ABSTRACT
Background:
Parents of children with intellectual and developmental disorders often experience potentially traumatic events while caring for their children. Heightened posttraumatic stress (PTS) and posttraumatic growth (PTG) have been found in this population.
Objective:
We aimed to explore risk and protective factors for their PTS and PTG.
Method:
A cross-sectional study was conducted with 385 parents (average age M = 43.14 years, SD = 7.40; 95.3% mothers).
Results:
Parenting trauma showed an adverse effect on developing PTS (beta = 0.25, p < .01) and a positive role in promoting PTG (beta = 0.16, p < .01). Social support was protective in its correlation with lower levels of PTS (beta = −0.12, p < .01) and higher levels of PTG (beta = 0.22, p < .01). Barriers to care were associated with increased PTS (beta = 0.23, p < .01), but unrelated to PTG (beta = .01, p = .855). Negative parenting showed a significant, but small, correlation with more severe PTS (beta = 0.11, p < .05), and was unrelated to PTG (beta = −0.09, p = .065).
Conclusions:
Our study increases the understanding of posttraumatic reactions in parents, predominantly mothers, of children with IDD and identified parenting-related trauma, social support, and barriers to mental health care as predictive factors of the reactions. More research is needed to confirm and validate the effects of the discussed factors. Although causation can not be inferred, prompt and adequate screening and therapeutic resources should be provided to those mothers who were exposed to multiple stressful caregiving events and had limited healthcare access and less support from their spouses, peers, and caregiving partners.
HIGHLIGHTS
Parents of a child with Intellectual and Developmental Disorders with parenting trauma had higher posttraumatic stress (PTS) and posttraumatic growth (PTG).
Social support was related to lower PTS and higher PTG.
Barriers to care were related to higher PTS but unrelated to PTG.
Antecedentes: Los padres de niños con trastornos intelectuales y del desarrollo a menudo experimentan eventos potencialmente traumáticos mientras cuidan a sus hijos. En esta población se han encontrado un elevado estrés postraumático (PTS por sus siglas en ingles) y crecimiento postraumático (PTG por sus siglas en ingles).
Objetivo: Nuestro objetivo fue explorar los factores protectores y de riesgo para PTS y PTG.
Método: Se realizó un estudio transversal con 385 padres (con edad promedio M = 43,14 años, DS = 7,40; 95,3% madres).
Resultados: El trauma parental mostró ser un efecto adverso en el desarrollo de PTS (beta = 0.25, p < 0.01) y un papel positivo en la promover el PTG (beta = 0.16, p < 0,01). El apoyo social fue protector en su correlación con niveles más bajos de PTS (beta = −0.12, p < .01) y niveles más altos de PTG (beta = 0.22, p < .01). Las barreras a la atención se asociaron con un aumento de PTS (beta = 0.23, p < 0.01), pero no se relacionaron con PTG (beta = 0.01, p = 0,855). La crianza negativa mostró una correlación significativa, pero pequeña, con PTS más severos (beta = 0.11, p < 0,05) y no estuvo relacionado con el PTG (beta = −0.09, p = 0.065).
Conclusiones: Nuestro estudio aumenta la comprensión de las reacciones postraumáticas en los padres, predominantemente madres, de niños con IDD e identificó el trauma relacionado con la crianza, el apoyo social y las barreras para la atención de la salud mental como factores predictivos de estas reacciones. Se necesita más investigación para confirmar y validar los efectos de los factores discutidos. Si bien no se puede inferir causalidad, se deben proporcionar recursos terapéuticos y de detección, rápidos y adecuados, a aquellas madres que estuvieron expuestas a múltiples eventos estresantes del cuidado y tuvieron acceso limitado a la atención médica y menos apoyo de sus cónyuges, compañeros y cuidadores.
背景:智力和发育障碍儿童的父母在照顾孩子时经常会经历潜在创伤性事件。在这一人群中发现了更高的创伤后应激 (PTS) 和创伤后成长 (PTG)。
目的:我们旨在探讨其 PTS 和 PTG 的风险和保护因素。
方法:对 385 名父母(平均年龄 M = 43.14 岁,SD = 7.40;95.3% 为母亲)进行了一项横断面研究。
结果:养育创伤对发展 PTS 有不良影响(β = 0.25,p < .01),对促进 PTG 有积极作用(β = 0.16,p < .01)。社会支持在与较低水平 PTS (beta = −0.12, p < .01) 和较高水平 PTG (beta = 0.22, p < .01) 相关方面具有保护性。护理障碍与 PTS 增加相关(β = 0.23,p < .01),但与 PTG 无关(β = .01,p = .855)。负性养育与更严重的 PTS 有显著但很小的相关(β = 0.11,p < .05),与 PTG 无关(β = −0.09,p = .065)。
结论:我们的研究增加了对 IDD 儿童父母(主要是母亲)的创伤后反应的理解,并确定了养育相关创伤、社会支持和心理健康护理障碍是这些反应的预测因素。需要更多的研究来确认和验证所讨论因素的影响。虽然无法推断因果关系,但应向那些经历过多重应激性护理事件、医疗保健机会有限且配偶、同龄人和护理伙伴支持较少的母亲提供及时和充分的筛查和治疗资源。
Intellectual and Developmental Disorder (IDD), sometimes referred to as neurodevelopmental disorders (ND), is characterized by cognitive impairment and dysfunction that limit one’s behaviours and physical and learning abilities, such as autism spectrum disorder (ASD), cerebral palsy, attention deficit hyperactivity disorder, down syndrome, epilepsy, and developmental speech or language disorders (World Health Organization, Citation2018). Parents of children with IDD have a heightened risk of experiencing traumatic experiences while caring for their children. The current identified potentially traumatizing events (PTE) related to caring for a child with IDD include life-threatening medical procedures, severe symptoms of children’s IDD (i.e. seizures), and challenging child behaviours (e.g. self-harming, aggression) (Carmassi et al., Citation2021; Christofferson et al., Citation2019; Stewart et al., Citation2020; Xiong, McGrath, Yakovenko, Thomson, & Kaltenbach, Citation2022). As a consequence, they are at a higher risk of experiencing posttraumatic stress (PTS) or posttraumatic stress disorder (PTSD) (Carmassi et al., Citation2018; Casey et al., Citation2012). So far, there has been little evidence on the risk factors, other than parenting-related PTE, of parental PTS. From the available observational studies, the prevalence of PTSD in these parents is approximately 20–30% (Cabizuca, Marques-Portella, Mendlowicz, Coutinho, & Figueira, Citation2009; Stewart et al., Citation2020), which is significantly higher than the rate of 8–9% in the general population (Kilpatrick et al., Citation2013; Van Ameringen, Mancini, Patterson, & Boyle, Citation2008).
Experiencing PTE can be meaningful and brings positive changes to parents’ life (Thomadaki, Citation2017). For example, posttraumatic growth (PTG; Tedeschi & Calhoun, Citation1996) was proposed as a positive legacy of trauma exposure. PTG consists of several dimensions: new possibilities, changes in relating to others, personal strength, spiritual changes, and appreciation of life (Tedeschi & Calhoun, Citation1996). A previous study of parents of children with chronic diseases estimated that approximately 62.7% of the parents experienced at least a moderate degree of PTG (Hungerbuehler, Vollrath, & Landolt, Citation2011). This finding has been replicated in parents of children with autism spectrum disorders (ASD; Qin et al., Citation2021) and parents of children with down syndrome (Counselman-Carpenter, Citation2016). The PTG was proposed to be associated with parents’ improved problem-solving capacity, parenting skills, and mental resilience (Counselman-Carpenter, Citation2016; Qin et al., Citation2021).
Greater exposure to PTE is related to more severe PTS. This is often called a ‘dose-response’ or ‘building block’ effect (Elbert, Schauer, & Neuner, Citation2015; Schauer et al., Citation2003). However, the effect of PTE dose on PTG is less clear. Tedeschi and Calhoun (Citation1996) noted that individuals who have survived traumatic events tended to report more positive changes than those without a history of trauma. Greater trauma exposure is generally associated with greater PTG (Leppma et al., Citation2018). However, Kira et al. (Citation2013) highlighted that this effect depends on the type of trauma experienced. For instance, it could be proposed that events that happened a single time (e.g. life-threatening IDD diagnosis of one’s child) were associated with PTG, while events that happened repetitively (e.g. violent, harmful or self-injurious behaviours of one’s child with IDD) did not show PTG effects. It is not yet clear if traumatic events that occur in different contexts play different roles; more specifically, it is unclear whether parenting trauma and general trauma are differentially associated with PTG.
Facing potential obstacles to accessing mental health supports could worsen one’s PTS symptoms (Ouimette et al., Citation2011). These obstacles could be from healthcare systems (e.g. long waitlists ad high costs), health professionals (e.g. lack of clinicians) (Paula et al., Citation2020) and help seekers’ personal and cultural beliefs (Sritharan & Koola, Citation2019). Westermeyer and colleagues (2002) found that veterans who reported barriers to accessing care exhibited high rates of concurrent and lifetime PTSD. Ouimette et al. (Citation2011) sampled 490 patients with PTSD and found their PTS was positively correlated with perceived barriers in seeking help. Whether such effect occurs in parent groups was rarely discussed, although it is clear that most parents of children with IDD experienced significant barriers to accessing mental health services, as revealed in a recent study from our team (Xiong, Kaltenbach, Yakovenko, Lebsack, & McGrath, Citation2022). Furthermore, modifiable obstacles affecting PTG have generally not been sufficiently documented. For example, it remains to be determined whether people who perceive more barriers tend to show weaker PTG. A study by Kent et al. (Citation2013) illustrated that for cancer survivors, help-seeking behaviours could facilitate participants’ PTG. In contrast, Matsui and Taku (Citation2016) reported mixed findings in their review and recommended further elaboration on the social and cultural contexts of barriers.
Social support, a protective factor for PTS, is well-studied for its protective role in the development and course of PTS (Cieslak et al., Citation2009; Hyman, Gold, & Cott, Citation2003). This protective effect has been documented in different groups (Cluver, Fincham, & Seedat, Citation2009; King, King, Keane, Fairbank, & Adams, Citation1998; Paxton, Robinson, Shah, & Schoeny, Citation2004), amongst them caregivers of children/adolescents with severe diseases (Carmassi et al., Citation2021), and parents of cancer survivors (Kazak et al., Citation1998). A meta-analysis (Prati & Pietrantoni, Citation2009) of 103 studies showed that social support was moderately correlated with PTG. This relationship was also found in mothers of children with ASDs (Zhang, Yan, Barriball, While, & Liu, Citation2015) and bereaved caregivers (Cadell & Regehr, Citation2003).
Compared to neurotypically developing peers, children with IDD were found to experience more coercive parenting (Sullivan & Knutson, Citation2000; Vig & Kaminer, Citation2002). Such negative parenting practice have been found to be correlated with poorer parental self-efficacy, worse parent–child relationships (Day et al., Citation2021), and higher levels of parental PTS (van Ee, Kleber, & Mooren, Citation2012). In contrast, a better parent–child relationship has been correlated with less parental stress and fewer mental health struggles (Dinshtein, Dekel, & Polliack, Citation2011). A potential factor protecting against PTS and promoting PTG is positive parent–child interactions and hostile parent–child interactions were associated with increased likelihood of a parent developing PTSD. Studies of the association between parent–child relationship factors and parental PTG have thus far yielded mixed findings (Qin et al., Citation2021). The associations between parenting and PTS or PTG observed in general parent populations are yet to be tested in the populations of interest (i.e. parents of children with IDD).
Based on current literature and knowledge gaps, we aimed to examine how (a) PTE (i.e. lifetime PTE and specific parenting PTE), (b) social support, (c) barriers in seeking support, and (d) parenting style explain PTS and PTG in parents of children with IDD. We examined which factors particularly contribute to such parents’ PTS and PTG.
Methods
Participants
Overall, 602 eligible parents/primary caregivers consented to the study. Approximately three fourths (76.41%; 460/602) of the participants completed all the scales. Non completion occurred when participants stopped filling in scales before they had completed all scales. In addition, participants omitted answering specific questions in scale, which led to missing values for the scale. After deleting non-completers (n = 142) and cases with over 25% missing values (n = 75), the rest of missing values was replaced with the variable means. Only a small proportion of values (1.09%) was imputed. A total of 385 participants entered the data analysis. The sample did not show significant difference from the other cases (i.e. non completers and excluded cases due to missing values) on key demographic characteristics, except for the type of child IDD diagnoses (see Additional File 1 for details).
Participants were parents or primary caregivers of children with developmental disabilities. Inclusion criteria were: (1) having a child diagnosed with an IDD, including ASD, Attention Deficit Hyperactivity Disorder (ADHD), Cerebral Palsy, Epilepsy, Global Developmental Delay, Down Syndrome, Fetal Alcohol Spectrum Disorder (FASD), severe learning disability, and/or any other diagnosis that influences how a child moves around, communicates their ideas, processes what they hear, or remembers things; (2) being able to read, write, and understand English; (3) living in Canada; (4) having access to a tablet, smartphone, or a computer with high-speed internet; and (5) consenting to participate in the study.
Procedure
The study was approved by the IWK Health Centre Research Ethics Board (REB # 1025477). A cross-sectional survey was developed and was open to participants from June 2020 to March 2021. All participants were recruited online via a publicly available link shared in a variety of avenues, including social media platforms, parent support groups, child disability organizations (e.g. Autism Canada), and parent partners of this study. The study platform was Research Electronic Data Capture (REDCap; Harris et al., Citation2009) hosted at the study team coordinating data collection institution at the University of Alberta.
All participants read the consent form and consented. Participants had the right to decline to participate at any point or to skip any question they wished. Following consent, participants were asked questions to assess their eligibility. Individuals who met all screening criteria were invited to proceed to the survey. For ineligible participants, participation ended at this stage. Participants completing the survey could choose to participate in a gift card draw as compensation. There were three draws, each for a $100 gift card.
Measures
Demographics
The measure of demographics included eligibility questions, questions about the parent and their family (e.g. age, gender, marital and employment status, education level, and family location), and questions about their child with IDDFootnote1 (i.e. children’s age, children’s diagnoses, year of the diagnosis, parental weekly caregiving time). PTE The Life Events Checklist for DSM-5 (LEC-5; Weathers et al., Citation2013) is a self-rating measure to assess a broad range of traumatic experiences, such as natural disasters, sexual assaults, and life-threatening illness (Weathers et al., Citation2013). Weathers et al. (Citation2013) showed the LEC-5 had acceptable stability and convergent validity with other established measures of traumatic event exposures. It has also been previously validated in caregivers (Allen, Citation2015). This study employed the version that uses yes/no response categories (Boughner, Thornley, Kharlas, & Frewen, Citation2016; Kaltenbach, Schauer, Hermenau, Elbert, & Schalinski, Citation2018). The LEC-5 is consisted of 17 items; the total possible range of the scale is 0–17.Footnote2
The Parenting Trauma Checklist (PTC, Xiong, McGrath, et al., Citation2022) consists of 17 items asking about parental PTE that occurred while caring for their child with IDD. The PTC captured the PTE that were not covered in the LEC-5. The scale was tested by our team and good construct validity was observed among 424 parents (Xiong, McGrath, et al., Citation2022). The validation of the PTC and the present study were both in a larger programme designed for parents of children with IDD. All 17 items are rated with yes or no and scored 1 or 0; this yields a possible range from 0 to 17.
PTS
The PTSD Checklist for DSM-5 (PCL-5; Weathers et al., Citation2013) is a validated 20-item scale that measures PTS based on DSM-5 criteria (American Psychiatric Association, Citation2013). The items are about the extent that participants were bothered by each PTS symptom in the past month, measured on a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely) (Blevins, Weathers, Davis, Witte, & Domino, Citation2015). Parents were asked to rate each item based on their three most stressful PTEs reported in the LEC-5 and the PTC. A total score (possible range: 0–80) indicates the severity of PTS. A cut-off score of 32 was used in this study to identify likely PTSD as recommended by the US National Center for PTSD (2016). The PCL-5 has been shown to possess strong reliability and validity; for example, the full scale shows high internal consistency in a college student sample (α = .94; Blevins et al., Citation2015). The internal consistency was strong for the whole scale in this study (Cronbach’s α = .94; McDonald’s ω = .94).
PTG
The 10-item Posttraumatic Growth Inventory – Short Form (PTGI-SF; Cann et al., Citation2010) was used to assess posttraumatic growth in the parents. The PTGI-SF is measured on a 6-point Likert scale ranged from 0 (no) to 5 (a very great degree) with a total possible range of 0–50. Higher scores in PTGI-SF indicate that more positive changes were experienced by the participants in response to the three most stressful PTEs as assessed by the LEC-5 and the PTC. The PTGI-SF showed a good internal consistency (Cronbach’s α = .86) and the Cronbach’s α for subscales ranged from acceptable to good (α = .68 to .80) (Cann et al., Citation2010). Both the original scale and the short form assess five aspects of PTG: (1) new possibilities, (2) relating to others, (3) personal strength, (4) spiritual changes, and (5) appreciation of life. Both subscale scores and a total score were calculated in accordance with previous studies (Albuquerque, Narciso, & Pereira, Citation2018; Tedeschi & Calhoun, Citation1996). In this study, internal consistency was good overall (Cronbach’s α = .88; McDonald’s ω = .87).
Barriers
The Parental Healthcare Barriers Scale (PBHS, Xiong, Kaltenbach, et al., Citation2022) includes 16 items that ask to what extent parents’ looking for and receiving help for their mental health challenges were affected by the listed obstacles. This scale was designed to quantify the barriers faced specifically by parents of children with IDDs and to facilitate efforts for reducing such barriers. Items are rated on a scale from 0 (not at all) to 4 (extremely). The total possible score ranges from 0 to 64; a higher score means more barriers were encountered by the respondent. The PHBS has 4 subscales, namely personal belief (5 items), support accessibility (3 items), resource availability (4 items), and emotional readiness (3 items), with an additional open-ended question at the end. The PHBS showed good reliability, convergent and discriminant validity, as assessed in a study conducted by us (Xiong, Kaltenbach, et al., Citation2022). The validation of the PHBS and the present study were both in a larger programme designed for parents of children with IDD. No previous scale for measuring barriers to care in parents of children with IDD was found before the larger programme. In this study, the internal consistency was acceptable to good overall (Cronbach’s α = .77; McDonald’s ω = .77); Cronbach’s α across subscales ranged from .57 to .69; McDonald’s ω ranged from .58 to .70.
Social support
The Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, Dahlem, Zimet, & Farley, Citation1988) is a commonly used 12-item self-report scale that assesses perceived support from (a) family, (b) friends, and (c) significant others. These three subscales have four items each. Items are each rated from 1 (Very strongly disagree) to 7 (Very strongly agree), yielding a potential range of 12–84 for the full scale. A total score, instead of subscales, was calculated because: (1) the total score showed good internal consistency (Cronbach’s α = .88 in Zimet et al.’s (Citation1988) study), and (2) our objective was to measure general perceptions of social support in one’s network as in previous studies (Dambi et al., Citation2018; Zimet et al., Citation1988). Levels of social support participants perceive increase as the total score increases. For our study, internal consistency was excellent for the full scale (Cronbach’s α = .92; McDonald’s ω = .92).
Parenting
The parenting subscale of the Parent and Family Adjustment Scales (PAFAS-Parenting; Sanders, Morawska, Haslam, Filus, & Fletcher, Citation2014) measured parenting practices and family relationships in 4 dimensions: parental consistency (5 items), coercive parenting (5 items), positive encouragement (3 items), and parent–child relationship (5 items). The scale has shown good construct and predictive validity (Sanders et al., Citation2014). A higher score indicates more negative parenting (i.e. lower level of consistency, more coercive parenting, lower level of positive encouragement, and worse parent–child relationship). A slightly adapted version of the PAFAS-parenting was used to measure parenting practices. One item from the coercive parenting subscale (item 9) was deleted due to legal concerns about duty to report because it asks about spanking children. Therefore, we used 17 items, each scored on a Likert scale from 0 (not at all) to 3 (very much); the total score could range from 0 to 51. The total score was calculated as our research question focused on broad concept of parenting interactions and practices. The PAFAS parenting scale used in the current study showed acceptable internal consistency (Cronbach’s α = .72; McDonald’s ω = .66). The internal consistency coefficients for parenting consistency (Cronbach’s α = .56; McDonald’s ω = .56), coercive parenting (Cronbach’s α = .75; McDonald’s ω = .75), positive encouragement (Cronbach’s α = .60; McDonald’s ω = .60), and parent–child relationship (Cronbach’s α = .82; McDonald’s ω = .83) were from poor to good.
Data analysis
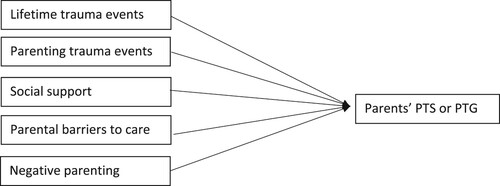
The data was analyzed with IBM SPSS Statistics 26 and R 4.0. To test the hypotheses, two hierarchical regression models were run – one for PTS (i.e. Model 1) and one for PTG (i.e. Model 2). As presented in , five risk and protective factors were examined as predictors – lifetime traumatic events, parenting trauma events, social support, barriers in help-seeking, and parenting style. For descriptive purposes, a cut-off score of 32 was used to obtain a provisional diagnosis of PTSD (i.e. whether or not participants developed PTSD based on their self-report). Relative assumptions of the two hierarchical regression models (i.e. Model 1, PTS as the dependent variable; Model 2, PTG as the dependent variable) were tested, including (a) normally distributed residuals, (b) homoscedasticity, (c) multicollinearity, (d) independence of residuals, (e) linearity, and (f) absence of influential outliers. All the assumptions were met except for the linearity between barriers in help-seeking and PTG. Since a linear relationship between the two factors was not observed, parental barriers to mental healthcare were not entered as a predictor in Model 2. The comparisons of PTS and PTG in different demographic groups were conducted by t tests and one-way ANOVAs.
Results
Demographics
A total of 385 parents of children with IDD formed the final sample for the study. Most participants were female (95.3%), biological parents (90.6%), and in a marital or common-law relationship (76.9%). The participants’ average age was 43.14 years (SD = 7.40, range = 24–69). Their children were diagnosed with a variety of IDD, including ASDs (46.0%), ADHD (41.6%), intellectual disabilities (22.2%), and global developmental delay (18.3%).Footnote3 The children had been diagnosed for an average of 7.60 years (SD = 5.72, range = 0–34). The parents reported on average 114.51 h caring for their children with IDD every week (SD = 52.41).
A detailed description of demographic variables is presented in of the Additional File 2. The effect of demographic variables on parental PTS and PTG were analyzed and reported in of the Additional File 2. No significant difference of parental PTS was found in difference sex groups (i.e. female vs. male), parent age groups, level of education, marital status, location, child age, relationship with child (i.e. biological parents vs. adoptive parents/stepparents and legal guardian), and years since child’s IDD diagnosis. No significant difference of PTG levels was found in sec groups, age, level of education, employment status, marital status, location, child age, weekly caregiving hours, number of children in the household, number of children with IDD in the household, and years since child’s IDD diagnosis.
Table 1. Sociodemographic characteristics of the participants.
Table 2. Group differences in the scores on the PCL-5.
A t test shows that parents who were biological parents of their children with IDD reported higher PTG than those who were adoptive parents/stepparents/legal guardians, p < .05. One-way ANOVAs and post hoc tests revealed that: (1) fulltime employers reported lower PTS symptoms than parttime employers (p < .05) and unemployed/stay-at-home parents (p < .01); (2) parents who spent more than 100 h per week caring for their children with IDD reported significantly higher PTS symptoms than those spent 50–100 h per week (p < .05); (3) parents who live with 3 or more kids reported significantly higher PTS than those with only 1 child (p < .05); (4) parents who cared for 2 or over 3 children with IDD had significantly higher PTS symptoms than those with 1 children with IDD, p < .01, p < .05, respectively.
Descriptive results
The sample reported an overall average score of 36.42 (SD = 17.80) on the PTS measure (intrusion symptoms M = 9.11, SD = 5.13; avoidance M = 4.05, SD = 2.52; negative alterations in cognitions and mood M = 13.06, SD = 7.12; alterations in arousal and reactivity M = 10.20, SD = 5.58). Approximately 60.3% (n = 232) parents qualified for a provisional PTSD diagnosis, as calculated using a cut-off score of 32 on the PCL-5. They reported an overall moderate level of PTG (M = 24.41, SD = 10.92), with higher levels of changes in appreciation of life (M = 6.82, SD = 2.52) and personal strength (M = 5.99, SD = 3.04), and slightly lower levels of changes in seeing new possibilities (M = 4.52, SD = 2.83), relating to others (M = 3.95, SD = 2.80), and spiritual change (M = 3.13, SD = 3.06).
Correlations between study variables are presented in . Notably, parenting and lifetime PTE revealed statistically significant positive relationships with both PTS (r(383) = .38, p < .01) and PTG (r(383) = .17, p < .01). Barriers showed a statistically significant positive correlation with PTS, r(383) = .37, p < .01, such that higher perceived or experienced barriers in help-seeking were related to more severe PTS. However, there was no significant relationship between barriers and PTG (r(383) = .01, p = .458). Negative parenting revealed only a small magnitude correlation with higher PTS (r(383) = .11, p < .05) and lower PTG (r(383) = −.15, p < .01).
Table 3. Means, standard deviations, and correlations between study variables.
Hierarchical linear regression models
Hierarchical linear regression was used to determine if the addition of social support and then of barriers in help-seeking and parenting separately improved the prediction of PTS over and above traumatic events alone (). The full model of traumatic events, social support, barriers in seeking mental health support, and parenting in predicting PTS was statistically significant, R2 = .305, p < .0005; adjusted R2 = .296. The parents’ lifetime trauma and parenting trauma contributed similarly to model 1, beta = .21, p < .01 for lifetime trauma, beta = .25, p < .01 for parenting trauma. The addition of social support to the prediction of PTS led to a statistically significant increase in R2 of .036, ΔF(1, 381) = 18.097, p < .0005. Similarly, barriers to healthcare support increased the prediction of PTS, with the change of R2 = .052, ΔF(1, 380) = 27.909, p < .0005. Parenting improved the prediction of PTS and also led to a statistically significant increase in R2 of .012, ΔF(1, 379) = 6.620, p < .05.
Table 4. Model 1: regression results using PTS as the criterion.
Following this, the four dimensions of the PHBS (i.e. personal belief, support accessibility, resource availability, and emotional readiness) entered the full model 1 simultaneously to explore their effects on PTS. Support accessibility (beta = .14, p < .01) and personal beliefs (beta = .18, p < .01) were significant predictors of parents’ PTS. Higher barriers in support accessibility and personal beliefs were associated with higher PTS. The barriers of emotional readiness (beta = −.05, p = .352) and resource availability (beta = .08, p = .114) were not significant predictors of PTS. No evidence of significant association was found between higher barriers in emotional readiness and PTS in the bivariate correlations, r(383) = .053, p = .151. While higher barriers in resource availability were positively correlated with higher PTS (r(383) = .28, p < .01), this effect was not confirmed in the predictive analysis in the context of other predictors.
In the second model, hierarchical linear regression was used to determine if the addition of social support and then of parenting improved the prediction of PTG over and above traumatic events alone. See for full details of the regression model. The full model of traumatic events, social support, and parenting to predict PTG was statistically significant, R2 = .094, p < .0005; adjusted R2 = .085. The addition of social support to the prediction of PTG led to a statistically increase in R2 = .054, ΔF(1, 381) = 22.536, p < .0005. The addition of parenting to the prediction of PTG did not lead to a statistically significant increase in R2. The predictive effect of parenting trauma (beta = .16, p < .01) was more reliable than that of lifetime trauma (beta = .08, p = .137).
Table 5. Model 2: Hierarchical regression results using PTG as the criterion.
Discussion
A web-based survey, administrated to 385 Canadian parents of children with IDD in 2020–2021, found that: (1) social support was a protective factor because of its associations with lower levels of PTS and enhanced PTG in parents; (2) parenting trauma contributed to the development of parental PTS and PTG, with its effect on PTG proving more robust than that of lifetime trauma; (3) parents who experienced higher barriers in seeking mental health support were likely to experience more PTS; however, PTG was unrelated to barriers in accessing support; (4) negative parenting practices did not show key effect on PTS or PTG.
A notable characteristic of parenting-related research is the predominant proportion of mothers in this and other studies in parents of children with IDD (Scherer, Verhey, & Kuper, Citation2019). It was hypothesized that mothers are more likely to take caregiving roles and may quit labour force (Seltzer, Floyd, Song, Greenberg, & Hong, Citation2003). Within the present study, we saw higher rates of PTSD prevalence (60.3%) and more severe overall PTS compared to other studies (Carmassi et al., Citation2018; Casey et al., Citation2012). Our convenience sample might not be generalizable to the overall population of parents of children with IDD as those with more negative reactions or more trauma experiences may have been more interested in the study and more likely to participate. There are no large population-based epidemiological surveys on PTSD prevalence among parents of children with IDD, especially during the COVID-19 pandemic. The negative impact of the lockdown manifested on public mental health, especially stress (Asmundson et al., Citation2020; Bentenuto, Mazzoni, Giannotti, Venuti, & de Falco, Citation2021), which can contribute to a possible heightened prevalence of PTSD. Parents of children with an IDD might have been particularly affected by pandemic conditions (Shorey, Lau, Tan, Ng, & Aishworiya, Citation2021). Additionally, there was a moderate level of parental PTG among our sample of parents of children with an IDD, which is consistent with other studies of parents of children with other chronic illnesses (Beighton & Wills, Citation2019; Hungerbuehler et al., Citation2011; Picoraro, Womer, Kazak, & Feudtner, Citation2014; Qin et al., Citation2021)
The exploration of risk and protective factors for parental PTS generated meaningful findings. Firstly, our study illustrated that, in addition to general PTE, parenting PTE was a positive predictor of PTS. The study confirmed a major finding of a previous study on PTS of mothers with children in neonatal intensive care units (Vanderbilt, Bushley, Young, & Frank, Citation2009). An increased caregiving burden (e.g. multiple children in the household and multiple children with IDD) could lead to higher PTS in parents. Secondly, our study verified the moderate inverse relationship between social support and PTS, supporting findings of previous research (Ouimette et al., Citation2011; Westermeyer, Canive, Thuras, Chesness, & Thompson, Citation2002). Thirdly, parental barriers were significantly positively correlated with parents’ PTS. This effect was manifested mainly through support availability and personal beliefs, which include limited access to the support, long wait lists for mental healthcare, stigma, and other negative beliefs about mental health treatments. Lastly, negative parenting only showed a relatively weak association with PTS. This implies that either negative parenting was not a key contributor to parents’ PTS, or that there was an interactive relationship between elevated PTS, negative parenting practices, and other factors yet to be identified (Christie, Hamilton-Giachritsis, Alves-Costa, Tomlinson, & Halligan, Citation2019).
The exploration of risk factors of PTG identified that both lifetime trauma events and parenting trauma events were independent positive predictors of PTG, both with a small effect size. When parenting trauma and other predictors were added into the model, the effect of lifetime trauma became smaller and non-significant across different steps in the regression model, while the effect from parenting trauma was more robust. To our knowledge, ours is the first study to directly compare both the effects of parenting trauma and lifetime general trauma. Our study found that the strength of the linear relationship between these traumatic events and PTG may depend on the type of PTE. Specifically, the traumatic events linked to parenting a child with medical complexities like IDD played a firmer, though small, role in the positive changes after trauma.
Our regression model for parental PTG explained a small amount of variance. Due to the limited research in the predictive factors of PTG among parents of children with IDD, current studies, including ours, haven’t revealed key framework of predicting their PTG (Alon, Citation2019; Byra & Ćwirynkało, Citation2020). The roles of sense of hope and self-efficacy in the model proposed by Byra and Ćwirynkało (Citation2020) may play an important role but have not yet been tested widely.
Social support showed key correlation with positive changes after the occurrence of traumatic events in this sample and other parent and caregiver groups (Cadell & Regehr, Citation2003; Prati & Pietrantoni, Citation2009; Zhang et al., Citation2015). The homogeneity of the findings from a variety of populations indicates the robust nature of the link between social support and PTG, although no directional conclusion could be made due to the cross-sectional nature of this and other studies (Cadell & Regehr, Citation2003; Prati & Pietrantoni, Citation2009; Zhang et al., Citation2015). The measurement of social support and PTG are both based on parents’ self-report. It could mean that parents who perceive higher social support tended to perceive higher PTG, and vice versa. Other factors, such as optimism and coping strategies, may play a role in this effect. For example, it has been found that perceived social support and PTG both show positive associations with optimism (Karademas, Citation2006; Prati & Pietrantoni, Citation2009).
Strengths, limitations and future directions
A strength of this study is the large nationwide sample. A total of 385 parents completed sufficient items on all measures to be used in the regression analyses. These parents had varied ages, employment statuses, levels of education, and children with a range of IDD diagnoses. Another main strength is that the study examined several novel research questions that have been rarely researched previously. For example, the study of population-specific trauma, negative parenting, and their impacts on people’s PTS and/or PTG are all understudied topics.
One limitation and characteristic of this study is the time in which it was conducted. The study was conducted between June 2020 and February 2021, at the height of the COVID-19 pandemic. The rapid change of lockdown policies caused great uncertainty and influenced families with children with an IDD (e.g. reduced childcare services and mandatory homeschooling), and profoundly changed stress levels (Bentenuto et al., Citation2021; Deacon et al., Citation2021; Deroches et al., Citation2021). This may have impacted the generalizability of the results of the study. For example, the high rate of PTSD in the study might be due to traumatic parenting experiences during the pandemic (e.g. a family member in intensive care with COVID-19), but the inference of the causality would require further research due to the cross-sectional design of our study. A second limitation consists of the use of a cross-sectional design and the recruitment of a convenience sample. Because of this, the direction for the relationships between some factors being examined (i.e. social support, parenting, and barriers to care) and outcome variables (i.e. PTS and PTG) could be bilateral. Future research should consider using a longitudinal design to demonstrate the temporal relations between the risk and protective factors studied here and PTS and PTG outcomes. Further studies are also required to explore the current understanding of risk and protective factors of parental PTS and PTG, such as child IDD symptom severity (López, Ortiz, & Noriega, Citation2019).
The convenience sampling approach performed in this study led to a trauma burdened, English-speaking sample of parents with Internet access and digital skills. Although the recruitment of highly trauma-exposed parents enabled the analysis of the effect of PTE on the outcome variables, the sampling method limited the generalizability of the findings in Francophone parents in Canada and people from remote areas with no or restricted access to the Internet. In the future, representative multiethnic national samples could be recruited and recruitment strategies for fathers of children with IDD should be established. This includes extending avenues of sampling in the work force, instead of social media groups. The potential gender difference of the discussed risk factors, especially parenting-related trauma, is to be examined.
Implications
The current study has several implications. Firstly, the high prevalence of self- reported PTSD (60.3% as screened by a cut-off score in the PCL-5) among parents of children with IDD suggests that prompt efforts to provide diagnosis and treatment for these parents should be facilitated by the healthcare system. Health professionals with expertise in IDD should be well informed that the treatments and mental health complications of children might also affect parental mental health and confidence to manage children’s behaviours (Brookman-Frazee, Citation2004).
Secondly, this study brought a novel perspective for disability communities. Caring for children with IDD is often deemed as burdensome, stressful, and challenging. This study suggests that while these burdens are evident, they may have positive as well as negative effects on parental mental health. Dissemination of this finding may instill a sense of hope and self-efficacy to parents.
Furthermore, dose–response effects of parenting trauma on both parents’ PTS symptomatology and their positive post-trauma changes suggests that, in clinical settings, sole evaluation of general trauma might not be sufficient or effective; rather, the impact of multiple traumas should be seen as cumulative, and it is important to consider the full range of traumatic experiences a parent of a child with IDD has experienced. Evaluation of parenting trauma will bolster understanding of trauma pathology, especially for those with high exposure to parenting traumatic events but low exposure to general trauma events.
Our study identified negative influences of parental healthcare obstacles over and above trauma exposure per se. To overcome such adverse impacts of barriers in support accessibility, healthcare systems should enhance accessibility of mental health services for parents of children with IDD and strengthen knowledge translation of evidence-based interventions for such parents. Furthermore, the positive influences of social support in both decreasing PTS and elevating PTG imply that psychological treatments designed to enhance the availability and quality of support networks may be helpful to maintain familial well-being and functioning in families with a child with IDD.
Conclusion
The present study describes the situation of parents, mostly mothers, of children with IDD pertaining to their PTS, PTG, exposure to parenting and lifetime traumatic experiences, and parenting barriers to mental health care. From a nationwide sample, risk and protective factors for PTS and PTG were examined. Parenting trauma displayed both a detrimental influence on mothers developing PTS and a beneficial role in promoting their PTG. Social support was protective for parents showing negative associations with PTS and positive associations with PTG. Barriers, especially barriers in support accessibility and personal beliefs, were found to be a risk factor for PTS, but were unrelated to PTG. Although negative parenting was weakly related to PTS, it was not a key contributing factor to either PTS or PTG. Our study increases understanding of mothers of children with IDD. Our study warrants development of PTSD treatments that overcome the barriers to treatment (e.g. time, cost, distance, availability, negative beliefs about treatment). Strategies to overcome the perception that parents should not get treatment because their role is to care for their children will be required if available treatments are to be used.
Availability of data and materials
The datasets used and/or analysed during the current study are not publicly available due to privacy reasons and regulations from the institution’s Research Ethics Board.
Supplemental Material
Download MS Word (16 KB)Supplemental Material
Download MS Word (33.8 KB)Acknowledgements
We thank our research team, especially Michelle Chisholm, Maria McGrath, Michael Nash, and Karen Turner. We are grateful for our research collaborators, especially Anselm Crombach, Lucy Lach, Janine Olthuis, and Maggie Schauer. We also thank all parent partners of this study: Angela McNair, Christine Kluczynski, David Bell, Hannah McGee, Jaime Lougheed-Winkler, Jeanine Lebsack, Kim Crowder, Kristine Russell, Rachel Martens, Sheila Kathleen Jennings, and Theresa Nguyen.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
1 If the parent had more than 1 child with IDD, they were asked to answer based on the one with the most severe challenges. If this was not possible, they were asked to answer for the oldest child with IDD.
2 Internal consistency was not examined for this scale or the LEC-5 because internal consistency is not a necessary property of PTE measures (Netland, Citation2001).
3 One child could be classified in more than one IDD type, as some parents had children with more than one IDD diagnosis.
References
- Albuquerque, S., Narciso, I., & Pereira, M. (2018). Posttraumatic growth in bereaved parents: A multidimensional model of associated factors. Psychological Trauma: Theory, Research, Practice, and Policy, 10(2), 199–207. https://doi.org/10.1037/tra0000305
- Allen, A. M. (2015). The impact of childhood trauma as moderated by PTSD, relationship with caregiver, and rumination [University of South Carolina Aiken]. https://scholarcommons.sc.edu/aiken_psychology_theses/12
- Alon, R. (2019). Social support and post-crisis growth among mothers of children with autism spectrum disorder and mothers of children with down syndrome. Research in Developmental Disabilities. https://doi.org/10.1016/j.ridd.2019.04.010
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, DC: American Psychiatric Pub.
- Asmundson, G. J. G., Blackstock, C., Bourque, M. C., Brimacombe, G., Crawford, A., Deacon, S. H., … Campbell-Yeo, M. (2020). Easing the disruption of COVID-19: Supporting the mental health of the people of Canada—October 2020—an RSC Policy Briefing. FACETS, 5(1), 1071–1098. https://doi.org/10.1139/facets-2020-0082
- Beighton, C., & Wills, J. (2019). How parents describe the positive aspects of parenting their child who has intellectual disabilities: A systematic review and narrative synthesis. Journal of Applied Research in Intellectual Disabilities, 32(5), 1255–1279. https://doi.org/10.1111/jar.12617
- Bentenuto, A., Mazzoni, N., Giannotti, M., Venuti, P., & de Falco, S. (2021). Psychological impact of Covid-19 pandemic in Italian families of children with neurodevelopmental disorders. Research in Developmental Disabilities, 109, 103840. https://doi.org/10.1016/j.ridd.2020.103840
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. https://doi.org/10.1002/jts.22059
- Boughner, E., Thornley, E., Kharlas, D., & Frewen, P. (2016). Mindfulness-related traits partially mediate the association between lifetime and childhood trauma exposure and PTSD and dissociative symptoms in a community sample assessed online. Mindfulness, 7(3), 672–679. https://doi.org/10.1007/s12671-016-0502-3
- Brookman-Frazee, L. (2004). Using parent/clinician partnerships in parent education programs for children with autism. Journal of Positive Behavior Interventions, 6(4), 195–213. https://doi.org/10.1177/10983007040060040201
- Byra, S., & Ćwirynkało, K. (2020). Do beliefs influence posttraumatic growth in fathers of children with intellectual disabilities? Research in Developmental Disabilities, 104, 103687. https://doi.org/10.1016/j.ridd.2020.103687
- Cabizuca, M., Marques-Portella, C., Mendlowicz, M. V., Coutinho, E. S., & Figueira, I. (2009). Posttraumatic stress disorder in parents of children with chronic illnesses: A meta-analysis. Health Psychology, 28(3), 379–388. https://doi.org/10.1037/a0014512
- Cadell, S., & Regehr, C. (2003). Factors contributing to posttraumatic growth: A proposed structural equation model. American Journal of Orthopsychiatry, 73(3), 279–287.
- Cann, A., Calhoun, L. G., Tedeschi, R. G., Taku, K., Vishnevsky, T., Triplett, K. N., & Danhauer, S. C. (2010). A short form of the posttraumatic growth inventory. Anxiety, Stress & Coping, 23(2), 127–137. https://doi.org/10.1080/10615800903094273
- Carmassi, C., Corsi, M., Bertelloni, C. A., Carpita, B., Gesi, C., Pedrinelli, V., … Dell’Osso, L. (2018). Mothers and fathers of children with epilepsy: Gender differences in post-traumatic stress symptoms and correlations with mood spectrum symptoms. Neuropsychiatric Disease and Treatment, 14, 1371–1379. https://doi.org/10.2147/NDT.S158249
- Carmassi, C., Dell’oste, V., Foghi, C., Bertelloni, C. A., Conti, E., Calderoni, S., … Dell’osso, L. (2021). Post-traumatic stress reactions in caregivers of children and adolescents/young adults with severe diseases: A systematic review of risk and protective factors. International Journal of Environmental Research and Public Health, 18(1), 1–20. https://doi.org/10.3390/ijerph18010189
- Casey, L. B., Zanksas, S., Meindl, J. N., Parra, G. R., Cogdal, P., & Powell, K. (2012). Parental symptoms of posttraumatic stress following a child’s diagnosis of autism spectrum disorder: A pilot study. Research in Autism Spectrum Disorders, 6(3), 1186–1193. https://doi.org/10.1016/j.rasd.2012.03.008
- Christie, H., Hamilton-Giachritsis, C., Alves-Costa, F., Tomlinson, M., & Halligan, S. L. (2019). The impact of parental posttraumatic stress disorder on parenting: A systematic review. European Journal of Psychotraumatology, 10(1), 1550345. https://doi.org/10.1080/20008198.2018.1550345
- Christofferson, J. L., Okonak, K., Kazak, A. E., Pierce, J., Kelly, C., Schifano, E., … Alderfer, M. A. (2019). Family consequences of potentially traumatic pediatric medical events: Implications for trauma-informed care. Journal of Family Psychology, 34(2), 237–246. https://doi.org/10.1037/fam0000597
- Cieslak, R., Benight, C., Schmidt, N., Luszczynska, A., Curtin, E., Clark, R. A., & Kissinger, P. (2009). Predicting posttraumatic growth among Hurricane Katrina survivors living with HIV: The role of self-efficacy, social support, and PTSD symptoms. Anxiety, Stress & Coping, 22(4), 449–463. https://doi.org/10.1080/10615800802403815
- Cluver, L., Fincham, D. S., & Seedat, S. (2009). Posttraumatic stress in AIDS-orphaned children exposed to high levels of trauma: The protective role of perceived social support. Journal of Traumatic Stress, 22(2), 106–112. https://doi.org/10.1002/jts.20396
- Counselman-Carpenter, E. A. (2016). The presence of posttraumatic growth (PTG) in mothers whose children are born unexpectedly with Down syndrome. Journal of Intellectual & Developmental Disability. https://doi.org/10.3109/13668250.2016.1247207
- Dambi, J. M., Corten, L., Chiwaridzo, M., Jack, H., Mlambo, T., & Jelsma, J. (2018). A systematic review of the psychometric properties of the cross-cultural translations and adaptations of the Multidimensional Perceived Social Support Scale (MSPSS). Health and Quality of Life Outcomes, 16(1), 1–19. https://doi.org/10.1186/s12955-018-0912-0
- Day, J. J., Hodges, J., Mazzucchelli, T. G., Sofronoff, K., Sanders, M. R., Einfeld, S., … Gray, K. M. (2021). Coercive parenting: Modifiable and nonmodifiable risk factors in parents of children with developmental disabilities. Journal of Intellectual Disability Research, 65(4), 306–319. https://doi.org/10.1111/jir.12813
- Deacon, S. H., Rodriguez, L. M., Elgendi, M., King, F. E., Nogueira-Arjona, R., Sherry, S. B., & Stewart, S. H. (2021). Parenting through a pandemic: Mental health and substance use consequences of mandated homeschooling. Couple and Family Psychology: Research and Practice, 10(4), 281–293. https://doi.org/10.1037/cfp0000171
- Deroches, D. I., Deacon, H., Rodriquez, L. M., Sherry, S. B., Nogueira-Arjona, R., Elgendi, M. M., … Stewart, S. H. (2021). Homeschooling during COVID-19: Gender differences in work–family conflict and alcohol use behaviour among romantic couples. Social Sciences, 10, 240. https://doi.org/10.3390/socsci10070240
- Dinshtein, Y., Dekel, R., & Polliack, M. (2011). Secondary traumatization among adult children of PTSD veterans: The role of mother-child relationships. Journal of Family Social Work, 14(2), 109–124. https://doi.org/10.1080/10522158.2011.544021
- Elbert, T., Schauer, M., & Neuner, F. (2015). Narrative exposure therapy (NET): reorganizing memories of traumatic stress, fear, and violence. Evidence Based Treatments for Trauma-Related Psychological Disorders. https://doi.org/10.1007/978-3-319-07109-1_12
- Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. https://doi.org/10.1016/j.jbi.2008.08.010
- Hungerbuehler, I., Vollrath, M. E., & Landolt, M. A. (2011). Posttraumatic growth in mothers and fathers of children with severe illnesses. Journal of Health Psychology, 16(8), 1259–1267. https://doi.org/10.1177/1359105311405872
- Hyman, S. M., Gold, S. N., & Cott, M. A. (2003). Forms of social support that moderate PTSD in childhood sexual abuse survivors. Journal of Family Violence, 18(5), 295–300. https://doi.org/10.1023/A:1025117311660
- Kaltenbach, E., Schauer, M., Hermenau, K., Elbert, T., & Schalinski, I. (2018). Course of mental health in refugees—a one year panel survey. Frontiers in Psychiatry, 9, 352. https://doi.org/10.3389/fpsyt.2018.00352
- Karademas, E. C. (2006). Self-efficacy, social support and well-being: The mediating role of optimism. Personality and Individual Differences, 40(6), 1281–1290. https://doi.org/10.1016/j.paid.2005.10.019
- Kazak, A. E., Stuber, M. L., Barakat, L. P., Meeske, K., Guthrie, D., & Meadows, A. T. (1998). Predicting posttraumatic stress symptoms in mothers and fathers of survivors of childhood cancers. Journal of the American Academy of Child & Adolescent Psychiatry, 37(8), 823–831. https://doi.org/10.1097/00004583-199808000-00012
- Kent, E. E., Alfano, C. M., Smith, A. W., Bernstein, L., Mctiernan, A., Baumgartner, K. B., & Ballard-Barbash, R. (2013). The roles of support seeking and race/ethnicity in posttraumatic growth among breast cancer survivors. Journal of Psychosocial Oncology, 31(4), 393–412. https://doi.org/10.1080/07347332.2013.798759
- Kilpatrick, D. G., Resnick, H. S., Milanak, M. E., Miller, M. W., Keyes, K. M., & Friedman, M. J. (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress. https://doi.org/10.1002/jts.21848
- King, L. A., King, D. W., Keane, T. M., Fairbank, J. A., & Adams, G. A. (1998). Resilience–recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: Hardiness, postwar social support, and additional stressful life events. Journal of Personality and Social Psychology, 74(2), 420–434. https://doi.org/10.1037/0022-3514.74.2.420
- Kira, I. A., Aboumediene, S., Ashby, J. S., Odenat, L., Mohanesh, J., & Alamia, H. (2013). The dynamics of posttraumatic growth across different trauma types in a Palestinian sample. Journal of Loss and Trauma, 18(2), 120–139. https://doi.org/10.1080/15325024.2012.679129
- Leppma, M., Mnatsakanova, A., Sarkisian, K., Scott, O., Adjeroh, L., Andrew, M. E., … McCanlies, E. C. (2018). Stressful life events and posttraumatic growth among police officers: A cross-sectional study. Stress and Health, 34(1), 175–186. https://doi.org/10.1002/smi.2772
- López, J., Ortiz, G., & Noriega, C. (2019). Crecimiento postraumático en padres de niños y adolescentes con cáncer [Posttraumatic growth in parents of children and adolescents with cancer]. Anales Del Sistema Sanitario de Navarra, 325–337. https://doi.org/10.23938/assn.0717
- Matsui, T., & Taku, K. (2016). A review of posttraumatic growth and help-seeking behavior in cancer survivors: Effects of distal and proximate culture. Japanese Psychological Research, 58(1), 142–162. https://doi.org/10.1111/jpr.12105
- Netland, M. (2001). Assessment of exposure to political violence and other potentially traumatizing events. A critical review. Journal of Traumatic Stress, 14(2), 311–326. https://doi.org/10.1023/A:1011164901867
- Ouimette, P., Vogt, D., Wade, M., Tirone, V., Greenbaum, M. A., Kimerling, R., … Rosen, C. S. (2011). Perceived barriers to care among veterans health administration patients with posttraumatic stress disorder. Psychological Services, 8(3), 212–223. https://doi.org/10.1037/a0024360
- Paula, C. S., Cukier, S., Cunha, G. R., Irarrázaval, M., Montiel-Nava, C., Garcia, R., … Rattazzi, A. (2020). Challenges, priorities, barriers to care, and stigma in families of people with autism: Similarities and differences among six Latin American countries. Autism, 24(8), 2228–2242. https://doi.org/10.1177/1362361320940073
- Paxton, K. C., Robinson, W. L., Shah, S., & Schoeny, M. E. (2004). Psychological distress for African-American adolescent males: Exposure to community violence and social support as factors. Child Psychiatry and Human Development, 34(4), 281–295. https://doi.org/10.1023/B:CHUD.0000020680.67029.4f
- Picoraro, J. A., Womer, J. W., Kazak, A. E., & Feudtner, C. (2014). Posttraumatic growth in parents and pediatric patients. Journal of Palliative Medicine, 17(2), 209–218. https://doi.org/10.1089/jpm.2013.0280
- Prati, G., & Pietrantoni, L. (2009). Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: A meta-analysis. Journal of Loss and Trauma, 14(5), 364–388. https://doi.org/10.1080/15325020902724271
- Qin, X., Feng, Y., Qu, F., Luo, Y., Chen, B., Chen, M., … Zhang, L. (2021). Posttraumatic growth among parents of children with autism spectrum disorder in China and its relationship to family function and mental resilience: A cross-sectional study. Journal of Pediatric Nursing, 57, e59–e67. https://doi.org/10.1016/j.pedn.2020.10.026
- Sanders, M. R., Morawska, A., Haslam, D. M., Filus, A., & Fletcher, R. (2014). Parenting and family adjustment scales (PAFAS): validation of a brief parent-report measure for use in assessment of parenting skills and family relationships. Child Psychiatry & Human Development, 45(3), 255–272. https://doi.org/10.1007/s10578-013-0397-3
- Schauer, M., Neuner, F., Karunakara, U., Klaschik, C., Robert, C., & Elbert, T. (2003). PTSD and the building block effect of psychological trauma among West Nile Africans. European Society for Traumatic Stress Studies Bulletin, 10(2), 5–6.
- Scherer, N., Verhey, I., & Kuper, H. (2019). Depression and anxiety in parents of children with intellectual and developmental disabilities: A systematic review and meta-analysis. PLoS ONE, 14(7), 1–18. https://doi.org/10.1371/journal.pone.0219888
- Seltzer, M. M., Floyd, F. J., Song, J., Greenberg, J. S., & Hong, J. (2003). Midlife and aging parents of adults with intellectual and developmental disabilities: Impacts of lifelong parenting. https://doi.org/10.1352/1944-7558-116.6.479
- Shorey, S., Lau, L. S. T., Tan, J. X., Ng, E. D., & Aishworiya, R. (2021). Families with children with neurodevelopmental disorders during COVID-19: A scoping review. Journal of Pediatric Psychology, 46(5), 514–525. https://doi.org/10.1093/jpepsy/jsab029
- Sritharan, B., & Koola, M. M. (2019). Barriers faced by immigrant families of children with autism: A program to address the challenges. Asian Journal of Psychiatry, 39, 53–57. https://doi.org/10.1016/j.ajp.2018.11.017
- Stewart, M., Schnabel, A., Hallford, D. J., McGillivray, J. A., Forbes, D., Foster, M., … Austin, D. W. (2020). Challenging child behaviours positively predict symptoms of posttraumatic stress disorder in parents of children with Autism Spectrum Disorder and Rare Diseases. Research in Autism Spectrum Disorders, 69, 101467. https://doi.org/10.1016/J.RASD.2019.101467
- Sullivan, P. M., & Knutson, J. F. (2000). Maltreatment and disabilities: A population-based epidemiological study. Child Abuse & Neglect, 24(10), 1257–1273. https://doi.org/10.1016/S0145-2134(00)00190-3
- Tedeschi, R. G., & Calhoun, L. G. (1996). The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. https://doi.org/10.1002/jts.2490090305
- Thomadaki, O. O. (2017). Bereavement, post-traumatic stress and post-traumatic growth: Through the lenses of positive psychology. European Journal of Psychotraumatology, 8(sup4), 1351220. https://doi.org/10.1080/20008198.2017.1351220
- Van Ameringen, M., Mancini, C., Patterson, B., & Boyle, M. H. (2008). Post-traumatic stress disorder in Canada. CNS Neuroscience and Therapeutics, 14(3), 171–181. https://doi.org/10.1111/j.1755-5949.2008.00049.x
- van Ee, E., Kleber, R. J., & Mooren, T. T. M. (2012). War trauma lingers on: Associations between maternal posttraumatic stress disorder, parent-child interaction, and child development. Infant Mental Health Journal, 33(5), 459–468. https://doi.org/10.1002/imhj.21324
- Vanderbilt, D., Bushley, T., Young, R., & Frank, D. A. (2009). Acute posttraumatic stress symptoms among urban mothers with newborns in the neonatal intensive care unit: A preliminary study. Journal of Developmental and Behavioral Pediatrics, 30(1), 50–56. https://doi.org/10.1097/DBP.0b013e318196b0de
- Vig, S., & Kaminer, R. (2002). Maltreatment and developmental disabilities in children. Journal of Developmental and Physical Disabilities, 14(4).
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The life events checklist for DSM-5 (LEC-5). Instrument available from https://www.ptsd.va.gov/professional/assessment/documents/LEC5_Standard_Self-report.PDF
- Westermeyer, J., Canive, J., Thuras, P., Chesness, D., & Thompson, J. (2002). Perceived barriers to VA mental health care among upper midwest American Indian veterans: Description and associations. Medical Care, 40(1 Suppl). https://doi.org/10.1097/00005650-200201001-00008
- World Health Organization. (2018). International classification of diseases 11th revision.
- Xiong, T., Kaltenbach, E., Yakovenko, I., Lebsack, J., & McGrath, P. J. (2022). How to measure barriers in accessing mental healthcare? Psychometric evaluation of a screening tool in parents of children with intellectual and developmental disabilities.
- Xiong, T., McGrath, P. J., Yakovenko, I., Thomson, D., & Kaltenbach, E. (2022). Parenting-related trauma exposure among parents of children with intellectual and developmental disorders: Development and validation of the Parenting Trauma Checklist. Journal of Traumatic Stress, 1–12. https://doi.org/10.1002/jts.22779
- Zhang, W., Yan, T. T., Barriball, K. L., While, A. E., & Liu, X. H. (2015). Post-traumatic growth in mothers of children with autism: A phenomenological study. Autism, 19(1), 29–37. https://doi.org/10.1177/1362361313509732
- Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. https://doi.org/10.1207/s15327752jpa5201_2