following exposure to chronic stress or trauma (Denckla et al., Citation2020; Masten & Barnes, Citation2018). More recent definitions emphasize maintaining a functional trajectory after trauma exposure (Denckla et al., Citation2020; Rakesh et al., Citation2019; Yehuda, Flory, Southwick, & Charney, Citation2006). Several risk and resilience factors influence the relationship between trauma and developing psychopathology including maladaptive coping behaviours such as substance use, poor social support, and vulnerable neurobiology (Allen, Crawford, & Kudler, Citation2016; Green, Calhoun, Dennis, & Beckham, Citation2010; Youssef et al. Citation2013a, Citation2013b).
Sociodemographic variables (age, sex and race/ethnicity), years of education, employment, income, occurrence of pre-traumatic and peri-traumatic events are associated with developing PTSD (Berger et al., Citation2012; Brewin, Andrews, & Valentine, Citation2000; Brunello et al., Citation2001; Ozer, Best, Lipsey, & Weiss, Citation2003; Schmidt et al., Citation2015; Wagner et al., Citation2020) and with resilience (Bonanno, Galea, Bucciarelli, & Vlahov, Citation2006; Bonanno, Galea, Bucciarelli, & Vlahov, Citation2007; Bonanno, Westphal, & Mancini, Citation2011; Portnoy et al., Citation2018). Systematic reviews found poor social support (Brewin et al., Citation2000) and peritraumatic dissociation (Ozer et al., Citation2003) to be the strongest predictors of PTSD. Although it is plausible that predictor variables are specific to the unique clinical presentation of PTSD that depend on trauma type (Brewin et al., Citation2000; Ozer et al., Citation2003), these clinical presentations or relationships have not been well characterized Yehuda and LeDoux (Citation2007). Epidemiological studies have found female sex, low social support, and young age to be more predictive of PTSD among civilians (Brunello et al., Citation2001), but these results have not been replicated in Veterans. Studies show mixed results of gender on PTSD among Veterans (Lapierre, Schwegler, & Labauve, Citation2007; Lehavot, Katon, Chen, Fortney, & Simpson, Citation2018; Maguen, Ren, Bosch, Marmar, & Seal, Citation2010). Race and ethnicity have shown mixed results as predictors of PTSD in civilians (Breslau et al., Citation2006; Himle, Baser, Taylor, Campbell, & Jackson, Citation2009) but showed robust associations in Veterans (Roberts, Gilman, Breslau, Breslau, & Koenen, Citation2011). Male sex and Asian ethnicity in residents of New York, New Jersey and Connecticut following September 2001, had positive associations with resilience and lower incidence of pre-traumatic and peri-traumatic events (Bonanno et al., Citation2006; Bonanno et al., Citation2007). Prior models of resilience have largely ignored factors that may contribute to favourable outcomes after trauma including other demographic factors like race (Herbert, Leung, Pittman, Floto, & Afari, Citation2018; Maschi, Shi, Forseth, Laureano, & Viola, Citation2017; Ore, Teufel-Shone, & Chico-Jarillo, Citation2016; Rao, Pell, & England-Kennedy, Citation2017; Teufel-Shone, Tippens, McCrary, Ehiri, & Sanderson, Citation2018), employment, social or unit support (Bonanno et al., Citation2011; Denckla et al., Citation2020; Pietrzak, Johnson, Goldstein, Malley, Rivers, et al., Citation2009; Pietrzak, Johnson, Goldstein, Malley, & Southwick, Citation2009), and lack of exposure to childhood trauma (Van Voorhees et al., Citation2012). Although the relationship between resilience and these factors has been examined previously in separate studies, prior regression models have not incorporated these predictor variables into a single model. However, Veterans showed no association between resilience and age, sex, number of deployments, or relationship/marital status (Herbert et al., Citation2018). Sex also did not explain resilience among Veterans after controlling for peritraumatic events (Portnoy et al., Citation2018).
Low Connor Davidson Resilience Scale (CD-RISC) scores in PTSD (Green et al., Citation2010) and high suicidal ideation/attempts among civilians and Veterans have been linked to low CD-RISC scores (Youssef et al., Citation2013a). In a subsample of the current MIRECC Repository (Brancu et al., Citation2017), 80% of Veterans with low CD-RISC and high combat exposure (25–41) on the Combat Exposure Scale (CES) had PTSD (Green et al., Citation2010); whereas only 20% of Veterans with high CD-RISC and high CES had PTSD (Green et al., Citation2010). Veterans with high CD-RISC scores had significantly lower depressive symptoms on the Beck Depression Inventory II (BDI-II) scores (Beck, Steer, & Brown, Citation1996) despite having high CES scores (Youssef et al. Citation2013b). Although this might lead to the inference that resilience and PTSD symptom severity are inversely correlated, variance in PTSD symptom severity has not been explained by quantitative resilience measures (Pietrzak, Johnson, Goldstein, Malley, Rivers, et al., Citation2009; Pietrzak, Johnson, Goldstein, Malley, & Southwick, Citation2009; Wolf et al., Citation2018; Daniels et al., Citation2012). The lack of psychometrically sound assessments of this multifactorial construct has posed a major limitation (Green et al., Citation2014; Windle, Bennett, & Noyes, Citation2011). Commonly used scales, such as the CD-RISC and the Deployment Risk and Resilience Inventory (DRRI-2) (Windle et al., Citation2011) model resilience with cognitive appraisal skills and flexibility to modify behaviour. Although CD-RISC has been used in multiple studies, it has been criticized for lacking a solid theoretical basis of resilience and lack of consistency (Green et al., Citation2010; Green et al., Citation2014; Windle et al., Citation2011). Hence, ten-item and two-item versions of the scale have been formulated using factor analyses (Green et al., Citation2014).
The focus of our study was to examine differential associations of socio-demographic and trauma variables with PTSD symptom severity vs. resilience. We used two methodologies to characterize these associations (Baker et al., Citation2009): 1) regression modelling and 2) structural equation modelling (SEM), which can discover latent variables of resilience. To narrow our focus, we searched previous studies that examined PTSD and resilience as two separate outcome variables in regression models. Two studies in Veterans applied similar paradigms (Youssef et al. Citation2013b; Green et al., Citation2010). Resilience, when defined as the lack of PTSD following trauma, was associated with predictor variables in civilians following 9/11 (Bonanno, Citation2004; Bonanno et al., Citation2006).
Our first aim was to characterize the relationship between PTSD severity and resilience as measured by the CD-RISC. We analyzed data from the PDMH, which is a well-organized data repository of Veterans (Brancu et al., Citation2017). Because prior research proposed that resilience is independent of PTSD (Yehuda et al., Citation2006), we tested regression models predicting PTSD severity and CD-RISC scores as dependent variables and childhood trauma, social support, combat exposure, and other demographic variables as independent variables. We hypothesized that despite being correlated (inversely), the independent variables would contribute differentially to PTSD symptom severity and CD-RISC scores. Finally, we hypothesized that resilience, as measured by the CD-RISC, would temper the relationship between combat exposure and PTSD symptom severity. Our second aim was to use SEM to discover latent variable(s) that measure resilience and examine how they relate to latent variables for trauma exposure and PTSD symptom severity. The second aim was implemented to support our long-term goal of modelling resilience as a latent construct derived from a broad array of biological markers such as neuroimaging, gene expression, epigenetics, autonomic arousal, EEG, eye tracking, and others (Rakesh et al., Citation2019). Although SEM can discover latent variables using manifest variables, quantifying the association between CD-RISC and PTSD severity scores and other variables is performed most effectively with regression modelling. Hence, we performed regression followed by SEM to inform us about possible combinations of manifest variables that are useful for modelling latent variables of trauma, resilience, and PTSD. Thus, we conceptualized resilience as a state variable that can be quantified across the lifespan rather than a trait variable (Rakesh et al., Citation2019).
2. Methods
2.1. Subjects
Subjects were recruited from 2005 through 2018 from the Mid-Atlantic PDMH Repository (Brancu et al., Citation2017). Inclusion and exclusion criteria for the PDMH repository have been reported previously (Brancu et al., Citation2017). Briefly, inclusion criterion required US military service (i.e. Veterans, active-duty personnel) after 9/11, and/or Reserve status (National Guard members and Reservists) on or after 11 September 2001. Exclusion criteria included primary language other than English, difficulty comprehending the informed consent form or process, and/or inability to travel to one of the participating four data-collection sites. Neither deployment nor health care treatment-seeking was required for study enrolment.
Subjects verbally confirmed their period of military service during an initial phone screening prior to participation and verified service status with a copy of their military service documentation at the in-person enrolment (Brancu et al., Citation2017). For the present analyses, we included 3876 subjects from the PDMH Repository. PTSD diagnosis was determined using the Structured Clinical Interview for DSM-IV-TR Axis I Disorders. The following variables from the Repository were examined: age, gender, race/ethnicity, CES score, CD-RISC score, DTS, MOSSS score, years of education, duration of employment in current job, history of inpatient and outpatient mental health treatment, highest rank while in military, and traumatic events in childhood/adulthood using the TLEQ. TLEQ subscales comprised the number of criterion-A events before deployment, during deployment, and after deployment.
2.2. Clinical assessments
2.2.1. CD-RISC
The CD-RISC, which contains 25 self-report items, was used in the PDMH repository given its superior reliability and validity when compared to other resilience scales (Windle et al., Citation2011). It is also predictive of PTSD occurrence and severity among civilians and military Veterans exposed to combat trauma (Green et al., Citation2014).
2.2.2. The Structured Clinical Interview for DSM-IV Axis I disorders (SCID-I)
The SCID (First, Gibbon, & Williams, Citation1994) was administered by trained mental health professionals to assess the current diagnosis of PTSD (Brancu et al., Citation2017).
2.2.3. PTSD symptom severity
PTSD symptom severity was assessed by self-report with the DTS questionnaire to rate frequency (0 = ‘not at all’ to 4 = ‘every day’) and severity (0 = ‘not at all distressing’ to 4 = ‘extremely distressing’) of 17 DSM-IV symptoms of PTSD. The DTS provided a frequency score ranging from 0 to 68, severity score ranging from 0 to 68, and a total score ranging from 0 to 136 (McDonald, Beckham, Morey, & Calhoun, Citation2009). The DTS is a reliable instrument and has demonstrated validity in OEF/OIF Veterans (McDonald et al., Citation2009).
2.2.4. Combat exposure
We administered the CES, which is a 7-item self-report questionnaire that quantifies wartime psychological trauma. Items were rated on a 5-point frequency (1 = ‘no’ or ‘never’ to 5 = ‘26 + times’ or ‘51 + times’), 5-point duration (1 = ‘never’ to 5 = ‘7 + months’), and a 45-point degree of loss (1 = ‘none’ to 45 = ‘76% or more’) scale. Respondents were asked to rate their exposure to various combat situations, such as firing rounds at the enemy and being on dangerous duty (Keane et al., Citation1989). The scale has been shown to be reliable and valid in OEF/OIF Veterans (Guyker et al., Citation2013).
2.2.5. Social support
The MOSSS was developed as part of the Medical Outcomes Study, was used to assess perceived social support (Sherbourne & Stewart, Citation1991). This instrument assessed several domains of social support including tangible support, emotional support, affective support, and positive support. The MOSSS consists of 19 items and has a Cronbach's alpha of 0.97 (Sherbourne & Stewart, Citation1991). It is a reliable and valid instrument to measure social support in Veterans (Brancu et al., Citation2014).
2.2.6. Trauma history
The TLEQ was used to assess the frequency and severity of traumatic experiences in childhood, adolescence, and adulthood. It contains 24 items that are subdivided into seven categories: accident/disaster, medical illness, adult physical violence, adult sexual assault, childhood physical violence, childhood sexual assault, war-zone exposure. Criterion-A events were reported for multiple categories prior to military service, during military service and after military service. Individual items and exposures were summed to calculate lifetime trauma exposure scores, the total number of events that caused fear, helplessness, and horror ranging from 0 to 23 (Clancy et al., Citation2006). The TLEQ has adequate reliability and validity in Veterans (Clancy et al., Citation2006).
2.2.7. Demographic information
The PDMH Repository included the following demographic variables: age, gender, race, years of education, months in the most recent employment, number of inpatient hospitalizations, number of outpatient treatment visits and highest rank attained in the military before discharge. Among these, gender, race, and rank after discharge were categorical variables. Gender was coded as male and female. For analyses, race was coded into six categories – Caucasian, African American, American Indian, Asian, Native Hawaiian or other Pacific Islander, and other race (). Military rank after discharge was coded into 22 categories ().
Table 1. Race codes for analyses.
Table 2. Military rank codes for analyses.
2.3. Analytic approach
We excluded 27 subjects from the PDMH sample of 3876 resulting in the present sample of 3849 subjects. Four Veterans were removed due to invalid CD-RISC scores (raw score = 0), and 23 Veterans were removed due to missing DTS scores. Study enrolment took place from 2005 (when the repository was initiated) until December 2018 (when we queried the repository). To prepare for linear regression modelling, we tested the collinearity of the predictor variables by performing correlations, t-tests and chi-squared analyses (). Correlation analyses were used to compare two continuous variables, t-tests were used to compare continuous variables across discrete groups, and Chi-squared tests were used to determine whether discrete variables were independent. To minimize inflation of variance, we calculated variance inflation factors (VIFs) for variables to be included in our regression models (Craney & Surles, Citation2002; Johnston, Jones, & Manley, Citation2018). Our cutoff for the VIF was 5 (Craney & Surles, Citation2002).
Table 3. Correlation matrix – MIRECC Post Deployment Mental Health (PDMH) dataset (n = 3849).
We constructed regression models first to quantify the relationship between variables and their effect sizes, followed by SEM to define latent variables for resilience, trauma and PTSD. Although linear regression models quantified associations between outcome variables (CD-RISC/DTS) and predictor variables, we performed SEM to discover latent variables of trauma, resilience and PTSD. We constructed separate regression models with DTS scores and CD-RISC scores as outcome measures because previous research suggests they are independent constructs (Bonanno, Citation2004; Bonanno et al., Citation2007). We subsequently performed SEM on 3849 subjects to calculate relationships between latent variables, which were derived from manifest variables. The main goal of SEM was to define a latent variable for resilience using measures from the PDMH repository. Akin to characterizing human intelligence using cognitive tests (Tarka, Citation2018), we modelled latent constructs for trauma, resilience and PTSD from manifest variables using structural equation modelling (SEM) (Cai, Citation2012; Tarka, Citation2018). We used the CES score and TLEQ Criterion-A events prior to military service, during military service and after military service to model the latent variable trauma. The latent variable illness was modelled on manifest variables such as DTS score, number of inpatient hospitalizations, and number of outpatient visits. For the latent variable resilience, we tested combinations of variables consisting of age, gender, race, years of education, military rank prior to discharge, and MOSSS until we attained an optimal latent variable fit by combining age, race, years of education and MOSSS. We used the latent variable analyses (LAVAAN) package in R and used weighted least squares (WLSM). This is a robust variant of the diagonally weighted least squares (DWLS) estimator. Path analyses model fit was deemed acceptable if the root mean square error of approximation (RMSEA) was ≤ 0.08 and the Tucker Lewis index (TLI) was ≥ 0.95 (Xia & Yang, Citation2019). We also applied SEM by replacing the latent variables with respective manifest scores to verify whether the latent variable approximated the manifest scores, which was our only means of testing SEM performance.
3. Results
3.1. Sample description
The average age of n = 3815 Veterans was 38 years (SD = 10 years, age was missing for 34 subjects). There were 2987 males and 862 females. Racial composition was 1837 Veterans who self-identified as Caucasian, 1799 as African American, and 201 comprising other racial categories (American Indian, Asian, Hispanic, Native Hawaiian or Pacific Islander). lists a comparison of demographic and clinical variables between PTSD and non-PTSD groups based on a DTS cut score of 32 (McDonald et al., Citation2009). We previously reported that a score of 32 on the DTS provided the most efficient tradeoff between false positive and false negative diagnostic classification (McDonald et al., Citation2009).
Table 4. Demographic and clinical characteristics (n = 3849).
3.2. Correlations and variance inflation factors (VIF)
lists correlation coefficients between all continuous variables, t-statistics between a continuous and a discrete variable, and chi-square statistics between discrete variables. Notably, the Pearson correlation between CD-RISC and MOSSS scores was 0.5, −0.6 between CD-RISC and DTS, −0.35 between MOSSS and DTS, 0.45 between DTS, and CES, −0.21 between CES and CD-RISC. CD-RISC and MOSSS were negatively correlated with all TLEQ scores.
We constructed regression models with DTS and CD-RISC as outcome measures. Predictor variables in these models included age, gender, race, MOSSS, CES, years of education, months of employment in last job, number of inpatient hospitalizations, number of outpatient visits, highest rank while in military, TLEQ number of criterion-A traumas prior to military service, TLEQ number of criterion-A traumas during military service and TLEQ number of criterion-A traumas following military service. All variables had VIF ≤ 5, which is deemed conservative (Craney & Surles, Citation2002; Johnston et al., Citation2018).
3.3. Summary of models
shows linear regression analyses examining CD-RISC scores as the dependent variable and independent variables being age, gender, race, CES scores, MOSSS scores, DTS scores, years of education, months of employment in most recent job, number of inpatient hospitalizations, number of outpatient visits, TLEQ number of criterion-A events prior to military service, TLEQ number of criterion-A traumas during military service and TLEQ number of criterion-A traumas after military service. CD-RISC showed significant positive association with MOSSS [t(2849) = 22.25, p < .0001], combat exposure [t(2849) = 3.90, p = .0001]. CD-RISC showed significant negative associations with DTS [t(2849) = −25.27, p < .0001] and number of inpatient hospitalizations [t(2849) = −1.98, p = .05]. Only MOSSS and DTS showed large effect sizes (Cohen’s d of 0.83 and 0.94 respectively), all other predictor variables showed small effect sizes (≤0.2).
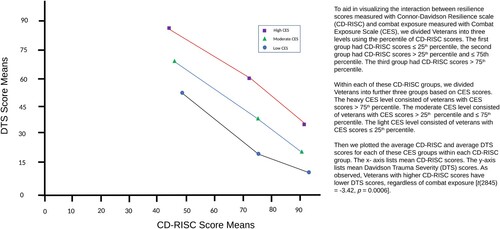
Table 5. CD-RISC associations with variables including PTSD severity.
shows the results of the linear regression with PTSD symptom severity using DTS scores as the outcome variable and predictor variables included age, gender, race, CD-RISC scores, CES scores, MOSSS scores, years of education, months of employment in most recent job, number of inpatient hospitalizations, number of outpatient visits, TLEQ number of criterion-A events prior to military service, TLEQ number of criterion-A events during military service and TLEQ number of criterion-A events after military service. DTS showed a significant positive association with combat exposure [t(2845) = 8.34, p < .0001], number of inpatient hospitalizations [t(2845) = 4.45, p ≤ .0001], number of outpatient visits [t(2845) = 12.14, p < .0001], and the number of TLEQ criterion-A events during military service [t(2845) = 3.39, p = .0008]. DTS showed a significant negative association with CD-RISC scores [t(2845) = −15.44, p < .0001]. There was a significant interaction effect between CD-RISC and CES [t(2845) = −3.42, p = .0006] in predicting DTS as seen in . Specifically, CES was positively correlated with DTS and the correlation was stronger for low CD-RISC scores and weaker for high CD-RISC scores. Only CD-RISC showed a medium effect size (Cohen’s d of 0.58) while all other predictor variables showed small effect sizes.
Table 6. DTS associations with variables including CD-RISC.
3.4. SEM results
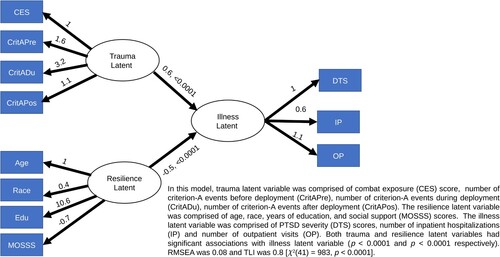
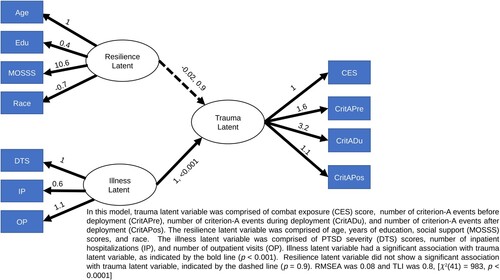
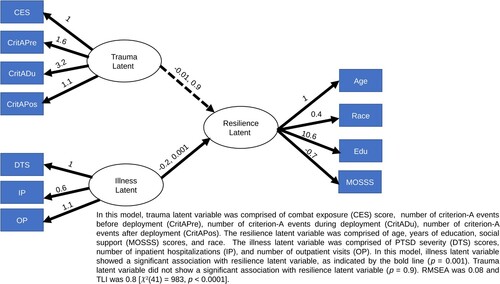
Factor analyses for these latent variables had an RMSEA of .08 and a TLI of 0.8. The confirmatory factor analyses for latent variables with optimal fit are listed in . The resilience latent variable had a positive association with social support (estimate = 10.6) and years of education (estimate = 0.4). Since race was a categorical variable, it would not be appropriate to interpret a linear relationship. The average CD-RISC score (±SD) was 71.4 (17.5) for Caucasian Veterans, 71.7 (Wagner et al., Citation2020) for African American Veterans, 72 (18.3) for Native-American Veterans, 69.7 (17.5) for Asian Veterans and 62.5 (20.6) for Pacific Islander Veterans.
Table 7. Structural equation modelling (SEM) latent variables.
3.5. Structural equation (SE) models
Four of the SE models we ran met our fit criteria. The other models are reported in the supplementary material. In SE Model 1 (), the illness latent variable was the outcome, while resilience and trauma latent variables were predictors. RMSEA was 0.08 and TLI was 0.8 (χ2 (41) = 983, p < .0001). Illness latent variable was negatively predicted by resilience latent variable (estimate = −0.5, p < .0001) and positively predicted by trauma (estimate = 0.6, p < .0001). SE Model 2(), examining trauma as an outcome measure, with resilience and illness as predictor variables had RMSEA of 0.08 and TLI of 0.8; (χ2 (41) = 983, p < .0001). The trauma latent variable was negatively predicted by the illness latent variable (estimate = 1, p < .0001). In SE Model 3 (), we examined resilience latent variable as an outcome variable with trauma and illness latent variables as predictors. RMSEA was 0.08 and TLI was 0.8 (χ22 (41) = 983, p < .0001). The resilience latent variable was negatively predicted by the illness latent variable (estimate = −0.2, p = .001).
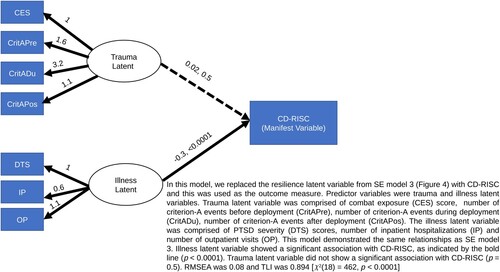
We also tested SE models by replacing each of the latent variables with the manifest scale score. For example, we tested SE Model 4 () in which the resilience latent variable was replaced with CD-RISC scores whilst preserving the trauma and illness latent variables. This model predicting CD-RISC scores with trauma and illness latent variables as predictors had an RMSEA of 0.08 and TLI of 0.894 (χ2 (18) = 462, p < .0001). CD-RISC scores were negatively predicted by the illness latent variable (estimate = −0.3, p < .0001) but not by the trauma latent variable (estimate = 0.02, p = .5). The other models are reported in the supplementary material.
4. Discussion
We studied the relationship of resilience to PTSD severity, trauma exposure, and other socio-demographic variables in a large cohort of 3849 Iraq and Afghanistan era Veterans. In regression analyses, resilience had a positive association with social support and combat exposure. With resilience as the outcome measure, social support had a large effect size, whereas the PTSD symptom severity outcome produced only a small effect size. In our regression models, both resilience and PTSD symptom severity had differential associations with other predictor variables such as age, gender, race, education, employment, CES score, number of inpatient hospitalizations, number of outpatient visits, and TLEQ Criterion-A scores. These differential associations provide support for resilience as a construct that coexists with PTSD, but also exists outside the context of trauma exposure and PTSD (Rakesh et al., Citation2019).
The association between PTSD symptom severity and combat exposure was modulated by resilience ( and ) such that CES was positively correlated with DTS and this correlation was stronger for low CD-RISC scores and weaker for high CD-RISC scores. This is consistent with previous literature showing resiliency moderates the relationship between childhood/combat trauma exposure and psychiatric disorders. Approximately 10–40% of individuals with PTSD report either childhood physical or childhood sexual abuse (Youssef et al. Citation2013b; Clancy et al., Citation2006; Dedert et al., Citation2009; Zaidi & Foy, Citation1994). This risk is moderated by resilience, such that individuals with high CD-RISC and childhood trauma are less likely to develop psychopathology than individuals with low CD-RISC and childhood trauma (Youssef et al. Citation2013b; Roy, Carli, & Sarchiapone, Citation2011).
Although we obtained optimum fit criteria with SE models that had an illness (), trauma () and resilience latent variables () as outcome measures, Model 1 () and Model 4 () deserve to be highlighted. In Model 1 (), illness is the outcome measure and is predicted significantly by both resilience and trauma. Model 1 comports with our conceptualization of resilience as a dynamic entity that changes through the lifespan, which is better captured as a latent construct. In this model, trauma is a latent variable encompassing combat exposure trauma (measured with combat exposure scale) experienced in early to mid-adulthood and childhood trauma (measured with the TLEQ) experienced in childhood, adolescence, during military service and after military service. By contrast, diagnostic assessment of PTSD (e.g. CAPS) is focused on a single criterion-A trauma, which is associated with the patient’s symptoms. Our model underscores that trauma is better conceptualized as a latent construct in so far as the cumulative effect of lifetime exposures influence PTSD severity as well as resilience. Thus, our model comports with a concept of resilience as a dynamic construct that changes over a lifetime that is not static. Model 1 also aligns with trauma and resilience interacting to produce PTSD (Rakesh et al., Citation2019). The SE model where resilience was swapped with CD-RISC score () showed approximately the same fit and relationship with other latent variables as SE Model 3 (). There is a lack of consensus on how to measure resilience and concerns about the validity of the CD-RISC (Green et al., Citation2014) and other instruments (Windle et al., Citation2011). It stands to reason that in the absence of a conceptually valid biological determinant of resilience, we can swap the resilience latent variable with the best currently available behavioural scale (CD-RISC). The ability to combine age, years of education, race, and MOSSS to obtain the information measured by the CD-RISC has value because these manifest variables are readily available in most studies whereas CD-RISC is less likely to be. This may be particularly valuable in analyzing data collected retrospectively that did not include the CD-RISC.
Previous studies have shown lower resilience (CD-RISC score) in traumatized individuals with PTSD (Green et al., Citation2010; Pietrzak, Johnson, Goldstein, Malley, Rivers, et al., Citation2009; Pietrzak et al., Citation2010). Previous studies have established that resilience protects against developing depressive symptoms, substance use disorders, medical illness, and suicidality, even after adjusting for PTSD (Youssef et al. Citation2013b; Green et al., Citation2010). Our results also show a positive correlation between combat exposure scale and PTSD severity, a positive correlation between social support and resilience, and a negative correlation between social support and PTSD severity. These are consistent with previous studies that have shown a protective effect of social support and resilience to PTSD symptom severity (Pietrzak, Johnson, Goldstein, Malley, Rivers, et al., Citation2009; Pietrzak, Johnson, Goldstein, Malley, & Southwick, Citation2009; Pietrzak et al., Citation2010). Although previous reports have shown a strong relationship between PTSD and social support when measured using the post-deployment social support scale (Pietrzak, Johnson, Goldstein, Malley, Rivers, et al., Citation2009) and using the MOSSS (Brancu et al., Citation2014), we were unable to replicate this. Perhaps because we used DTS instead of PTSD diagnosis (Brancu et al., Citation2014) or PCL-M (Pietrzak et al., Citation2010). A prior study by Green et al with a PDMH subsample, which comprised 13% (n = 497) of the present sample size, showed an interaction effect between resilience and combat exposure in Veterans with PTSD (Green et al., Citation2010) such that higher levels of resilience were particularly protective among individuals with high combat exposure. We were able to replicate this result in a larger size sample (n = 3849).
A few studies have examined a plausible surrogate measure of resilience called discrepancy-based psychiatric resilience (DBPR) (Amstadter, Maes, Sheerin, Myers, & Kendler, Citation2016; Sheerin, Lind, et al., Citation2018; Sheerin et al., Citation2019; Sheerin, Stratton, et al., Citation2018). DBPR is obtained by linearly regressing global severity index scores (GSI) T-scores from the Symptom Checklist-90 Item-Revised (SCL-90) (the outcome measure) onto the number of traumatic event types endorsed from the TLEQ (predictor) (Sheerin et al., Citation2019). Akin to DBPR, our analyses with a latent construct represent a fledgling approach to quantifying a resilience factor that we term the r-factor. The proposed r-factor captures a biological multi-omic risk score (MORS) derived from genetic, serum, brain imaging, epigenetic, psychophysiological, gut microbiome, and other markers (Feder, Nestler, & Charney, Citation2009; Rakesh et al., Citation2019; Russo, Murrough, Han, Charney, & Nestler, Citation2012). In our analyses, we used demographic variables and behavioural scales to mimic this approach, but we expect longitudinal studies will be able to model a latent construct of resilience using biological markers. Modelling a diverse array of environmental exposures such as prenatal stress, childhood trauma, adult trauma, stressful life events, social support, psychosocial deprivation, neglect, social stress, air pollution, water pollution, lead exposure, poverty, and many other sociodemographic parameters will contribute to a robust construction of a resilience (Rakesh et al., Citation2019). Current measures of resilience are compared to CD-RISC simply because we lack robust biological markers for resilience.
Furthermore, each of these biological parameters may interact with various environmental inputs to influence resilience. Biological and environmental exposure parameters could be differentially weighted depending on the relative contribution of each parameter to resilience. Our idea is akin to a polygenic risk score (PRS), which is simply the weighted sum of individual genetic markers that contribute to the risk of developing a given condition. An objective score such as MORS could quantify the risk of developing PTSD following trauma exposure and serve as a mediator to assess treatment response (Juster et al., Citation2011; Rakesh et al., Citation2019).
4.1. Limitations
An important limitation of the present study is our reliance on self-reported measures, and a single instrument to measure resilience. While we were able to assess several demographic variables in relation to PTSD and resilience, it will be important for future research to examine biological and genetic contributors that impact resilience. In addition, a quantified way to measure resilience as a multifactorial determinant requires that these factors supplement our clinical scales and demographic variables (Rakesh et al., Citation2019). Our findings apply to Veterans and may not generalize to civilians due to differences in stressors and overall resilience (Haley, Citation1998; Kang & Bullman, Citation1998; Smith et al., Citation2008). Thus, our results require replication in civilian datasets (Rakesh et al., Citation2019). Finally, the cross-sectional study design we employed is unable to make causal inferences, which could be remedied by a longitudinal design.
5. Conclusion
We found differential contributions of demographic variables, social support, and trauma variables to outcome variables such as DTS and CD-RISC. In addition, SEM was used to identify a latent construct of resilience based on education level, social support, race, military rank at discharge, and age. The use of latent constructs of resilience moves the field one small step closer to constructing resilience as a state rather than a trait variable, as was implemented by CD-RISC. Thus, we used SEM to derive latent constructs from manifest scores. Our results support a conceptualization of resilience as a multifactorial determinant that coexists with PTSD, a state rather than a trait variable, and can be quantified with biological and behavioural metrics.
Supplemental Material
Download MS Word (2.9 MB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Funding
Supported by the VA Mid-Atlantic Mental Illness Research, Education and Clinical Center (MIRECC) [Center Director, PI of PDMH study, John Fairbank] of the Department of Veterans Affairs, United States Office of Mental Health and Suicide Prevention and the VA Mid-Atlantic Healthcare Network (VISN 6). John Fairbank is also supported by Substance Abuse and Mental Health Services Administration (SAMHSA) and the Office of Refugee Resettlement/ Administration for Children and Families (ORR/ACF). Dr. Morey is funded by the Department of Veterans Affairs under grant number I01CX002293, National Institute of Mental Health (NIMH) under grant numbers R01MH111671 and R01MH129832.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Data availability statement
The data that support the findings of this study may be available on request from the corresponding author. Additional approvals may be required. The data are not publicly available due to privacy or ethical restrictions.
References
- Allen, J. P., Crawford, E. F., & Kudler, H. (2016). Nature and treatment of comorbid alcohol problems and post traumatic stress disorder among American military personnel and Veterans. Alcohol Research, 38(1), 133–140.
- Amstadter, A. B., Maes, H. H., Sheerin, C. M., Myers, J. M., & Kendler, K. S. (2016). The relationship between genetic and environmental influences on resilience and on common internalizing and externalizing psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology, 51(5), 669–678.
- Baker, D. G., Heppner, P., Afari, N., Nunnink, S., Kilmer, M., Simmons, A., … Bosse, B. (2009). Trauma exposure, branch of service, and physical injury in relation to mental health among U.S. Veterans returning from Iraq and Afghanistan. Military Medicine, 174(8), 773–778.
- Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation.
- Berger, W., Coutinho, E. S., Figueira, I., Marques-Portella, C., Luz, M. P., Neylan, T. C., ... Mendlowicz, M. V. (2012). Rescuers at risk: A systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Social Psychiatry and Psychiatric Epidemiology, 47(6), 1001–1011. doi:10.1007/s00127-011-0408-2
- Bonanno, G. A. (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? The American Psychologist, 59(1), 20–28.
- Bonanno, G. A., Galea, S., Bucciarelli, A., & Vlahov, D. (2006). Psychological resilience after disaster: New York city in the aftermath of the September 11th terrorist attack. Psychological Science, 17(3), 181–186.
- Bonanno, G. A., Galea, S., Bucciarelli, A., & Vlahov, D. (2007). What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology, 75(5), 671–682.
- Bonanno, G. A., Westphal, M., & Mancini, A. D. (2011). Resilience to loss and potential trauma. Annual Review of Clinical Psychology, 7, 511–535.
- Brancu, M., Thompson, N. L., Beckham, J. C., Green, K. T., Calhoun, P. S., Elbogen, E. B., … Wagner, H. R. (2014). The impact of social support on psychological distress for U. S. Afghanistan/Iraq era veterans with PTSD and Other Psychiatric Diagnoses. Psychiatry Res, 217(1-2), 86–92. doi:10.1016/j.psychres.2014.02.025
- Brancu, M., Wagner, H. R., Morey, R. A., Beckham, J. C., Calhoun, P. S., Tupler, L. A., … Fairbank, J. A. (2017). The Post-Deployment Mental Health (PDMH) study and repository: A multi-site study of US Afghanistan and Iraq era veterans. International Journal of Methods in Psychiatric Research, 26(3). doi:10.1002/mpr.1570
- Breslau, J., Aguilar-Gaxiola, S., Kendler, K. S., Su, M., Williams, D., & Kessler, R. C. (2006). Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychological Medicine, 36(1), 57–68.
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766.
- Brunello, N., Davidson, J. R., Deahl, M., Kessler, R. C., Mendlewicz, J., Racagni, G., … Zohar, J. (2001). Posttraumatic stress disorder: Diagnosis and epidemiology, comorbidity and social consequences, biology and treatment. Neuropsychobiology, 43(3), 150–162. doi:10.1159/000054884
- Cai, L. (2012). Latent variable modeling. Shanghai Archives of Psychiatry, 24(2), 118–120.
- Clancy, C. P., Graybeal, A., Tompson, W. P., Badgett, K. S., Feldman, M. E., Calhoun, P. S., … Beckham, J. C. (2006). Lifetime trauma exposure in veterans with military-related posttraumatic stress disorder: Association with current symptomatology. Journal of Clinical Psychiatry, 67(9), 1346–1353. doi:10.4088/jcp.v67n0904
- Craney, T. A., & Surles, J. G. (2002). Model-dependent variance inflation factor cutoff values. Quality Engineering, 14(3), 391–403.
- Daniels, J. K., Hegadoren, K. M., Coupland, N. J., Rowe, B. H., Densmore, M., Neufeld, R. W., & Lanius, R. A. (2012). Neural correlates and predictive power of trait resilience in an acutely traumatized sample: A pilot investigation. Journal of Clinical Psychiatry, 73(3), 327–332. doi:10.4088/JCP.10m06293
- Dedert, E. A., Green, K. T., Calhoun, P. S., Yoash-Gantz, R., Taber, K. H., Mumford, M. M., … Beckham, J. C. (2009). Association of trauma exposure with psychiatric morbidity in military veterans who have served since September 11, 2001. Journal of Psychiatric Research, 43(9), 830–836.
- Denckla, C. A., Cicchetti, D., Kubzansky, L. D., Seedat, S., Teicher, M. H., Williams, D. R., & Koenen, K. C. (2020). Psychological resilience: An update on definitions, a critical appraisal, and research recommendations. European Journal of Psychotraumatology, 11(1), Article 1822064. doi:10.1080/20008198.2020.1822064
- Epidemiology Program P-DHG, Office of Patient Care Services, Veterans Health Administration, Department of Veterans Affairs. Analysis of VA Health Care Utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) Veterans January 2017 [Available from: https://www.publichealth.va.gov/docs/epidemiology/healthcare-utilization-report-fy2015-qtr3.pdf#.
- Feder, A., Nestler, E. J., & Charney, D. S. (2009). Psychobiology and molecular genetics of resilience. Nature Reviews Neuroscience, 10(6), 446–457.
- First, M. B., Gibbon, M., & Williams, J. B. W. (1994). Structured Clinical Interview for Axis I DSM-IV Disorders. Version 20. New York, NY: Biometrics Research Department.
- Fulton, J. J., Calhoun, P. S., Wagner, H. R., Schry, A. R., Hair, L. P., Feeling, N., … Beckham, J. C. (2015). The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans: A meta-analysis. Journal of Anxiety Disorders, 31, 98–107. doi:10.1016/j.janxdis.2015.02.003
- Green, K. T., Calhoun, P. S., Dennis, M. F., Mid-Atlantic Mental Illness Research E, Clinical Center W, & Beckham, J. C. (2010). Exploration of the resilience construct in posttraumatic stress disorder severity and functional correlates in military combat veterans who have served since September 11, 2001. Journal of Clinical Psychiatry, 71(7), 823–830.
- Green, K. T., Hayward, L. C., Williams, A. M., Dennis, P. A., Bryan, B. C., Taber, K. H., … Calhoun, P. S. (2014). Examining the factor structure of the Connor–Davidson Resilience Scale (CD-RISC) in a post-9/11 U.S. Military veteran sample. Assessment, 21(4), 443–451. doi:10.1177/1073191114524014
- Guyker, W. M., Donnelly, K., Donnelly, J. P., Dunnam, M., Warner, G. C., Kittleson, J., … Meier, S. T. (2013). Dimensionality, reliability, and validity of the combat experiences scale. Military Medicine, 178(4), 377–384. doi:10.7205/MILMED-D-12-00223
- Haley, R. W. (1998). Point: Bias from the “healthy-warrior effect” and unequal follow-up in three government studies of health effects of the Gulf War. American Journal of Epidemiology, 148(4), 315–323.
- Herbert, M. S., Leung, D. W., Pittman, J. O. E., Floto, E., & Afari, N. (2018). Race/ethnicity, psychological resilience, and social support among OEF/OIF combat veterans. Psychiatry Research, 265, 265–270.
- Himle, J. A., Baser, R. E., Taylor, R. J., Campbell, R. D., & Jackson, J. S. (2009). Anxiety disorders among African Americans, blacks of Caribbean descent, and non-Hispanic whites in the United States. Journal of Anxiety Disorders, 23(5), 578–590.
- Hoge, C. W., Auchterlonie, J. L., & Milliken, C. S. (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA, 295(9), 1023–1032.
- Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351(1), 13–22.
- Johnston, R., Jones, K., & Manley, D. (2018). Confounding and collinearity in regression analysis: A cautionary tale and an alternative procedure, illustrated by studies of British voting behaviour. Quality & Quantity, 52(4), 1957–1976.
- Juster, R. P., Bizik, G., Picard, M., Arsenault-Lapierre, G., Sindi, S., Trepanier, L., … Lupien, S. J. (2011). A transdisciplinary perspective of chronic stress in relation to psychopathology throughout life span development. Development and Psychopathology, 23(3), 725–776. doi:10.1017/S0954579411000289
- Kang, H. K., & Bullman, T. (1998). Counterpoint: Negligible “healthy-warrior effect” on Gulf War Veterans’ mortality. American Journal of Epidemiology, 148(4), 324–325. discussion 34-8.
- Keane, T., Fairbank, J., Caddell, J., Zimering, R. T., Taylor, K. L., & Mora, C. A. (1989). Clinical evaluation of a measure to assess combat exposure. Psychological Assessment, 1(1), 53–55.
- Lapierre, C. B., Schwegler, A. F., & Labauve, B. J. (2007). Posttraumatic stress and depression symptoms in soldiers returning from combat operations in Iraq and Afghanistan. Journal of Traumatic Stress, 20(6), 933–943.
- Lehavot, K., Katon, J. G., Chen, J. A., Fortney, J. C., & Simpson, T. L. (2018). Post-traumatic stress disorder by gender and veteran status. American Journal of Preventive Medicine, 54(1), e1–e9.
- Maguen, S., Ren, L., Bosch, J. O., Marmar, C. R., & Seal, K. H. (2010). Gender differences in mental health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care. American Journal of Public Health, 100(12), 2450–2456.
- Maschi, T., Shi, Q., Forseth, K., Laureano, P., & Viola, D. (2017). Exploring the association between race and health among older adults who are incarcerated. Social Work in Public Health, 32(3), 143–153.
- Masten, A. S., & Barnes, A. J. (2018). Resilience in children: Developmental perspectives. Children (Basel), 5(7), 98.
- McDonald, S. D., Beckham, J. C., Morey, R. A., & Calhoun, P. S. (2009). The validity and diagnostic efficiency of the Davidson Trauma Scale in military veterans who have served since September 11th, 2001. Journal of Anxiety Disorders, 23(2), 247–255.
- Ore, C. E., Teufel-Shone, N. I., & Chico-Jarillo, T. M. (2016). American Indian and Alaska Native resilience along the life course and across generations: A literature review. American Indian and Alaska Native Mental Health Research (Online), 23(3), 134–157.
- Ozer, E. J., Best, S. R., Lipsey, T. L., & Weiss, D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129(1), 52–73.
- Pietrzak, R. H., Johnson, D. C., Goldstein, M. B., Malley, J. C., Rivers, A. J., Morgan, C. A., & Southwick, S. M. (2009). Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom: The role of resilience, unit support, and postdeployment social support. Journal of Special Operations Medicine, 9(3), 74–78. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19739480
- Pietrzak, R. H., Johnson, D. C., Goldstein, M. B., Malley, J. C., Rivers, A. J., Morgan, C. A., & Southwick, S. M. (2010). Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom: The role of resilience, unit support, and post deployment social support. Journal of Affective Disorders, 120(1-3), 188–192. doi:10.1016/j.jad.2009.04.015
- Pietrzak, R. H., Johnson, D. C., Goldstein, M. B., Malley, J. C., & Southwick, S. M. (2009). Psychological resilience and postdeployment social support project against traumatic stress and depressive symptoms in soldiers returning from Operations Enduring Freedom and Iraqi Freedom. Journal of Special Operations Medicine, 9(3), 67–73. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19739479
- Portnoy, G. A., Relyea, M. R., Decker, S., Shamaskin-Garroway, A., Driscoll, M., Brandt, C. A., & Haskell, S. G. (2018). Understanding gender differences in resilience among Veterans: Trauma history and social ecology. Journal of Traumatic Stress, 31(6), 845–855. doi:10.1002/jts.22341
- Rakesh, G., Morey, R. A., Zannas, A. S., Malik, Z., Marx, C. E., Clausen, A. N., … Szabo, S. T. (2019). Resilience as a translational endpoint in the treatment of PTSD. Molecular Psychiatry, 24(9), 1268–1283.
- Rao, S., Pell, D., & England-Kennedy, E. S. (2017). Suicide, resilience, and connectedness across the lifespan: Lessons from American Indian and Alaska native elders. Family & Community Health, 40(4), 347–356.
- Roberts, A. L., Gilman, S. E., Breslau, J., Breslau, N., & Koenen, K. C. (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine, 41(1), 71–83.
- Roy, A., Carli, V., & Sarchiapone, M. (2011). Resilience mitigates the suicide risk associated with childhood trauma. Journal of Affective Disorders, 133(3), 591–594.
- Russo, S. J., Murrough, J. W., Han, M. H., Charney, D. S., & Nestler, E. J. (2012). Neurobiology of resilience. Nature Neuroscience, 15(11), 1475–1484.
- Schmidt, U., Willmund, G. D., Holsboer, F., Wotjak, C. T., Gallinat, J., Kowalski, J. T., & Zimmermann, P. (2015). Searching for non-genetic molecular and imaging PTSD risk and resilience markers: Systematic review of literature and design of the German armed forces PTSD biomarker study. Psychoneuroendocrinology, 51, 444–458.
- Sheerin, C. M., Amstadter, A. B., Kurtz, E. D., Bountress, K. E., Stratton, K. J., McDonald, S. D., & Mid-Atlantic VA MIRECC Workgroup. (2019). The association of resilience on psychiatric, substance use, and physical health outcomes in combat trauma-exposed military service members and veterans. European Journal of Psychotraumatology, 10(1), Article 1625700.
- Sheerin, C. M., Lind, M. J., Brown, E. A., Gardner, C. O., Kendler, K. S., & Amstadter, A. B. (2018). The impact of resilience and subsequent stressful life events on MDD and GAD. Depression and Anxiety, 35(2), 140–147. doi:10.1002/da.22700
- Sheerin, C. M., Stratton, K. J., Amstadter, A. B., Education Clinical Center Mirecc Workgroup T, & McDonald, S. D. (2018). Exploring resilience models in a sample of combat-exposed military service members and veterans: A comparison and commentary. European Journal of Psychotraumatology, 9(1), Article 1486121. doi:10.1002/da.22700
- Sherbourne, C. D., & Stewart, A. L. (1991). The MOS social support survey. Social Science & Medicine (1982), 32(6), 705–714.
- Smith, T. C., Ryan, M. A., Smith, B., Gackstetter, G. D., Wells, T. S., Amoroso, P. J., … Millennium Cohort Study, T. (2008). Re: “Psychiatric diagnoses in historic and contemporary military cohorts: Combat deployment and the healthy warrior effect”. American Journal of Epidemiology, 168(9), 1094–1095.
- Tarka, P. (2018). An overview of structural equation modeling: Its beginnings, historical development, usefulness and controversies in the social sciences. Quality & Quantity, 52(1), 313–354.
- Teufel-Shone, N. I., Tippens, J. A., McCrary, H. C., Ehiri, J. E., & Sanderson, P. R. (2018). Resilience in American Indian and Alaska Native Public Health: An underexplored framework. American Journal of Health Promotion: AJHP, 32(2), 274–281.
- Thomas, M. M., Harpaz-Rotem, I., Tsai, J., Southwick, S. M., & Pietrzak, R. H. (2017). Mental and physical Health conditions in US combat Veterans: Results from the National Health and resilience in Veterans study. The Primary Care Companion for Cns Disorders, 19(3).
- Van Voorhees, E. E., Dedert, E. A., Calhoun, P. S., Brancu, M., Runnals, J., Beckham, J. C., & VA-Mid-Atlantic MIRECC. (2012). Childhood trauma exposure in Iraq and Afghanistan war era veterans: Implications for posttraumatic stress disorder symptoms and adult functional social support. Child Abuse & Neglect, 36(5), 423–432. doi:10.1016/j.chiabu.2012.03.004
- Wagner, S. L., White, N., Fyfe, T., Matthews, L. R., Randall, C., Regehr, C., … Fleischmann, M. H. (2020). Systematic review of posttraumatic stress disorder in police officers following routine work-related critical incident exposure. American Journal of Industrial Medicine, 63(7), 600–615. doi:10.1002/ajim.23120
- Windle, G., Bennett, K. M., & Noyes, J. (2011). A methodological review of resilience measurement scales. Health and Quality of Life Outcomes, 9(8), 8.
- Wolf, E. J., Miller, M. W., Sullivan, D. R., Amstadter, A. B., Mitchell, K. S., Goldberg, J., & Magruder, K. M. (2018). A classical twin study of PTSD symptoms and resilience: Evidence for a single spectrum of vulnerability to traumatic stress. Depression and Anxiety, 35(2), 132–139. doi:10.1002/da.22712
- Xia, Y., & Yang, Y. (2019). RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: The story they tell depends on the estimation methods. Behavior Research Methods, 51(1), 409–428.
- Yehuda, R., Flory, J. D., Southwick, S., & Charney, D. S. (2006). Developing an agenda for translational studies of resilience and vulnerability following trauma exposure. Annals of the New York Academy of Sciences, 1071, 379–396.
- Yehuda, R., & LeDoux, J. (2007). Response variation following trauma: A translational neuroscience approach to understanding PTSD. Neuron, 56(1), 19–32.
- Youssef, N. A., Green, K. T., Beckham, J. C., & Elbogen, E. B. (2013a). A 3-year longitudinal study examining the effect of resilience on suicidality in veterans. Annals of Clinical Psychiatry, 25(1), 59–66.
- Youssef, N. A., Green, K. T., Dedert, E. A., Hertzberg, J. S., Calhoun, P. S., Dennis, M. F., … Beckham, J. C. (2013b). Exploration of the influence of childhood trauma, combat exposure, and the resilience construct on depression and suicidal ideation among U.S. Iraq/Afghanistan era military personnel and veterans. Archives of Suicide Research, 17(2), 106–122.
- Zaidi, L. Y., & Foy, D. W. (1994). Childhood abuse experiences and combat-related PTSD. Journal of Traumatic Stress, 7(1), 33–42.