ABSTRACT
Background
Childhood maltreatment (CM) is frequently linked to interpersonal problems such as difficulties in social relationships, loneliness, and isolation. These difficulties might partly stem from troubles regulating comfortable interpersonal distance (CIPD).
Objective
We experimentally investigated whether CM manifests in larger CIPD and whether all subtypes of CM (i.e., physical, emotional, or sexual abuse and physical or emotional neglect) affect CIPD.
Methods
Using the stop-distance method (i.e. a team member approached participants until the latter indicated discomfort), we assessed CIPD in 84 adults with a self-reported history of CM (24 with depressive symptoms) and 57 adult controls without a history of CM (without depressive symptoms).
Results
Adults with CM showed a larger CIPD (Mdn = 86 cm) than controls (Mdn = 68 cm), and CIPD was largest for those with CM combined with current depressive symptoms (Mdn = 145 cm) (p’s < .047). In the latter group, all subtypes of CM were associated with a larger CIPD compared to controls (p’s < .045). In the CM group without depressive symptoms, only those with emotional abuse (p = .040) showed a larger CIPD than controls.
Conclusions
These results add to findings of differential socio-emotional long-term consequences of CM, depending upon the subtype of CM. Future research should explore whether a larger CIPD has a negative impact on social functioning in individuals exposed to CM, particularly in those with depressive symptoms.
HIGHLIGHTS
Adults with child maltreatment (CM) prefer larger physical distances.
• This effect is more pronounced in those with CM and depressive symptoms.
• Troubled regulation of physical distance might contribute to interpersonal problems.
Antecedentes:
El maltrato infantil (CM en su sigla en inglés) se vincula frecuentemente a problemas interpersonales como dificultades en las relaciones sociales, soledad y aislamiento. Estas dificultades pueden deberse en parte a problemas para regular la distancia interpersonal cómoda (CIPD en su sigla en inglés).
Objetivo:
Investigamos experimentalmente si CM se manifiesta en mayor CIPD y si todos los subtipos de CM (es decir, abuso físico, emocional o sexual y negligencia física o emocional) afectan la CIPD.
Método:
Utilizando el método de distancia de parada (es decir, un miembro del equipo se acercó a los participantes hasta que indicaran malestar), evaluamos la CIPD en 84 adultos con antecedentes autoreportados de CM (24 con síntomas depresivos) y 57 controles adultos sin antecedentes de CM (sin síntomas depresivos).
Resultados:
Los adultos con CM mostraron una CIPD mayor (Mdn = 86 cm) que los controles (Mdn = 68 cm), y la CIPD fue mayor para aquellos con CM combinado con síntomas depresivos actuales (Mdn = 145 cm) (p < .047). En el último grupo, todos los subtipos de CM se asociaron con una CIPD mayor en comparación con los controles (p < .045). En el grupo de CM sin síntomas depresivos, solo aquellos con maltrato emocional (p = .040) mostraron una CIPD mayor que los controles.
Conclusiones:
Estos resultados se suman a los hallazgos de las consecuencias socioemocionales diferenciales a largo plazo del CM, según el subtipo. La investigación futura debería explorar si una CIPD mayor tiene un impacto negativo en el funcionamiento social en individuos expuestos a CM, particularmente en aquellos con síntomas depresivos.
背景: 儿童虐待 (CM) 经常与人际关系问题有关,例如社会关系困难、孤独和孤立。这些困难可能部分源于调节舒适人际距离(CIPD)的困难。
目的: 我们通过实验研究了 CM 是否表现出在更大的 CIPD,以及 CM 所有亚型(即身体、情感或性虐待以及身体或情感忽视)是否都会影响 CIPD。
方法: 使用停止距离法(即,一名团队成员接近参与者,直到后者表示不适),我们评估了 84 名有自我报告 CM 史的成年组(24 名有抑郁症状)和 57 名没有CM史的成人对照组的 CIPD(没有抑郁症状)。
结果: CM 成人组的 CIPD (Mdn = 86 cm) 比对照组 (Mdn = 68 cm) 大,CM 合并当前抑郁症状的 CIPD 最大 (Mdn = 145 cm) (p < .047)。在后一组中,与对照组相比,CM 的所有亚型都与更大的 CIPD 相关(p < .045)。在没有抑郁症状的 CM 组中,只有那些有情绪虐待的人 (p = .040) 表现出比对照组更大的 CIPD。
结论: 这些结果增加了 CM 不同社会情感长期后果的发现,取决于 CM 的亚型。未来的研究应该探索更大的 CIPD 是否对暴露于 CM 个体的社会功能产生负面影响,尤其是那些有抑郁症状的个体。
Growing up in a safe and stable environment where a child’s physical and emotional needs are met is crucial for the development and health of a child. However, childhood maltreatment (CM) is a major public health concern across the globe, affecting millions of children every year (Stoltenborgh, Bakermans-Kranenburg, Alink, & Ijzendoorn, Citation2015). CM is linked to various long-term interpersonal problems such as difficulties in relationships (Colman & Widom, Citation2004), loneliness, and social isolation (Loos & Alexander, Citation1997). These impairments are alarming, given that supportive relationships are a major resilience factor protecting against the development of mental disorders (Holz, Tost, & Meyer-Lindenberg, Citation2020; Pfaltz et al., Citation2021) and can also help to break the cycle of intergenerational transmission of maltreatment (Thornberry et al., Citation2013).
1.1. CM and its link to interpersonal difficulties
While there is consistent evidence that children and adults with a history of CM experience difficulties in social functioning (Anthonysamy & Zimmer-Gembeck, Citation2007; Colman & Widom, Citation2004; McCrory, Ogle, Gerin, & Viding, Citation2019; Zamir, Citation2021), very little research has focused on the underlying processes leading to such difficulties. In a recent review, Zamir (Citation2021) concludes that CM is associated with an overall decrease in relationship quality which might at least in part stem from a greater tendency for interpersonal conflicts (Bigras, Godbout, Hébert, Runtz, & Daspe, Citation2015), and ineffective communication (Busby, Walker, & Holman, Citation2011; Whisman, Citation2014). Importantly, individuals with CM often experience fear of intimacy (e.g. Davis, Petretic-Jackson, & Ting, Citation2001), struggle with social withdrawal (Hildyard & Wolfe, Citation2002) and feel less well accepted by their partners (Vaillancourt-Morel, Rellini, Godbout, Sabourin, & Bergeron, Citation2019). Both fear of intimacy and a tendency towards social withdrawal might make it difficult to build and maintain meaningful relationships (Barzeva, Richards, Meeus, & Oldehinkel, Citation2021; Thelen, Vander Wal, Thomas, & Harmon, Citation2000). To develop interventions that improve the quality of social relationships and mental health, it is thus important to identify the pathways leading to interpersonal problems in those affected by CM.
1.2. Relationship between CIPD and experiences of CM
An important, yet understudied, potential link between CM and interpersonal difficulties is the regulation of (physical) closeness and distance. The physical distance kept between oneself and others that cannot be intruded without causing emotional and physical (Åhs, Dunsmoor, Zielinski, & LaBar, Citation2015; Hayduk, Citation1978) discomfort is described by the term personal space (Hayduk, Citation1978) or interpersonal distance (Kaitz, Bar-Haim, Lehrer, & Grossman, Citation2004). To date, different health conditions have been associated to either larger (e.g. social anxiety (Perry, Rubinsten, Peled, & Shamay-Tsoory, Citation2013)), post-traumatic stress disorder (Bogovic, Mihanovic, Jokic-Begic, & Svagelj, Citation2014) or smaller (e.g. schizophrenia (Di Cosmo et al., Citation2018)) preferences for CIPD. In the context of trauma and anxiety, personal space is also referred to as a personal ‘safety zone’ as its shape and size are flexible to situational circumstances such as (perceived or actual) threat (Cole, Balcetis, & Dunning, Citation2013). Children learn to regulate the size of their personal space while growing up (Aiello & De Carlo Aiello, Citation1974). People who experienced CM often become hypervigilant towards threat (McCrory et al., Citation2011; Teicher & Samson, Citation2016). CM might thus result in greater CIPD. More specifically, threatening experiences such as physical and sexual abuse directly violate children’s personal space, potentially affecting the development of CIPD. Indeed, physically abused children show larger CIPD compared to non-abused children (Vranic, Citation2003). In her study, Vranic (Citation2003) assessed CIPD using the well-established (Bogovic et al., Citation2014; Hayduk, Citation1978; Kaitz et al., Citation2004; Maier et al., Citation2020; Perry et al., Citation2013) and reliable (Hayduk, Citation1983) experimental stop-distance task, i.e. children were approached by members of the study team and instructed to say stop once they started feeling uncomfortable with the physical distance between them. A larger CIPD, assessed with the same task, has also been observed in adults with post-traumatic stress disorder (Bogovic et al., Citation2014) and with a history of different types of CM (Maier et al., Citation2020), pointing to long-term effects of CM on CIPD. Though subtype specific effects are documented for other socio-emotional processes (e.g. facial emotion processing (Iffland & Neuner, Citation2020)) and previous research highlights the importance to distinguish between experiences of threat and deprivation (e.g. McLaughlin, Sheridan, & Lambert, Citation2014), studies assessing the relationship between specific types of CM and CIPD are lacking.
1.3. CM and depression
Individuals with CM are at risk to develop symptoms of depression (Humphreys, LeMoult, Wear, Piersiak, & Gotlib, Citation2020) or post-traumatic stress disorder (Gardner, Thomas, & Erskine, Citation2019; Hepp, Schmitz, Urbild, Zauner, & Niedtfeld, Citation2021; Vranceanu, Hobfoll, & Johnson, Citation2007), with particularly high levels in those affected by emotional abuse and neglect (Humphreys et al., Citation2020). Depressive symptoms have been linked to larger CIPD in women suffering from eating disorders (Welsch, Hecht, Kolar, Witthöft, & Legenbauer, Citation2020) and in adults with adjustment disorder with depressed mood (Ponizovsky et al., Citation2013). It is however unknown whether the relationship between CM and CIPD is affected by depressive symptoms.
1.4. Aims and hypotheses
The current study aimed to examine the effect of CM on CIPD in adults, taking subtypes of CM into account. In addition, we aimed to investigate the effect of depressive symptomatology on the relationship between CM and CIPD. Building on prior research demonstrating a larger CIPD in adults with experiences of CM (Maier et al., Citation2020) and in adults with depressive symptoms (Ponizovsky et al., Citation2013; Welsch et al., Citation2020), we hypothesized that adults with a history of CM, both with and without depressive symptoms, prefer a larger CIPD. Furthermore, we explored whether all subtypes of CM are linked to CIPD. As CM is associated with revictimization across the life-span (Charak et al., Citation2020; Goemans, Viding, & McCrory, Citation2021), we additionally performed secondary analyses to explore whether total number of experienced traumatic events positively correlate with CIPD.
2. Methods
2.1. Participants
CIPD of 90 adults with and 59 adults without self-reported history of CM was assessed between 2017 and 2019 as part of a larger project on socio-emotional consequences of CM. Thus, exclusion criteria (life-time psychotic symptoms, substance or alcohol abuse during past 12 months, insufficiently corrected vision, medical conditions and medication intake affecting psychophysiological measurements (e.g. antiepileptics, antipsychotics or benzodiazepines), pregnancy, acute suicidality) were based on this larger study. Research has demonstrated more pronounced long-term effects of accumulating rather than isolated traumatic childhood experiences (e.g. more pronounced externalizing behaviour and emotion dysregulation (Jonson-Reid, Kohl, & Drake, Citation2012; Warmingham, Handley, Rogosch, Manly, & Cicchetti, Citation2019)). Therefore, and given that regulation of CIPD is a developmental task during childhood (Aiello & De Carlo Aiello, Citation1974), we assumed that chronic, rather than isolated experiences of CM would be related to the hypothesized alterations in CIPD. To be included in the CM group, participants thus had to report chronic forms of CM (see Methods and Procedures section).
The final sample considered for data analysis consisted of 141 German-speaking participants (76% female, mean age 27 ± .77, 81% with a high school degree or higher). shows detailed sample characteristics. Since the groups differed in age and sex, effects of age and sex on CIPD were explored. Neither age nor sex had a significant effect on CIPD (see Supplement). Of all included participants, 18 (13%) reported current use of other psychotropic medication (e.g. Selective Serotonin Reuptake Inhibitors) and 45 (31.47%) were currently diagnosed with one or more mental disorders.
Table 1. Demographic and psychometric characteristics.
2.2. Methods and procedures
The study was approved by the Cantonal Ethics Committee of Zurich (identification number: 2017-00713). All participants gave written informed consent. During visit 1, CM, additional trauma history, current depressive symptoms, and other mental disorders were assessed by the German version of the Childhood Trauma Questionnaire (CTQ), short version (Bader, Hänny, Schäfer, Neuckel, & Kuhl, Citation2009), the trauma checklist of the Posttraumatic Diagnostic Scale (PDS; Ehlers, Steil, Winter, & Foa, Citation1996), the Beck Depression Inventory (BDI; Beck, Steer, & Brown, Citation1996; Hautzinger, Citation1994), and the diagnostic interview for mental disorders (DIPS; Margraf, Cwik, Pflug, & Schneider, Citation2017; Margraf, Cwik, Suppiger, & Schneider, Citation2018). If the maltreatment cut-off score for one of the maltreatment subscales of the CTQ (Bernstein et al., Citation2003) was reached, participants were asked whether they had been exposed to this specific type of abuse so often that they had expected it to happen again. If participants answered with no for all of the subscales on which they had reached the cut-off score, they were excluded from the analysis as they were considered to have been exposed to isolated events.
During visit 2, CIPD (measured in cm from participant’s to experimenter’s toes) was assessed using the stop-distance method (Hayduk, Citation1978, Citation1983; Kaitz et al., Citation2004). Prior research shows that, generally, CIPD towards males are larger than distances towards females (Uzzell & Horne, Citation2006; Vranic, Citation2003). Thus, to standardize and minimize the impact of gender of the approaching person on CIPD, participants were frontally approached by a female member of the current study team and asked to say stop once they started feeling slightly uncomfortable (distance 1, D1) and very uncomfortable (distance 2, D2) (Kaitz et al., Citation2004). The approaching member of the study team stopped walking either as soon as participants said stop (whereupon the CIPD was measured as the distance in cm between the participant and the approaching team member) or as soon as a distance of 10 cm was reached. In the latter case, participants were asked if they would have tolerated physical contact. If they answered yes, CIPD was set to 0 cm, otherwise to 10 cm. Participants were informed that the approaching female was a member of the study team but were not introduced to her until completion of the paradigm.
Eye-gaze is an important non-verbal behaviour associated with the regulation of CIPD (Bailenson, Blascovich, Beall, & Loomis, Citation2001, Citation2003) especially in individuals with high levels of social anxiety (Wieser, Pauli, Grosseibl, Molzow, & Mühlberger, Citation2010). It has been theorized that mutual eye-gaze increases CIPD to regulate the level of intimacy one feels comfortable with (Bailenson et al., Citation2001, Citation2003). Individuals with a history of CM often experience difficulties with intimacy (Davis et al., Citation2001; Vaillancourt-Morel et al., Citation2019) and anxiety (Gardner et al., Citation2019). To minimize the impact of these factors while standardizing conditions across participants, members of the study team were instructed to direct their gaze on the chin of participants. Furthermore, approaching members of the study team were instructed to walk with a speed of 15–20 cm per second.
2.3. Data analysis
Inspection of the data with histograms revealed extreme skews to the right in all variables of interest and the existence of extreme values. Transformations did not lead to approximate normal distributions. Thus, non-parametric analyses were carried out.
The sample was first divided into a CM and a control group, based on participants’ CTQ scores (Bader et al., Citation2009; Bernstein et al., Citation2003). According to the classification of Bernstein and colleagues (Bernstein et al., Citation2003), participants who reported at least low to moderate scores in one of the subscales of the CTQ (i.e. ≥10 for emotional neglect, ≥8 for physical neglect, ≥9 for emotional abuse, ≥8 for physical abuse and ≥6 for sexual abuse) were assigned to the CM group. Therefore, the maximum CTQ score for participants of the control group was 36. Additionally, all participants who scored low to moderate in one of the subscales of the CTQ were assigned to the respective subgroup. Four participants from the CM group reported having experienced an isolated event of physical or sexual abuse and were excluded from the analysis. Since subclinical forms of depression such as minor depression also have an impact on social functioning (Rodríguez, Nuevo, Chatterji, & Ayuso-Mateos, Citation2012; Wagner et al., Citation2000) and previous research on CIPD and depressive symptoms (Ponizovsky et al., Citation2013; Welsch et al., Citation2020) relied upon the BDI score (Beck et al., Citation1996), the CM group was further divided according to their BDI scores rather than relying on the diagnosis as assessed with the DIPS. Based on the absence (scores of 0–13) or presence (scores > 13) of depressive symptoms, the CM group was divided into 60 participants without (CM−) and 24 participants with depressive symptoms (CM+). Participants from the control group with a BDI < 14 were categorized as controls (n = 57).Footnote1
2.3.1. Impact of CM and depression on CIPD
Independent samples Kruskal–Wallis tests were conducted to examine group differences (controls, CM−, CM+) in D1 and D2. Significant main effects were followed up with Mann–Whitney U tests. Exact p values (1-tailed) were used. All p-values were Bonferroni–Holm (Holm, Citation1979) corrected. Effect sizes (Cohen’s d) and 95% confidence intervals (CI) were calculated.
2.3.2. Impact of CM subtypes and depression on CIPD
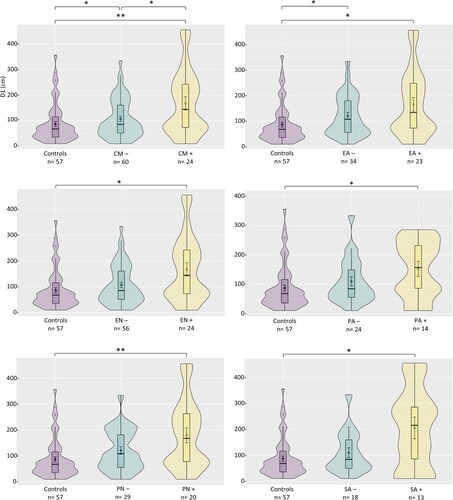
The CM group was further divided into the 5 subtypes of CM (Bader et al., Citation2009; Bernstein et al., Citation2003), with and without depressive symptoms (Beck et al., Citation1996). The n per subgroup are presented in . For each CM subtype, independent samples Kruskal–Wallis tests were conducted to assess group differences (controls, CM subtype −, CM subtype +) in D1 and D2. Significant main effects were followed up with Mann–Whitney U tests. Exact p values (2-tailed) were Bonferroni–Holm corrected within each subgroup analysis. Effect sizes (Cohen’s d) and 95% confidence intervals (CI) were calculated.
Figure 1. Data distribution of all groups on distance 1 (D1). Note. Black bars within box plots display medians. Rhombi within box plots represent means. Error bars represent the 95% confidence intervals. The shapes of the violins display the frequencies of the values. * p < .05. ** p < .01. Results for D2 were identical except for the EA− group (who did not differ significantly from controls on D2). CM = child maltreatment; EA = emotional abuse; EN = emotional neglect; PA = physical abuse; PN = physical neglect; SA = sexual abuse; − = without depressive symptoms; + = with depressive symptoms.
2.3.3. Impact of number of additional traumatic experiences on CIPD
As a secondary analysis, independent samples Kruskal–Wallis tests were used to explore whether the number of additional traumatic experiences (i.e. the number of traumatic experiences according to the PDS (Ehlers et al., Citation1996) excluding CM experiences) affect D1 and D2. Of our complete sample (controls and CM−/+), 91 individuals reported traumatic experiences (one trauma: n = 42; two or more traumas: n = 49). The Mdn of experienced traumas across control and CM− participants was 1, the Mdn across CM+ participants was 2, Max of experienced traumas: 6. With this lack of variance not allowing for dimensional analyses, a variable with three categories of traumatic experiences was created: (1) none, (2) one, (3) two or more. Exact p values (2-tailed) were obtained.
3. Results
3.1. Group differences in D1
Results showed that there were significant differences in D1 between the CM+ group (Mdn = 145 cm), the CM− group (Mdn = 86 cm), and the controls (Mdn = 68 cm), H(2) = 10.46, p = .005. Post-hoc tests showed that both CM groups had a greater D1 than controls, p = .028 (CM−), p = .005 (CM+). The CM+ group had a greater D1 than the CM− group (p = .047). shows the statistical values from all paired group comparisons.
Table 2. Group comparisons on D1 and D2.
For all five subtypes of CM, differences in D1 between the three groups were significant, H(2) = 10.26, p = .018 (emotional neglect); H(2) = 11.85, p = .015 (physical neglect); H(2) = 10.49, p = .020 (emotional abuse); H(2) = 6.99, p = .030 (sexual abuse); H(2) = 7.71, p = .042 (physical abuse). Post-hoc tests showed that, for all subtypes of CM, differences between the CM subtype groups with depressive symptoms vs. controls were significant, p = .003 (emotional neglect), p = .002 (physical neglect), p = .005 (emotional abuse), p = .015 (sexual abuse), p = .015 (physical abuse). Those with emotional abuse without depressive symptoms showed a greater D1 than controls (p = .040). Differences between all other subgroups were not significant (all p’s > .058) ()
3.2. Group differences in D2
Results showed that there were significant differences in D2 between the CM+ group (Mdn = 38.50 cm), the CM− group (Mdn = 20.00 cm), and the controls (Mdn = 10.00 cm), H(2) = 11.13, p = .004. Post-hoc tests showed that differences were significant between both CM groups and the controls, p = .028 (CM−), p = .002 (CM+). The CM+ group had a greater D2 than the CM− group (p = .039) ()
For all five subtypes of CM, differences in D2 between the three groups were significant, H(2) = 10.83, p = .010 (emotional neglect); H(2) = 12.18, p = .016 (physical neglect); H(2) = 9.83, p = .018 (emotional abuse); H(2) = 10.20, p = .014 (sexual abuse); H(2) = 8.05, p = .018 (physical abuse). Post-hoc tests showed that, for all five subtypes of CM, differences between the groups with depressive symptoms vs. controls were significant, p = .001 (emotional neglect), p = .001 (physical neglect), p = .003 (emotional abuse), p = .004 (sexual abuse), p = .010 (physical abuse). Differences between all other subgroups were not significant (all p’s > .066) ()
3.2.1. Impact of number of traumatic experiences on CIPD
Results showed that there were no significant differences between the three groups (no traumatic experience, one traumatic experience, two or more traumatic experiences), H(2) = .30, p = .862 (D1); H(2) = 1.12, p = .571 (D2).
4. Discussion
Our results demonstrate that adults with a history of CM with and without depressive symptoms show a greater CIPD than adults without a history of CM (and without depressive symptoms). This effect was particularly pronounced for individuals with CM with depressive symptoms. Our results also demonstrate that all subtypes of CM modulate CIPD, yet this finding was restricted to individuals with CM with depressive symptoms. In individuals with CM without depressive symptoms, CIPD was only greater for those who had experienced emotional abuse (and only for D1). The number of additional trauma experiences (other than CM) did not affect CIPD. This study thus highlights that the tolerance of physical closeness is particularly impaired when individuals report both experiences of CM and current depressive symptoms.
A larger CIPD in adults with a history of CM might serve a protective function resulting out of hypervigilance towards threat, involving (hyper)activity of the amygdala (Gerin et al., Citation2019; McCrory et al., Citation2011). As suggested by Maier and colleagues (Maier et al., Citation2020), abnormal neural responses to social signals (e.g. facial expressions; McCrory et al., Citation2013) and alterations in the perception of touch (Maier et al., Citation2020) in individuals with CM might be based on learning experiences and result in discomfort in situations of physical proximity and, consequently, a larger CIPD. However, the mechanisms through which subtypes of CM lead to this discomfort might be different depending upon the subtype of CM. According to McLaughlin and colleagues (McLaughlin et al., Citation2014), experiences of threat (e.g. sexual and physical abuse) are distinct from experiences of deprivation (e.g. emotional and physical neglect). Through a developmental perspective, individuals who experienced abuse grew up in an environment where their physical and/or emotional boundaries were repeatedly violated. They might thus have learned to associate physical closeness with danger, resulting in larger CIPD. On the other hand, individuals who experienced neglect might not feel comfortable with (too much) physical closeness – an experience that they are not familiar with and that might trigger fears of being hurt as well as feelings of shame, related to perceptions of being inferior or unlovable (Pilkington, Bishop, & Younan, Citation2021). Even though in our study, only emotional abuse affected CIPD independently of current depressive symptoms, it would be important to assess this relationship in longitudinal studies, potentially leading to the development of different therapeutical approaches depending upon the (predominant) subtype of CM.
Negative self-thoughts are a core feature of depressive symptoms. In line with our finding of largest CIPD in individuals with current symptoms of depression, it has been shown that in individuals with a diagnosis of adjustment disorder with depressed mood, the BDI items referring to self-dislike and social withdrawal are associated with larger CIPD towards strangers and significant others (Ponizovsky et al., Citation2013). These depressive symptoms may protect individuals from potential danger of rejection by unknown others (Allen & Badcock, Citation2003). Heightened rejection sensitivity is present in both depressive disorders and in adults with a history of CM (Luterek, Harb, Heimberg, & Marx, Citation2004; Nenov-Matt et al., Citation2020). Our findings might therefore reflect the degree to which interpersonal contact is avoided to prevent social rejection. Future research should investigate the impact of rejection sensitivity on the relationship between depression, CM and CIPD.
Lastly, psychological theories such as the self-trauma model (Briere, Citation2002) and recent research findings suggest that adult survivors of CM may mistrust their romantic partners and believe that others are intrusive, rejecting or unavailable (Briere, Citation2002; Hepp et al., Citation2021; McKay et al., Citation2021; Vaillancourt-Morel et al., Citation2019). Together with other frequent consequences of CM (e.g. fear of intimacy (Davis et al., Citation2001)) and a tendency to become hyperaware of potentially threating stimuli (McCrory et al., Citation2011), these negative perceptions of interaction partners might trigger avoidance behaviour and, ultimately, result in larger CIPD as a way to protect oneself (de Haan, Smit, Van der Stigchel, & Dijkerman, Citation2016). Further studies should explore whether these interpersonal problems and negative beliefs about others relate to CIPD and whether they are particularly pronounced in those who prefer a larger CIPD. It is also crucial to disentangle whether CIPD mainly serves as a behavioural correlate or directly contributes to the development of these interpersonal problems. For instance, an individual with a larger CIPD might feel overwhelmed once others unconsciously overstep their personal boundaries and react with physical and emotional fear reactions (Åhs et al., Citation2015; Hayduk, Citation1978) in distances which others (without trauma exposure) would still consider appropriate. Affected individuals might prefer to avoid interpersonal situations and socially withdraw to navigate this distress. Likewise, their interaction partners could perceive them in a negative way (e.g. due to a lack of positive social signals; Hepp, Störkel, Kieslich, Schmahl, & Niedtfeld, Citation2018) and decide to limit further contact. Both possibilities might negatively impact relationships and make it difficult for individuals with experiences of CM to establish additional social bonds.
4.1. Limitations and conclusions
The group sizes in the current study varied as a result of the prevalence of experiences of CM and current depressive symptoms. In line with the prevalence of depression in individuals with CM (Braithwaite, O’Connor, Degli-Esposti, Luke, & Bowes, Citation2017; Humphreys et al., Citation2020), the CM− group was larger than the CM+ group. Future research should aim to include depressive symptoms as specific criterion to achieve a larger sample size for this group.
The sexual abuse subgroup was small. However, this is a reflection of the prevalence of sexual abuse in the population (12.7% for sexual abuse and 36.3% for emotional abuse; Stoltenborgh et al., Citation2015). In the current sample, 67.8% participants reported emotional abuse and 36.9% sexual abuse. Future research should aim to specifically recruit individuals with sexual abuse to achieve a larger sample size for this group to further disentangle the specific effects of sexual abuse on the development of CIPD.
It should be noted that subtypes of CM frequently co-occur (e.g. Vachon, Krueger, Rogosch, & Cicchetti, Citation2015). Our sample consisted of adults with a history of multiple subtypes of CM (i.e. 76% of the two CM groups reported experiences of more than one subtype). This overlap in experiences makes it difficult to draw conclusions about the effects of specific CM experiences on CIPD. In line with previous research (e.g. Warmingham et al., Citation2019; Ziobrowski et al., Citation2020) future studies could address this issue through person-centered approaches such as latent class analysis that enable to catch the specific patterns of CM and investigate their impact on CIPD.
While effects of depressive symptoms on CIPD have been documented before (e.g. Ponizovsky et al., Citation2013), differences in CIPD between the CM− and the CM+ group might instead be caused by more severe experiences of CM (i.e. we found higher CTQ total scores in the CM+ than in the CM− group, see Table S3, Supplement). However, self-report measures such as the CTQ can be affected by depressive recall bias, leading to the question of whether the CM+ group effectively experienced more severe CM than the CM− group.
While our in-person approach allows for a high ecological validity, participants were aware that their preferred distance would be measured, which may have affected their behaviour, given that interpersonal distance is usually regulated unconsciously. It should also be noted that participants were aware that the approaching person was a member of the study team, and that the experimenter was present during the whole task. Therefore, participants might have felt safer in their personal space compared to a real first encounter. Individuals with experiences of CM thus prefer larger CIPD even in situations where they know that they are safe. Nevertheless, studies using real-life settings where participants are blind to study purposes are needed to replicate the current findings and to explore whether the need for larger CIPD might be more pronounced when encountering a stranger in everyday life.
Further, we assessed preferred distance towards a female stranger and the majority of our sample was female, limiting generalizability of our findings to all genders. Since prior research points towards differences in CIPD depending upon the gender of the approaching person (Uzzell & Horne, Citation2006; Vranic, Citation2003) future research should explore potential effects of experimenter sex on participants’ CIPD. Additionally, participants were approached by one of twenty different study members and thus individual differences of the approaching female might have impacted the results. To limit this influence in future studies, it would be desirable to keep the number of different interaction partners as low as possible.
Despite these limitations, our findings may have important implications for the daily-life and for social functioning and well-being of affected individuals. Unwanted intrusion by strangers into one’s personal space causes discomfort (Hayduk, Citation1978) and likely leads to physical fear reactions (Åhs et al., Citation2015). Our findings might therefore explain the occurrence of initial panic attacks in situations where strangers are standing close and it is difficult to escape (e.g. elevators, public transport). When others are getting close, individuals with a larger CIPD may show nonverbal signals associated with feelings of being uncomfortable (e.g. dismissive facial expressions or body postures). Some individuals might also feel triggered and reminded of their trauma, leading to emotional distress and affective responses such as shame and anger (Kleim, Graham, Bryant, & Ehlers, Citation2013). These signals may impair establishing contacts, reduce positive social signals and prohibit social interactions, which are important for well-being. Affected individuals might thus benefit from learning on how to feel safe within their personal space, which may affect how others perceive them.
In sum, our results provide further evidence that CM affects preferences of physical closeness and distance. Future research should aim to disentangle the underlying processes of how increased CIPD develops, to aid our understanding of interpersonal problems in those affected by CM and to, ultimately, develop corresponding interventions. Future research could investigate whether individuals with CM also prefer larger distances to close others such as partners, which could be related to difficulties in close relationships (Colman & Widom, Citation2004). Additionally, future research should aim to consider the influence of culture (Sorokowska et al., Citation2017) on preferences for interpersonal distance, e.g. through cross-cultural collaborations such as the Global Collaboration on Traumatic Stress (Schnyder et al., Citation2017; Olff et al., Citationn.d.).
Supplemental Material
Download MS Word (28.1 KB)Acknowledgements
This study was approved by the cantonal ethics committee Zurich (identification number: 2017-00713) and was funded by the EMDO foundation (grant to Monique Pfaltz and Tanja Wingenbach).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, [MCP]. The data are not publicly available due to information that could compromise the privacy of research participants.
Additional information
Funding
Notes
1 Two participants from the control group scored above 13 on the BDI and were exempt from the analyses.
References
- Åhs, F., Dunsmoor, J. E., Zielinski, D., & LaBar, K. S. (2015). Spatial proximity amplifies valence in emotional memory and defensive approach-avoidance. Neuropsychologia, 70, 476–485. doi:10.1016/j.neuropsychologia.2014.12.018
- Aiello, J. R., & De Carlo Aiello, T. (1974). The development of personal space: Proxemic behavior of children 6 through 16. Human Ecology, 2, 177–189. doi:10.1007/BF01531420
- Allen, N. B., & Badcock, P. B. T. (2003). The social risk hypothesis of depressed mood: Evolutionary, psychosocial, and neurobiological perspectives. Psychological Bulletin, 129, 887–913. doi:10.1037/0033-2909.129.6.887
- Anthonysamy, A., & Zimmer-Gembeck, M. J. (2007). Peer status and behaviors of maltreated children and their classmates in the early years of school. Child Abuse & Neglect, 31, 971–991. doi:10.1016/j.chiabu.2007.04.004
- Bader, K., Hänny, C., Schäfer, V., Neuckel, A., & Kuhl, C. (2009). Childhood Trauma Questionnaire – Psychometrische Eigenschaften einer deutschsprachigen version. Zeitschrift für Klinische Psychologie und Psychotherapie, 38, 223–230. doi:10.1026/1616-3443.38.4.223
- Bailenson, J. N., Blascovich, J., Beall, A. C., & Loomis, J. M. (2001). Equilibrium theory revisited: Mutual gaze and personal space in virtual environments. Presence: Teleoperators and Virtual Environments, 10, 583–598. doi:10.1162/105474601753272844
- Bailenson, J. N., Blascovich, J., Beall, A. C., & Loomis, J. M. (2003). Interpersonal distance in immersive virtual environments. Personality and Social Psychology Bulletin, 29, 819–833. doi:10.1177/0146167203029007002
- Barzeva, S. A., Richards, J. S., Meeus, W. H. J., & Oldehinkel, A. J. (2021). Social withdrawal and romantic relationships: A longitudinal study in early adulthood. Journal of Youth and Adolescence, 50, 1766–1781. doi:10.1007/s10964-021-01469-1
- Beck, A. T., Steer, R. A., & Brown, G. (1996). Manual for the Beck depression inventory–II. San Antonio: Psychological Corporation.
- Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., & Ahluvalia, T. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27, 169–190. doi:10.1016/S0145-2134(02)00541-0
- Bigras, N., Godbout, N., Hébert, M., Runtz, M., & Daspe, M-È. (2015). Identity and relatedness as mediators between child emotional abuse and adult couple adjustment in women. Child Abuse & Neglect, 50, 85–93. doi:10.1016/j.chiabu.2015.07.009
- Bogovic, A., Mihanovic, M., Jokic-Begic, N., & Svagelj, A. (2014). Personal space of male war veterans with posttraumatic stress disorder. Environment and Behavior, 46, 929–945. doi:10.1177/0013916513477653
- Braithwaite, E. C., O’Connor, R. M., Degli-Esposti, M., Luke, N., & Bowes, L. (2017). Modifiable predictors of depression following childhood maltreatment: A systematic review and meta-analysis. Translational Psychiatry, 7, e1162–e1162. doi:10.1038/tp.2017.140
- Briere, J. (2002). Treating adult survivors of severe childhood abuse and neglect: Further development of an integrative model. APSAC Handb (pp. 175–203). Child Maltreatment 2nd Ed, Thousand Oaks, CA: Sage Publications, Inc.
- Busby, D. M., Walker, E. C., & Holman, T. B. (2011). The association of childhood trauma with perceptions of self and the partner in adult romantic relationships. Personal Relationships, 18, 547–561. doi:10.1111/j.1475-6811.2010.01316.x
- Charak, R., Vang, M. L., Shevlin, M., Ben-Ezra, M., Karatzias, T., & Hyland, P. (2020). Lifetime interpersonal victimization profiles and mental health problems in a nationally representative panel of trauma-exposed adults from the United Kingdom. Journal of Traumatic Stress, 33, 654–664. doi:10.1002/jts.22527
- Cole, S., Balcetis, E., & Dunning, D. (2013). Affective signals of threat increase perceived proximity. Psychological Science, 24, 34–40. doi:10.1177/0956797612446953
- Colman, R. A., & Widom, C. S. (2004). Childhood abuse and neglect and adult intimate relationships: A prospective study. Child Abuse & Neglect, 28, 1133–1151. doi:10.1016/j.chiabu.2004.02.005
- Davis, J. L., Petretic-Jackson, P. A., & Ting, L. (2001). Intimacy dysfunction and trauma symptomatology: Long-term correlates of different types of child abuse. Journal of Traumatic Stress, 14, 63–79. doi:10.1023/A:1007835531614
- de Haan, A. M., Smit, M., Van der Stigchel, S., & Dijkerman, H. C. (2016). Approaching threat modulates visuotactile interactions in peripersonal space. Experimental Brain Research, 234, 1875–1884. doi:10.1007/s00221-016-4571-2
- Di Cosmo, G., Costantini, M., Salone, A., Martinotti, G., Di Iorio, G., & Di Giannantonio, M. (2018). Peripersonal space boundary in schizotypy and schizophrenia. Schizophrenia Research, 197, 589–590. doi:10.1016/j.schres.2017.12.003
- Ehlers, A., Steil, R., Winter, H., & Foa, E. B. (1996). Deutschsprachige Übersetzung der Posttraumatic Diagnostic Scale von Foa (1995) (Unveröffentlichtes Manuskript). Department of Psychiatry, Warneford Hospital, Oxford.
- Gardner, M. J., Thomas, H. J., & Erskine, H. E. (2019). The association between five forms of child maltreatment and depressive and anxiety disorders: A systematic review and meta-analysis. Child Abuse & Neglect, 96, 104082. doi:10.1016/j.chiabu.2019.104082
- Gerin, M. I., Viding, E., Pingault, J.-B., Puetz, V. B., Knodt, A. R., & Radtke, S. R. (2019). Heightened amygdala reactivity and increased stress generation predict internalizing symptoms in adults following childhood maltreatment. Journal of Child Psychology and Psychiatry, 60, 752–761. doi:10.1111/jcpp.13041
- Goemans, A., Viding, E., & McCrory, E. (2021). Child maltreatment, peer victimization, and mental health: Neurocognitive perspectives on the cycle of victimization. Trauma, Violence & Abuse, doi:10.1177/15248380211036393
- Hautzinger, M. (1994). Beck-Depressions-Inventar (BDI) Bearbeitung der deutschen Ausgabe. Testhandbuch Bern Gött Tor Seattle.
- Hayduk, L. A. (1978). Personal space: An evaluative and orienting overview. Psychological Bulletin, 85, 117–134. doi:10.1037/0033-2909.85.1.117
- Hayduk, L. A. (1983). Personal space: Where we now stand. Psychological Bulletin, 94, 293–335. doi:10.1037/0033-2909.94.2.293
- Hepp, J., Schmitz, S. E., Urbild, J., Zauner, K., & Niedtfeld, I. (2021). Childhood maltreatment is associated with distrust and negatively biased emotion processing. Borderline Personality Disorder and Emotion Dysregulation, 8, 5. doi:10.1186/s40479-020-00143-5
- Hepp, J., Störkel, L. M., Kieslich, P. J., Schmahl, C., & Niedtfeld, I. (2018). Negative evaluation of individuals with borderline personality disorder at zero acquaintance. Behaviour Research and Therapy, 111, 84–91. doi:10.1016/j.brat.2018.09.009
- Hildyard, K. L., & Wolfe, D. A. (2002). Child neglect: Developmental issues and outcomes. Child Abuse & Neglect, 26, 679–695. doi:10.1016/S0145-2134(02)00341-1
- Holm, S. (1979). A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics, 6, 65–70.
- Holz, N. E., Tost, H., & Meyer-Lindenberg, A. (2020). Resilience and the brain: A key role for regulatory circuits linked to social stress and support. Molecular Psychiatry, 25, 379–396. doi:10.1038/s41380-019-0551-9
- Humphreys, K. L., LeMoult, J., Wear, J. G., Piersiak, H. A., & Gotlib, I. H. (2020). Child maltreatment and depression: A meta-analysis of studies using the Childhood Trauma Questionnaire. Child Abuse & Neglect, 102, 104361. doi:10.1016/j.chiabu.2020.104361
- Iffland, B., & Neuner, F. (2020). Varying cognitive scars – Differential associations between types of childhood maltreatment and facial emotion processing. Frontiers in Psychology, 11, 732. doi:10.3389/fpsyg.2020.00732
- Jonson-Reid, M., Kohl, P. L., & Drake, B. (2012). Child and adult outcomes of chronic child maltreatment. Pediatrics, 129, 839–845. doi:10.1542/peds.2011-2529
- Kaitz, M., Bar-Haim, Y., Lehrer, M., & Grossman, E. (2004). Adult attachment style and interpersonal distance. Attachment & Human Development, 6, 285–304. doi:10.1080/14616730412331281520
- Kleim, B., Graham, B., Bryant, R. A., & Ehlers, A. (2013). Capturing intrusive re-experiencing in trauma survivors’ daily lives using ecological momentary assessment. Journal of Abnormal Psychology, 122, 998–1009. doi:10.1037/a0034957
- Loos, M. E., & Alexander, P. C. (1997). Differential effects associated with self-reported histories of abuse and neglect in a college sample. Journal of Interpersonal Violence, 12, 340–360. doi:10.1177/088626097012003002
- Luterek, J. A., Harb, G. C., Heimberg, R. G., & Marx, B. P. (2004). Interpersonal rejection sensitivity in childhood sexual abuse survivors: Mediator of depressive symptoms and anger suppression. Journal of Interpersonal Violence, 19, 90–107. doi:10.1177/0886260503259052
- Maier, A., Gieling, C., Heinen-Ludwig, L., Stefan, V., Schultz, J., & Güntürkün, O. (2020). Association of childhood maltreatment with interpersonal distance and social touch preferences in adulthood. American Journal of Psychiatry, 177, 37–46. doi:10.1176/appi.ajp.2019.19020212
- Margraf, J., Cwik, J. C., Pflug, V., & Schneider, S. (2017). Strukturierte klinische Interviews zur Erfassung psychischer Störungen über die Lebensspanne: Gütekriterien und Weiterentwicklungen der DIPS-Verfahren. Zeitschrift für Klinische Psychologie und Psychotherapie, 46, 176–186. doi:10.1026/1616-3443/a000430
- Margraf, J., Cwik, J. C., Suppiger, A., & Schneider, S. (2017). DIPS open access: Diagnostic interview for mental disorders [DIPS Open Access: Diagnostisches Interview bei psychischen Störungen]. Bochum: Mental Health Research and Treament Center, Ruhr-Universität Bochum. doi:10.13154/rub.100.89
- McCrory, E. J., Brito, S. A. D., Sebastian, C. L., Mechelli, A., Bird, G., & Kelly, P. A. (2011). Heightened neural reactivity to threat in child victims of family violence. Current Biology, 21, R947–R948. doi:10.1016/j.cub.2011.10.015
- McCrory, E. J., De Brito, S. A., Kelly, P. A., Bird, G., Sebastian, C. L., & Mechelli, A. (2013). Amygdala activation in maltreated children during pre-attentive emotional processing. British Journal of Psychiatry, 202, 269–276. doi:10.1192/bjp.bp.112.116624
- McCrory, E., Ogle, J. R., Gerin, M. I., & Viding, E. (2019). Neurocognitive adaptation and mental health vulnerability following maltreatment: The role of social functioning. Child Maltreatment, 24, 435–451. doi:10.1177/1077559519830524
- McKay, M. T., Cannon, M., Chambers, D., Conroy, R. M., Coughlan, H., & Dodd, P. (2021). Childhood trauma and adult mental disorder: A systematic review and meta-analysis of longitudinal cohort studies. Acta Psychiatrica Scandinavica, 143, 189–205. doi:10.1111/acps.13268
- McLaughlin, K. A., Sheridan, M. A., & Lambert, H. K. (2014). Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neuroscience & Biobehavioral Reviews, 47, 578–591. doi:10.1016/j.neubiorev.2014.10.012
- Nenov-Matt, T., Barton, B. B., Dewald-Kaufmann, J., Goerigk, S., Rek, S., & Zentz, K. (2020). Loneliness, social isolation and their difference: A cross-diagnostic study in persistent depressive disorder and borderline personality disorder. Frontiers in Psychiatry, 11. doi:10.3389/fpsyt.2020.608476
- Olff, M., Bakker, A., Frewen, P., Aakvaag, H., Ajdukovic, D., & Brewer, D. (n.d.). Screening for consequences of trauma – An update on the global collaboration on traumatic stress. European Journal of Psychotraumatology, 11, 1752504. doi:10.1080/20008198.2020.1752504
- Perry, A., Rubinsten, O., Peled, L., & Shamay-Tsoory, S. G. (2013). Don’t stand so close to me: A behavioral and ERP study of preferred interpersonal distance. NeuroImage, 83, 761–769. doi:10.1016/j.neuroimage.2013.07.042
- Pfaltz, M., Halligan, S., Haim-Nachum, S., Sopp, R., Åhs, F., Bachem, R., & Seedat, S. (2021). Social functioning in individuals affected by childhood maltreatment: Establishing a research agenda to inform interventions. Psychotherapy and Psychosomatics. doi:10.31219/osf.io/7hsek
- Pilkington, P. D., Bishop, A., & Younan, R. (2021). Adverse childhood experiences and early maladaptive schemas in adulthood: A systematic review and meta-analysis. Clinical Psychology & Psychotherapy, 28, 569–584. doi:10.1002/cpp.2533
- Ponizovsky, A. M., Finkelstein, I., Poliakova, I., Mostovoy, D., Goldberger, N., & Rosca, P. (2013). Interpersonal distances, coping strategies and psychopathology in patients with depression and schizophrenia. World Journal of Psychiatry, 3, 74–84. doi:10.5498/wjp.v3.i3.74
- Rodríguez, M. R., Nuevo, R., Chatterji, S., & Ayuso-Mateos, J. L. (2012). Definitions and factors associated with subthreshold depressive conditions: A systematic review. BMC Psychiatry, 12, 181. doi:10.1186/1471-244X-12-181
- Schnyder, U., Schäfer, I., Aakvaag, H. F., Ajdukovic, D., Bakker, A., & Bisson, J. I. (2017). The global collaboration on traumatic stress. European Journal of Psychotraumatology, 8, 1403257. doi:10.1080/20008198.2017.1403257
- Sorokowska, A., Sorokowski, P., Hilpert, P., Cantarero, K., Frackowiak, T., & Ahmadi, K. (2017). Preferred interpersonal distances: A global comparison. Journal of Cross-Cultural Psychology, 48, 577–592. doi:10.1177/0022022117698039
- Stoltenborgh, M., Bakermans-Kranenburg, M. J., Alink, L. R. A., & Ijzendoorn, M. H. (2015). The prevalence of child maltreatment across the globe: Review of a series of meta-analyses. Child Abuse Review, 24, 37–50. doi:10.1002/car.2353
- Teicher, M. H., & Samson, J. A. (2016). Annual research review: Enduring neurobiological effects of childhood abuse and neglect. Journal of Child Psychology and Psychiatry, 57, 241–266. doi:10.1111/jcpp.12507
- Thelen, M. H., Vander Wal, J. S., Thomas, A. M., & Harmon, R. (2000). Fear of intimacy among dating couples. Behavior Modification, 24, 223–240. doi:10.1177/0145445500242004
- Thornberry, T. P., Henry, K. L., Smith, C., Ireland, T. O., Greenman, S. J., & Lee, R. D. (2013). Breaking the cycle of maltreatment: The role of safe, stable, and nurturing relationships. Journal of Adolescent Health, 53, S25–S31. doi:10.1016/j.jadohealth.2013.04.019
- Uzzell, D., & Horne, N. (2006). The influence of biological sex, sexuality and gender role on interpersonal distance. British Journal of Social Psychology, 45, 579–597. doi:10.1348/014466605X58384
- Vachon, D. D., Krueger, R. F., Rogosch, F. A., & Cicchetti, D. (2015). Different forms of child maltreatment have comparable consequences among children from low-income families. JAMA Psychiatry, 72, 1135–1142. doi:10.1001/jamapsychiatry.2015.1792
- Vaillancourt-Morel, M.-P., Rellini, A. H., Godbout, N., Sabourin, S., & Bergeron, S. (2019). Intimacy mediates the relation between maltreatment in childhood and sexual and relationship satisfaction in adulthood: A dyadic longitudinal analysis. Archives of Sexual Behavior, 48, 803–814. doi:10.1007/s10508-018-1309-1
- Vranceanu, A.-M., Hobfoll, S. E., & Johnson, R. J. (2007). Child multi-type maltreatment and associated depression and PTSD symptoms: The role of social support and stress. Child Abuse & Neglect, 31, 71–84. doi:10.1016/j.chiabu.2006.04.010
- Vranic, A. (2003). Personal space in physically abused children. Environment and Behavior, 35, 550–565. doi:10.1177/0013916503035004006
- Wagner, H. R., Burns, B. J., Broadhead, W. E., Yarnall, K. S., Sigmon, A., & Gaynes, B. N. (2000). Minor depression in family practice: Functional morbidity, co-morbidity, service utilization and outcomes. Psychological Medicine, 30, 1377–1390. doi:10.1017/s0033291799002998
- Warmingham, J. M., Handley, E. D., Rogosch, F. A., Manly, J. T., & Cicchetti, D. (2019). Identifying maltreatment subgroups with patterns of maltreatment subtype and chronicity: A latent class analysis approach. Child Abuse & Neglect, 87, 28–39. doi:10.1016/j.chiabu.2018.08.013
- Welsch, R., Hecht, H., Kolar, D. R., Witthöft, M., & Legenbauer, T. (2020). Body image avoidance affects interpersonal distance perception: A virtual environment experiment. European Eating Disorders Review, 28, 282–295. doi:10.1002/erv.2715
- Whisman, M. A. (2014). Dyadic perspectives on trauma and marital quality. Psychological Trauma: Theory, Research, Practice, and Policy, 6, 207–215. doi:10.1037/a0036143
- Wieser, M. J., Pauli, P., Grosseibl, M., Molzow, I., & Mühlberger, A. (2010). Virtual social interactions in social anxiety–the impact of sex, gaze, and interpersonal distance. Cyberpsychology, Behavior, and Social Networking, 13, 547–554. doi:10.1089/cyber.2009.0432
- Zamir, O. (2021). Childhood maltreatment and relationship quality: A review of type of abuse and mediating and protective factors. Trauma, Violence & Abuse, doi:10.1177/1524838021998319
- Ziobrowski, H. N., Buka, S. L., Austin, S. B., Sullivan, A. J., Horton, N. J., & Simone, M. (2020). Using latent class analysis to empirically classify maltreatment according to the developmental timing, duration, and co-occurrence of abuse types. Child Abuse & Neglect, 107, 104574. doi:10.1016/j.chiabu.2020.104574
