ABSTRACT
Background: Many countries pay special attention to the transition of their military personnel from deployment to home via post-deployment adaptation programmes (PDAPs).
Objective: This systematic review aims to provide a structured analysis of structure, process, and outcomes based on available empirical evidence for PDAPs.
Methods: A systematic literature search was performed to identify original peer-reviewed studies on PDAP in six databases (MEDLINE, Embase, PsycINFO, Cochrane Central Register of Controlled Trials, PTSDPubs, and OpenGrey). The overall risk of bias of the articles was assessed using GRADE guidelines. The literature was analysed in its description of PDAP structure, process, and outcomes. In addition, when effects were reported, these were extracted.
Results: The search resulted in 1535 unique records that were screened for eligibility; 16 articles were included, of which only three showed low risk of bias according to GRADE. Few studies clearly described and investigated PDAP structure elements (i.e. combat exposure), process elements (i.e. who delivered the intervention), and other outcome elements (i.e. adjustment issues). Most articles included some form of third location decompression (N = 10; psychoeducation and time to rest and relax on a location that is not in the mission theatre or at home) and Battlemind (N = 4; interactive training focusing on how to adapt skills and cognitions after deployment at home). The results suggest positive mental health effects and satisfaction of these two types of PDAP, although the evidence is poor.
Conclusions: Empirical, high-quality evidence for PDAP is scarce. In addition, the existing literature reveals a lack of systematic method in describing the goals of PDAP and the ways of achieving these. This leads to incomparability between studies and hinders the building of a knowledge base on PDAPs. A structure is proposed for describing the structure, process, and outcomes of PDAPs with measured effects.
HIGHLIGHTS
High -quality evidence for post-deployment adaptation programmes is scarce.
Programme structure, process, and aims with measured effects are not delineated.
Positive mental health effects are reported for Battlemind and third location decompression.
Antecedentes: Muchos países ponen especial atención a la transición de su personal militar desde el despliegue al hogar por medio de los programas de adaptación luego del despliegue (PDAPs en su sigla en inglés).
Objetivo: Esta revisión sistemática busca proveer un análisis estructurado de la estructura, proceso y resultados basados en la evidencia empírica disponible para PDAPs.
Método: Se realizó una búsqueda sistemática de la literatura para identificar estudios originales revisados por pares en PDAP en seis bases de datos (MEDLINE, Embase, PsycINFO, Cochrane Central Register of Controlled Trials, PTSDPubs y OpenGrey). El riesgo de sesgo general de los artículos fue evaluado usando las guías de GRADE. La literatura fue analizada en su descripción de la estructura, proceso y resultados de PDAP. Además, se extrajeron los efectos cuando fueron reportados.
Resultados: La búsqueda resultó en 1535 registros únicos que fueron evaluados por la idoneidad; 16 artículos fueron incluidos, de los cuales solo 3 mostraron bajo riesgo de sesgo de acuerdo con GRADE. Pocos estudios describieron e investigaron claramente los elementos de la estructura (por ej., exposición a combate), los elementos del proceso (por ej., quien entrego la intervención), y otros elementos de los resultados (por ej., problemas de adaptacion). La mayoría de los artículos incluyeron alguna forma de descompresión en un tercer lugar (N = 10; psicoeducación y tiempo para descansar y relajarse en un lugar que no sea el teatro de la misión o en el hogar) y Mentalidad de Batalla [Battlemind] (N = 4; un entrenamiento interactivo centrado en cómo adaptar habilidades y cogniciones luego del despliegue en el hogar). Los resultados sugieren efectos positivos para la salud mental y satisfacción de esos dos tipos de PDAP, aunque la evidencia es escasa.
Conclusiones: La evidencia empírica de alta calidad para PDAP es escasa. Además, la literatura existente revela una carencia de un método sistemático en describir los objetivos de PDAP y las formas de lograrlos. Esto lleva a que los estudios no sean comparables y limita la construcción de una base de conocimiento sobre PDAP. Se propone una estructura para describir la estructura, proceso, y los resultados de PDAPs con los efectos medidos.
背景:许多国家特别关注通过部署后适应计划 (PDAP) 将其军事人员从部署到回家的过渡。
目的:本系统综述旨在基于已有 PDAP 实证证据,对结构、过程和结果进行结构化分析。
方法:进行了系统文献检索,以找到六个数据库(MEDLINE、Embase、PsycINFO、Cochrane Central Register of Controlled Trials、PTSDPubs 和 OpenGrey)中关于 PDAP 的原始同行评审研究。文章的总体偏差风险使用 GRADE 指南进行评估。在对 PDAP 结构、过程和结果的描述方面对文献进行了分析。此外,当报告了效应时,这些效应会被提取出来。
结果:搜索结果筛选出 1535 条唯一记录符合资格;纳入 16 篇文章,其中仅 3 篇根据 GRADE 显示低偏差风险。很少有研究清楚地描述和考查 PDAP 结构要素(即,战斗暴露)、过程要素(即,谁实施了干预)和其他结果要素(即,适应问题)。大多数文章都包括某种形式的第三地点减压(N = 10;心理教育以及在不在任务战区或家中的地点休息和放松的时间)和 Battlemind(N = 4;关注部署后回家如何适应技能和认知的互动培训)。结果表明这两种类型的 PDAP 对心理健康有积极的影响和满意度,尽管证据较少。
1. Introduction
Returning home after military deployment is often accompanied by drastic changes in the environment of military personnel, not only concerning the physical surroundings (e.g. change in climate), but also mentally (e.g. experienced threat) and socially (e.g. lack of privacy) (Adler, Zamorski, & Britt, Citation2011). The majority of military personnel reintegrates successfully in home life and many experience positive effects of deployment (Adler et al., Citation2011; Duel & Reijnen, Citation2021). However, the transition home is also often experienced as a challenge (Black, Westwood, & Sorsdal, Citation2007). Negative post-deployment effects, such as experiencing feelings of anger and alienation, and risk-taking behaviour are reported (Adler, Britt, Castro, McGurk, & Bliese, Citation2011), as well as difficulties in finding new employment and (re-)establishing social relationships (Sayer et al., Citation2010). Further, a proportion of deployed service members develops clinical symptoms or disorders after deployment, such as post-traumatic stress and depression (Eekhout, Reijnen, Vermetten, & Geuze, Citation2016; Hoge et al., Citation2004).
To prevent these negative post-deployment effects, intervening in the seminal transition-home phase (the adaptation period) has been proposed. Indeed, many countries pay special attention to this transition phase from deployment to home (Vermetten et al., Citation2014), which makes sense given their (moral, economic, and legal) responsibility for the healthcare of their military personnel. Several post-deployment adaptation programmes (PDAPs) have been implemented to this end, which typically are provided directly following deployment for all military personnel (Fertout et al., Citation2011; Hacker Hughes et al., Citation2008; Mulligan, Fear, Jones, Wessely, & Greenberg, Citation2011; Vermetten et al., Citation2014).
PDAPs often contain (a combination of) two components: decompression and psychoeducation. The first component, decompression, denotes the importance of having time to rest and relax (to ‘decompress’) among those with whom you were deployed before returning home (Hacker Hughes et al., Citation2008). Often, decompression is organized in a location that is neither in the theatre nor in the home country (i.e. in a ‘third location’). The first component is therefore often called ‘third location decompression’ (TLD). The second component, psychoeducation, is aimed at providing information on the possible psychological effects of deployment. Different formats of providing psychoeducation are applied, ranging from a lecture format (where one person provides oral information to a large group) to small group discussions (where trainers ask questions to a small group to stimulate interaction between participants).
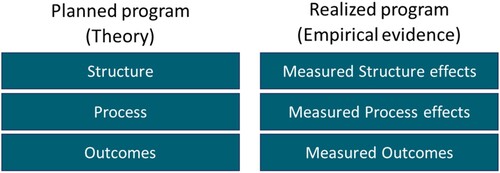
Although several countries have employed some form of PDAP, an overview of empirical studies on PDAP is lacking. A structured evaluation of PDAPs not only is warranted from an academic standpoint (i.e. what a priori assumptions and expected outcomes are described), but also helps policy improvement (i.e. what conditions are necessary). Two well-described models of evaluation are relevant here, described by Stake (Citation1967) and Donabedian (Citation1988) (see also Dückers & Thormar, Citation2015). Based on these models, three elements in the evaluation of interventions such as PDAPs can be discerned. First, structure elements denote the expectations, conditions, or circumstances that are important for the programmes to take place (settings, material resources, and organizational structure, e.g. when and where the programme takes place). Secondly, process elements concern the transactions that actually happen during giving and receiving care/information (what is done by the programme giver and receiver, e.g. didactical sessions or group discussions). Thirdly, outcome elements describe the effect of the programme on groups or individuals (improved behaviour, e.g. reduced symptoms, satisfaction with care).
In the Stake countenance model, a further distinction is made between the planned programme and the realized programme. This distinction can be used to identify gaps between PDAP policy and its actual execution. This leads to the evaluation model shown in , where a planned part and a realized part are distinguished for the three main elements (structure, process, and outcome). This model provides a detailed structure for the evaluation of educational or healthcare programmes (i.e. van Herpen, Dückers, Schaap, Olff, & te Brake, Citation2022), which is helpful in this review to thoroughly analyse information.
Figure 1. The Stake countenance model (Stake, Citation1967), integrated with terminology from Donabedian (Citation1988), to evaluate educational healthcare programmes. Blocks represent different elements, and the interactions between all of the blocks are also of interest.
The overall goal of this review is to provide more insight into PDAPs in order to facilitate future research on its quality and effectiveness, and inform policy makers on the current status of the field. Three aims are distinguished. The first aim is to provide an overview of the existing empirical literature on PDAPs. Secondly, based on the found literature and using the Stake countenance model, the planned theoretical ideas for PDAPs are delineated, distinguishing PDAP structure, process, and outcomes. A third aim is to delineate the measured realized effects for structure, process, and outcome factors for PDAPs.
2. Method
2.1. Search process and study selection
This study applied guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher, Liberati, Tetzlaff, & Altman, Citation2009) (see flow diagram in , and Supplementary material for search terms and the PRISMA checklist). A search was performed on 23 March 2021 in MEDLINE (including PubMed), Embase, PsycINFO, Cochrane Central Register of Controlled Trials, PTSDPubs, and OpenGrey. The search included terms specifying (1) the military population (e.g. ‘military personnel’), and (2a) a combination of mental health and post-deployment (e.g. ‘mental health and (post deployment)’) or (2b) specific currently employed (post-)deployment healthcare programmes (e.g. ‘third location decompression’).
Figure 2. Flow diagram of the systematic literature search for empirical studies on post-deployment adaptation programmes.
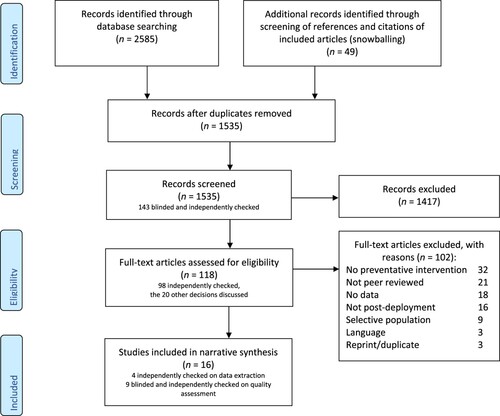
Included were articles investigating (1) deployed military personnel, (2) an active intervention for all personnel deployed, and (3) the timing of the intervention [this should be (directly) following return from deployment and before returning home]. Only publications that report original data (i.e. no reviews) and that were published in English-language peer-reviewed journals were included. Titles and abstracts of identified articles were screened and marked as ‘exclusion’, ‘maybe’, or ‘inclusion’ based on the inclusion criteria. The full text of these articles was then screened based on the inclusion criteria. Screening was conducted by MK with independent checks performed by HtB; differences in categorization were discussed until consensus was reached (see ). In addition, in order to identify recently published articles, MK screened references and citations of included articles, and reference lists of recent reviews (snowballing). This was done up to August 2021.
2.2. Data extraction and quality assessment
To provide an overview of the existing empirical literature on PDAPs (aim 1), the following data were extracted from included articles: study authors and year of publication, country, design and type of research, participants and deployment, groups studied, duration, time of delivery, and who delivered PDAP, study assessment times, outcomes assessed, the (validated) measures used, and reported effects. In addition, quality assessment was performed using nine criteria of methodological quality and risk of bias following GRADE guidelines (Guyatt et al., Citation2011). Differences in quality assessment were resolved with discussion and consensus. A study quality score was calculated for each study (range 0–10; the criterion study design was scored 0/1/2, the other eight criteria were scored 0/1; a higher number indicates an overall low risk of bias). In the data extraction and quality assessment steps, an independent check was performed by HtB and differences were discussed (see ).
2.3. Narrative synthesis
To create an overview of the planned theoretical ideas for PDAPs (aim 2), included articles were narratively described using the three elements outlined in the Stake model: structure, process, and outcome. This information is derived mostly from the Introduction and Methods sections of the studies. The PDAP structure is defined as expectations, conditions, or circumstances that are important for the PDAP. The PDAP process is defined as processes or activities in PDAP to transfer information or initiate a change. The PDAP outcome is defined as abilities, achievements, and attitudes that are expected to result from the PDAP.
To delineate the measured realized effects for structure, process, and outcome factors for PDAPs (aim 3), the available empirical evidence provided in the included articles was summarized for each of the three Stake elements. This information is derived from the Results and Discussion sections of the studies.
3. Results
To address the first aim, a total of 2585 articles were identified with our search and 49 were additionally identified using snowballing. After removal of duplicates, the titles and abstracts of 1535 articles were assessed for eligibility. A random independent check of screening (N = 143) revealed no missing inclusions. A total of 118 articles were found to be eligible for full text screening. Based on the full text paper, 102 papers were excluded since these were mostly no preventive intervention (N = 32), not peer reviewed (N = 21), or did not report on empirical data (N = 18) (for the other reasons, see ). This led to the final inclusion of 16 studies for further analysis.
An overview of the 16 studies is presented in (planned PDAP elements) and (realized PDAP elements), which will be discussed below. Four types of PDAP are mentioned: third location decompression (TLD, N = 10), Battlemind training (N = 4), psychological debriefing (N = 3), and a homecoming briefing (N = 1) (see Box 1). Concerning the quality of the studies, the average quality score is 6 (on a 10-point scale, where a higher number indicates a lower risk of bias), ranging between 3 and 10. Specifically, three studies of high quality (quality score > 7), six studies of moderate quality (score 6–7), and seven studies of low quality (score < 6) were found (see for details).
Third location decompression (TLD): time to rest and relax on a location that is not in the mission theatre or at home, combined with a psychoeducation component (Hacker Hughes et al., Citation2008).
Battlemind: a training system developed by the Walter Reed Army Institute of Research as a support programme for military personnel, consisting of training packages pre-, during, and post-deployment (Adler et al., Citation2009; Mulligan et al., Citation2012).
Psychological debriefing: aimed at individuals who have experienced a potential traumatic event to let them emotionally process their experience using counselling techniques (Deahl et al., Citation2000; Greenberg et al., Citation2003; Orsillo et al., Citation1998).
Homecoming briefing: psychoeducation on post-deployment functioning, and includes topics such as how to reintegrate with family, common symptoms of stress, and where to seek help (Iversen et al., Citation2008).
Table 1. Planned intervention process details of empirical studies on post-deployment adaptation programmes (N = 16).
Table 2. Study details and realized outcomes of empirical studies on post-deployment adaptation programmes (PDAPs) (N = 16).
Table 3. Quality assessment scores of studies investigating post-deployment adaptation programmes (PDAPs).
Table 4. Summary of the post-deployment adaptation programme (PDAP) results represented in the Stake countenance model structure.
3.1. Planned elements of PDAP
To address the second aim, the planned theoretical elements of the Stake model (structure, process, and outcome) are discussed below (see ). Where possible, a separate description is provided for each of the four identified PDAPs: TLD, Battlemind training, psychological debriefing, and a homecoming briefing.
3.1.1. Planned PDAP structure
Planned structure involves descriptions of expectations or circumstances that affect the PDAP. The 16 articles described a number of structural aspects – these were common for (did not differ between) all four PDAP types. All included articles investigate PDAP for deployed military personnel, which implies that PDAP is intended to be a follow-up to actual deployment. However, the description of what actually constitutes a ‘deployment’ varies. All authors (except for Burdett, Jones, Fear, Wessely, & Greenberg, Citation2011, who do not specify the deployment context) argue that PDAP is intended for personnel that was ‘exposed’ to combat, traumatic events, stressful events, restrictive/high-tempo/in theatre/dangerous environment, unfamiliar experiences, difficult events, conflict zones, conflict between personal and political views, boredom, isolation, frustration about significance of service, unpredictability, shifting rules of engagement, and fear for safety of lives. Some authors further suggest that PDAP is best provided in cohesive groups (Deahl et al., Citation2000; Wood et al., Citation2018) that experienced high exposure (Adler, Bliese, McGurk, Hoge, & Castro, Citation2009; Mulligan et al., Citation2012; Schneider et al., Citation2016).
3.1.2. Planned PDAP process
The PDAP process comprises processes or activities in PDAP to transfer information or initiate a change. Process factors differed for TLD, Battlemind, psychological debriefing, and homecoming briefing. Therefore, process factors are discussed for each type of PDAP separately below.
3.1.2.1. Third location decompression
Ten studies focus on TLD. All 10 TLD studies describe a number of common factors: TLD is a period of time spent on a location that is neither in theatre nor in the home country; TLD is delivered directly after leaving the operational area, and before returning to the home environment; TLD includes time to rest and relax and contains some form of psychoeducation (Burdett et al., Citation2011; Currie, Day, & Kelloway, Citation2011; de Terte, Wray, & O'Sullivan, Citation2014; Garber & Zamorski, Citation2012; Iversen et al., Citation2008; Jones et al., Citation2011, Citation2013; Mulligan et al., Citation2012; Wood et al., Citation2018; Zamorski, Guest, Bailey, & Garber, Citation2012). The allowance to drink alcohol is also part of some TLD programmes (Burdett et al., Citation2011; Jones et al., Citation2011, Citation2013; de Terte et al., Citation2014). The actual ‘third location’ varies between studies, ranging from a military base or camp (de Terte et al., Citation2014; Schneider et al., Citation2016) to four- to five-star civilian resort hotels (Garber & Zamorski, Citation2012; Zamorski et al., Citation2012), either in a stop-over country (Burdett et al., Citation2011; Currie et al., Citation2011; Garber & Zamorski, Citation2012; Jones et al., Citation2011, Citation2013; Mulligan et al., Citation2012; Zamorski et al., Citation2012) or at sea (Wood et al., Citation2018).
The psychoeducation component of TLD can be mandatory or elective and consists of educational presentations, discussions, viewing a (training) movie, or (optional) one-on-one support. The content varies from: coping with stress [positive and negative coping strategies, psychological effects (Garber & Zamorski, Citation2012; Mulligan et al., Citation2012; Zamorski et al., Citation2012)], to reintegration or readjustment [including reintegrating with family and friends, alcohol misuse, risk of driving (Burdett et al., Citation2011; de Terte et al., Citation2014; Garber & Zamorski, Citation2012; Jones et al., Citation2011, Citation2013; Mulligan et al., Citation2012; Zamorski et al., Citation2012)], reviewing deployment difficulties and accomplishments (de Terte et al., Citation2014; Zamorski et al., Citation2012), and identification of mental health problems and finding mental healthcare (Jones et al., Citation2013; Zamorski et al., Citation2012).
Not all studies report detailed information on the organization of educational sessions. Based on the studies that report details (see ), the duration varies from 24 h to more than 2 weeks, the group size for educational talks ranges from 1 to 50, and the intervention is delivered by clinicians, and military and civilian non-clinicians.
Besides the 10 studies on TLD, one study investigated time spent on a military base in the home country before post-deployment leave (decompression), which will be discussed under ‘TLD’ as well (Iversen et al., Citation2008).
3.1.2.2. Battlemind
Four studies review post-deployment Battlemind training (Adler et al., Citation2009; Garber & Zamorski, Citation2012; Mulligan et al., Citation2012; Zamorski et al., Citation2012), of which one also reviews post-deployment Battlemind psychological debriefing (Adler et al., Citation2009). All studies describe the following common factors: Battlemind addresses the cognitions and skills which are necessary in combat but need to be adapted for the transition home, emphasizes a positive approach, and underlines that problems at home [e.g. post-traumatic stress disorder (PTSD), alcohol misuse] are consequences of maladaptive coping skills. The content of Battlemind training was either reviewing coping skills (Adler et al., Citation2009; Mulligan et al., Citation2012; Zamorski et al., Citation2012) and/or reviewing movies of military cases with a transitioning or mental health problem (Garber & Zamorski, Citation2012; Mulligan et al., Citation2012). Further, information is adapted for different countries (Garber & Zamorski, Citation2012; Mulligan et al., Citation2012; Zamorski et al., Citation2012). For example, whereas the theme ‘loaded weapons at home’ was relevant in the US sessions, in the UK the theme ‘alcohol misuse’ was deemed more relevant (Mulligan et al., Citation2012). Post-deployment Battlemind psychological debriefing constitutes briefly describing a difficult event that occurred during combat, but minimizes the recollection of the events, focuses on the transition home, and reinforces that the events occurred in the past (Adler et al., Citation2009).
Central to the Battlemind approach is an interactive group discussion in order to engage deployed personnel and to enable sharing experiences of coming home (Garber & Zamorski, Citation2012; Mulligan et al., Citation2012; Zamorski et al., Citation2012). The information is delivered by trained staff, in mixed teams [civilian/military, clinical/non-clinical (Adler et al., Citation2009; Mulligan et al., Citation2012; Zamorski et al., Citation2012)], military or civilian clinicians (Garber & Zamorski, Citation2012), or clinicians only (Zamorski et al., Citation2012). Battlemind was provided as part of TLD in three studies (Garber & Zamorski, Citation2012; Mulligan et al., Citation2012; Zamorski et al., Citation2012). In one study, Battlemind is provided on its own, directly after returning home from deployment (Adler et al., Citation2009).
Three of the four studies report detailed information on educational sessions (Adler et al., Citation2009; Garber & Zamorski, Citation2012; Zamorski et al., Citation2012) (see ). The number of sessions in the training ranges from one single session to multiple sessions during 7 days. Participation is sometimes mandatory, but in other instances optional. Group size varied between two and 225 participants, and the session duration was 40–60 min.
3.1.2.3. Psychological debriefing
Psychological debriefing was investigated in three studies (Deahl et al., Citation2000; Greenberg et al., Citation2003; Orsillo, Roemer, Litz, Ehlich, & Friedman, Citation1998). The studies provide scarce details on the actual methods used in the programme (see ); only one study reports a 2 h duration in groups of eight to 10, accompanied by ‘experienced debriefers’, delivered immediately following return from deployment (Deahl et al., Citation2000).
3.1.2.4. Homecoming briefing
One study examined a homecoming briefing (Iversen et al., Citation2008). The duration of a homecoming briefing session is approximately 2 h and is delivered in the chain of command or by a (mental) healthcare professional (Iversen et al., Citation2008). Of note, standard homecoming briefings are also included as a control condition in studies (N = 2) investigating Battlemind (Adler et al., Citation2009; Mulligan et al., Citation2012). Most studies fail to provide details on the exact process of delivery.
3.1.3. Planned PDAP outcomes
The planned PDAP outcome involves descriptions of abilities, achievements, and attitudes that are expected to result from the PDAP. The studies describe three general outcomes: (1) to mitigate adverse (clinical) psychological consequences (N = 6; for Battlemind, TLD, psychological debriefing, and homecoming briefing); (2) to aid the transition from combat to home (N = 9; Battlemind and TLD) and to unwind among colleagues with whom one was in combat (N = 3; TLD). Specific planned outcomes are mentioned, but the emphasis differs between TLD and the other three PDAPs. Details are described below.
3.1.3.1. Third location decompression
The specific abilities that are targeted by TLD to achieve the three mentioned main outcomes concern overall health and well-being. TLD is described to target all three main goals by encouraging social support (Burdett et al., Citation2011; Jones et al., Citation2011, Citation2013; Schneider et al., Citation2016; Wood et al., Citation2018). TLD targets both aims number 2 and 3 (aiding the transition home and unwinding together) by discussing operational experiences (Burdett et al., Citation2011; Fertout, Jones, & Greenberg, Citation2012; Jones et al., Citation2011), fostering relaxation (Burdett et al., Citation2011; Fertout et al., Citation2012; Schneider et al., Citation2016), reintroducing alcohol in a controlled environment (Burdett et al., Citation2011; Fertout et al., Citation2012; Jones et al., Citation2011, Citation2013), and starting a ‘post-operational stress management process’ (Fertout et al., Citation2012; Jones et al., Citation2011, Citation2013). That is, several countries are developing policies which mandate that military personnel returning home from deployment have to go through a number of steps before they return to their normal duties (Fertout et al., Citation2011). Usually, this includes primary (prevent negative consequences), secondary (early detection of mental health problems), and tertiary (treatment of mental health problems) prevention. In this light, TLD is described as a form of ‘primary prevention’.
The second main aim (aiding the transition home) is targeted by TLD by increasing knowledge on reintegration/psychoeducation, stepping down from the operations tempo, or adjusting to a non-combat zone, promoting resilience and recovery (Schneider et al., Citation2016), acknowledging the efforts of personnel (Currie et al., Citation2011), reflecting on deployment experiences (Currie et al., Citation2011), preparing for returning home (Garber & Zamorski, Citation2012), providing time to process experiences (Wood et al., Citation2018), becoming aware of benefits (Wood et al., Citation2018), adjusting to time zone shift (Wood et al., Citation2018), and achieving a sense of closure (Garber & Zamorski, Citation2012). In order to address main aim 3 (to unwind together), TLD is described to promote collecting thoughts (Jones et al., Citation2011).
3.1.3.2. Battlemind, psychological debriefing, and homecoming briefing
Battlemind, psychological debriefing, and homecoming briefing aim to mitigate deployment effects (main goal 1) in different ways. Battlemind specifically aims to reframe transition difficulties and reinforce adaptive cognitions and skills (Adler et al., Citation2009; Mulligan et al., Citation2012; Zamorski et al., Citation2012). Psychological debriefing aims to help military personnel to recognize and express thoughts and feelings about their recent deployment (Orsillo et al., Citation1998) in order to emotionally and cognitively process the experience (Deahl et al., Citation2000). In their article on homecoming briefing, Iversen et al. (Citation2008) do not specify its aims.
3.2. Realized elements of PDAP
To address the third aim of our study, the realized elements (i.e. the effects that were assessed) of the 16 included studies are discussed (see ). The 16 studies were conducted in four countries: the UK (N = 8), the USA (N = 4), Canada (N = 3), and New Zealand (N = 1). The research design of the studies varied from randomized trials (N = 3) and group comparison studies (N = 6) to studies that evaluate levels of general satisfaction (N = 7). The N in the included studies also varied considerably, ranging from 106 to 22,113 deployed military employees (mean = 4045). Studies investigated deployment to Iraq or Afghanistan (N = 13), Bosnia (N = 2), and, incidentally, deployment to Kuwait, Qatar, Kyrgyzstan, the Persian Gulf, and Somalia. Timing of assessments varied between 0 and 120 months after PDAP, ranging from directly after the intervention (N = 9) and between 3 and 6 months (N = 8), to longer than 6 months (N = 4). Only three studies reported assessments at baseline (i.e. before PDAP).
The reported effects between realized structure, process, and outcome (i.e. the right side of the Stake model in ) were differentiated in this review. The most frequent effects that are assessed (and measures used) are: PTSD or PTSD symptoms (N = 10; PTSD Checklist, Primary Care PTSD Screen, Post-Traumatic Symptom Scale 10 items, Impact of Event scale), alcohol (mis)use (N = 6) (Alcohol Use Disorders Identification Test, two-item conjoint screen for alcohol), stigma (N = 4; Likert scales), depression (N = 3; Hospital Anxiety and Depression Scale, Patient Health Questionnaire), and general health (N = 3; General Health Questionnaire).
3.2.1. Realized PDAP structure
Realized structure involved the observed effects of expectations or circumstances on PDAP. The included studies only investigated these effects for TLD and Battlemind; these are discussed below.
3.2.1.1. Third location decompression
Jones et al. (Citation2013) reported that military personnel with low and modest exposure to combat have lower levels of mental health problems after TLD compared to a group without TLD. No differences between individually deployed soldiers and formed units were reported in TLD usefulness (Fertout et al., Citation2011, Citation2012). Further, high reported helpfulness or usefulness of TLD was associated with: low rank (Fertout et al., Citation2012; Jones et al., Citation2011), high willingness to participate (Fertout et al., Citation2012; Jones et al., Citation2011), a first TLD (compared to a second or subsequent), high adjustment concerns (e.g. concerns about re-establishing relationships), having a combat role versus no combat role (Jones et al., Citation2011), and high operational exposure (Fertout et al., Citation2012).
3.2.1.2. Battlemind
Positive mental health effects of Battlemind were especially found in subgroups with high combat exposure; see details on the outcome effects below (Adler et al., Citation2009; Mulligan et al., Citation2012). This confirmed the authors’ expectation that Battlemind works best for highly combat-exposed individuals (Adler et al., Citation2009; Mulligan et al., Citation2012).
3.2.2. Realized PDAP process
The realized process concerns the observed effects of PDAP processes or activities on the PDAP. These factors were only investigated for TLD and Battlemind, and are discussed below.
3.2.2.1. Third location decompression
Two studies report on the period of time spent on a third location after deployment. Iversen et al. (Citation2008) found no association with PTSD prevalence and time spent on a military base in their home country immediately after deployment (decompression). A comparison between return in 12 days (by sea) or 24 h (by air) yielded no differences for most outcome measures (see ). Some inconsistent results were found (Wood et al., Citation2018): return by sea was related to higher PTSD and feeling better prepared for returning home at 3 months, and lower stigma at 6 months and fewer medical referrals at 3 and 6 months, compared to return by air. Thus, the optimal decompression duration is unclear.
3.2.2.2. Battlemind
Large-group versus small-group delivery of Battlemind training and debriefing was investigated by Adler et al. (Citation2009), but no consistent effects of group size were found. It was found that Battlemind sessions (with lots of interaction in educational sessions) had mental health benefits for individuals with high combat exposure, compared to a (less interactive) homecoming briefing (Adler et al., Citation2009; Mulligan et al., Citation2012).
Zamorski et al. (Citation2012) investigated adjustments of the Battlemind-educational component of TLD (see ). Providing a mandatory programme in cohesive groups (as opposed to electives) and adding an experienced veteran as co-trainer (as opposed to training by a clinician only), as well as adjusting the content to Canada, resulted in higher satisfaction, more positive attitudes towards mental healthcare, and more self-efficacy (Zamorski et al., Citation2012). Thus, providing interactive training sessions versus didactic sessions, co-delivered by a veteran, seems to be beneficial, especially after high combat exposure, irrespective of group size.
3.2.3. Realized PDAP outcomes
The realized PDAP outcome involves main effects of PDAP, such as abilities, achievements, and attitudes. For all four types of PDAP (TLD, Battlemind, psychological debriefing, and homecoming briefing), outcomes were investigated.
3.2.3.1. Third location decompression
In total, 10 studies investigated TLD outcomes. Two studies compared deployed groups with TLD versus without TLD, the former group showing less PTSD (Jones et al., Citation2013; Schneider et al., Citation2016), fewer depression symptoms (Schneider et al., Citation2016), lower levels of post-deployment relationship conflict (Schneider et al., Citation2016), fewer physical symptoms (Jones et al., Citation2013), and less alcohol abuse (Jones et al., Citation2013) within 1 year after deployment. No differences between with TLD and without TLD were found in rates of mental health diagnoses by clinicians (Schneider et al., Citation2016) or in readjustment issues (e.g. ‘I found it difficult to adjust to being back home’) (Jones et al., Citation2013).
Seven studies investigated the perceived helpfulness and usefulness of TLD (Burdett et al., Citation2011; Currie et al., Citation2011; de Terte et al., Citation2014; Fertout et al., Citation2012; Garber & Zamorski, Citation2012; Jones et al., Citation2011; Zamorski et al., Citation2012). Overall, 45–95% of respondents rated TLD as helpful and useful, and experienced positive effects of TLD (e.g. TLD ‘gave me time to unwind before heading back home’) (de Terte et al., Citation2014). Answers to an open question (‘What did you think about decompression and can it be improved in any way?’) showed largely positive responses (Burdett et al., Citation2011). The perceived effectiveness of TLD also shows a small positive correlation with emotional attachment to the organization (affective commitment), co-worker support, and homecoming events (Currie et al., Citation2011). Thus, TLD seems to be beneficial and is perceived as helpful.
3.2.3.2. Battlemind
Two randomized studies compared the effects of Battlemind training with a standard post-deployment briefing. Adler et al. (Citation2009) reported fewer depression symptoms at follow-up in the Battlemind group compared to the standard briefing group. Mulligan et al. (Citation2012) did not report significant differences in mental health or stigma at follow-up between the groups. In subgroups with high combat exposure, differences between Battlemind and standard briefing were found in both studies in depression, PTSD, sleeping problems, stigma, and alcohol use, showing positive effects of Battlemind, but this was not the case for binge drinking (Adler et al., Citation2009; Mulligan et al., Citation2012). Zamorski et al. (Citation2012) reported that the majority of participants was satisfied with the Battlemind-educational component of TLD. Thus, Battlemind seems to have positive mental health effects, especially for high-exposure individuals, and is rated positively.
3.2.3.3. Psychological debriefing
In a randomized study of psychological debriefing, Deahl et al. (Citation2000) found no effect on PTSD and depression symptoms 6 months after deployment, although a reduction in feelings of anxiety was found. However, the same study also found aversive effects of psychological debriefing: stress from traumatic events and general complaints were actually lower in the control group compared to the psychological debriefing group. In a survey by Orsillo et al. (Citation1998), receiving psychological debriefing was not correlated with general mental health. Yet, a satisfaction survey by Greenberg et al. (Citation2003) showed that 67% of peacekeepers were in favour of performing psychological debriefing after deployment. Thus, psychological debriefing has more averse than beneficial effects on mental health, yet it is rated positively.
3.2.3.4. Homecoming briefing
Iversen et al. (Citation2008) found the prevalence of PTSD to be lower in a group that received a homecoming briefing (psychoeducation) versus a group without a homecoming briefing, 1–3 years after deployment. Of note, when standard homecoming briefings as a control condition were compared directly to Battlemind, it seems that Battlemind approaches have better mental health outcomes, indicating that Battlemind is superior to standard homecoming briefing (Adler et al., Citation2009; Mulligan et al., Citation2012).
4. Discussion
The first aim of this study was to provide an informative overview of available empirical studies on PDAPs. A systematic literature review identified 16 studies, of which only three could be considered to be of high quality (i.e. they had low risk of bias). From these studies, four main PDAPs were distinguished: TLD, Battlemind, psychological debriefing, and a homecoming briefing. In the articles found, TLD was most frequently investigated (N = 10).
Using the identified studies as a basis, the second aim was to describe the a priori planned programme concerning the PDAPs, distinguishing between aspects concerning planned structure, process, and outcomes. Essential PDAP structural conditions were described as (high) exposure during deployment, and being deployed in groups. The PDAP types varied in the process described (i.e. number of educational sessions, duration, location, delivered by whom). The main PDAP outcomes were described as (1) mitigating the psychological consequences of deployment, (2) aiding the transition from combat to home, and (3) unwinding with those with whom you were in combat.
As a third aim, the studies were examined for empirical evidence, thereby addressing the actual realized programme. Most studies focused on the psychological consequences of deployment, describing positive effects of TLD, Battlemind, and a homecoming briefing. Mainly negative effects were reported for psychological debriefing. Interestingly, the other main outcomes (aiding the transition home, unwinding together), as well as PDAP structure and process, were less reported on. Overall, there is a lack of concrete definitions of structure, process, and outcome of PDAPs. This hampers measurement of the expected outcome effects, and designing high-quality studies to systematically evaluate PDAP.
4.1. Unravelling intentions, practice, and outcomes
Systematically disentangling planned and realized structure, process, and outcomes of PDAPs can help in structuring and comparing future PDAP evaluation research. For instance, our analysis shows that most studies focus on mental health effects, while other intended outcomes receive little attention. Most notably, ‘aiding the transition home’ and ‘unwinding together’ are frequently mentioned as important outcomes of PDAPs, but these are scarcely included in the actual measurements. To this end, we would suggest including measures such as unit cohesion, social support, perceived organizational support, relaxation, and ease of post-deployment reintegration into social (e.g. work, family), physical (e.g. time zone, climate), and mental (e.g. feeling safe at home, operations tempo) environments. With respect to social support and cohesive groups, it is also of interest to compare reservists and individual augmentees to formed units or groups owing to their increased risk of psychological injuries post-deployment (Ursano et al., Citation2017).
In applying Stake, a number of structure and process factors were found to be deemed important for PDAP effectiveness: rank, cohesive groups, exposure, willingness to participate, emotional attachment to the organization, homecoming events, the combination of a military trainer and clinician providing the educational sessions, and interaction in educational sessions. Future research should include these aspects, not only as outcomes, but also concerning their definitions. For instance, the definition of exposure differed between studies. Some studies conceptualize the deployment itself as exposure to a (negative) traumatic event or combat, while this may not be accurate for all deployments (e.g. not-war-related deployments in ‘safe countries’) (Yehuda, Vermetten, McFarlane, & Lehrner, Citation2014). Furthermore, different types of PDAPs seem applicable to different levels of exposure, e.g. Battlemind specifically targets combat experiences. Indeed, evidence suggests Battlemind to be more applicable after high combat exposure, while TLD is more suitable after moderate to low combat exposure, when compared on mental and physical health effects. These findings suggest that a more tailored approach to the application and execution of PDAP should be considered, matching the level of exposure.
4.2. Comparison with other literature
Psychoeducation is a common planned process element in the description of all PDAPs. High satisfaction and perceived helpfulness of PDAPs was consistently reported and some evidence was found for the effectiveness of Battlemind and TLD in this review. Although other studies also found high satisfaction, the effectiveness of a single session of psychoeducation after a potential traumatic event in reducing symptoms is widely disputed (Brooks, Weston, Wessely, & Greenberg, Citation2021). Perhaps specific elements of PDAPs are crucial for this positive outcome; for example, the unique context of military deployment, as suggested elsewhere (Yehuda et al., Citation2014). This further stresses the importance of delineating structure, process, and outcome elements of PDAPs in future research in order to pinpoint which factors are related to this positive outcome. Outcomes on psychological debriefing in PDAPs (i.e. negative mental health effects were found), on the other hand, were completely in line with reviews on psychological debriefing in broader populations among civilians. It is therefore recommended to avoid using psychological debriefing (Rose, Bisson, Churchill, & Wessely, Citation2002; Sijbrandij, Olff, Reitsma, Carlier, & Gersons, Citation2006; Van Emmerik, Kamphuis, Hulsbosch, & Emmelkamp, Citation2002).
The three main PDAP goals reviewed here were also reported elsewhere. In previous reviews, an additional main goal of TLD is mentioned: ‘to recognize and reward the deployed troops for their experiences’ (Soir, Citation2017; Vermetten et al., Citation2014). This goal is only mentioned as a secondary goal by Currie et al. (Citation2011) in the current review. This difference could be a result of the fact that the included articles originated from only four countries (the UK, the USA, Canada, and New Zealand), while the other reviews included more countries. This warrants further attention.
With respect to the influence of exposure, a dose–effect relationship between mental health outcomes and the number of deployments is suggested from the broader literature (Hoge et al., Citation2004; Sundin et al., Citation2014). This supports the recommendation to differentiate between groups with different amounts of deployment, their needs, and which type of PDAP fits best. Potentially, applying a mixed methods approach, combining qualitative interviews with quantitative data collection, in groups with high versus low exposure could elucidate which aspects worked for whom in PDAP.
4.3. Strengths and limitations
This is the first structured assessment of empirical evidence for PDAPs. A systematic literature search was performed and two independent reviewers performed screening. However, only 16 relevant studies could be identified, of which only three studies were be considered to be of high quality. Baseline measures (before the PDAP) were scarce and none of the studies included pre-deployment measurements [e.g. on (mental) health and life satisfaction].
The application of the Stake model is also a strength of this study. Our goal was to further provide structure in existing studies on PDAP by delineating structural, process, and outcome elements. In doing so, this proved to be complicated because different studies did not apply this structure. For instance, Adler et al. (Citation2009) described an interaction between group, exposure, and mental health effect. This can be a measure of structure (exposure), process (group size), and outcome (mental health). This made it hard to separate the realized outcome, process, and structural elements. Further, during the reviewing process, choices were made on where PDAP factors fit the Stake model best. For example, the authors decided to describe duration, location, and intervention delivery under process, whereas one could argue that these are structural factors of PDAPs.
5. Conclusions
Although PDAPs are advocated and internationally widely used, high-quality literature is lacking describing the structural conditions needed, the exact processes used, and the outcomes that are expected. As a consequence, it is hard to assess the applicability of different approaches to PDAPs, let alone to compare their effectiveness. In this article, a first step was taken in alleviating this situation. Based on the available empirical literature concerning PDAPs, the proposed structure, process, and outcomes, as well as their measured effects, were distilled. The literature described four types of PDAP: TLD, Battlemind, psychological debriefing, and homecoming briefing. Reported information on structure, process, and outcomes was scarce, specifically conceptualizing factors such as ‘exposure’, ‘transition’, and ‘unwind together’. Positive mental health effects were found for TLD, Battlemind, and homecoming briefing, but the overall quality of most studies was low. Psychoeducation was found to reduce negative mental health effects, especially interactive forms provided by a the combination of a clinician and military trainer, and was highly valued by military personnel. More high-quality studies on PDAP are needed that not only report outcomes, but also more comprehensively describe the PDAPs’ intended structure, process, and outcomes.
Ethics statement
No review board approval was acquired to perform this systematic review. No informed consent was acquired.
Supplemental Material
Download MS Word (37.4 KB)Acknowledgements
We thank Elbert Geuze and Martine Hueting for their valuable comments on study execution and the early drafts of this manuscript.
Data availability statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Adler, A. B., Bliese, P. D., McGurk, D., Hoge, C. W., & Castro, C. A. (2009). Battlemind debriefing and Battlemind training as early interventions with soldiers returning from Iraq: Randomization by platoon. Journal of Consulting and Clinical Psychology, 77(5), 928–940. doi:10.1037/a0016877 PubMed PMID: 19803572.
- Adler, A. B., Britt, T. W., Castro, C. A., McGurk, D., & Bliese, P. D. (2011). Effect of transition home from combat on risk-taking and health-related behaviors. Journal of Traumatic Stress, 24(4), 381–389.
- Adler, A. B., Zamorski, M., & Britt, T. W. (2011). The psychology of transition: Adapting to home after deployment. In A. B. Adler, P. D. Bliese, & C. A. Castro (Eds.), Deployment psychology: Evidence-based strategies to promote mental health in the military (pp. 153–174). Washington, DC: American Psychological Association.
- Black, T., Westwood, M. J., & Sorsdal, M. N. (2007). From the front line to the front of the class: Counseling students who are military veterans. In J. A. Lippincott & R. B. Lippincott (Eds.), Special populations in college counseling: A handbook for mental health professionals (pp. 3–20). Alexandria, VA: American Counseling Association.
- Brooks, S. K., Weston, D., Wessely, S., & Greenberg, N. (2021). Effectiveness and acceptability of brief psychoeducational interventions after potentially traumatic events: A systematic review. European Journal of Psychotraumatology, 12(1), 1923110.
- Burdett, H., Jones, N., Fear, N. T., Wessely, S., & Greenberg, N. (2011). Early psychosocial intervention following operational deployment: Analysis of a free text questionnaire response. Military Medicine, 176(6), 620–625.
- Currie, S. L., Day, A., & Kelloway, E. K. (2011). Bringing the troops back home: Modeling the postdeployment reintegration experience. Journal of Occupational Health Psychology, 16(1), 38–47.
- de Terte, I., Wray, M., & O'Sullivan, P. (2014). The perceived value of third-location decompression by New Zealand Defence force personnel. Military Behavioral Health, 2(2), 189–196.
- Deahl, M., Srinivasan, M., Jones, N., Thomas, J., Neblett, C., & Jolly, A. (2000). Preventing psychological trauma in soldiers: The role of operational stress training and psychological debriefing. British Journal of Medical Psychology, 73(1), 77–85.
- Donabedian, A. (1988). The quality of care: How can it be assessed? Jama, 260(12), 1743–1748.
- Duel, J., & Reijnen, A. (2021). The long-term effects of military deployments and their relation with the quality of life of Dutch veterans. Military Behavioral Health, 9(2), 160–169.
- Dückers, M. L., & Thormar, S. B. (2015). Post-disaster psychosocial support and quality improvement: A conceptual framework for understanding and improving the quality of psychosocial support programs. Nursing & Health Sciences, 17(2), 159–165.
- Eekhout, I., Reijnen, A., Vermetten, E., & Geuze, E. (2016). Post-traumatic stress symptoms 5 years after military deployment to Afghanistan: An observational cohort study. The Lancet Psychiatry, 3(1), 58–64.
- Fertout, M., Jones, N., & Greenberg, N. (2012). Third location decompression for individual augmentees after a military deployment. Occupational Medicine, 62(3), 188–195. doi:10.1093/occmed/kqr217. Epub 20120112. PubMed PMID: 22247240
- Fertout, M., Jones, N., Greenberg, N., Mulligan, K., Knight, T., & Wessely, S. (2011). A review of United Kingdom Armed Forces’ approaches to prevent post-deployment mental health problems. International Review of Psychiatry, 23(2), 135–143.
- Garber, B. G., & Zamorski, M. A. (2012). Evaluation of a third-location decompression program for Canadian forces members returning from Afghanistan. Military Medicine, 177(4), 397–403. doi:10.7205/MILMED-D-11-00302. PubMed PMID: 22594129.
- Greenberg, N., Thomas, S. L., Iversen, A., Unwin, C., Hull, L., & Wessely, S. (2003). Do military peacekeepers want to talk about their experiences? Perceived psychological support of UK military peacekeepers on return from deployment. Journal of Mental Health, 12(6), 565–573.
- Guyatt, G., Oxman, A. D., Akl, E. A., Kunz, R., Vist, G., Brozek, J., … Jaeschke, R. (2011). GRADE guidelines: 1. Introduction – GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology, 64(4), 383–394.
- Hacker Hughes, J. G., Earnshaw, N. M., Greenberg, N., Eldridge, R., Fear, N. T., French, C., et al. (2008). The use of psychological decompression in military operational environments. Military Medicine, 173(6), 534–538.
- Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351(1), 13–22.
- Hotopf, M., Hull, L., Fear, N. T., Browne, T., Horn, O., Iversen, A., Jones, M., Murphy, D., Bland, D., Earnshaw, M., Greenberg, N., Hacker Hughes, J., Tate, A. R., Dandeker, C., Rona, R., & Wessely, S. (2006). The health of UK military personnel who deployed to the 2003 Iraq war: A cohort study. Lancet, 367(9524), 1731–1741.
- Iversen, A. C., Fear, N. T., Ehlers, A., Hughes, J. H., Hull, L., Earnshaw, M., … Hotopf, M. (2008). Risk factors for post-traumatic stress disorder among UK Armed forces personnel. Psychological Medicine, 38(4), 511–522.
- Jones, N., Burdett, H., Wessely, S., & Greenberg, N. (2011). The subjective utility of early psychosocial interventions following combat deployment. Occupational Medicine, 61(2), 102–107. doi:10.1093/occmed/kqq182. Epub 20101231. PubMed PMID: 21196471
- Jones, N., Jones, M., Fear, N. T., Fertout, M., Wessely, S., & Greenberg, N. (2013). Can mental health and readjustment be improved in UK military personnel by a brief period of structured postdeployment rest (third location decompression)? Occupational and Environmental Medicine, 70(7), 439–445. doi:10.1136/oemed-2012-101229. Epub 20130226. PubMed PMID: 23444279
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Group* P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269.
- Mulligan, K., Fear, N. T., Jones, N., Alvarez, H., Hull, L., Naumann, U., … Greenberg, N. (2012). Postdeployment Battlemind training for the UK armed forces: A cluster randomized controlled trial. Journal of Consulting and Clinical Psychology, 80(3), 331.
- Mulligan, K., Fear, N. T., Jones, N., Wessely, S., & Greenberg, N. (2011). Psycho-educational interventions designed to prevent deployment-related psychological ill-health in Armed Forces personnel: A review. Psychological Medicine, 41(4), 673–686.
- Orsillo, S. M., Roemer, L., Litz, B. T., Ehlich, P., & Friedman, M. J. (1998). Psychiatric symptomatology associated with contemporary peacekeeping: An examination of post-mission functioning among peacekeepers in Somalia. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies, 11(4), 611–625.
- Rose, S., Bisson, J., Churchill, R., & Wessely, S. (2002). Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews, 2, CD000560. doi:10.1002/14651858.CD000560. PubMed PMID: 12076399.
- Sayer, N. A., Noorbaloochi, S., Frazier, P., Carlson, K., Gravely, A., & Murdoch, M. (2010). Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatric Services, 61(6), 589–597.
- Schneider, K. G., Bezdjian, S., Burchett, D., Isler, W. C., Dickey, D., & Garb, H. N. (2016). The impact of the United States Air Force Deployment Transition Center on postdeployment mental health outcomes. Military Psychology, 28(2), 89–103.
- Sijbrandij, M., Olff, M., Reitsma, J. B., Carlier, I. V., & Gersons, B. P. (2006). Emotional or educational debriefing after psychological trauma: Randomised controlled trial. The British Journal of Psychiatry, 189(2), 150–155.
- Soir, E. D. (2017). Psychological Adjustment After Military Operations: The Utility of Postdeployment Decompression for Supporting Health Readjustment. Handbook of Military Psychology. Cham: Springer. pp. 89–103.
- Stake, R. (1967). The countenance of educational evaluation. Department for Exceptional Children, Gifted Children Section.
- Sundin, J., Herrell, R. K., Hoge, C. W., Fear, N. T., Adler, A. B., Greenberg, N., … Bliese, P. D. (2014). Mental health outcomes in US and UK military personnel returning from Iraq. The British Journal of Psychiatry, 204(3), 200–207.
- Ursano, R. J., Wang, J., Fullerton, C. S., Ramsawh, H., Gifford, R. K., Russell, D., … Galea, S. (2017). Post-deployment mental health in reserve and national guard service members: Deploying with or without one’s unit and deployment preparedness. Military Medicine, 183(1-2), e51–ee8. doi:10.1093/milmed/usx002
- Van Emmerik, A. A., Kamphuis, J. H., Hulsbosch, A. M., & Emmelkamp, P. M. (2002). Single session debriefing after psychological trauma: A meta-analysis. The Lancet, 360(9335), 766–771.
- van Herpen, M. M., Dückers, M. L., Schaap, R., Olff, M., & te Brake, H. (2022) Online one-stop shop for disaster response services after the MH17 airplane crash: An evaluation study. Frontiers in Public Health, 855. doi:10.3389/fpubh.2022.832840
- Vermetten, E., Greenberg, N., Boeschoten, M. A., Delahaije, R., Jetly, R., Castro, C. A., & McFarlane, A. C. (2014). Deployment-related mental health support: Comparative analysis of NATO and allied ISAF partners. European Journal of Psychotraumatology, 5(1), 23732.
- Wood, M. D., Adler, A. B., Bliese, P. D., McGurk, D., Castro, C. A., Hoge, C. W., & Koffman, R. (2018). Psychological adjustment after combat deployment: Decompression at home versus at sea. Military Behavioral Health, 6(4), 259–270.
- Yehuda, R., Vermetten, E., McFarlane, A. C., & Lehrner, A. (2014). PTSD in the military: Special considerations for understanding prevalence, pathophysiology and treatment following deployment. European Journal of Psychotraumatology, 5(1), 25322.
- Zamorski, M. A., Guest, K., Bailey, S., & Garber, B. G. (2012). Beyond Battlemind: Evaluation of a new mental health training program for Canadian forces personnel participating in third-location decompression. Military Medicine, 177(11), 1245–1253. doi:10.7205/MILMED-D-12-00064. PubMed PMID: 23198497.
