ABSTRACT
Background:
Despite the high prevalence of mental illness in forcibly displaced people, their utilization of mental health services is low. Major barriers to seeking mental health services include mental health self-stigma. To address this issue, the psychoeducational short film ‘Coping with Flight and Trauma’ was developed as a brief online intervention.
Objective:
The present study aims to evaluate the feasibility and acceptance of the newly developed 10 min film, and to assess changes in self-stigma and help seeking.
Method:
The evaluation of the film was conducted using a mixed-methods design with an online survey including the Self-Stigma of Mental Illness Scale, help seeking, and mental health variables at baseline, postintervention, and 3 month follow-up, in addition to telephone interviews postintervention with a randomly selected volunteer subsample.
Results:
A total of 134 participants with a forced displacement history within the past 8 years took part in the study, of whom 66% scored as having probable post-traumatic stress disorder (PTSD), depression, and/or anxiety. The results revealed emotional, cognitive, and behavioural changes postintervention. Directly after watching the film, participants reported reduced self-stigma and increased openness towards accessing mental health services. At follow-up, precisely 3.8 months later, these changes were no longer significant, yet 11% of participants reported having started psychotherapy since watching the film. Probable PTSD was associated with higher self-stigma at all three time-points. The majority (90%) would recommend watching the film to other forcibly displaced people.
Conclusions:
Self-stigma was shown to be a robust and persistent issue, which tends to be underestimated by individuals not affected by mental illness. Low-threshold psychoeducational online interventions may be a promising tool to reduce barriers to accessing mental health services for forcibly displaced people, e.g. by being implemented in stepped-care models.
HIGHLIGHTS
Mental health self-stigma was shown to be a persistent and underestimated burden in forcibly displaced people.
Psychoeducational online interventions are promising for addressing the burden of self-stigma and reducing barriers to seeking mental health services.
Antecedentes: A pesar de la alta prevalencia de enfermedades mentales en las personas desplazadas por la fuerza, la utilización que hacen de los servicios de salud mental es baja. Las principales barreras en la búsqueda de servicios de salud mental incluyen el autoestigma en salud mental. Para abordar este tema, se desarrolló el cortometraje psicoeducativo ‘Afrontando la huida y el trauma’ como una breve intervención en línea.Objetivo: El presente estudio pretende evaluar la viabilidad y la aceptación del nuevo cortometraje de 10 minutos con personas desplazadas por la fuerza y evaluar los cambios en el autoestigma y la búsqueda de ayuda.Método: La evaluación de la película se llevó a cabo mediante un diseño de métodos mixtos con una encuesta en línea que incluía la Escala de Autoestigma sobre la Enfermedad Mental, la búsqueda de ayuda y las variables de salud mental al inicio, después de la intervención y a los 3 meses de seguimiento, además de entrevistas telefónicas individuales cualitativas después de la intervención con una submuestra de voluntarios seleccionados al azar.Resultados: N = 134 participantes con una historia de desplazamiento forzado en los últimos ocho años tomaron parte en el estudio, de los cuales el 66% puntuó como probable trastorno de estrés postraumático (TEPT), depresión y/o ansiedad. Los resultados revelaron cambios emocionales, cognitivos y conductuales tras la intervención. Inmediatamente después de ver la película, los participantes informaron de una reducción del autoestigma y una mayor apertura para acceder a los servicios de salud mental. En el seguimiento, precisamente 3,8 meses después, estos cambios ya no eran significativos, pero el 11% de los participantes declararon haber iniciado una psicoterapia desde que vieron la película. El probable TEPT se asoció con un mayor autoestigma en las tres mediciones. La mayoría (90%) recomendaría ver la película a otras personas desplazadas por la fuerza.Conclusiones: El autoestigma demostró ser un fuerte problema y persistente que tiende a ser subestimado por los individuos no afectados por la enfermedad mental. Las intervenciones psicoeducativas en línea de bajo umbral podrían ser una herramienta prometedora para reducir las barreras de acceso a los servicios de salud mental para las personas desplazadas por la fuerza, por ejemplo, mediante su aplicación en modelos de atención escalonada.
背景:尽管被迫流离失所者的精神障碍患病率很高,他们对心理健康服务的利用率很低。寻求心理健康服务的主要障碍包括心理健康自我污名。为了解决这个问题,心理教育短片“应对逃离和创伤”被开发为一个简短的在线干预。
目的:本研究旨在评估新开发的有关被迫流离失所者 10 分钟电影的可行性和接受度,并评估自我污名和求助的变化。
方法:使用混合方法设计和在线调查对影片进行评估,包括在基线、干预后和 3 个月随访时的精神疾病自我污名量表、求助和心理健康变量,以及对随机选择的志愿者子样本进行干预后的定性个人电话采访。
结果:134 名在过去 8 年内有被迫流离失所史的参与者参加了本研究,其中 66% 的参与者被评分为可能患有创伤后应激障碍 (PTSD)、抑郁和/或焦虑。结果揭示了干预后的情绪、认知和行为变化。一看完电影后,参与者报告了降低的自我污名和增高的对获得心理健康服务的开放性。在精确的到3.8 个月后的随访中,这些变化不再显著,但 11% 的参与者报告说自从观看电影后就开始了心理治疗。在全部 3 次测量中,可能的 PTSD 都与较高的自我污名相关。大多数人(90%)会向其他被迫流离失所的人推荐观看这部电影。
结论:自我污名被证明是一个往往被未受精神障碍影响个体低估的强大而持久的问题。低门槛心理教育在线干预可能是一种很有前景的工具,可以减少被迫流离失所者获得心理健康服务的障碍,例如。通过在阶梯式护理模型中实施。
1. Introduction
At the end of 2020, there were 82.4 million forcibly displaced people worldwide, including 20.7 million refugees and 4.1 million asylum seekers (United Nations High Commissioner for Refugees, Citation2021). Research shows a high prevalence of mental illnesses following flight experiences (Blackmore et al., Citation2020). In the context of record high forced displacement, the prevalence of 31.5% for post-traumatic stress disorder (PTSD) (Blackmore et al., Citation2020), with a high risk of chronicity (Blackmore et al., Citation2020; Denkinger et al., Citation2021), is especially alarming. There is meta-analytic evidence that psychosocial interventions for PTSD are effective in reducing PTSD symptoms among forcibly displaced people (Gwozdziewycz & Mehl-Madrona, Citation2013; Kip, Priebe, Holling, & Morina, Citation2020; Nosè et al., Citation2017). However, in contrast to the utilization of somatic healthcare services (Kiss, Pim, Hemmelgarn, & Quan, Citation2013; Norredam et al., Citation2004), the utilization of mental health services is low among forcibly displaced people in host countries (Satinsky, Fuhr, Woodward, Sondorp, & Roberts, Citation2019). A systematic review suggests that a reason for this treatment gap may lie in the stigma associated with having a mental illness and the stigma associated with seeking mental health services (Satinsky et al., Citation2019).
Sociologist Erving Goffman defined the concept of stigma as an ‘attribute that is deeply discrediting’ and reduces the stigmatized person ‘from a whole and usual person to a tainted discounted one’ (Goffman, Citation1963, p. 3). It can be differentiated into public stigma (labels and stereotypes dominant in a society) and self-stigma (the internalization of the public stigma by members of the stigmatized group) (Corrigan, Citation2004). Perceptions of public stigma associated with mental illness can influence the experience of self-stigma, which, in turn, affects help-seeking attitudes and behaviour (Vogel, Wade, & Hackler, Citation2007).
Stigma has been shown to be especially high in ethnic minorities and people from a refugee background (Kira et al., Citation2014). However, most mental health stigma research has been conducted within Western populations in Western countries (Livingston & Boyd, Citation2010; Schnyder, Panczak, Groth, & Schultze-Lutter, Citation2017). In accordance with the United Nations High Commissioner for Refugees (UNHCR) guidance for mental health and psychosocial support, which recommends taking ‘measures to combat stigma and discrimination of people with mental disorders’ (UNHCR, Citation2013, p. 22), there is a clear need for specific, culture-sensitive interventions to reduce mental health self-stigma in underserved groups such as forcibly displaced people.
Interventions that produce fundamental changes in attitudes and beliefs may be particularly beneficial when aiming to change stigma (Link & Phelan, Citation2001). Although mental health stigma studies among forcibly displaced people remain rare (Mills et al., Citation2020), studies indicate that psychoeducational interventions can lead to an improvement in mental health literacy and a reduction in mental health stigma (Kelly, Jorm, & Wright, Citation2007; Tsang et al., Citation2016). In recent years, one study found that men from a refugee background who participated in an online psychoeducational intervention including short videos showed greater help-seeking behaviours and smaller increases in self-stigma in the following month than a waiting-list control group (Nickerson et al., Citation2020), while an evaluation of a psychoeducational smartphone-based app for Syrian refugees showed a significant and sustained treatment effect for reducing self-stigma (Röhr et al., Citation2021). These initial findings are promising for the effectiveness of psychoeducational online interventions in reducing self-stigma. However, the paucity of research in this area demonstrates a need for further development and scientific evaluation of similar brief interventions.
The present study aims to evaluate a newly developed 10 min film, ‘Coping with Flight and Trauma’, which explains PTSD symptoms and how these could be treated. We hypothesized that forcibly displaced people would report reduced self-stigma related to mental illnesses and increased openness towards accessing mental health services directly after watching the film and at follow-up, and increased help-seeking behaviours at follow-up, compared to before watching the film.
Five research questions were addressed in this study:
What are the specific benefits of providing a web-based psychoeducational film for forcibly displaced populations?
What are the specific risks in that matter?
Does self-stigma of mental illness decrease postintervention and are such changes sustained at follow-up measurement 3 months later?
Does openness towards accessing mental health services increase postintervention and are such changes sustained?
Does PTSD psychopathology influence changes in self-stigma and openness towards accessing mental health services?
2. Method
2.1. Study design
The study was conducted using a convergent parallel mixed-methods design (Creswell & Creswell, Citation2017). The quantitative component consists of a pretest–post-test follow-up quasi-experimental design and took place via the online survey software Unipark EFS Survey (Questback, Citation2021). The qualitative component comes from open-text questionnaire items at post-test and follow-up and individual semi-structured interviews following the post-test with a randomly selected volunteer subsample.
2.2. Ethical considerations
The study was approved by the Clinical Ethics Committee of the University Hospital Tübingen (no. 112/2019BO1). Participants gave informed consent to participate and to be contacted again. All data were deidentified.
2.3. Participants
Recruitment took place between June and November 2020. Adults with forced displacement experiences within the past 8 years who were literate in English, German, or Arabic were eligible for participation. Following recommended recruitment strategies for populations underrepresented in research, such as people from refugee backgrounds (Roehr et al., Citation2019), a multi-strategic recruitment method involving snowball sampling was conducted. Specific organizations and institutions in the field were informed about the study via e-mail and asked to forward the information. Moreover, study information was published in asylum-specific Facebook groups. Recruitment took place in Germany; however, residency in Germany was not a requirement for participation. Finally, 134 participants were included in the study.
2.4. Intervention
As an easily accessible (‘low-threshold’) psychoeducational intervention, a newly developed animated 10 min film named ‘Coping with Flight and Trauma’ was used. In the film, two fictional characters from a refugee background (one woman, one man) share their experiences; and one female and one male psychotherapist provide psychoeducational information about post-traumatic stress symptoms and introduce the concept of group and individual psychotherapy. At the end of the film, information about further help services is presented. The film is available in English, Arabic, and German: https://www.youtube.com/playlist?list=PLjQMEeEDuy2sm3w50Wd-mGuzIsuwv5gCU.
As a minimal intervention, the film was developed with the option to be implemented within a broader stepped-care context – an approach where lower cost and lower intensity interventions are provided first, and more intensive and costly interventions are provided in a next step, if needed (Haaga, Citation2000).
2.4.1. Development of the film
The film was developed by the research team, consisting of psychologists and physicians, in close cooperation with refugio stuttgart e.v., a psychosocial centre for forcibly displaced people in Germany, and with support from the Center for Media Competence, University of Tübingen. With the aim of informing people about PTSD, coping strategies, and offers of professional help, the research team developed a film script in German based on previous research in the field (e.g. Denkinger et al., Citation2021). To receive feedback on the first version of the script, an expert focus group session was conducted in September 2017 with three experts working with forcibly displaced people in the psychosocial and psychotherapeutic settings of refugio stuttgart e.v. The focus group session was recorded, transcribed, and analysed using qualitative content analysis (Mayring, Citation2010). Eight recommendations for the development of psychoeducational interventions for traumatized refugees emerged (see supplementary material 1). Following these recommendations, the film script was finalized. The final German script was then translated to Arabic and English, and back-translated to German by two separate people. In this forward–backward translation process, the study team as well as native Arabic- and English-speaking mental health professionals were involved to ensure the cultural accuracy of the translations.
Within the animation process, we focused on providing clear information without showing potentially retraumatizing scenes graphically. Each animated scene was discussed with the mental health professionals of the study team before it was finalized. The first version of the film was piloted in two group settings with mental health professionals working in the psychosomatic clinic of the University Hospital of Tübingen and at refugio stuttgart e.v. to receive open feedback from the perspective of experts in the field. In the next step, the film was piloted with two refugees (one woman, one man) in a one-on-one setting. Semi-structured interviews were conducted, including questions regarding the film’s understandability, culture adequacy, authenticity, room for identification, and first impressions towards the film and the protagonists. The viewers could also provide open feedback, critique, and ideas for improvement on every aspect of the film. For instance, an earlier version of the film showed interpreters, which the viewers perceived as irritating in the animation. The film was then adapted and finalized accordingly in June 2019.
2.5. Measures
The online questionnaire was delivered in German, English, and Arabic, and included three validated questionnaires measuring mental health symptoms and self-stigma, as well as self-developed questionnaire items assessing sociodemographics, variables regarding attitudes towards and use of psychotherapy, and the feasibility and acceptance of the film. Questionnaire items were developed in German, based on the study team’s clinical and research experience and previous literature. When available, previously translated and validated versions of questionnaires were used [i.e. Patient Health Questionnaire-4 (PHQ-4), Short Screening Scale for Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) Posttraumatic Stress Disorder]. Otherwise, questionnaires and self-developed questionnaire items were translated by native speakers using a forward–backward translation method (Beaton, Bombardier, Guillemin, & Ferraz, Citation2002). The online survey was piloted using the think-aloud method (Prüfer & Rexroth, Citation2005) with a convenience sample of two men and seven women (including five mental health professionals and one Arabic-speaking refugee). To ensure cultural adequacy and translation accuracy, two native speakers of each study language participated in their mother tongue. To ensure sufficient understandability, each language version was also piloted with one non-native speaker.
2.5.1. Patient Health Questionnaire-4 (PHQ-4)
The Patient Health Questionnaire-4 (PHQ-4) (Kliem et al., Citation2016; Löwe et al., Citation2010) was used to measure the core criteria for depression and anxiety over the past 2 weeks. This ultra-brief self-report screening scale consists of a two-item depression scale (PHQ-2) and a two-item anxiety scale [Generalized Anxiety Disorder two-item (GAD-2) scale]. The total PHQ-4 score ranges from 0 to 12, with a higher sum-score representing higher distress. For the PHQ-2 and the GAD-2, a cut-off score of ≥ 3 was suggested to detect probable depression or anxiety. It has been shown that scores ascertained with different language versions of the PHQ-4 and with people of different cultural backgrounds (German host population, migrants, and refugees) can be compared in a statistically meaningful way (Tibubos & Kröger, Citation2020). Validated within the German general population, the internal consistency of the PHQ-4 was α = .78 (Löwe et al., Citation2010). Cronbach’s alpha in the present baseline sample was α = .83.
2.5.2. Short Screening Scale for DSM-IV Posttraumatic Stress Disorder
The Short Screening Scale for DSM-IV Posttraumatic Stress Disorder (Breslau, Peterson, Kessler, & Schultz, Citation1999; Siegrist & Maercker, Citation2010) was used to measure seven PTSD symptoms within the past month. A sum-score can be formed based on the number of symptoms, ranging from 0 to 7. For probable PTSD, a cut-off of ≥ 4 is recommended (Breslau et al., Citation1999). Within the German general population, Cronbach’s alpha of .90 was found (Siegrist & Maercker, Citation2010). Cronbach’s alpha in the present baseline sample was α = .85.
2.5.3. Self-Stigma of Mental Illness (SSOMI) scale
The Self-Stigma of Mental Illness (SSOMI) scale (Tucker et al., Citation2013) was used to measure the stigma that the participant associates with being labelled mentally ill. The scale consists of 10 items (e.g. ‘My self-esteem would decrease if I had a mental illness’ or ‘It would make me feel inferior to have a mental illness’), which respondents can rate on a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicate higher levels of self-stigma. Previous studies found Cronbach’s alpha ranging from .69 to .93 (Mullen & Crowe, Citation2017; Tucker et al., Citation2013). Cronbach’s alpha in the present baseline sample was α = .84.
2.5.4. Sociodemographic variables
Sociodemographic characteristics (e.g. age, gender, home country, marital status, religion, education, current residency, time since flight) were assessed.
2.5.5. Mental health services
Current and previous experiences with psychotherapy were assessed. On a seven-point Likert scale from 1 (very low) to 7 (very high), the willingness to seek treatment in the future if mental health problems emerge, and the likelihood of recommending psychotherapy to a friend if he or she suffers from mental health problems were assessed.
2.5.6. Feasibility and acceptance
On seven-point Likert scales, nine questionnaire items regarding feasibility and acceptance were developed for the post-test questionnaire (e.g. ‘How well did you understand the film language wise?’). See for all nine items (Cronbach’s α = .89). We additionally asked whether participants would recommend the film to other forcibly displaced people (answer options: yes; no) and whether any problems occurred while watching the movie (answer options: no; yes, technical problems; yes, interruptions; yes, inattention; yes, emotional problems; yes, other). Furthermore, open-text questions were included postintervention and at follow-up (‘Do you have suggestions/comments/feedback regarding the film?’).
2.5.7. Qualitative interview guide
A semi-structured interview guide was developed consisting of open-ended questions regarding the practicability (‘Did you encounter any problems watching and understanding the film?’), and acceptance of the film (‘What do you think of the film? What did you like and what didn’t you like about the film?’) and effects experienced while and after watching the film (‘Did the film change your mind about specific aspects?’).
2.6. Study procedure
Participants could choose between a German, Arabic, and English version of the online survey. They were then informed about the study goals, risks, benefits, and data security, and had to agree with the terms of the study to continue. All participants had the chance to win one of six tablet PCs and one of 10 vouchers for a bookstore. Participants were asked to develop a personal code, so that their baseline data could be matched with their follow-up data anonymously. After completing the baseline questionnaire, the film and then the post-test questionnaire were presented. Participants were then asked about their interest in taking part in a telephone interview and/or the follow-up survey. Interviews were conducted anonymously in German, English, or Arabic with randomly selected volunteering participants (n = 19). Interviewers were the first author (MSc psychologist) and the fifth author (MA in Arabic Studies). No language barriers were apparent. Three months after the baseline assessment, participants received a link via e-mail to the follow-up questionnaire.
2.7. Quantitative data analysis
Analyses were conducted using IBM SPSS version 27, R and R studio (R Core Team, Citation2021). Linear mixed-model computations were obtained from the lme4 and lmerTest R packages (Bates et al., Citation2014; Kuznetsova et al., Citation2017). For baseline sample description, means (M), standard deviation (SD), distributions, and valid percentages are reported, and t-tests for independent samples were conducted to assess differences in self-stigma at baseline. Paired-sample t-tests were used to assess pre–post differences. Linear mixed models were used to analyse the effect of time (before and after watching the film) and probable PTSD on self-stigma and openness towards accessing mental health services. An ‘openness towards accessing mental health services’ sum-score was composed from two self-developed questionnaire items on a seven-point Likert scale (‘Willingness to seek help if having mental health problems in the future’ and ‘Willingness to recommend professional help if a friend struggles with mental health problems’; Cronbach’s α = .67–.79). Post-hoc contrasts were used to allow for pairwise comparisons. The level of significance was set at α = .05.
2.8. Qualitative data analysis
The audio-recorded interviews were transcribed and anonymized. Transcripts and open-text answers on the questionnaire were analysed using qualitative content analysis (Mayring, Citation2010) with the help of the software MAXQDA (Kuckartz & Rädiker, Citation2019). Two coders (the first and fifth authors) independently conducted a summarizing analysis of a sample of transcripts to derive themes from the data. By structuring and hierarchizing these inductively derived themes, a coding tree was developed consisting of three categories and eight subcategories. Descriptions of the categories and exemplary quotes were agreed upon within the research team. Then, two researchers independently assigned relevant text sections of all transcripts and open-text answers to the subcategories. This coding process included test trails, comparisons, discussion, and adaptation loops of the coding tree. Discrepancies in assignments of the two coders were discussed, when needed with a third researcher, and a final version of the assignments was developed in an agreement process.
3. Results
3.1. Quantitative baseline results (T0)
3.1.1. Sample
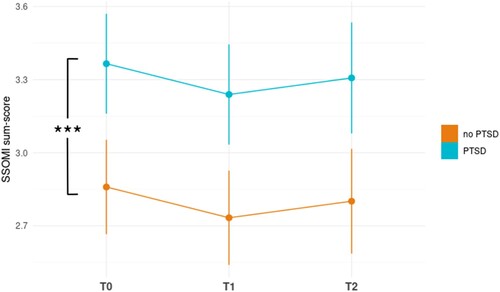
In total, 134 participants, with a mean age of 31.12 years (SD = 8.39, range: 18–66 years), were included at baseline (). The majority of participants self-identified as men (n = 97, 72.4%), 38 as women (28.4%), one person as man and woman, and one person reported man and other. Participants had arrived in the host country an average of 4.33 years before study participation (SD = 1.52, range: 0.16–8.00 years). An average of 12.29 years of school attendance (SD = 2.56, range: 1–14 years) was reported. shows exclusion and dropouts of participants during the study process.
Figure 1. Flowchart of the study process. PHQ-4, Patient Health Questionnaire-4; SSOMI, Self-Stigma of Mental Illness; PTSD, post-traumatic stress disorder.
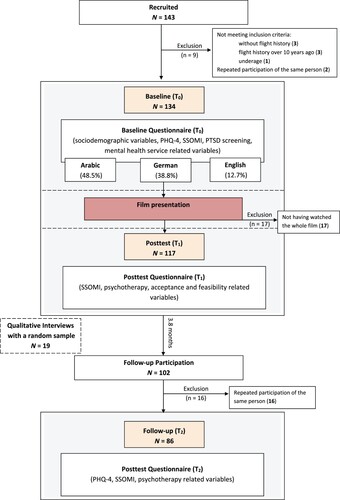
Table 1. Sociodemographic characteristics of baseline participants (N = 134).
3.1.2. Short Screening Scale for DSM-IV Posttraumatic Stress Disorder
A majority of participants reported having experienced a situation where they were filled with horror and anxiety (n = 115, 85.8%) and felt helpless (n = 113, 84.3%). Fifty-five participants (42.6%) scored above the cut-off, indicating probable PTSD, with a mean sum-score of 2.98 (SD = 2.39).
3.1.3. PHQ-4
At baseline, a PHQ-4 score of M = 5.7 (SD = 3.43) was found. Half of the participants (n = 65, 50.0%) scored above the cut-off on the depression subscale (M = 2.85, SD = 1.83); regarding the anxiety subscale, 42.8% (n = 62) scored above the cut-off (M = 2.87, SD = 1.91).
3.1.4. Psychotherapy
Forty-nine participants (36.6%) reported already being in contact with mental health services ().
Table 2. Participants’ reported past and current experiences with psychotherapy.
3.1.5. Self-stigma
At baseline, there was a SSOMI sum-score of M = 3.09 (SD = 0.77, range: 1.1–4.8). Participants’ SSOMI scores did not significantly differ by gender, age, time since arrival in host country, or previous experiences with mental health services (). However, there were significant differences in self-stigma with regard to mental health burdens. Self-stigma ratings were on average 0.65 points higher on the SSOMI five-point Likert scale (95% confidence interval 0.36; 0.93) for people who reported above at least one cut-off score for anxiety, depression, or PTSD.
Table 3. Differences in self-stigma at baseline across sociodemographic variables, mental health symptoms, and mental health service utilization.
3.2. Quantitative post-test results (T1)
The majority of participants (n = 114, 85.1%) watched the film by themselves; 10.4% (n = 14) reported watching the film together with family/friends and 4.5% (n = 6) in the company of a professional (e.g. social worker, psychotherapist).
3.2.1. Negative effects
One-fifth of participants (n = 27, 20.1%) reported emotional problems while watching the film. Seventeen participants (12.7%) reported that they stopped watching the film. Of these, four people stated emotional problems (23.6%), two people inattention (11.8%), one person technical issues (5.9%), and one the length of the film (5.9%) as the reasons for discontinuing. Nine participants did not specify a reason. Only participants who reported watching the whole film are included in further data analysis (see ).
3.2.2. Feasibility and acceptance of the film
The majority of participants would recommend watching the film to other forcibly displaced people (n = 105, 89.7%). On average, the film was rated as rather good. The feasibility and acceptance of the film could be documented ().
Table 4. Feasibility, acceptance, and perceived effects of the film (N = 117).
3.2.3. Short-term changes in self-stigma after watching the film
A paired-sample t-test revealed a significant reduction in self-stigma of mental illness measured by the SSOMI sum-score directly after watching the film (M = 2.98, SD = 0.87), compared to before watching the film (M = 3.11, SD = 0.77) [t(108) = 2.36, p = 0.02].
3.3. Quantitative follow-up results (T2)
The follow-up questionnaire was completed by 86 participants, on average 3.8 months after the baseline assessments. Over one quarter (26.5%) of the baseline sample was lost to follow-up; no reasons for dropout were reported. For 16 follow-up responses, the matching baseline data could not be identified since the personal code was not consistently reported.
3.3.1. Long-term changes after watching the film
lists the agreement to 10 statements on cognitive and behavioural changes after having watched the film. While half of participants talked about their mental health burdens with others since having watched the film, 10.7% reported having started psychotherapy.
Table 5. Follow-up reports on cognitive and behavioural changes after watching the film.
3.3.2. Longitudinal changes in self-stigma
To assess the overall effect of the intervention at postintervention and follow-up, we computed 3 × 2 (time × probable PTSD) linear mixed models. We ran three different models and compared their model fit: a random intercept model, a random intercept model with the interaction term between time and probable PTSD, and a random slope model. A comparison of fit statistics as well as a likelihood ratio test confirmed that the most parsimonious model, the random intercept model without the interaction term, generated the best model fit. Qualitatively, the results were the same regardless of the model choice.
There was no significant effect of time on self-stigma [F(2,174) = 1.75, p = .18]. There was a significant main effect of probable PTSD [F(1,109.1) = 14.50, p < .001]. As can be seen in , this indicates higher self-stigma in people with probable PTSD (M = 3.32, SD = 0.83) than in people without (M = 2.83, SD = 0.77). No significant interaction effect between time and probable PTSD occurred [F < 1].
3.3.3. Longitudinal changes in openness towards accessing mental health services
To assess the willingness to seek help as an outcome variable, a similar analytic approach to evaluating self-stigma was used. Here, the random slope model without interaction term (probable PTSD) yielded the best model fit.
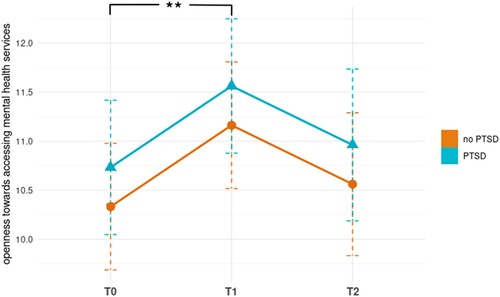
There was a significant main effect for time on openness towards accessing mental health services [F(2,113.7) = 6.53, p = .002], but no significant effect for PTSD [F(1,104.5) = .668, p = .409]. To analyse how much of the variance in openness towards accessing mental health services is attributable to differences between subjects and which proportion of the variance varied over time within subjects, we computed intraclass correlations. A significant proportion, 51% [χ2(1) = 57, p < .001], of the help-seeking variance can be explained by differences between subjects, whereas the remainder of the variance is within-person change across the three measurement points.
Post-hoc comparisons with a p-value adjustment by the Tukey method showed that openness towards accessing mental health services increased significantly directly after watching the film (M = 11.63, SE = 0.26) compared to before watching the film (M = 10.45, SE = 0.27) (p = .004), and stayed slightly increased at follow-up (M = 11.038, SE = 0.31), with no significant difference compared to either T1 (p = .742) or T0 (p = .132) ().
Figure 3. Longitudinal changes in openness towards accessing mental health services for participants with probable post-traumatic stress disorder (PTSD) and without PTSD. Openness towards accessing mental health services sum-scores range from 2 to 14, with higher scores indicating higher openness. **p < .01.
3.4. Qualitative results
3.4.1. Sample
After completing the postintervention questionnaire, participants could open another questionnaire assessing their interest in a telephone interview. Of the 115 people completing this questionnaire, 102 participants (88.7%) reported their willingness to talk about the film with a member of the study team. Following random selection until data reached saturation, 19 participants were interviewed (13 men, six women). Interviewees came from Syria (n = 14), Afghanistan (n = 1), Iraq (n = 1), Iran (n = 1), Eritrea (n = 1), and Turkey (n = 1), with 16 interviews conducted in German, two in Arabic, and one in English.
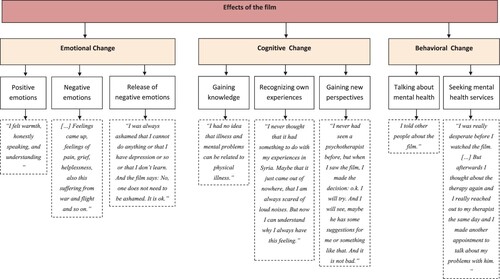
3.4.2. Effects of the film
By analysing the interviews and the answers to the open-ended questionnaire items, the theme ‘effects of the film’, with the three categories, ‘emotional change’, ‘cognitive change’, and ‘behavioural change’, was derived (). Detailed descriptions of the categories alongside example quotations are presented in the supplementary material 2.
4. Discussion
The film ‘Coping with Flight and Trauma’ was developed as a low-threshold psychoeducational online intervention for forcibly displaced people to reduce barriers in accessing mental health services. The present study documents the feasibility and high acceptance of the short film, as 90% would recommend watching the film to other forcibly displaced people. Emotional, cognitive, and behavioural responses to the intervention were found in a highly burdened sample. As the main findings, the study shows reduced self-stigma and increased openness towards accessing mental health services postintervention. Even though these changes were no longer significant 3.8 months after watching the film, increased help-seeking behaviour had been reported at follow-up.
The present study confirms a mental health treatment gap in forcibly displaced people (Boettcher et al., Citation2021; Satinsky et al., Citation2019). Prevalence rates for probable mental illness are high in the current sample, even compared to other forcibly displaced populations (Blackmore et al., Citation2020), providing a strong indication for mental health services. However, only 7% of participants were enrolled in psychotherapy at baseline. This divergence once more underlines the necessity of interventions addressing the treatment gap.
The previous literature suggests that mental health self-stigma is a major barrier in seeking help (Satinsky et al., Citation2019). Self-stigma was found in the present sample as well, independent of gender or age. By showing that self-stigma was influenced neither by time since arrival in the host country nor by previous experiences with professional mental health services, the present study suggests that mental health self-stigma is a persistent issue with low chances of spontaneous remission, even when in contact with professional help services.
Importantly, self-stigma was higher in people who reported mental health problems than in people who did not. The difference was found for probable PTSD, depression, and anxiety, but showed the highest effect size for PTSD. This seems to be robust and persistent over time, as self-stigma was higher in people with probable PTSD on all three measurements. This finding is in line with previously found associations between stigma and psychological symptoms (Byrow et al., Citation2019; Kira et al., Citation2015; Lindheimer et al., Citation2020; Livingston & Boyd, Citation2010) and supports the notion that stigma can be seen as a major mental health burden contributing to already existing mental illness (Kira et al., Citation2014). Moreover, since the SSOMI questionnaire asks hypothetical questions (‘if I had a mental illness’), the present results add that self-stigma in people with mental health burdens is even higher than people without mental illness expect it to be. This may lead to an underestimation of self-stigma in people who are not affected by mental illness.
The present study shows that participants report reduced self-stigma postintervention. However, this needs to be interpreted with caution since there were no significant changes in self-stigma over time when comparing all three measurements in a linear mixed model. This discrepancy may be due to the smaller follow-up sample. The missing long-term changes in self-stigma need to be considered in the face of competing messages reinforcing stigma that may have been received within the broader community in the time between the intervention and the follow-up measurement. Compared to Nickerson et al. (Citation2020), who showed increasing mental health self-stigma in refugees over time, even in a treatment group that received an 11-module stigma reduction intervention, the present results may still be a favourable development.
Directly after watching the film, increased openness towards accessing mental health services was reported. Openness towards the topic of mental health after watching the film can also be seen in the fact that 89% of participants agreed to be contacted for an interview about their experiences with the film. This is in line with findings showing that online interventions can lead to greater help-seeking intentions in people with a refugee background (Nickerson et al., Citation2020). At follow-up, openness towards accessing mental health services stayed slightly but not significantly increased. Competing messages within the community may have been influential once again. Embedding the film in a broader stepped-care context including community-based anti-stigma interventions could be beneficial.
Although the assessed changes are no longer significant at follow-up, there are still various behavioural changes that happened within the 3.8 months after watching the film. Approximately half of participants reported having conversations about mental health burdens and 11% had started psychotherapy since watching the film. These behavioural changes, including the increase in psychotherapy utilization compared to the 7% at baseline, are especially notable since evidence on behavioural changes due to self-stigma interventions beyond 4 weeks is rare (Thornicroft et al., Citation2016).
The present study identified several relevant aspects of the postintervention changes in attitude and behaviour. Approximately half of participants reported having gained new information about mental health and treatment options from the short film and 56% agreed that the film helped them to understand their own symptoms better, and potentially even to recognize their symptoms as belonging to a traumatic response for the first time. This is particularly interesting since the present sample is highly educated, with an average of 12.3 years of school education. Participants described the realization that other people experience the same struggles as they do. Feelings of hope, understanding, relief, motivation, courage, and a reduction of shame and desperation were reported, as well as the wish for social connection after watching the film. These could be important aspects to assess in future intervention studies.
Considering potential risks of the interventions, it is important to state that one-fifth of participants reported negative emotions such as helplessness or fear as a reaction to the film, and four people stopped watching the film because of these emotional problems. Qualitative interviews revealed that reminders of war and flight in the film were a cause of negative emotions. Negative emotions such as fear of reminders of trauma and hopelessness have previously been documented in other samples of forcibly displaced people as well (Tran et al., Citation2021) and can therefore be generally interpreted as frequent burdens, but also as potential side effects of psychoeducational interventions. Such negative effects have also been reported in other studies investigating psychoeducational films (Nickerson et al., Citation2020; von Maffei et al., Citation2015). However, in contrast to the present study, previous studies often used films in addition to personal contact or additional interventions. Given the reported negative responses, it may be beneficial to use psychoeducational films in a stepped-care context, where more specialized professional help is available when needed.
4.1. Limitations and implications for future research
Several limitations should be considered when interpreting the results. Importantly, the present study can only assess intrapersonal change over time. Because of the uncontrolled study design, we cannot rule out that the reported changes may be a general effect of time. Since the present study confirms the feasibility and acceptance of the intervention and suggests emotional, cognitive, and behavioural changes, the link between these changes and the intervention should be tested in a randomized controlled trial.
When interpreting the present results, it is also important to consider that the study’s sample was well educated, with an average of 12 years of schooling. This may be due to the online setting, which may have created a selection bias which limits the generalizability of the study’s results to less educated populations. However, this selection bias may be present when trying to reach forcibly displaced people with an online intervention outside the evaluation process as well.
Moreover, the majority of participants came from Syria (53.7%) and were male (72.4%). This distribution is similar to the general population of forcibly displaced people in Germany and common for current samples in this research area (Bär et al., Citation2021; Lindheimer et al., Citation2020). Even though, in the present sample and previous research (Livingston & Boyd, Citation2010), no gender differences in self-stigma were found, gender differences in help seeking are a common finding (Maguen et al., Citation2012; Marshall et al., Citation2006). Therefore, future studies should be conducted with other populations.
Based on the findings of this study, we would recommend that a longitudinal randomized controlled trial be conducted to examine potential long-term effects further, especially with a focus on the implementation of minimal interventions into stepped-care models that also include larger community-focused strategies to reduce mental health stigma.
5. Conclusion
The present study suggests that watching the newly developed film ‘Coping with Flight and Trauma’ is associated with emotional, cognitive, and behavioural changes, including short-term reduction in self-stigma, increased openness towards mental health services, and increased help-seeking behaviour. Therefore, web-based, psychoeducational short films can be seen as helpful tools to reduce barriers to accessing mental health services in forcibly displaced people.
Supplemental Material
Download MS Word (15.3 KB)Supplemental Material
Download MS Word (18.1 KB)Data availability statement
The data that support the findings of this study are available from the corresponding author, JKD, upon reasonable request. The data are not publicly available owing to privacy reasons.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Bär, J., Pabst, A., Röhr, S., Luppa, M., Renner, A., Nagl, M., … König, H.-H. (2021). Mental health self-stigma of Syrian refugees with posttraumatic stress symptoms: Investigating sociodemographic and psychopathological correlates. Frontiers in Psychiatry, 12, 1113.
- Bates, D., Mächler, M., Bolker, B., & Walker, S. (2014). Fitting linear mixed-effects models using lme4. arXiv preprint arXiv: 1406.5823.
- Beaton, D., Bombardier, C., Guillemin, F., & Ferraz, M. B. (2002). Recommendations for the cross-cultural adaptation of health status measures. New York: American Academy of Orthopaedic Surgeons, 12, 1–9.
- Blackmore, R., Boyle, J. A., Fazel, M., Ranasinha, S., Gray, K. M., Fitzgerald, G., … Gibson-Helm, M. (2020). The prevalence of mental illness in refugees and asylum seekers: A systematic review and meta-analysis. PLoS Medicine, 17(9), e1003337.
- Boettcher, V. S., Nowak, A. C., & Neuner, F. (2021). Mental health service utilization and perceived barriers to treatment among adult refugees in Germany. European Journal of Psychotraumatology, 12(1), 1910407.
- Breslau, N., Peterson, E. L., Kessler, R. C., & Schultz, L. R. (1999). Short screening scale for DSM-IV posttraumatic stress disorder. American Journal of Psychiatry, 156(6), 908–911.
- Byrow, Y., Pajak, R., McMahon, T., Rajouria, A., & Nickerson, A. (2019). Barriers to mental health help-seeking amongst refugee men. International Journal of Environmental Research and Public Health, 16(15), 2634.
- Corrigan, P. (2004). How stigma interferes with mental health care. American Psychologist, 59(7), 614–625.
- Creswell, J. W., & Creswell, J. D. (2017). Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks, CA: Sage.
- Denkinger, J. K., Rometsch, C., Engelhardt, M., Windthorst, P., Graf, J., Pham, P., … Junne, F. (2021). Longitudinal changes in posttraumatic stress disorder after resettlement among Yazidi female refugees exposed to violence. JAMA Network Open, 4(5), e2111120–e2111120.
- Goffman, E. (1963). Stigma: Notes on the Management of Spoiled Identity. New York: Simon & Schuster.
- Gwozdziewycz, N., & Mehl-Madrona, L. (2013). Meta-analysis of the use of narrative exposure therapy for the effects of trauma among refugee populations. The Permanente Journal, 17(1), 70.
- Haaga, D. A. (2000). Introduction to the special section on stepped care models in psychotherapy. Journal of Consulting and Clinical Psychology, 68(4), 547–548.
- Kelly, C. M., Jorm, A. F., & Wright, A. (2007). Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Medical Journal of Australia, 187(7), S26.
- Kip, A., Priebe, S., Holling, H., & Morina, N. (2020). Psychological interventions for posttraumatic stress disorder and depression in refugees: A meta-analysis of randomized controlled trials. Clinical Psychology & Psychotherapy, 27(4), 489–503.
- Kira, I. A., Lewandowski, L., Ashby, J. S., Templin, T., Ramaswamy, V., & Mohanesh, J. (2014). The traumatogenic dynamics of internalized stigma of mental illness among Arab American, Muslim, and refugee clients. Journal of the American Psychiatric Nurses Association, 20(4), 250–266.
- Kira, I. A., Ramaswamy, V., Lewandowski, L., Mohanesh, J., & Abdul-Khalek, H. (2015). Psychometric assessment of the Arabic version of the Internalized Stigma of Mental Illness (ISMI) measure in a refugee population. Transcultural Psychiatry, 52(5), 636–658.
- Kiss, V., Pim, C., Hemmelgarn, B. R., & Quan, H. (2013). Building knowledge about health services utilization by refugees. Journal of Immigrant and Minority Health, 15(1), 57–67.
- Kliem, S., Mößle, T., Klatt, T., Fleischer, S., Kudlacek, D., Kröger, C., … Wiltink, J. (2016). Psychometric evaluation of an Arabic version of the PHQ-4 based on a representative survey of Syrian refugees. Psychotherapie, Psychosomatik, Medizinische Psychologie, 66(9–10), 385–392.
- Kuckartz, U., & Rädiker, S. (2019). Analyzing Qualitative Data with MAXQDA. Basel, Switzerland: Springer.
- Kuznetsova, A., Brockhoff, P. B., & Christensen, R. H. (2017). Lmertest package: Tests in linear mixed effects models. Journal of Statistical Software, 82(1), 1–26.
- Lindheimer, N. C., Karnouk, C., Hahn, E., Churbaji, D., Schilz, L., Rayes, D., … Böge, K. (2020). Exploring the representation of depressive symptoms and the influence of stigma in Arabic-speaking refugee outpatients. Frontiers in Psychiatry, 11, 1192.
- Link, B. G., & Phelan, J. C. (2001). Conceptualizing stigma. Annual Review of Sociology, 27(1), 363–385.
- Livingston, J. D., & Boyd, J. E. (2010). Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social Science & Medicine, 71(12), 2150–2161.
- Löwe, B., Wahl, I., Rose, M., Spitzer, C., Glaesmer, H., Wingenfeld, K., … Brähler, E. (2010). A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders, 122(1–2), 86–95.
- Maguen, S., Cohen, B., Cohen, G., Madden, E., Bertenthal, D., & Seal, K. (2012). Gender differences in health service utilization among Iraq and Afghanistan veterans with posttraumatic stress disorder. Journal of Women’s Health, 21(6), 666–673.
- Marshall, G. N., Berthold, S. M., Schell, T. L., Elliott, M. N., Chun, C.-A., & Hambarsoomians, K. (2006). Rates and correlates of seeking mental health services among Cambodian refugees. American Journal of Public Health, 96(10), 1829–1835.
- Mayring, P. (2010). Qualitative inhaltsanalyse. In G. Mey & K. Mruck (Eds.), Handbuch Qualitative Forschung in der Psychologie (pp. 601–613). Wiesbaden: VS Verlag für Sozialwissenschaften.
- Mills, H., Mulfinger, N., Raeder, S., Ruesch, N., Clements, H., & Scior, K. (2020). Self-help interventions to reduce self-stigma in people with mental health problems: A systematic literature review. Psychiatry Research, 284, 112702.
- Mullen, P. R., & Crowe, A. (2017). Self-Stigma of mental illness and help seeking Among school counselors. Journal of Counseling & Development, 95(4), 401–411.
- Nickerson, A., Byrow, Y., Pajak, R., McMahon, T., Bryant, R. A., Christensen, H., & Liddell, B. J. (2020). ‘Tell your story’: A randomized controlled trial of an online intervention to reduce mental health stigma and increase help-seeking in refugee men with posttraumatic stress. Psychological Medicine, 50(5), 781–792.
- Norredam, M., Krasnik, A., Sorensen, T. M., Keiding, N., Michaelsen, J. J., & Nielsen, A. S. (2004). Emergency room utilization in Copenhagen: A comparison of immigrant groups and Danish-born residents. Scandinavian Journal of Public Health, 32(1), 53–59.
- Nosè, M., Ballette, F., Bighelli, I., Turrini, G., Purgato, M., Tol, W., … Barbui, C. (2017). Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: Systematic review and meta-analysis. PloS one, 12(2), e0171030.
- Prüfer, P., & Rexroth, M. (2005). Kognitive interviews.
- Questback, G. (2021). Unipark EFS survey. In Questback GmbH Cologne, Germany. https://www.unipark.com.
- R Core Team. (2021). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. https://www.R-project.org/
- Roehr, S., Wittmann, F., Jung, F., Hoffmann, R., Renner, A., Dams, J., Grochtdreis, T., Kersting, A., König, H.-H., & Riedel-Heller, S. G. (2019). Strategies to Recruit refugees for intervention studies: Lessons learned from the “sanadak” trial. Psychotherapie, Psychosomatik, Medizinische Psychologie, 69(12), 484–489.
- Röhr, S., Jung, F. U., Pabst, A., Grochtdreis, T., Dams, J., Nagl, M., … Kersting, A. (2021). A self-help app for Syrian refugees with posttraumatic stress (Sanadak): Randomized controlled trial. JMIR MHealth and UHealth, 9(1), e24807.
- Satinsky, E., Fuhr, D. C., Woodward, A., Sondorp, E., & Roberts, B. (2019). Mental health care utilisation and access among refugees and asylum seekers in Europe: A systematic review. Health Policy, 123(9), 851–863.
- Schnyder, N., Panczak, R., Groth, N., & Schultze-Lutter, F. (2017). Association between mental health-related stigma and active help-seeking: Systematic review and meta-analysis. The British Journal of Psychiatry, 210(4), 261–268.
- Siegrist, P., & Maercker, A. (2010). Deutsche Fassung der Short Screening Scale for DSM-IV Posttraumatic Stress Disorder. Trauma & Gewalt, 3, 208–213.
- Thornicroft, G., Mehta, N., Clement, S., Evans-Lacko, S., Doherty, M., Rose, D., Koschorke, M., Shidhaye, R., O’Reilly, C., & Henderson, C. (2016). Evidence for effective interventions to reduce mental-health-related stigma and discrimination. The Lancet, 387(10023), 1123–1132.
- Tibubos, A. N., & Kröger, H. (2020). A cross-cultural comparison of the ultrabrief mental health screeners PHQ-4 and SF-12 in Germany. Psychological Assessment, 32(7), 690–697.
- Tran, V. M., Fozouni, L., Denkinger, J. K., Rometsch, C., Junne, F., Vinck, P., & Pham, P. (2021). Factors influencing utilization and perception of health care: A qualitative study among traumatized Yazidi refugees in Germany. BMC Psychiatry, 21(1), 1–12.
- Tsang, H. W., Ching, S., Tang, K., Lam, H., Law, P. Y., & Wan, C. (2016). Therapeutic intervention for internalized stigma of severe mental illness: A systematic review and meta-analysis. Schizophrenia Research, 173(1–2), 45–53.
- Tucker, J. R., Hammer, J. H., Vogel, D. L., Bitman, R. L., Wade, N. G., & Maier, E. J. (2013). Disentangling self-stigma: Are mental illness and help-seeking self-stigmas different? Journal of Counseling Psychology, 60(4), 520–531.
- UNHCR. (2013). Operational guidance mental health psychosocial support programming for refugee operations.
- United Nations High Commissioner for Refugees. (2021). Figures at a glance. https://www.unhcr.org/figures-at-a-glance.html
- Vogel, D. L., Wade, N. G., & Hackler, A. H. (2007). Perceived public stigma and the willingness to seek counseling: The mediating roles of self-stigma and attitudes toward counseling. Journal of Counseling Psychology, 54(1), 40–50.
- von Maffei, C., Görges, F., Kissling, W., Schreiber, W., & Rummel-Kluge, C. (2015). Using films as a psychoeducation tool for patients with schizophrenia: A pilot study using a quasi-experimental pre-post design. BMC Psychiatry, 15(1), 1–7.