ABSTRACT
Background:
Understanding the course of post-traumatic stress disorder (PTSD) and the factors that impact this is essential to inform decisions about when and for whom screening and intervention are likely to be beneficial.
Objective:
To provide meta-analytic evidence of the course of recovery from PTSD in the first year following trauma, and the factors that influence that recovery.
Method:
We conducted a meta-analysis of observational studies of adult PTSD prevalence which included at least two assessments within the first 12 months following trauma exposure, examining prevalence statistics through to 2 years post-trauma. We examined trauma intentionality (intentional or non-intentional), PTSD assessment method (clinician or self-report), sample sex distribution, and age as moderators of PTSD prevalence over time.
Results:
We identified 78 eligible studies including 16,484 participants. Pooled prevalence statistics indicated that over a quarter of individuals presented with PTSD at 1 month post-trauma, with this proportion reducing by a third between 1 and 3 months. Beyond 3 months, any prevalence changes were detected over longer intervals and were small in magnitude. Intentional trauma, younger age, and female sex were associated with higher PTSD prevalence at 1 month. In addition, higher proportions of females, intentional trauma exposure, and higher baseline PTSD prevalence were each associated with larger reductions in prevalence over time.
Conclusions:
Recovery from PTSD following acute trauma exposure primarily occurs in the first 3 months post-trauma. Screening measures and intervention approaches offered at 3 months may better target persistent symptoms than those conducted prior to this point.
HIGHLIGHTS
PTSD rates in the immediate aftermath of trauma exposure decline from 27% at 1 month to 18% at 3 months post-trauma, showing significant spontaneous recovery.
Problems appear to stabilize after 3 months.
Screening/intervention for PTSD at 3 months post-trauma is indicated.
Antecedentes:
La comprensión del curso del trastorno de Estrés Postraumático (TEPT) y los factores que lo impactan son esenciales para la toma de decisiones informadas acerca de cuándo y para quién es probable que la detección e intervención sean beneficiosas.
Objetivo:
Proporcionar evidencia meta-analítica del curso de la recuperación del TEPT en el primer año después de un trauma y los factores que influyen en esa recuperación.
Método:
Condujimos un metaanálisis de estudios observacionales de la prevalencia de TEPT en adultos que incluyeron al menos dos evaluaciones dentro de los primeros doce meses después de la exposición a un trauma, examinando las estadísticas de prevalencia hasta los 2 años posteriores al trauma. Examinamos la intencionalidad del trauma (intencional o no), métodos de evaluación del TEPT (clínicos o auto-reporte), distribución por sexo de la muestra y edad como moderadores de prevalencia de TEPT a lo largo del tiempo.
Resultados:
Identificamos 18 estudios elegibles con 16.484 participantes. Las estadísticas de prevalencia agrupadas indicaron que más de una cuarta parte de los individuos presentaron TEPT un mes después de un trauma, y esta proporción se redujo a un tercio entre 1 y 3 meses. Más allá de los 3 meses, los cambios de prevalencia se detectaron en intervalos más largos y fueron de magnitud pequeña. El trauma intencional, ser más joven y sexo femenino se asociaron con una mayor prevalencia de TEPT al mes. Además, las proporciones más altas de mujeres, la exposición a trauma intencional y la prevalencia inicial más alta de TEPT se asociaron con mayores reducciones en la prevalencia en el tiempo.
Conclusiones:
La recuperación del TEPT después de la exposición a un trauma agudo ocurre principalmente en los primeros 3 meses posteriores al trauma. Las medidas de detección y enfoques terapéuticos ofrecidos a los tres meses pueden abordar mejor los síntomas persistentes que los realizados antes de este momento.
背景:
了解创伤后应激障碍 (PTSD) 病程以及影响对于决定何时以及对谁进行筛查和干预的重要因素可能是有益的。
目的:
提供关于创伤后第一年 PTSD 恢复过程以及影响恢复因素的元分析证据。
方法:
我们对成人 PTSD 患病率的观察性研究进行了元分析,包括在创伤暴露后的前 12 个月内至少进行两次评估考查创伤后 2 年患病率的统计数据。我们考查了创伤意向性(故意或非故意)、PTSD 评估方法(临床医生或自我报告)、样本性别分布和年龄作为 PTSD 患病率随时间变化的调节因素。
结果:
我们确定了 78 项符合条件的研究,包括 16,484 名参与者。汇总患病率统计数据表明,超过四分之一的个体在创伤后 1 个月出现 PTSD,这一比例在 1 到 3 个月之间减少了三分之一。检测到超过 3 个月更长的时间间隔内的一些流行率变化且幅度很小。故意创伤、年龄较小和女性与 1 个月时较高的 PTSD 患病率有关。此外,较高比例的女性、故意创伤暴露和较高的基线 PTSD 患病率均与随时间推移患病率的大幅下降相关。
结论:
急性创伤暴露后 PTSD 的恢复主要发生在创伤后的前 3 个月。在 3 个月时提供的筛查措施和干预方法可能比在此前进行的那些更能针对持续性症状。
1. Introduction
The majority of adults will be exposed to one or more traumatic events during their lifetime and a significant minority will develop post-traumatic stress disorder (PTSD) or other mental health problems as a consequence (Breslau, Citation2009), causing marked impairments in overall quality of life (Olatunji, Cisler, & Tolin, Citation2007). PTSD can take a chronic course, lasting many years if left untreated. However, there is also a degree of natural recovery over time, with many more individuals experiencing PTSD symptoms in the acute aftermath of trauma than will develop chronic disorder. For example, one systematic review concluded that half of individuals diagnosed with PTSD achieve remission without treatment within 3 years (Morina, Wicherts, Lobbrecht, & Priebe, Citation2015). Understanding the time course of such recovery is critical to informing decisions around screening and intervention. Research has indicated that intervening too early following trauma has the potential to disrupt coping (Rose, Bisson, Churchill, & Wessely, Citation2004), and knowing the point at which remission becomes relatively unlikely can also support targeted treatment of likely chronic presentations.
In children, a meta-analysis investigating PTSD prevalence and symptom severity in the first 12 months post-trauma concluded that there was a period of spontaneous recovery in the initial 3–6 months post-trauma, with only small improvements seen after this point (Hiller et al., Citation2017). These findings are similar to results from a multi-study sample of 7–18-year-olds, in which a natural 25% decline in child PTSD symptoms was observed at 3 months, with little improvement thereafter (Hiscox et al., Citation2022). In the adult literature, a systematic review of longitudinal studies between 1998 and 2010 found the median prevalence of PTSD in adults exposed to trauma to be 28.8% at 1 month, declining to 17% at 12 months, with most evidence of changes in median prevalence within the first 6 months (Santiago et al., Citation2013). Conclusions based on comparing median prevalence across studies over time are limited, as prevalence estimates at different time-points will be based on different pools of studies, and a lack of appropriate pooling of data may also result in erroneous conclusions. Meta-analysis of the adult longitudinal evidence base is essential to confirm whether the course of PTSD recovery is the same as or different from that observed in children, and at what point remission becomes unlikely without treatment.
Relatedly, while there is evidence about factors that make one more or less likely to develop PTSD following a traumatic event (Brewin, Andrews, & Valentine, Citation2000), there is less evidence about the factors that predict the likely chronicity of PTSD once diagnosed. One widely replicated finding is that exposure to intentional traumas (e.g. physical or sexual assault, combat) versus non-intentional traumas (e.g. accidents, natural disasters) is associated with a higher likelihood of developing PTSD, as well as with more severe symptoms (Birkeland, Skar, & Jensen, Citation2021). For example, a review of the World Health Organization World Mental Health survey data collected from 24 countries (n = 68,894) found that exposure to intentional traumas was typically associated with higher conditional risk for PTSD than exposure to non-intentional traumas (e.g. 11.4% PTSD following intimate partner or sexual violence versus 2.0% following accidental injury) (Kessler et al., Citation2017). Several theories have been proposed to explain the higher prevalence of PTSD following intentional trauma, including higher levels of distress during the trauma (Ozer, Best, Lipsey, & Weiss, Citation2003), increased negative beliefs (Christiansen & Hansen, Citation2015), and loss of social support (Jiang, Webster, Robinson, Kassam-Adams, & Richmond, Citation2018). There is also evidence that the type of exposure can lead to different symptom manifestations (Birkeland et al., Citation2021) and influence the course of PTSD, with some studies reporting that intentional trauma is associated with poorer recovery (Hiscox et al., Citation2022; Santiago et al., Citation2013).
Females also have at least a two-fold higher risk of developing PTSD following a traumatic event than males – the lifetime prevalence of PTSD is approximately 10% in women and 5% in men (Olff, Citation2017). The mechanisms underlying this higher risk in females are unclear, but may include the gender roles and expectations (Christiansen & Berke, Citation2020), sex differences in cognitive–behavioural responses (Christiansen & Hansen, Citation2015), emotional memory consolidation (Hsu et al., Citation2018), and biological factors related to the stress response, which may bias females and males towards different psychopathology (Bangasser, Eck, & Ordoñes Sanchez, Citation2019; Takai et al., Citation2007). Despite consistent evidence of a higher prevalence of PTSD in females versus males, there is less certainty on whether there are sex differences in the course of PTSD over time. Some studies have found that females are more likely than males to develop chronic PTSD (Breslau & Davis, Citation1992; Pietrzak, Van Ness, Fried, Galea, & Norris, Citation2013), as well as having higher comorbid rates of depression and anxiety disorders and an increased risk for other chronic diseases and mortality (Roberts et al., Citation2020). However, other studies have found that sex is not an important factor for predicting long-term PTSD course (e.g. Morina et al., Citation2014; Yin, Wu, Yu, & Liu, Citation2019).
The age at which one is exposed to a trauma may also be important in predicting the course of PTSD. As we age, there are factors that could make it more difficult to deal with a traumatic event, such as changes in role (e.g. retirement; Lipton et al., Citation1986), decreases in social support, and cognitive impairment (Aldwin, Sutton, Chiara, & Spiro, Citation1996; Burri, Maercker, Krammer, & Simmen-Janevska, Citation2013). On the other hand, increased age can bring resilience and increased coping strategies (Moos, Brennan, Schutte, & Moos, Citation2006). However, in those who experience their index trauma during adulthood, it is unclear whether and how the age at which they experienced that event impacts on the course of PTSD. Some studies have found age to be a predictor of a more chronic course (e.g. Galatzer-Levy et al., Citation2013; McLaughlin et al., Citation2011; Pietrzak et al., Citation2013), whereas other studies have found no such relationship (e.g. Dickstein, Suvak, Litz, & Adler, Citation2010; Freedman, Brandes, Peri, & Shalev, Citation1999).
Finally, the way in which PTSD is assessed has also been found to impact upon prevalence estimates, with self-report measures giving higher prevalence estimates, possibly owing to not accounting for functional impairment caused by PTSD symptoms (Richardson, Frueh, & Acierno, Citation2010). It is important to gain an accurate picture of how these factors impact upon PTSD chronicity in order to determine those for whom PTSD screening and intervention will be most appropriate.
We conducted a systematic review and meta-analysis of longitudinal studies of PTSD in adults, excluding treatment trials. We used meta-analysis to determine pooled estimates of the prevalence of PTSD at specific post-trauma time-points over 2 years following trauma exposure, as well as changes in prevalence between specific time-points. The primary aim was to investigate the pattern of PTSD prevalence over this 24 month window to determine when further recovery becomes unlikely. Given the inconsistencies in the literature on factors which predict recovery or chronicity of PTSD over time, the second aim was to explore potential moderators of both prevalence rates and change. Here, we focused on trauma type (intentional versus unintentional) and assessment type (self-report versus diagnostic interviews), as well as subject-level characteristics of age and sex.
2. Method
2.1. Pre-registration
This review was preregistered on PROSPERO (CRD42018105334).
2.2. Search criteria
PsychINFO, PubMed, and the Published International Literature on Traumatic Stress (PILOTS) database were searched for publications between 1980 [when PTSD was first introduced to the Diagnostic and Statistical Manual of Mental Disorders (DSM)] and November 2019. Search terms were ‘posttraumatic stress’ OR ‘post-traumatic stress’ OR ‘post traumatic stress’ OR ‘PTSD’ AND ‘longitudinal’ OR ‘trajector*’ OR ‘prospective’. Age filters were applied to search for samples from 18 years upwards. Searches were restricted to title and abstract. Search terms were developed in collaboration with a university librarian.
2.3. Inclusion and exclusion criteria
Study samples were included if: they included individuals who had experienced an index trauma, as defined by DSM-IV or DSM-V (APA, Citation2013), after the age of 18 years; they utilized a longitudinal design; they used a standardized measurement of PTSD (self-report or diagnostic interview); and they reported PTSD prevalence for at least two of the following time-points: 1 month, 3 months (± 1 month), 6 months (± 1 month), 9 months (± 1 month), and 12 months (± 1 month). Samples were excluded if: the time between the assessment and trauma was unclear; they were treatment trials or documented that the majority of the sample had received treatment for PTSD during the follow-up period; they focused on individuals with moderate to severe brain injury (likely to influence the course of recovery); they categorized PTSD based on DSM-III criteria (owing to significant disparities between DSM-III and later revisions); there was selective follow-up of participants (e.g. only PTSD cases); or they were not reported in English.
2.4. Procedure
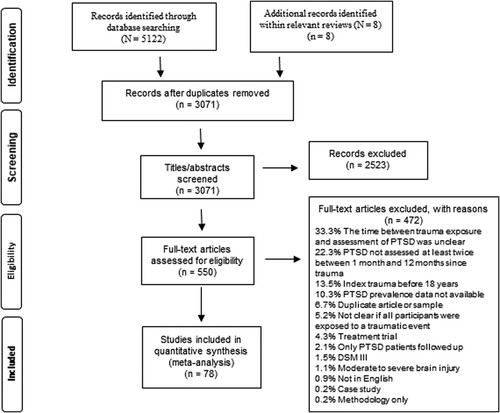
Articles were identified following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (). The initial search identified 3071 abstracts for screening once duplicates were removed. Hand searching of studies within relevant reviews identified an additional eight articles not identified within the electronic search. The abstracts were then screened against the inclusion exclusion criteria by PD and JA, with good agreement (kappa = .87). This left 548 articles for which the full texts were reviewed against the inclusion/exclusion criteria. Interrater reliability was conducted on 10% of the articles, with strong agreement (kappa = .96). At each stage of screening, any disagreements relating to inclusion or exclusions were resolved through consensus meetings, with any decisions impacting on the selection of articles retrospectively applied to all papers. Following full-text screening, 105 articles were identified for inclusion. The main reason for exclusion of studies at this stage was an unclear time elapsed between trauma exposure and assessment (33%). Of the 105 included articles, 37 provided no information on PTSD prevalence. In these cases, authors were emailed for further information, with 10 authors providing the necessary information, requiring 27 articles to be excluded. Thus, the final review included 78 articles.
2.5. Data extraction
Data extraction was conducted by PD and JA. The accuracy of data extraction was assessed for 10% of studies, with strong agreement (98% accuracy). Data extracted were: number of individuals with PTSD and sample size at each time-point recorded, including time-points beyond 12 months where reported; country of study; average age; percentage male; trauma type (intentional or unintentional trauma); and PTSD measurement type (i.e. self-report or diagnostic interviews). Where samples included both intentional and unintentional trauma, the coding was defined by the most prevalent type of trauma within the sample. In studies that used both diagnostic interviews and self-report measures, we extracted the data from the assessment measure with the most time-points available.
2.6. Data analysis strategy
Meta-analyses were conducted using R version 3.6.2 (R Core Team, Citation2019) for pooled prevalence at each time-point (point prevalence) and change in prevalence (prevalence change) between time-points for up to 2 years following a traumatic event. Random effects modelling with 95% confidence limits was used for all estimates (Riley et al., Citation2011). The ‘metaprop’ command was used to derive the pooled prevalence of PTSD for the time-points where two or more studies included data: time (T)1 (1 month), T2 (3 months), T3 (6 months), T4 (9 months), T5 (12 months), T6 (15 months), T7 (18 months), and T9 (24 months). Prevalence data were transformed using the double arcsine transformation, recommended where proportions are near to zero (Barendregt, Doi, Lee, Norman, & Vos, Citation2013), and subsequently back-transformed and converted to a percentage to ease interpretation.
Absolute prevalence estimates may be misleading to interpret in relation to change over time in situations where different studies contribute data at different time-points. Specifically, if there is significant heterogeneity in baseline levels of PTSD across studies, then differences in prevalence across time-points are unlikely to reflect true change (Hiller et al., Citation2016). This issue is avoided using pooled estimates of change in prevalence in each study as the change accounts for starting levels of PTSD. Percentage change in prevalence was calculated as: (Proportion with PTSD at Tx − Proportion of PTSD at Tx − 1)/Proportion with PTSD at Tx − 1, where Tx − 1 and Tx are the earlier and later time-points, respectively. Where there was attrition between time-points, we assumed that the proportion lost to follow-up was equal for those with PTSD and those without PTSD unless reported otherwise. The ‘metabin’ function was used to pool prevalence change statistics for: 1 month to 3 months, 1 month to 6 months, 1 month to 12 months, 3 months to 6 months, 3 months to 12 months, 6 months to 12 months, and 12 months to 24 months.
Heterogeneity across studies was quantified using the I2 statistic, which provides an estimate of the percentage of the total observed variability that is due to true prevalence differences rather than random variation (Higgins, Thompson, Deeks, & Altman, Citation2003). Where significant heterogeneity was identified, we explored the impact of moderators, determined a priori, on point prevalence estimates and prevalence change over time. A range of relevant moderators which may impact PTSD prevalence and course were identified at protocol stage, but the exact choice of moderators analysed was finalized following study selection where it was clear which variables were consistently reported between studies. No analysis was conducted before the selection of these moderators. The final selected moderators were: trauma type (coded as intentional events, such as assaults, which were inflicted by another person, vs unintentional traumas, such as accidents and natural disasters); measurement type (diagnostic interview vs self-report); sex (percentage male); and age. The categorical variables of trauma type and measurement type were examined as moderators using separate subgroup analyses, with between-group differences assessed using the Cochran’s Q statistic. Owing to differences observed within intentional trauma exposure in the context of active military (Fear et al., Citation2010) and occupational settings (i.e. police; Skogstad et al., Citation2013), differences between intentional and unintentional trauma were also explored excluding these trauma samples from the analysis. Subgroup analyses were only conducted for time-points/characteristics where a minimum of four studies in each subgroup were available (Fu et al., Citation2011). The percentage of the sample that was male and age were analysed as continuous variables using meta-regression. Meta-regression was only conducted where the number of studies k ≥ 10 (Borenstein, Hedges, Higgins, & Rothstein, Citation2011). Separate univariate rather than multivariate analyses were conducted because of the small number of studies that included all moderators and to reduce the risk of overfitting (Higgins & Thompson, Citation2004). To check the robustness of regression models, permutation tests were run on those found to be significant (Higgins & Thompson, Citation2004).
3. Results
3.1. Results summary
In total, 78 studies, representing 79 independent samples, were included in the meta-analysis. The details of these samples are shown in Table A1 (Appendix A in the supplementary material). Sample sizes ranged from 21 to 989 participants, with the mean ages of samples ranging from 24.3 to 83.4 years old and the percentage of males making up the sample ranging from 0 to 100 (an overall average of 53%). The majority of studies were from the USA (k = 31), Australia (k = 12), and the UK (k = 10). Studies recruited participants after a variety of types of traumatic events, including physical and sexual assault, life-threatening health problems in self or a close family member, terrorist attack, natural disaster, and pregnancy loss. The most common trauma exposure was motor vehicle accidents (k = 22), an unintentional trauma, with the most common intentional trauma exposure being physical assault (k = 6).
All included studies used DSM-IV criteria for diagnosing PTSD, with the exception of one (Petrinec & Martin, Citation2018) which used DSM-5 criteria. Fifty-seven samples used self-report measures to assess PTSD prevalence, and 21 studies used diagnostic interview, with 17 different PTSD measures used in total.
3.2. Proportion of PTSD at each time-point
The overall pooled PTSD prevalence at 1, 3, 6, 9, 12, and 24 months post-trauma is shown in . (Forest plots for all time-points, including split by trauma type and assessment measure, can be found in Appendix B in the supplementary material.) The highest PTSD prevalence was seen at 1 month post-trauma, with a pooled prevalence of 27.0%. At 3 months, this figure had fallen to 17.6%. The prevalence of PTSD remained relatively stable over the subsequent time-points, with a pooled PTSD prevalence of 16.9% at 12 months and overlapping confidence intervals (CIs) for all prevalence estimates from 3 months onwards (). At the 24 month time-point, 20.7% of individuals were still experiencing PTSD.
Table 1. Results from the meta-analyses conducted at each time-point after trauma exposure, showing pooled prevalence of post-traumatic stress disorder (PTSD) up to 24 months.
3.3. Prevalence change between time-points
The results of prevalence change analysis are presented in . Between 1 and 3 months post-trauma, there was a 9% reduction in PTSD prevalence. The prevalence of PTSD reduced by 5.8% between 1 and 6 months and by 8.9% between 1 and 12 months. By contrast, between 3 and 6 months, there was no evidence of a reduction in prevalence. Small reductions in prevalence were observed between 3 and 12 months and between 6 and 12 months. Over the longer term, between 12 and 24 months, there was no evidence of change in levels of PTSD.
Table 2. Results from the meta-analyses of the changes in absolute post-traumatic stress disorder (PTSD) prevalence between time-points, as measured by risk difference.
3.4. Intentional vs unintentional trauma
The pooled prevalence of PTSD across studies for each of the time-points following exposure to intentional and unintentional trauma separately is shown in . There were no significant differences in PTSD prevalence between intentional or unintentional trauma exposure at 1, 3, 6, or 12 months following exposure (all p > .502). When police (k = 1) and military (k = 1) samples were excluded from the intentional trauma subgroup, there were effects of trauma type at 1 month (Q = 5.68, df = 1, p = .017), with 42.4% PTSD prevalence following intentional trauma versus 23.8% following unintentional trauma (see ), but not at 3 or 6 months (p > .235) (subgroup analyses were not conducted at 12 months because of a lack of available studies at this time-point). Heterogeneity remained significant within subgroups at each time-point (all I2 > 80%).
Table 3. Results from the meta-analyses conducted at each time-point after trauma exposure comparing post-traumatic stress disorder (PTSD) prevalence following either intentional or unintentional trauma exposure.
Across all studies, there was no evidence for differences in change of prevalence between any time-points following exposure to intentional versus unintentional trauma (1–3 months; 1–6 months; 3–12 months; all p > .292). When analyses were rerun with military and police trauma removed from the intentional trauma category, there were significant differences in prevalence change from 1 to 3 months (Q = 5.68, df = 1, p = .0172), with an absolute PTSD prevalence reduction following intentional trauma exposure of 27.4% (95% CI 11.43 to 43.41) compared to 7.33% (95% CI 3.17 to 11.49) following unintentional trauma. There remained no evidence for differences in prevalence change from 1 to 6 months (p = .505). Sufficient studies were not available to assess differences in change across other time-points once military/police samples were removed.
3.5. Diagnostic interviews vs self-report measures
When comparing the results of studies that used self-report measures with those that used diagnostic interviews at each time-point, there were differences in prevalence rates at 3 months and 12 months, with a higher prevalence of PTSD observed for studies using self-report measures (). There was significant heterogeneity within subgroups at all time-points (all I2 > 85%).
Table 4. Results from the meta-analyses conducted at each time-point after trauma exposure comparing post-traumatic stress disorder (PTSD) prevalence following self-report measures and diagnostic interviews.
When comparing change in PTSD prevalence between time-points for studies using diagnostic interviews and those using self-report measures, significant differences were found between 3 and 12 months (Q = 8.95, df = 1, p = .0028) with a 0.2% (95% CI −1.36% to 0.09%) reduction in absolute PTSD prevalence for diagnostic interviews compared with a 4.67% (95% CI −7.38% to −1.99%) reduction with self-report measures. There was no evidence for differences in prevalence change for diagnostic interview and self-report measurement of PTSD between 1 and 3 months (Q = 0.40, df = 1, p = .525), 1 and 6 months (Q = 0, df = 1, p = .974), 1 and 12 months (Q = 2.13, df = 1, p = .145), or 6 and 12 months (Q = 1.36, df = 1, p = .243).
3.6. Age and sex
The results of meta-regression of age and sex are presented in . The mean age of the sample was negatively associated with the prevalence of PTSD at 1 month (R2 = 12.6%), but not at other time-points. There was no relationship between mean age and change in prevalence between any time-points (all p > .29, all R2 < 1%). (Note that reported R2 values are pseudo-R2 values, which provide an estimate of the explained heterogeneity; see Raudenbush, 2009, for further details of their calculation.)
Table 5. Meta-regression of point prevalence.
The percentage of the sample that were male was negatively associated with point prevalence at 1 month and 3 months, but not at 6 months or 12 months post-trauma (). Analyses of prevalence change indicated that the percentage of the sample that was male was positively associated with prevalence change at 1 to 3 months (b = 0.002, 95% CI 0.0005 to 0.004, R2 = 26.7%), 1 to 6 months (b = 0.002, 95% CI 0.0004 to 0.003, R2 = 36.8%), 3 to 6 months (b = 0.0012, 95% CI 0.0001 to 0.0022, R2 = 30.4%), and 3 and 12 months (b = 0.0009, 95% CI 0.0001 to 0.0016 95% CI, R2 = 0%). As positive values of prevalence change indicate an increase in PTSD, a higher proportion of males in the sample was associated with less recovery over time at each of these intervals. Percentage male was not significantly associated with the change in PTSD prevalence between 1 and 12 months (b = 0.003, 95% CI −0.001 to 0.007, R2 = 12.6).
3.7. Baseline PTSD prevalence
Significant heterogeneity was present in PTSD prevalence across studies. As higher initial levels of PTSD may allow for more reduction over time, we tested for moderation of change by baseline PTSD prevalence in post-hoc analyses. The baseline prevalence was the prevalence at the earlier time-point when looking at prevalence change between two time-points (e.g. 1 month is baseline when looking at the 1 to 3 month prevalence change). Baseline PTSD prevalence was found to predict prevalence change between 1 and 3 months (b = -0.0049, 95% CI −0.0065 to −0.0033, R2 = 67.9%), 1 and 6 months (b = -0.0044, 95% CI −0.0062 to −0.0026, R2 = 73.8%), 3 and 6 months (b = -0.0018, 95% CI −0.0031 to −0.0004, R2 = 94.9%), and 3 and 12 months (b = -0.0022, 95% CI −0.0031 to −0.0012, R2 = 99.3%), with higher baseline prevalence being strongly associated with greater prevalence reduction over every time interval (See Appendix B, in the supplementary material, to aid interpretation).
3.8. Publication bias
Funnel plots were inspected for possible publication bias (i.e. preference for publication where PTSD rates were higher). Funnel plots were symmetrical for all point prevalences (1, 3, 6, 9, and 12 months) except at 24 months, providing little evidence of publication bias.
4. Discussion
We used a meta-analytic approach to determine the pooled prevalence rates of PTSD at different time-points post-trauma and changes in the prevalence of PTSD over time. The results showed that in the month following trauma, an estimated 27% of individuals were experiencing PTSD. While there was a significant reduction in prevalence from 1 to 3 months, after this time the rates of PTSD remained relatively stable. At the 2 year follow-up, 21% of individuals exposed to trauma were still experiencing PTSD. This pattern of observations was similar based on point prevalence estimates and on analyses of prevalence change over time, providing a robust picture of the extent of PTSD recovery over different time intervals following trauma.
The overall pooled prevalence rates of PTSD in the year following trauma were 27% at 1 month, 18% at 3 months, 20% at 6 months, 21% at 9 months, 17% at 12 months, and 21% at 24 months, estimates that are broadly consistent with conclusions based on non-meta-analytic review of the longitudinal evidence base (Santiago et al., Citation2013). It is striking to note that prevalence estimates at 2 years post-trauma were similar to those present at 3 months, highlighting the potentially chronic nature of PTSD once established. This pattern of significant prevalence reduction in PTSD between 1 and 3 months but relatively stable prevalence rates thereafter was also replicated in analyses of prevalence change statistics. Our meta-analysis found that the only significant reductions occurred when later prevalence rates were compared to the 1 month prevalence. From 3 months post-trauma, evidence of further significant change in prevalence rates was lacking. Analyses of prevalence change statistics provide important confirmation of the conclusions from point prevalence analyses as they are based on examining change scores from within the same study, whereas point prevalence estimates at different time-points may pool evidence from different and heterogeneous studies. These findings highlight that for a significant proportion of individuals with PTSD there is a period of remission in the initial 1–3 months following trauma. However, beyond this, there appears to be limited further recovery and PTSD is likely to be extremely persistent over time if left untreated. Timely provision of evidence-based interventions to reduce the potentially chronic course of PTSD following trauma is essential.
In line with previous research, we found higher rates of PTSD following intentional versus unintentional trauma at 1 month (Kessler et al., Citation2017). However, we also found evidence that intentional trauma was associated with higher levels of prevalence reduction between 1 and 3 months. Beyond this initial point, there were no differences by trauma type in prevalence across the time-points, suggesting that higher rates of remission may offset initially higher levels of PTSD among those exposed to intentional trauma. It is noteworthy that this increased prevalence in PTSD at 1 month following intentional trauma was only evident when excluding two samples where intentional trauma exposures occurred in the context of policing and military combat. Intentional trauma exposure within professional contexts may be mitigated against within these samples; previous research has found prior experience and training in military samples to be related to rates of PTSD (Hunt, Wessely, Jones, Rona, & Greenberg, Citation2014), with preparedness within professional contexts potentially increasing feelings of control and self-efficacy and reducing subsequent peritraumatic reactions (Bonanno et al., Citation2012; Whealin, Ruzek, & Southwick, Citation2008).
The trajectories found in this meta-analysis for intentional and unintentional trauma exposure contrast with the conclusions of a previous review, where prevalence rates of PTSD following unintentional trauma were found to be higher than for intentional trauma initially, but while prevalence rates reduced for unintentional trauma over time they increased for intentional trauma (Santiago et al., Citation2013). There are several possible explanations for these discrepant findings. First, Santiago et al. (Citation2013) derived trends based on median PTSD prevalence across studies, whereas the pooled prevalence estimates provided by meta-analysis provide a more accurate assessment of prevalence based on available study data. Secondly, we excluded from our review samples where the timeline between trauma exposure and PTSD measurement was unclear. These included two studies of refugee populations that had been exposed to war (Roth, Ekblad, & Ågren, Citation2006; Vojvoda, Weine, McGlashan, Becker, & Southwick, Citation2008), with likely multiple trauma exposures, ongoing instability, and lack of social support, which were included in the review by Santiago et al. (Citation2013). More broadly, the need for a clear timeline limited our meta-analysis predominantly to single-incident trauma samples. Individuals with more chronic trauma presentations may have different recovery trajectories and prevalence rates over time as a result of symptoms of complex PTSD and ongoing instability and risk of further trauma (Cloitre, Citation2021). It will be important for future research to explore the recovery trajectories following more complex trauma presentations. However, the results from our meta-analysis indicate that following exposure to predominantly single-incident traumas, there is little difference in recovery trajectories following intentional or unintentional trauma exposure.
In terms of the impact of the assessment measure on PTSD prevalence over time, significant differences were observed when PTSD was assessed using self-report measures versus diagnostic interviews, with studies employing self-report measures generally reporting higher PTSD prevalence. These observations based on point-prevalence are in line with the conclusions of a review of cross-sectional studies of PTSD prevalence (Richardson et al., Citation2010). Despite these differences in prevalence at individual time-points, the relative change in PTSD prevalence over time was similar for both diagnostic interview and self-report measures. This suggests that while self-report and diagnostic interview may generate different absolute prevalence estimates, these approaches are likely to be similarly sensitive to detecting change in PTSD over time.
We also found evidence of sex differences in PTSD prevalence and change over time. Specifically, a higher proportion of females in the sample was associated with a higher prevalence of PTSD at 1 and 3 months following trauma. However, a higher proportion of females was also associated with a greater reduction in PTSD prevalence relatively consistently across the first 12 months post-trauma. This female recovery advantage may be partly explained by higher initial levels of PTSD among females, with baseline PTSD levels being a strong predictor of recovery. Nonetheless, even once baseline prevalence had been controlled for, a higher proportion of females was associated with greater prevalence reduction between 1 and 6 months. Our observations should be considered in the context of the essentially single-incident trauma studies that contributed to our analysis, which resulted in the exclusion of some complex traumas (e.g. sexual abuse) to which females may be particularly vulnerable (Giarratano, Ford, & Nochajski, Citation2020). However, our findings are consistent with clinical observations from some studies which found that females may be more responsive to treatment for PTSD than males (e.g. Galovski, Blain, Chappuis, & Fletcher, Citation2013; Tarrier, Sommerfield, Pilgrim, & Faragher, Citation2000). Such an increased treatment effect has been hypothesized to result from an increased willingness (or perhaps familiarity resulting from implicit societal norms) in females to disclose their psychological difficulties (Purves & Erwin, Citation2004; Tarrier et al., Citation2000). It is possible that similar factors may have contributed to the larger reduction in PTSD over time observed among females versus males in the current study. Such possible sex differences in the factors contributing to recovery warrant further investigation.
Finally, we explored the relationship between the mean age of the sample and prevalence of PTSD over time, finding that while younger age was associated with higher PTSD 1 month following trauma, it was not at any other time-point, nor was it related to change in prevalence over time. Younger participants may have more intense initial emotional reactions to trauma or fewer coping resources, or may experience qualitatively different traumas to older participants (e.g. certain types of assaultive violence tend to affect younger men and women) (Kessler et al., Citation2017). It should be highlighted that participants’ average ages in the included studies were young to middle-aged, and only one study had an average of over 60 years. Therefore, the current meta-analysis does not provide evidence either way as to how older age might influence remission from PTSD.
4.1. Clinical implications
Our findings have important clinical implications for the screening and delivery of interventions aimed at treating PTSD following single-incident trauma. Because our inclusion criteria required studies to have a clear time between trauma and follow-up, studies of multiple, prolonged, or complex traumas were excluded and therefore our findings do not have direct implications for these trauma types. When considering intervention following trauma, it is important to provide treatment at the time most likely to outperform natural rates of recovery to ensure cost-effective provision of care, while also ensuring that treatment is provided in a timely manner to prevent more intractable difficulties from developing. Research has also indicated that immediate interventions following trauma can sometimes be detrimental to recovery and disrupt coping (Rose et al., Citation2004). From our analysis, remission within the initial 3 month period post-trauma is evident. However, beyond this, a strong case should be made for the provision of interventions, such as evidenced-based psychological therapies (Bisson, Roberts, Andrew, Cooper, & Lewis, Citation2013), to address the chronic course of PTSD seen in a substantial proportion of individuals exposed to trauma. Of course, while intervention at around 3 months post-trauma may be broadly appropriate, individuals experiencing particularly high levels of distress and/or functional impairment due to PTSD during the initial post-trauma period may require more immediate support. In assessing individuals presenting to mental health services with likely PTSD, clinicians should assess the length of time that symptoms have been present, and if this exceeds 3 months it should be considered unlikely that an individual will recover from PTSD without an intervention that targets the underlying maintenance factors of PTSD. Our study has indicated that such an approach is warranted both in individuals who have experienced intentional trauma and in those who have experienced unintentional trauma. Our study also suggests that while males are less likely to develop PTSD in the month following trauma, they are also less likely to recover, making targeted, timely intervention important.
The measurement of PTSD using diagnostic interviews resulted in a lower prevalence of PTSD than that of self-report. While it is not possible in this study to assess the relative accuracy of these two forms of assessment, in clinical settings screening based on self-report may minimize the risk of missing potential cases of PTSD, with follow-up interviews to confirm diagnosis and fully assess levels of distress and functional impairment. This can then allow for a clinical judgement around the provision of care, or symptom monitoring if it is deemed more appropriate. As self-report measures and diagnostic interviews resulted in similar time courses of PTSD recovery, both assessments have the potential to identify those most at risk of developing more chronic PTSD symptoms.
4.2. Limitations
First, a high level of heterogeneity was observed across studies included in the meta-analyses, particularly in analyses of point prevalence, and which was not accounted for by our selected moderators. Significant heterogeneity in prevalence estimates is not unexpected given the inclusion of 79 studies, exploring a range of traumas in participants from a diverse range of cultural and social contexts. It is essential to interpret findings considering this high degree of heterogeneity, particularly when interpreting absolute prevalence statistics. Secondly, PTSD prevalence was measured using a wide variety of measures, and within self-report measures there was inconsistency in the cut-off used to classify probable PTSD, which is likely to have contributed to heterogeneity in point prevalence estimates. More weight should be given to the pattern of prevalence change over time, rather than absolute point prevalence statistics. Thirdly, when conducting the meta-analysis of changes in PTSD prevalence between time-points, it was necessary to assume that those individuals who were diagnosed with PTSD at the later time-point were individuals diagnosed with PTSD at the previous time-point, which does not account for the possibility of new onsets of PTSD at later time-points. Nonetheless, the existing literature suggests that only a small proportion appear to develop delayed-onset PTSD, with only 3.5% of PTSD cases occurring after the 3 month period (Santiago et al., Citation2013). In addition, unless otherwise reported, it was assumed that the rates of dropout were the same for PTSD cases and non-cases. If differential dropout were systematically present, this could bias estimates of PTSD prevalence over time.
Importantly, to examine the course of PTSD recovery without treatment, this review excluded treatment trials and those studies where it was documented that the majority of participants received treatment for PTSD within the follow-up period. The majority of studies included in our review did not report on treatment usage during the follow-up period, with a minority stating explicitly that participants did not receive any treatment and 11 studies reporting on treatment use within their studies. Types of treatment received by participants across those 11 studies varied. Some studies reported psychotropic (e.g. anxiolytics, sedatives) or opioid medication usage in the hours or days following trauma, which is relatively unlikely to have influenced of the course of recovery from 1 month onwards, the focal timeframe for our analyses. Other studies reported on wider treatment access, typically over a longer timeframe (between 1 and 13 months post-trauma). This was highly variable across studies: for example, Vranceanu et al. (Citation2014) reported that 1% received ‘psychotherapy’ at 1–2 months post-trauma, whereas Roy-Burne et al. (Citation2004) reported that 43% ‘visited a mental health provider’ after 1 month. It is likely that some degree of treatment for PTSD or other mental disorders as part of routine care is also present during follow-up periods in those studies which do not report it. We were unable to capture or account for this. Unaccounted-for access to interventions may have contributed to the unexplained heterogeneity in our analyses. Notwithstanding this limitation, we note that the majority of recovery within our review was found to occur within the first 3 months following trauma, with little change in PTSD prevalence observed beyond this point. It is relatively unlikely that participants would have received evidenced-based interventions for PTSD within this early timeframe, increasing the confidence that these changes in prevalence reflect the course of recovery from PTSD without treatment.
5. Conclusions
This study reports the first meta-analysis of change in PTSD prevalence in the first 2 years following trauma. The results indicate that spontaneous remission occurs within the initial period post-trauma, but this is limited, such that beyond 3 months post-trauma there was little evidence of further reduction in the prevalence of PTSD. At the 2 year follow-up, one in five individuals exposed to trauma were still experiencing PTSD. We found intentional versus unintentional trauma exposure to predict higher rates of PTSD in the first month following exposure, but not at later time-points. We also found that while samples with a higher percentage of females were associated with higher PTSD prevalence rates after 1 month, a higher percentage of females was also associated with a larger reduction in PTSD prevalence over time. Future research should prioritize the identification of further moderators that may explain differences in recovery to help in the provision of interventions for populations potentially at risk of developing a more chronic course of PTSD.
Supplemental Material
Download Zip (3.8 MB)Supplemental Material
Download MS Word (28.8 KB)Supplemental Material
Download MS Word (3.9 MB)Supplemental Material
Download MS Word (23.2 KB)Acknowledgements
The authors would like to thank Justin Hodds, subject librarian, for advice on the search strategy, and Dr Tim Cadman for providing advice at the data analysis and interpretation stage. We would also like to thank all the authors who provided additional data which were unavailable in the original publication of their studies.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- References listed are limited to those referred to in the text of the article. For references included in the meta-analysis, please see Appendix C in the supplementary material.
- Aldwin, C. M., Sutton, K. J., Chiara, G., & Spiro, A., 3rd (1996). Age differences in stress, coping, and appraisal: Findings from the normative aging study. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 51(4), 179–188.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
- Bangasser, D. A., Eck, S. R., & Ordoñes Sanchez, E. (2019). Sex differences in stress reactivity in arousal and attention systems. Neuropsychopharmacology, 44(1), 129–13we9. doi:10.1038/s41386-018-0137-2
- Barendregt, J. J., Doi, S. A., Lee, Y. Y., Norman, R. E., & Vos, T. (2013). Meta-analysis of prevalence. Journal of Epidemiology and Community Health, 67(11), 974–978. doi:10.1136/jech-2013-203104
- Birkeland, M. S., Skar, A. M. S., & Jensen, T. K. (2021). Do different traumatic events invoke different kinds of post-traumatic stress symptoms? European Journal of Psychotraumatology, 12(sup1), 1866399. doi:10.1080/20008198.2020.1866399
- Bisson, J. I., Roberts, N. P., Andrew, M., Cooper, R., & Lewis, C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews, (12), CD003388.
- Bonanno, G. A., Mancini, A. D., Horton, J. L., Powell, T. M., LeardMann, C. A., Boyko, E. J., & Millennium Cohort Study Team. (2012). Trajectories of trauma symptoms and resilience in deployed US military service members: Prospective cohort study. The British Journal of Psychiatry, 200(4), 317–323. doi:10.1192/bjp.bp.111.096552
- Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods, 1(2), 97–111. doi:10.1002/jrsm.12
- Breslau, N., & Davis, G. C. (1992). Posttraumatic stress disorder in an urban population of young adults: Risk factors for chronicity. The American Journal of Psychiatry, 149(5), 671–675. doi:10.1176/ajp.149.5.671
- Breslau, N. (2009). The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma, Violence, & Abuse, 10(3), 198–210. doi:10.1177/1524838009334448
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. doi:10.1037/0022-006X.68.5.748
- Burri, A., Maercker, A., Krammer, S., & Simmen-Janevska, K. (2013). Childhood trauma and PTSD symptoms increase the risk of cognitive impairment in a sample of former indentured child laborers in old age. PLOS ONE, 8(2), e57826. doi:10.1371/journal.pone.0057826
- Christiansen, D. M., & Berke, E. T. (2020). Gender- and sex-based contributors to sex differences in PTSD. Current Psychiatry Reports, 22(4), 19. doi:10.1007/s11920-020-1140-y
- Christiansen, D. M., & Hansen, M. (2015). Accounting for sex differences in PTSD: A multi-variable mediation model. European Journal of Psychotraumatology, 6, 26068. doi:10.3402/ejpt.v6.26068
- Cloitre, M. (2021). Complex PTSD: Assessment and treatment. European Journal of Psychotraumatology, 12(sup1), 1866423. doi:10.1080/20008198.2020.1866423
- Dickstein, B. D., Suvak, M., Litz, B. T., & Adler, A. B. (2010). Heterogeneity in the course of posttraumatic stress disorder: Trajectories of symptomatology. Journal of Traumatic Stress, 23, 331–339. doi:10.1002/jts.20523
- Fear, N. T., Jones, M., Murphy, D., Hull, L., Iversen, A. C., Coker, B., & Greenberg, N. (2010). What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. The Lancet, 375, 1783–1797. doi:10.1016/S0140-6736(10)60672-1
- Freedman, S. A., Brandes, D., Peri, T., & Shalev, A. (1999). Predictors of chronic post-traumatic stress disorder. A prospective study. British Journal of Psychiatry, 174, 353–359. doi:10.1192/bjp.174.4.353
- Fu, R., Gartlehner, G., Grant, M., Shamliyan, T., Sedrakyan, A., Wilt, T. J., … Trikalinos, T. A. (2011). Conducting quantitative synthesis when comparing medical interventions: AHRQ and the effective Health care program. Journal of Clinical Epidemiology, 64(11), 1187–1197. doi:10.1016/j.jclinepi.2010.08.010
- Galatzer-Levy, I. R., Ankri, Y., Freedman, S., Israeli-Shalev, Y., Roitman, P., Gilad, M., & Shalev, A. Y. (2013). Early PTSD symptom trajectories: Persistence, recovery, and response to treatment: Results from the Jerusalem Trauma Outreach and Prevention Study (J-TOPS). PLoS One, 8(8), e70084. doi:10.1371/journal.pone.0070084
- Galovski, T. E., Blain, L. M., Chappuis, C., & Fletcher, T. (2013). Sex differences in recovery from PTSD in male and female interpersonal assault survivors. Behaviour Research and Therapy, 51(6), 247–255. doi:10.1016/j.brat.2013.02.002
- Giarratano, P., Ford, J. D., & Nochajski, T. H. (2020). Gender differences in complex posttraumatic stress symptoms, and their relationship to mental health and substance abuse outcomes in incarcerated adults. Journal of Interpersonal Violence, 35(5–6), 1133–1157. doi:10.1177/0886260517692995
- Higgins, J.P., & Thompson, S.G. (2004). Controlling the risk of spurious findings from meta-regression. Statistics in Medicine, 23, 1663–1682. doi:10.1002/sim.1752
- Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557–560. doi:10.1136/bmj.327.7414.557
- Hiller, R. M., Meiser-Stedman, R., Fearon, P., Lobo, S., McKinnon, A., Fraser, A., & Halligan, S. L. (2016). Research review: Changes in the prevalence and symptom severity of child post-traumatic stress disorder in the year following trauma – A meta-analytic study. Journal of Child Psychology and Psychiatry, 57(8), 884–898. doi:10.1111/jcpp.12566
- Hiscox, L. V., Bray, S., Fraser, A., Meiser-Stedman, R., Seedat, S., & Halligan, S. L. (2022). Sex differences in the severity and natural recovery of child PTSD symptoms: A longitudinal analysis of children exposed to acute trauma. Psychological Medicine, 1–7. doi:10.1017/S0033291721004694
- Hsu, C.-M. K., Kleim, B., Nicholson, E. L., Zuj, D. V., Cushing, P. J., Gray, K. E., … Felmingham, K. L. (2018). Sex differences in intrusive memories following trauma. PLoS One, 13(12), e0208575-e0208575.
- Hunt, E. J. F., Wessely, S., Jones, N., Rona, R. J., & Greenberg, N. (2014). The mental health of the UK armed forces: Where facts meet fiction. European Journal of Psychotraumatology, 5, 10.3402/ejpt.v3405.23617.
- Jiang, T., Webster, J. L., Robinson, A., Kassam-Adams, N., & Richmond, T. S. (2018). Emotional responses to unintentional and intentional traumatic injuries among urban black men: A qualitative study. Injury, 49(5), 983–989. doi:10.1016/j.injury.2017.12.002
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., … Koenen, K. C. (2017). Trauma and PTSD in the WHO World Mental Health surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. doi:10.1080/20008198.2017.1353383
- Lipton, M. I., & Schaffer, W. R. (1986). Post-traumatic stress disorder in the older veteran. Military Medicine, 151(10), 522–524. doi:10.1093/milmed/151.10.522
- McLaughlin, K. A., Berglund, P., Gruber, M. J., Kessler, R. C., Sampson, N. A., & Zaslavsky, A. M. (2011). Recovery from PTSD following hurricane Katrina. Depression and Anxiety, 28(6), 439–446. doi:10.1002/da.20790
- Moos, R. H., Brennan, P. L., Schutte, K. K., & Moos, B. S. (2006). Older adults’ coping with negative life events: Common processes of managing health, interpersonal, and financial/work stressors. The International Journal of Aging and Human Development, 62(1), 39–59. doi:10.2190/ENLH-WAA2-AX8J-WRT1
- Morina, N., Wicherts, J. M., Lobbrecht, J., & Priebe, S. (2014). Remission from post-traumatic stress disorder in adults: A systematic review and meta-analysis of long term outcome studies. Clinical Psychology Review, 34(3), 249–255. doi:10.1016/j.cpr.2014.03.002
- Olatunji, B. O., Cisler, J. M., & Tolin, D. F. (2007). Quality of life in the anxiety disorders: A meta-analytic review. Clinical Psychology Review, 27(5), 572–581. doi:10.1016/j.cpr.2007.01.015
- Olff, M. (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8(sup4), 1351204. doi:10.1080/20008198.2017.1351204
- Ozer, E. J., Best, S. R., Lipsey, T. L., & Weiss, D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129(1), 52–73. doi:10.1037/0033-2909.129.1.52
- Petrinec, A. B., & Martin, B. R. (2018). Post-intensive care syndrome symptoms and health-related quality of life in family decision-makers of critically ill patients. Palliative and Supportive Care, 16(6), 719–724. doi:10.1017/S1478951517001043
- Pietrzak, R. H., Van Ness, P. H., Fried, T. R., Galea, S., & Norris, F. H. (2013). Trajectories of posttraumatic stress symptomatology in older persons affected by a large-magnitude disaster. Journal of Psychiatric Research, 47(4 PG-520–6), 520–526. https://doi.org/10.1016/j.jpsychires.2012.12.005
- Purves, D. G., & Erwin, P. G. (2004). Post-traumatic stress and self-disclosure. Journal of Psychology: Interdisciplinary and Applied, 138(1), 23–34. doi:10.3200/JRLP.138.1.23-34
- R Core Team. (2018). R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing.
- Richardson, L. K., Frueh, B. C., & Acierno, R. (2010). Prevalence estimates of combat-related post-traumatic stress disorder: Critical review. Australian and New Zealand Journal of Psychiatry, 44(1), 4–19. doi:10.3109/00048670903393597
- Riley, R. D., Higgins, J. P. T., & Deeks, J. J. (2011). Interpretation of random effects meta-analyses. BMJ, 342, d549. doi:10.1136/bmj.d549
- Roberts, A. L., Kubzansky, L. D., Chibnik, L. B., Rimm, E. B., & Koenen, K. C. (2020). Association of posttraumatic stress and depressive symptoms with mortality in women. JAMA Netw Open, 3 (12), e2027935. doi:10.1001/jamanetworkopen.2020.27935
- Rose, S.C., Bisson, J., Churchill, R., & Wessely, S. (2002). Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews, (2), CD000560.
- Roth, G., Ekblad, S., & Ågren, H. (2006). A longitudinal study of PTSD in a sample of adult mass-evacuated Kosovars, some of whom returned to their home country. European Psychiatry, 21(3), 152–159. doi:10.1016/j.eurpsy.2005.11.004
- Roy-Byrne, P. P., Russo, J., Michelson, E., Zatzick, D., Pitman, R. K., & Berliner, L. (2004). Risk factors and outcome in ambulatory assault victims presenting to the acute emergency department setting: Implications for secondary prevention studies in PTSD. Depress Anxiety, 19, 77–84. doi:10.1002/da.10132
- Santiago, P. N., Ursano, R. J., Gray, C. L., Pynoos, R. S., Spiegel, D., Lewis-Fernandez, R., & Fullerton, C. S. (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLoS One, 8(4), e59236. doi:10.1371/journal.pone.0059236
- Skogstad, M., Skorstad, M., Lie, A., Conradi, H. S., Heir, T., & Weisæth, L. (2013). Work-related post-traumatic stress disorder. Occupational Medicine, 63(3), 175–182. doi:10.1093/occmed/kqt003
- Takai, N., Yamaguchi, M., Aragaki, T., Eto, K., Uchihashi, K., & Nishikawa, Y. (2007). Gender-specific differences in salivary biomarker responses to acute psychological stress. Annals of the New York Academy of Sciences, 1098(1), 510–515. doi:10.1196/annals.1384.014
- Tarrier, N., Sommerfield, C., Pilgrim, H., & Faragher, B. (2000). Factors associated with outcome of cognitive-behavioural treatment of chronic post-traumatic stress disorder. Behaviour Research and Therapy, 38(2), 191–202. doi:10.1016/S0005-7967(99)00030-3
- Vojvoda, D., Weine, S. M., McGlashan, T. H., Becker, D. F., & Southwick, S. M. (2008). Posttraumatic stress disorder symptoms in Bosnian refugees 3 1/2 years after resettlement. Journal of Rehabilitation Research and Development, 45, 421–426.
- Vranceanu, A., Bachoura, A., Weening, A., Vrahas, M., Smith, R. M., & Ring, D. (2014). Psychological factors predict disability and pain intensity after skeletal trauma. The Journal of Bone & Joint Surgery, 96, e20. doi:10.2106/JBJS.L.00479
- Whealin, J. M., Ruzek, J. I., & Southwick, S. (2008). Cognitive–behavioral theory and preparation for professionals at risk for trauma exposure. Trauma, Violence, & Abuse, 9(2), 100–113. doi:10.1177/1524838008315869
- Yin, Q., Wu, L., Yu, X., & Liu, W. (2019). Neuroticism predicts a long-term PTSD after earthquake trauma: The moderating effects of personality. Frontiers in Psychiatry, 10. doi:10.3389/fpsyt.2019.00657.