ABSTRACT
Introduction: Although evidence-based treatments for posttraumatic stress disorder (PTSD) in adolescents and young adults exist, affected youth do not have sufficient access to these treatments due to structural and attitudinal barriers. Internet- and mobile-based interventions (IMIs) can help fill this healthcare gap, but such programmes have not yet been sufficiently evaluated in youth with PTSD.
Aim: This study aims to investigate the feasibility of an IMI for youth with PTSD in a one-arm, non-randomised, prospective proof-of-concept feasibility study.
Methods: We aim to recruit 32 youth between 15 and 21 years old with clinically relevant posttraumatic stress symptoms (CATS ≥ 21), who will receive access to the IMI. The IMI consists of nine sessions involving psychoeducation, emotion regulation and coping skills, written-based imaginal exposure, cognitive restructuring and relapse prevention. Participants will be guided by an eCoach, who provides weekly semi-standardised written feedback on completed sessions and adherence reminders. We will use a formal feasibility framework to assess different dimensions of feasibility: (1) recruitment capability and resulting sample characteristics, (2) data collection procedures and outcome measures, (3) acceptability of the IMI and study procedures, (4) resources and ability to manage and implement the study and IMI and (5) participants’ responses to the IMI in terms of symptom severity and satisfaction. Additionally, potential negative effects related to the intervention will be assessed. Assessments take place pre-, mid- and post-intervention and at follow-up, including semi-structured clinical telephone interviews for PTSD diagnostics at pre- and post-intervention assessment. Qualitative interviews will be conducted to investigate the youth perspectives on the IMI.
Discussion: This study aims to determine the feasibility of a guided IMI for youth with PTSD to adapt the IMI as closely as possible to youth needs and to inform the design, procedure and safety management of a large-scale efficacy RCT.
Trial registration: German Clinical Trials Register identifier: DRKS00023341.
HIGHLIGHTS
Evidence-based care for adolescents after trauma is not widely available.• This study evaluates the feasibility of a guided trauma-focused Internet intervention as a time- and location-independent low-threshold treatment option for adolescents and young adults with posttraumatic stress disorder.
Introducción: Aunque existen tratamientos basados en la evidencia para el trastorno de estrés postraumático (TEPT) en adolescentes y adultos jóvenes, los jóvenes afectados no tienen suficiente acceso a estos tratamientos debido a barreras estructurales y actitudinales. Las intervenciones basadas en Internet y dispositivos móviles (IMI en su sigla en inglés) pueden ayudar a llenar este vacío en la atención de salud, pero tales programas aún no se han evaluado suficientemente en jóvenes con TEPT.
Objetivo: Este estudio tiene como objetivo investigar la factibilidad de una IMI para jóvenes con TEPT en un estudio de factibilidad de prueba de concepto prospectivo, no aleatorio, de un solo brazo.
Métodos: Nuestro objetivo es reclutar a 32 jóvenes entre 15 y 21 años con síntomas de estrés postraumático clínicamente relevantes (CATS > 21), que recibirán acceso a la IMI. La IMI consta de nueve sesiones que involucran psicoeducación, regulación emocional y habilidades de afrontamiento, exposición imaginada basada en escritos, reestructuración cognitiva y prevención de recaídas. Los participantes serán guiados por un eCoach, que proporcionará comentarios escritos semiestandarizados semanales sobre las sesiones completadas y recordatorios de adherencia. Usaremos un marco de factibilidad formal para evaluar las diferentes dimensiones de factibilidad: (1) capacidad de reclutamiento y características de la muestra resultante, (2) procedimientos de recopilación de datos y de las medidas del resultado, (3) aceptabilidad de la IMI y los procedimientos del estudio, (4) recursos y capacidad para gestionar e implementar el estudio y la IMI y (5) las respuestas de los participantes a la IMI en términos de la gravedad de los síntomas y la satisfacción. Además, se evaluarán los posibles efectos negativos relacionados con la intervención. Las evaluaciones se realizan antes, durante y después de la intervención y durante el seguimiento, incluyendo entrevistas telefónicas clínicas semiestructuradas para el diagnóstico de TEPT en la evaluación previa y posterior a la intervención. Se realizarán entrevistas cualitativas para investigar las perspectivas de los jóvenes sobre la IMI.
Discusión: Este estudio tiene como objetivo determinar la factibilidad de una IMI guiada para jóvenes con TEPT para adaptar la IMI lo más cerca posible a las necesidades de los jóvenes y para informar el diseño, el procedimiento y la gestión de la seguridad de un ECA de eficacia a gran escala.
引言:尽管存在针对青少年和年轻人的创伤后应激障碍 (PTSD) 循证治疗,由于结构和态度障碍,患病青少年无法充分获得这些治疗。基于互联网和移动设备的干预措施 (IMI) 可以帮助填补这一医护空白,但此类计划尚未在PTSD 青年患者中得到充分评估。
目的:本研究旨在于一项单臂、非随机、前瞻性的可行性概念验证研究中考查 IMI 对 PTSD 青年患者的可行性。
方法:我们旨在招募 32 名年龄在 15 至 21 岁之间、具有临床相关创伤后应激症状 (CATS > 21) 的青年,他们将获得 IMI。 IMI 由九个课程组成,涉及心理教育、情绪调节和应对技巧、基于书面的想象暴露、认知重组和预防复发。参与者将由一名对已完成课程提供每周半标准化书面反馈和遵守提醒的电子教练指导。我们将使用正式的可行性框架来评估可行性的不同维度:(1) 招募能力和由此产生的样本特征,(2) 数据收集过程和结果测量,(3) IMI 和研究程序的可接受性,(4) 管理和实施研究与 IMI 的资源和能力,以及 (5) 参与者在症状严重程度和满意度方面对 IMI 的反响。此外,将评估干预相关的潜在负面影响。评估在干预前、中、后和随访中进行,包括干预前、后评估中对 PTSD 诊断进行半结构化临床电话访谈。将进行定性访谈以调查青年对 IMI 的看法。
讨论:本研究旨在确定为PTSD 青年患者提供指导性 IMI 的可行性,以使 IMI 尽可能适应青少年的需求,并为大规模疗效 RCT 的设计、程序和安全管理提供信息。
1. Theoretical background
More than 10% of adolescents and young adults (referred to collectively as ‘youth’ in this paper) experience at least one traumatic event, such as serious injury, abuse or physical assault (Pillhofer, Ziegenhain, Nandi, Fegert, & Goldbeck, Citation2011). About 16% of youth who have experienced a potentially traumatic event develop a PTSD (Alisic et al., Citation2014). A prevalence study estimated the lifetime prevalence for PTSD in youth to be around 1.3% and showed a strong association between PTSD and other mental disorders such as depression and anxiety (Perkonigg, Kessler, Storz, & Wittchen, Citation2000). If PTSD symptoms are left untreated, they often persist (Scheeringa, Zeanah, Myers, & Putnam, Citation2005; Yule et al., Citation2000) and have a negative impact on the psychosocial, emotional and academic development, placing a high burden on both the individual and society (Dams et al., Citation2020; Habetha et al., Citation2012; Makley & Falcone, Citation2010; Ogle, Rubin, & Siegler, Citation2013; Porche, Fortuna, Lin, & Alegria, Citation2011). To prevent long-term consequences, timely treatment options should be available for affected individuals when needed.
International and national treatment guidelines (ISTSS Guidelines Committee, Citation2019; National Institute for Health and Care Excellence, Citation2018; Phoenix Australia Centre for Posttraumatic Mental Health, Citation2020; Schäfer et al., Citation2019) consistently recommend trauma-focused cognitive–behavioural therapy (tf-CBT) for treating youth PTSD. Psychological approaches based on tf-CBT, compared to waitlist conditions, have been shown to be effective in reducing PTSS, with small effects of d = 0.37 for family therapy to large effects of d = 1.17 for tf-CBT developed by Cohen and colleagues or cognitive processing therapy and d = 2.94 for cognitive therapy (Mavranezouli et al., Citation2020). Tf-CBT has been shown to decrease dysfunctional posttraumatic cognitions and also comorbid depression and anxiety (Goldbeck, Muche, Sachser, Tutus, & Rosner, Citation2016). In addition, an increase in the quality of life of youths after tf-CBT was observed (Aas, Iversen, Holt, Ormhaug, & Jensen, Citation2019).
However, the dissemination of evidence-based trauma-focused psychotherapy in routine care is limited (Kazlauskas et al., Citation2016; Rosner et al., Citation2020). Lack of training, negative attitudes towards evidence-based practices (Lilienfeld, Ritschel, Lynn, Cautin, & Latzman, Citation2013), fears that trauma exposure may lead to an exacerbation of symptoms, dysfunctional behaviour (e.g. suicidality) and treatment dropout (Becker, Zayfert, & Anderson, Citation2004; Finch, Ford, Grainger, & Meiser-Stedman, Citation2020; van Minnen, Hendriks, & Olff, Citation2010) are some reasons therapists resist offering trauma-focused treatment. In addition, attitudinal barriers may prevent youth from accessing treatment. Such barriers include fear of stigmatisation, feelings of shame and a preference for self-help (Gulliver, Griffiths, & Christensen, Citation2010; Rosner et al., Citation2020). Moreover, structural barriers to treatment utilisation for youth include long waiting times (BPtK, Citation2018), long distances to the nearest practice, dependence on public transportation or other people for travel, lack of knowledge about available services and problems navigating the healthcare system (Gulliver et al., Citation2010).
Internet- and mobile-based interventions (IMIs) can help to overcome some of the current limitations of the healthcare system regarding trauma-focused treatment. IMIs are defined as self-help-based interventions delivered via the Internet with or without a form of guidance (Ebert et al., Citation2018). When compared to face-to-face therapy, the advantages of IMIs include increased (1) accessibility, (2) scalability, (3) flexibility in place and time, (4) self-direction and self-pacing (Boulos, Brewer, Karimkhani, Buller, & Dellavalle, Citation2014; Lin, Ebert, Lehr, Berking, & Baumeister, Citation2013) and (5) anonymity. Given the high availability of mobile devices and Internet affinity among youth (Feierabend, Rathgeb, & Reutter, Citation2019; UNICEF, Citation2017), IMIs have the potential to reach young people in their familiar Internet environment earlier than traditional treatment approaches and may thus also reach youth who do not feel ready for face-to-face therapy.
IMIs have been shown to be effective in treating a range of mental health disorders in youth, including depression and anxiety (Ebert et al., Citation2015; Grist, Croker, Denne, & Stallard, Citation2019; Vigerland et al., Citation2016). For the treatment of youth with traumatic experiences, IMIs have not yet been sufficiently developed and evaluated. However, for PTSD in adults, guided IMIs following the principles of tf-CBT (i-tf-CBTs) are included in some treatment guidelines (ISTSS, Citation2019), as they have been shown to be efficacious in reducing PTSS (Kuester, Niemeyer, & Knaevelsrud, Citation2016; Sijbrandij, Kunovski, & Cuijpers, Citation2016; Steubl, Sachser, Baumeister, & Domhardt, Citation2021), with effects comparable in size to face-to-face CBT. Concerning PTSD in youth, only two pilot studies have evaluated i-tf-CBT so far in specific trauma populations. In a group of young Dutch victims of sexual violence (n = 7), an online programme consisting of ten writing sessions over 9–16 weeks showed promising improvements in PTSS and general psychopathology with medium-to-high within-group effect sizes (d = .70–1.1; de Haas, Hoing, Schrieken, Tsagana, Citation2009). Promising results have also been found in a group of young German survivors of long-term paediatric cancer (n = 20). After ten online writing sessions over 5 weeks, PTSS declined with a pre–post within-group effect size of d = .63 (Seitz, Knaevelsrud, Duran, Waadt, Loos, et al., Citation2014). To the best of our knowledge, there is no IMI that addresses PTSD in youth exposed to different types of trauma. Moreover, despite the initial promising results and high treatment satisfaction (Seitz, Knaevelsrud, Duran, Waadt, & Goldbeck, Citation2014), randomised controlled trials (RCTs) investigating the efficacy of i-tf-CBT in youth are currently lacking. Before conducting a RCT, investigating the feasibility of an i-tf-CBT within a proof-of-concept study could be beneficial to more clearly identify individual needs of youth with PTSD and to derive adaptations for a more tailored intervention and more economical study-design.
1.1. Objectives of the current trial
This study aims to investigate the feasibility of a guided trauma-focused IMI for PTSD in youth, irrespective of the nature of trauma experienced, in a one-arm proof-of-concept study as required for a subsequent large-scale RCT. Following the recommendations by Orsmond and Cohn (Citation2015), feasibility was evaluated in terms of the following specific dimensions: (1) recruitment capability and resulting sample characteristics; (2) data collection procedures and outcome measures; (3) acceptability of the IMI, i.e. adherence and study procedures; (4) resources and ability to manage and implement the study and IMI; and (5) participants’ preliminary responses to the IMI, i.e. in terms of symptom severity and satisfaction. Additionally potential negative effects related to the intervention (e.g. suicidality, symptom deterioration) will be assessed.
2. Methods
2.1. Trial design
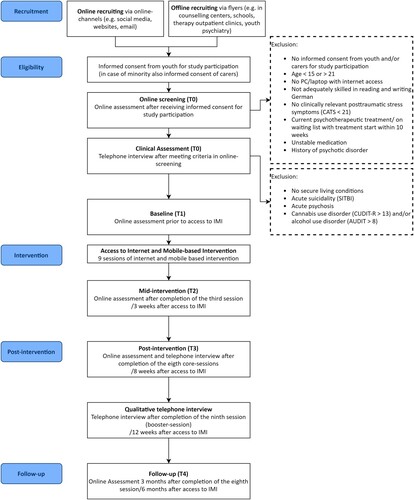
This is a proof-of-concept feasibility study with a one-arm, non-randomised design. The study will be reported in accordance with CONSORT guidelines for randomised pilot and feasibility trials and the complementary recommendations for conducting and reporting non-randomised pilot and feasibility studies (Eldridge et al., Citation2016; Lancaster & Thabane, Citation2019). The study flow is shown in . The study has been approved by the Ethics Committee of the German Psychological Society (DGPs, the Society, EbertDavidDaniel2020-09-16-VA) and is registered in the German Clinical Trial Registry (GCTR, DRKS00023341). This study is part of the collaborative BestForCan project, which aims at disseminating the tf-CBT developed by Cohen and colleagues (Cohen, Mannarino, & Deblinger, Citation2017) for children, adolescents and young adults after child abuse and neglect (Rosner et al., Citation2020). The study is funded by the Federal Ministry of Education and Research (BMBF, grant number 01KR1804D).
2.2. Participants
2.2.1. Inclusion and exclusion criteria
We will include youth who (a) suffer from clinically relevant PTSS measured with the Child and Adolescent Trauma Screen (CATS ≥ 21; Sachser et al., Citation2017), (b) complete a semi-structured clinical telephone interview in which a diagnosis of PTSD, amongst other aspects, will be assessed via on the Clinician-Administered PTSD Scale for DSM-5 (CAPS-CA 5; Pynoos et al., Citation2015), a clinician-rated PTSD diagnosis is, however, not required for study inclusion, (c) have secure living conditions, (d) are between 15 and 21 years old, (e) provide informed consent (in case of minors, both caregivers have to provide informed consent as well /in case of sole custody or legal custody, only one informed consent provided by the person with custody is sufficient for participation) digitally signed via email or by post, (f) have a laptop or computer with access to the Internet as the intervention is desktop-based and (g) are adequately skilled in reading and writing in German. Individuals will be excluded if they suffer from severe mental symptoms other than PTSS that require psychiatric treatment, namely, (h) history of psychotic disorder/acute psychosis measured by items adapted from the Diagnostic Interview for Mental Disorders for Children (Kinder-DIPS, Schneider, Pflug, In-Albon, & Margraf, Citation2017), (i) acute suicidality measured by items adapted from the Self-Injurious Thoughts and Behaviours Interview (SITBI, Nock, Holmberg, Photos, & Michel, Citation2007) or (j) alcohol use disorder as measured by the Alcohol Use Disorders Identification Test (AUDIT > 8; Saunders, Aasland, Babor, de la Fuente, & Grant, Citation1993) or cannabis use disorder as measured by the Cannabis Use Disorder Identification Test-Revised (CUDIT-R > 13; Adamson et al., Citation2010). In addition, we will exclude individuals (k) if their current medication started shortly before the study or is about to change during the study phase (within the subsequent 10 weeks) or (l) if they currently receive psychotherapy or are currently on a waiting list for psychotherapy starting within the next 10 weeks. Beyond these criteria, there are no further reasons for exclusion due to comorbidities.
2.2.2. Sample size
We calculated our sample size for evaluation of participants’ preliminary responses to the IMI in terms of PTSS. A sample size calculation conducted with G*Power (Version 3.1.9.4; Faul, Erdfelder, Lang, & Buchner, Citation2007) for a two-sided t-test for dependent groups revealed that 32 participants would be sufficient to detect pre–post changes within PTSS of d = 0.6 at a significance level of 0.05 with a statistical power of 0.90. For i-tf-CBT, only two reference studies in adolescent samples report medium-to-high pre–post effect sizes in reducing PTSS (d = .63; Seitz, Knaevelsrud, Duran, Waadt, Loos, et al., Citation2014; d = 1.0; de Haas, Höing, & Schrieken, Citation2009). As this is the first feasibility study to evaluate an IMI for PTSD in youth independent of trauma type, we conservatively estimated a medium effect size of d = 0.6. Taking into account that a number of twelve interviews is considered to be sufficient to induce data saturation in qualitative research (Guest, Bunce, & Johnson, Citation2006), the calculated sample size would allow to identify essential topics of the pre-defined meta-themes in the analysis of the qualitative interviews. To account for the expected high pre-treatment withdrawal from study participation, which has been observed in previous studies with a similar target group (Haas, Höing, & Schrieken, Citation2009; Lange & Ruwaard, Citation2010), we aim to screen N = 150 youth.
2.2.3. Recruitment
Youth will be recruited via various online (e.g. study webpage, webpage of the BestForCan study, Facebook, Instagram and TikTok) and offline channels (e.g. flyers in schools/counselling centres/therapy outpatient clinics/youth psychiatry). Interested individuals can contact the study team by leaving a valid email, a name (pseudonym) and their age on a contact form on the study webpage (http://hellobetter.de/star-studie/). The study team will then email prospective participants information on the procedure and conditions of participation, data security and their right to withdraw from the study at any time, along with an informed consent form. In case of minors, the email includes information and consent form for the caregivers/person with custody as well. Participants then have to provide their written informed consent, which includes providing an emergency contact. For minors, both caregivers/the person with custody also have to provide informed consent.
2.2.4. Eligibility
After providing informed consent, study eligibility will be assessed in a two-step procedure: in an initial online screening, study applicants will self-report on criteria (b)–(e), (h), (k) and (l). If these criteria are met, youth will be invited to a clinical assessment of criteria (f), (g), (i), (j) and (m) via a semi-structured clinical telephone interview conducted by a licensed psychotherapist. In addition, the incidence of other (serious) adverse events within the last 6 months and resulting possible contraindications (e.g. upcoming court case, upcoming imprisonment) for study participation will be assessed. Prospective participants will also develop a stepped emergency plan and consent to an anti-suicide contract for the study period. After completion of the interview, the psychotherapists will provide their clinical judgement on final study eligibility based on the collected interview data and their clinical expertise. If an individual is decided to be eligible for the study, they will be invited to the baseline assessment (T1). After completing the baseline assessment, all participants will receive an account on the intervention platform, which can be autonomously accessed via private login data. Excluded youth get the offer discussing appropriate help offers within a further telephone interview with a study team member and they receive a list of individualised on-site help offers for their region of residence via email.
2.3. Internet- and mobile-based intervention
2.3.1. Treatment principles and development
The IMI follows the principles of tf-CBT and includes the key components of existing first-line face-to-face treatments for PTSD such as (1) psychoeducation, (2) emotion regulation and coping skills, (3) imaginal exposure to the traumatic event and (4) cognitive restructuring (Dorsey, Briggs, & Woods, Citation2011; Schnyder et al., Citation2015). Treatment components were drawn from evidence-based treatment manuals for PTSD (Cohen et al., Citation2017; Rosner, König, Neuner, Schmidt, & Steil, Citation2014; Seitz, Knaevelsrud, Duran, Waadt, & Goldbeck, Citation2014; Sloan & Marx, Citation2019; Spence et al., Citation2011), dialectical behavioural therapy (DBT; Linehan, Citation2014) and self-help materials for PTSD (Williams & Poijula, Citation2012). Psychotherapists experienced in treating youth with PTSD and experts in developing IMIs adapted the treatment components for Internet-based guided self-help use and to the needs of youth.
2.3.2. Structure and session content
The IMI is divided into three thematic units: (1) safety and coping skills, (2) trauma processing and (3) consolidation/integration over nine sessions (eight core sessions and one booster session 4 weeks after completion of the core sessions). The length of one session is estimated between 30 and 60 min. Participants are advised to complete one session per week (12 weeks in total). For an overview of the content of single sessions, see Table A1 (Appendix).
2.3.2.1. Safety and coping skills (Sessions 1–3)
In Session 1, participants are encouraged to clarify their treatment motives and define personal treatment goals. They then receive psychoeducation about traumatic experiences and PTSS and information about the rationale of trauma-focused therapy. In Session 2, participants learn about physiological arousal effects of trauma and practice relaxation skills for different levels of arousal (e.g. self-soothing techniques and distress tolerance skills). Session 3 starts with psychoeducation about emotions and basic principles of cognitive coping. Participants are then encouraged to try an acceptance-based approach for dealing with overwhelming negative emotions.
2.3.2.2. Trauma processing (Sessions 4–6)
In each trauma processing session, participants are encouraged to write for 30 min about their most impactful traumatic experience in report form. In Session 4, imaginal exposure of the traumatic event starts with the first of three written trauma narratives from a neutral observer perspective without immersing themselves too deep into their emotions and thoughts. In Session 5, participants are asked to write the trauma narrative from a first-person perspective, including more details. In their last report in Session 6, participants are asked to add detailed, specific thoughts and feelings to their report. In each session, the coping strategies learned in session 2 and 3 are presented again and participants are encouraged to pay attention to their stress levels and to use the techniques learned if needed.
2.3.2.3. Consolidation/Integration (Sessions 7–9)
In Session 7, maladaptive thoughts about the trauma and trauma consequences are identified and restructured using cognitive restructuring techniques (e.g. change of perspective, probability analysis). In addition, participants are guided to develop new positive and helpful thoughts. Session 8 conveys principles of relapse prevention: participants develop personal strategies to deal with critical trauma-related situations in their future, can inform themselves about posttraumatic growth and are encouraged to think about positive changes or factors that manifested after trauma exposure or during trauma mastery. The booster Session 9 concludes the IMI by reviewing key components and by giving participants the opportunity to realign their personal goals.
2.3.3. Web-based implementation
The IMI is located on an eHealth intervention platform accessible via a web browser from a computer. A web-based session consists of written content with optional drop-down sections (‘read more’, ‘tips’) to facilitate further reading or support, if needed. Illustrative pictures, videos and audio are integrated to use a wide range of learning techniques and address different learning types. To ensure the usability of the IMI and to enhance a sense of active participation and autonomy, participants receive tailored answers to their written statements and choose between or add their own response options during exercises. To personalise the IMI, information already provided by participants (e.g. type of trauma) will be referred to in later sessions. Further, three fictional case descriptions are introduced, whose characters vary in age, gender, ethnicity and type of trauma experienced, e.g. physical violence, sexual assault and car accident. Between sessions, participants are encouraged to work on the exercise for daily life, which aims to facilitate the transfer of treatment content into everyday life. Participants are also advised to keep a diary and to (re)activate their individual resources (e.g. completing sports, meeting friends, taking a walk). To support regular use of the diary and daily planning of resources, participants can download a complementary smartphone app to use the diary. All materials (documents or audio files) relevant for completing the exercises in daily life and a summary of the session completed can be downloaded at the end of each session.
2.3.4. Guidance
Participants receive content-focused feedback, including guidance by an eCoach, throughout the intervention. The eCoach sends individualised and semi-standardised written feedback on completed sessions according to a manual via the online platform, as well as adherence reminders in case a module is not completed within 7 days (Zarski et al., Citation2016). The feedback has the primary purpose of potential crisis monitoring and supporting, encouraging and motivating participants, as well as promoting adherence to the intervention and, if necessary, offering guidance or discussing open questions. The eCoaches are psychotherapists in training who are trained for eCoaching as part of the study and will be supervised by a licensed psychotherapist with extensive clinical expertise in treating youth with PTSD. In addition, participants can receive further support from a licensed psychotherapist via telephone if needed.
2.4. Assessments
2.4.1. Points of assessments
Assessments are planned for screening (self-rated online assessment and clinician-rated telephone interview), at baseline (T1; self-rated online assessment prior to IMI access), mid-intervention (T2; self-rated online assessment after completion of the third session, or 3 weeks after IMI access), post-intervention (T3; self-rated online assessment and clinician-rated telephone interview after completion of the eight core sessions, or 8 weeks after IMI access) and at follow-up (T4; self-rated online assessment 6 months after IMI access). A qualitative telephone interview will take place after completion of the booster session, or 12 weeks after IMI access. The online assessments will be conducted via a secure online platform. All interviews will be scheduled via an online timetable and will be recorded. On the intervention platform, we will collect feedback on completed sessions and track objective user data. For an overview of measures and assessments, see . Participants will receive incentives in the form of vouchers for the completion of the baseline assessment (T1; €15) and follow-up (T4; €15), resulting in a total compensation of €30 for study completion.
Table 1. Constructs with measures and points of assessment.
2.4.2. Screening measures
PTSSs are assessed by the CATS (20 items; score range: 0–40; Sachser et al., Citation2017), which screens for exposure to potentially traumatic events with 15 items. The following 20 items directly map onto the DSM-5 criteria for PTSD, including the subscales ‘re-experiencing’ (five items; score range: 0–15), ‘avoidance’ (two items; score range: 0–6), ‘negative alterations in cognition and mood’ (seven items; score range: 0–21) and ‘hyperarousal’ (six items; score range: 0–18), with higher scores indicating higher symptom severity. Reliability of the CATS is reported to be excellent in German youth who experienced a traumatic event (α = .90; Sachser et al., Citation2017).
Diagnosis of PTSD is evaluated with the CAPS-CA 5 (30 items; Pynoos et al., Citation2015). No studies have evaluated the psychometric properties of the German version used in this study. The German version of the CAPS-CA IV showed good inter-rater reliability (k = .68) and high internal consistency of the total symptom score (α = .79) in adolescents with PTSD (Sachser et al., Citation2017). The CAPS-CA 5 showed high internal consistency (α = .89) in a sample of Portuguese adolescents (Barroca et al., Citation2022).
Acute psychotic symptoms are measured with items adapted from the Kinder-DIPS (5 items; Schneider et al., Citation2017), and history of psychotic disorders is assessed using one self-developed item (‘Have you ever been treated for, or diagnosed with, psychosis or schizophrenia by a doctor?’).
Acute suicidality is measured using items from the SITBI (nine items; Nock et al., Citation2007).
Alcohol use disorder is measured by the AUDIT (ten items; score range: 0–40; cutoff for alcohol dependency disorder > 8; Saunders et al., Citation1993), which has excellent reliability in German adults (α = .95; Dybek et al., Citation2006) and also satisfactory reliability in German sample of healthy students (α = .77; Rumpf, Wohlert, Freyer-Adam, Grothues, & Bischof, Citation2013).
Cannabis use disorder is measured by the CUDIT-R (ten items; score range: 0–40; cutoff for cannabis dependency disorder > 13; Adamson et al., Citation2010), which similarly shows excellent reliability in adults in New Zealand (α = .91; Adamson et al., Citation2010). The reliability has been shown to be excellent within a cross-cultural validation study among English and Spanish speaking healthy students (α = .82; Mezquita, Bravo, Pilatti, Ortet, & Ibáñez, Citation2022).
Living conditions are assessed using three clinician-rated self-developed items assessing whether the adolescents feel safe, are exposed to any threat at home or in their close environment or have trauma-related perpetrator contact.
2.4.3. Feasibility measures
2.4.3.1. Recruitment capability and resulting sample characteristics
Recruitment data will be tracked based on the number of people who access the website applying for study participation and in addition to the use of different recruitment channels.
Sociodemographics (e.g. gender, residence, education level) and help-seeking behaviour will be assessed with standard and self-developed items.
2.4.3.2. Data collection procedures and outcome measures
Comprehensibility of the items, stress associated with the assessments and time required for data collection are assessed with self-developed items.
2.4.3.3. Acceptability of the IMI and the study procedures
Attitudes towards IMIs in general are assessed by the Attitudes Towards Psychological Online Interventions Questionnaire (APOI; 16 items; Schröder et al., Citation2015), including the subscales scepticism/perception of risks (4 items, score range: 4–20) and technologisation threat (4 items, score range: 4–20), confidence in effectiveness (4 items, score range: 4–20) and anonymity benefits (4 items, score range: 4–20). Higher scores on the total scale indicate a more positive attitude towards IMIs. Reliability of the subscales has been shown to be acceptable in a sample of adults in Germany (α = .62–.72; Schröder et al., Citation2015).
Study adherence is measured by the number of completed online (k = 5) and telephone assessments (k = 3).
Intervention adherence is assessed based on objective user data from the intervention platform (i.e. number of modules completed, number of logins with timestamps) and via self-reported engagement and acceptance (i.e. number of times the exercise is performed in everyday life, compatibility of exercises with daily life). We will report the percentage of interventions completed and number of intervention completers.
Overall acceptability of the IMI is assessed based on seven open-ended questions in the qualitative interview concerning the acceptability dimensions of a treatment, as recommended by Sekhon, Cartwright, and Francis (Citation2017) including (1) affective attitude, (2) burden, (3) ethicality, (4) intervention coherence, (5) opportunity costs, (6) perceived effectiveness and (7) and self-efficacy.
Acceptability of individual sessions is measured by four self-report items on the usefulness, feasibility, comprehensibility and aesthetics assessed on the intervention platform at the end of each session.
2.4.3.4. Resources and ability to manage and implement the study and IMI
Extent and intensity of guidance provided in this study is measured by eCoaching data (e.g. time spent on guidance, number) and intensity of additional support (e.g. number of telephone contacts with a clinician).
Extent and intensity of study administration is assessed by data from clinical interviews (e.g. time required for diagnostic interviews) and administrative contact with the study team (e.g. number of study adherence reminders sent).
2.4.3.5. Preliminary evaluation of participant responses to the IMI
In addition to its use as a screening tool, the CATS is also used to measure PTSS and the CAPS-CA 5 to assess PTSD diagnosis at post-treatment and follow-up.
Depressive symptoms will be assessed by the Patient Health Questionnaire (PHQ-9; 9 items; score range: 0–27 Kroenke, Spitzer, & Williams, Citation2001), referring to the previous 2 weeks, with higher scores indicating higher symptom severity. The PHQ-9 has demonstrated excellent reliability in a German sample of youth with depression (α = .90; Sachser et al., Citation2017).
Anxiety symptoms will be assessed using the Generalized Anxiety Disorder Assessment (GAD-7; seven items; score range: 0–21; Spitzer, Kroenke, Williams, & Löwe, Citation2006), referring to the previous 2 weeks, with higher scores indicating higher symptomatology. The GAD-7 has revealed excellent reliability in a German sample of youth with anxiety disorders (α = .90; Sachser et al., Citation2017).
Health-related quality of life is assessed by the KIDSCREEN-10-Index (ten items; score range: 0–40; Ravens-Sieberer et al., Citation2010), with lower scores indicating unhappiness and dissatisfaction regarding peers, family and school life (Ravens-Sieberer et al., Citation2010). Its reliability has been shown to be good in German youth with traumatisation (α = .80; Weber, Jud, Landolt, & Goldbeck, Citation2017).
Posttraumatic cognition will be assessed by the Child Posttraumatic Cognitions Inventory Short Version (CPTCI-SF; ten items; McKinnon et al., Citation2016) including the subscales ‘permanent and disturbing change’ (six items, score range: 6–24) and ‘fragile person in a scary world’ (four items, score range: 4–16). The CPTCI-SF has shown excellent reliability in youth in England, East Anglia and Australia who have been exposed to a traumatic event in the last six months (α = .92; McKinnon et al., Citation2016).
Treatment satisfaction is assessed with the Client Satisfaction Questionnaire adapted for Internet interventions (CSQ-I; eight items, score range: 8–32; Attkisson & Zwick, Citation1982; Boß et al., Citation2016), with higher scores indicating greater satisfaction with the IMI. The scale showed good psychometric properties in German adults with stress-elevated or depressive symptoms (McDonald’s omega = .93–.95; Boß et al., Citation2016).
2.4.3.6. Evaluation of potential risks and possible negative effects
Suicidality will be assessed by the suicide item 9 of the Beck Depression Inventory-II: This questionnaire consists of 21 groups of statements. Please read each group of statements carefully. And then pick out the one statement in each group that best describes the way you have been feeling during the past two weeks, including today. with answers options for item 9 ‘suicidal thoughts or wishes’: ‘I don't have any thoughts of killing myself.’ (0), ‘I have thoughts of killing myself, but I would not carry them out.’ (1), ‘I would like to kill myself’ (2), and ‘I would kill myself if I had the chance’ (3) (BDI-II item 09; score range: 0–3; Hautzinger, Keller, & Kühner, Citation2006).
Potential negative effects of the IMI will be assessed using the Negative Effects Questionnaire (NEQ; 20 items; Rozental, Kottorp, Boettcher, Andersson, & Carlbring, Citation2016). The NEQ measures the frequency (score range: 0–20) and impact (score range: 0–80) of different negative effects during the treatment period. Internal consistency of the NEQ is reported to be excellent (α = .95) in Swedish adults (Rozental et al., Citation2016).
Other (serious) adverse events and their association with intervention participation are systematically assessed with self-developed items. Incident of (S)AEs is documented by the study personnel and will be forwarded to the principal investigator of the study. Adverse events are defined as unintended symptoms or conditions that are inconsistent in nature or severity with the present information about the effects of the intervention (Rozental et al., Citation2014). Serious adverse events are defined as (1) emergency hospitalisation due to mental illness; (2) involuntary breakdown of a close, important relationship; (3) intoxication with a psychotropic substance requiring medical care; (4) self-injury (intentional) requiring medical care; (5) suicide or suicide attempt; (6) acute psychosis; (7) delinquent behaviour; (8) aggression towards persons or objects; and (9) insecure living conditions.
Deterioration of PTSS during study participation will be assessed as a possible risk with the CATS at pre-, mid-, and post-intervention, and at follow-up.
2.5. Safety management
As a prerequisite for participation, youth need to (1) list an adult emergency contact in their informed consent who is verified and informed about the study by study administrators, (2) develop a stepped emergency plan and (3) consent to the anti-suicide contract in the telephone screening (T0). Furthermore, (4) youth with acute suicidal intentions or plans are identified during the telephone screening, excluded from participation and referred to alternative mental health services in their area of residence. During study participation, participants can report suicidal ideation during IMI sessions, within online assessments (T2 and T4) by scoring > 0 on BDI-II item 9 (Hautzinger et al., Citation2006) and during telephone interviews. They are also encouraged to discuss any negative changes in their mood and behaviour with their eCoach via private chat. If a serious adverse event is identified in any of the monitoring modes, participants will receive a reminder of their emergency plan and will be called by a licensed psychotherapist, with whom immediate coping strategies can be discussed in addition to more intensive, stepped-up treatment as necessary. Finally, if necessary, the emergency contact will be informed. With regard to PTSS deterioration, there are no criteria (cutoff scores) pre-defined, which will cause study discontinuation or immediate referral to on-site psychotherapy. Instead, participants reporting a significant and persistent worsening of their symptoms (via private Chat with their eCoaches or via email to the studyteam) get offered a telephone consultation with the study therapists. Within this consultation, if consistent with the clinical judgment of the therapist, on-site therapy and study discontinuation may be recommended.
2.6. Statistical analysis
Following the guidelines for reporting non-randomised pilot and feasibility studies, all primary analyses will be based on the per protocol principle (Lancaster & Thabane, Citation2019). In addition, we will analyse the data based on the intention-to-treat principle to reduce bias. Analyses will be performed using R statistics software (R Core Team, Citation2009). The significance level for all analyses will be set to 0.05. All analysis will be explorative. We will report descriptive statistics for all outcomes at each timepoint (i.e. mean and standard deviations for continuous outcomes, counts and percentages for categorical outcomes). We will report descriptive statistics for all outcomes at each timepoint (i.e. mean and standard deviations for continuous outcomes, counts and percentages for categorical outcomes). Regarding the preliminary evaluation of participant responses to the intervention in terms of posttraumatic symptom severity (CATS), depressive symptoms (PHQ-9), anxiety symptoms (GAD-7), health-related quality of life (KIDSCREEN), and posttraumatic cognitions (CPTCI-SF), group differences between pre- (T1) and post- intervention (T3), between pre-intervention (T1) and follow-up (T4), as well as between post-intervention (T3) and follow-up (T4) will be analysed using a two-sided t-test for dependent groups. Cohen’s d within-group-effect sizes and their 95% CIs will be reported (Hedges & Olkin, Citation1985). Additionally, we will calculate the reliable change index (RCI) (Jacobson & Truax, Citation2004) from pre- (T1) to post-intervention (T3), from pre-intervention (T1) to follow-up (T4) as well as from post-intervention (T3) to follow up (T4) to test for clinically significant improvement and deterioration of PTSS on a single person level. Additionally, the frequency of occurrence of negative effects and their association to intervention participation will be analysed.
2.7. Analysis of qualitative interviews
Qualitative semi-structured interviews will be conducted via telephone interviews to assess patient perspectives on the intervention regarding expectations, acceptability as suggested by Sekhon et al.’s (Citation2017) criteria, content and quality, perceived usefulness and efficacy, mechanisms of change, individual fit, guidance, active engagement and adherence and safety. All qualitative data will be audiotaped and transcribed verbatim using the software MAXQDA. The evaluation relies on qualitative content analyses, following Mayring (Citation2010) and Kuckartz, Ebert, Rädiker, and Stefer (Citation2009). Two independent raters will code all transcripts based on the coding guide so that inter-rater agreement can be calculated as a measure of the reliability of the results.
3. Discussion
With this study, we aim to develop and evaluate an IMI for youth with PTSD. To determine the feasibility of delivering the IMI and conducting a follow-up RCT, we will use a formal feasibility framework for our evaluation, considering recruitment capability and sample characteristics, data collection procedures and outcome measures, acceptability of the IMI and study procedures and resources and capacity for study management and implementation, together with participants’ responses to the IMI, i.e. in terms of symptom severity and potential negative effects (Orsmond & Cohn, Citation2015). The results derived from this feasibility study will be of particular importance to adapt the IMI even more closely to the needs of youth and to inform the design, procedure and safety management of the subsequent RCT.
This feasibility study has several strengths. It will significantly contribute to the literature and empirically tested IMIs for PTSD in youth, because, to the best of our knowledge, it is the first to investigate the feasibility of a guided trauma-focused IMI for the treatment of PTSD in youth. Participation in the study and IMI is low threshold, due to the online format (e.g. flexibility in time and place, enhanced feeling of anonymity due to the lack of face-to-face contact). In contrast with traditional face-to-face therapy, the IMI has the potential to overcome barriers (e.g. stigma, shame) which youth report when seeking treatment (Gulliver et al., Citation2010; Rosner et al., Citation2020). The IMI delivers treatment based on the principles of tf-CBT, which are among first-line treatment recommendations for PTSD in youth. Compared to existing programmes, this IMI addresses a large group of trauma-exposed youth by including all types of trauma. Implementation and delivery of such an IMI if it shows to be effective might be from particular importance to further disseminate evidence-based trauma-focused methods and a way to reach youth at a lower threshold earlier than traditional treatment. Thus, IMIs could be a first step into treatment or to be used for bridging waiting times for on-site psychotherapy in addition to stand-alone application.
This study has the following limitations: First, selection bias might occur due to the necessity of providing written informed consent of both caregivers among underage youth due to ethical considerations and data regulations. For that reason, underage youth with inner familiar trauma might not be able to participate because they might not receive consent for study participation from their parents. Second, not all instruments selected were validated in German adolescent samples. Further, we had to keep the number of questionnaires and items limited to ensure the economic feasibility of the assessments in youth. Therefore, we decided to use the short version of the PTCI and we did not include measures for assessing potential mediators. Third, we did not include measures to distinguish between the diagnosis PTSD and complex PTSD. Future studies should use the longer version of the CPTCI, as it is more likely to capture the cognitions of adolescents with multiple traumatisation and should assess mediating constructs such as emotion regulation (Sharma-Patel & Brown, Citation2016). Furthermore, both the diagnosis of PTSD and complex PTSD, should be assessed in future studies, e.g. with the International Trauma Questionnaire (Cloitre, Hyland, Prins, & Shevlin, Citation2021). The generalizability of the sample might be limited due to the necessity of having access to a laptop/PC. Developing a version adaptive for mobile devices was not possible for our intervention due to technical requirements. Concerning the high user rate of mobile phones within youth, the possibility of developing a desktop and mobile-based intervention should be investigated in future research.. Furthermore, the generalizability of the study results will be limited to German-speaking youth without recent severe self-injurious behaviour, acute suicidality and substance dependence. Concerning a possible transfer of the study results into other health care system, further research should investigate the need for cultural adaptations of the intervention first (Heim & Kohrt, Citation2019). A culture-sensitive i-tf-CBT may have the potential to improve health care especially in underserved populations or war-afflicted areas. Finally, since the study is a feasibility study without a control group and randomisation, no conclusions can be drawn about its efficacy in reducing PTSS. Consequently, the follow-up is restricted to 3 months and thus does not provide information about long-term effects. If the feasibility trial is successful, a subsequent robust RCT is necessary to evaluate the efficacy of the IMI in reducing PTSS and PTSD. Further studies and analyses are needed to understand for which youth an IMI is effective and under what circumstances, as well as how the IMI can be optimised to improve individualised fit.
To conclude, an IMI for youth with PTSD has the potential to reach traumatised adolescents with evidence-based care earlier, and at a lower threshold, as compared to traditional approaches. Therefore, it may reduce disease burden and healthcare costs both at an individual and societal level.
Availability of data and material
Upon request from the authors.
Consent for publication
All authors have read the manuscript and approved its publication.
Date of first enrolment
04 August 2021
Ethics approval and consent to participate
The DGPs approved the research protocol (DGPs, the Society, EbertDavidDaniel2020-09-16-VA). The consent to participate is available in German and was reviewed by the Institutional Review Board.
Supplemental Material
Download MS Word (49.1 KB)Acknowledgements
We would like to acknowledge Thorsten Sukale, Verena Schmitz and Emilia Pekarek for contributing to development of the IMI, as well as study implementation and administration. All authors have read and approved the final manuscript. DE is the principal investigator of the study. CeS drafted the original design of the study for the grant application and advised CS and AZ on the design of the intervention. AZ and CS developed and implemented the intervention, will conduct the study and drafted the manuscript.
Disclosure statement
Christina Schulte (CS), Cedric Sachser (CeS), Anna-Carlotta Zarski (AZ) and Rita Rosner have nothing to disclose. David Daniel Ebert (DE) reports other from Get.On Institute, personal fees from Sanofi, personal fees from Novartis, personal fees from Minddistrict, personal fees from Lantern, personal fees from Schoen Kliniken, personal fees from Ideamed, grants from EU H2020, grants from BMBF, outside the submitted work; and Dr. Ebert has served as a consultant to/on the scientific advisory boards of Sanofi, Novartis, Minddistrict, Lantern, Schoen Kliniken, Ideamed and German health insurance companies (BARMER, Techniker Krankenkasse) and a number of federal chambers for psychotherapy. He is also a stakeholder in the institute for health training online (formerly GET.ON, now HelloBetter), which aims to implement scientific findings related to digital health interventions into routine care. HelloBetter distributes the Internet platform for the digital intervention under study.
Data availability statement
As this manuscript describes a study protocol, provision of a dataset is not applicable. Instead, we provide a trial registration: German Clinical Trial Registry (GCTR, DRKS00023341), Registered 20 July 2021, https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00023341
Additional information
Funding
References
- Aas, E., Iversen, T., Holt, T., Ormhaug, S. M., & Jensen, T. K. (2019). Cost-effectiveness analysis of trauma-focused cognitive behavioral therapy: A randomized control trial among Norwegian youth. Journal of Clinical Child and Adolescent Psychology, 48(sup1), S298–S311. doi:10.1080/15374416.2018.1463535
- Adamson, S. J., Kay-Lambkin, F. J., Baker, A. L., Lewin, T. J., Thornton, L., Kelly, B. J., & Sellman, J. D. (2010). An improved brief measure of cannabis misuse: The Cannabis use disorders identification test-revised (CUDIT-R). Drug and Alcohol Dependence, 110(1–2), 137–143. doi:10.1016/j.drugalcdep.2010.02.017
- Alisic, E., Zalta, A. K., Van Wesel, F., Larsen, S. E., Hafstad, G. S., Hassanpour, K., & Smid, G. E. (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: Meta-analysis. In British journal of psychiatry (Vol. 204, Issue 5, pp. 335–340). Royal College of Psychiatrists. doi:10.1192/bjp.bp.113.131227
- Attkisson, C. C., & Zwick, R. (1982). The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning, 5(3), 233–237. doi:10.1016/0149-7189(82)90074-X
- Barroca, I., Velosa, A., Cotovio, G., Santos, C. M., Riggi, G., Costa, R. P., … Carvalho, P. S. (2022). Translation and validation of the clinician administered PTSD Scale (CAPS-CA-5) for Portuguese children and adolescents. Acta Medica Portuguesa, 35, 13. doi:10.20344/amp.16718
- Becker, C., Zayfert, C., & Anderson, E. (2004). A survey of psychologists attitudes towards and utilization of exposure therapy for PTSD. Behaviour Research and Therapy, 42, 277–292. http://digitalcommons.trinity.edu/psych_faculty/7. doi:10.1016/S0005-7967(03)00138-4
- Boß, L., Lehr, D., Reis, D., Vis, C., Riper, H., Berking, M., & Ebert, D. D. (2016). Reliability and validity of assessing user satisfaction with web-based health interventions. Journal of Medical Internet Research, 18(8), e234. doi:10.2196/jmir.5952
- Boulos, K. M. N., Brewer, A. C., Karimkhani, C., Buller, D. B., & Dellavalle, R. P. (2014). Mobile medical and health apps: State of the art, concerns, regulatory control and certification. Online Journal of Public Health Informatics, 5(3), 229. doi:10.5210/ojphi.v5i3.4814
- BPtK. (2018). Ein Jahr nach der Reform der Psychotherapie-Richtlinie – Wartezeiten 2018. https://www.bptk.de/wp-content/uploads/2019/01/20180411_bptk_studie_wartezeiten_2018.pdf
- Cloitre, M., Hyland, P., Prins, A., & Shevlin, M. (2021). The international trauma questionnaire (ITQ) measures reliable and clinically significant treatment-related change in PTSD and complex PTSD. European Journal of Psychotraumatology, 12(1), doi:10.1080/20008198.2021.1930961
- Cohen, J. A., Mannarino, A. P., & Deblinger, E. (2017). Treating Trauma and Traumatic Grief in Children and Adolescents. New York: The Guilford Press.
- Dams, J., Rimane, E., Steil, R., Renneberg, B., Rosner, R., & König, H.-H. (2020). Health-related quality of life and costs of posttraumatic stress disorder in adolescents and young adults in Germany. Frontiers in Psychiatry, 11, 697. doi:10.3389/fpsyt.2020.00697
- Dorsey, S., Briggs, E. C., & Woods, B. A. (2011). Cognitive-behavioral treatment for posttraumatic stress disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America, 20(2), 255–269. doi:10.1016/j.chc.2011.01.006
- Dybek, I., Bischof, G., Grothues, J., Reinhardt, S., Meyer, C., Hapke, U., … Rumpf, H. J. (2006). The reliability and validity of the alcohol use disorders identification test (AUDIT) in a German general practice population sample. Journal of Studies on Alcohol, 67(3), 473–481. doi:10.15288/jsa.2006.67.473
- Ebert, D. D., Van Daele, T., Nordgreen, T., Karekla, M., Compare, A., Zarbo, C., … Baumeister, H. (2018). Internet- and mobile-based psychological interventions: Applications, efficacy, and potential for improving mental health. European Psychologist, 23, 167–187. doi:10.1027/1016-9040/A000318
- Ebert, D. D., Zarski, A. C., Christensen, H., Stikkelbroek, Y., Cuijpers, P., Berking, M., & Riper, H. (2015). Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: A meta-analysis of randomized controlled outcome trials. doi:10.1371/journal.pone.0119895
- Eldridge, S. M., Chan, C. L., Campbell, M. J., Bond, C. M., Hopewell, S., Thabane, L., … Tugwell, P. (2016). CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. The BMJ, 355, doi:10.1136/bmj.i5239
- Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. doi:10.3758/BF03193146
- Feierabend, S., Rathgeb, T., & Reutter, T. (2019). Jugend-Information-Medien-Studie 2019. Basisuntersuchung zum Medienumgang 12- bis 19-Jähriger. https://www.mpfs.de/studien/jim-studie/2019/
- Finch, J., Ford, C., Grainger, L., & Meiser-Stedman, R. (2020). A systematic review of the clinician related barriers and facilitators to the use of evidence-informed interventions for post traumatic stress. Journal of Affective Disorders, 263, 175–186. doi:10.1016/j.jad.2019.11.143
- Goldbeck, L., Muche, R., Sachser, C., Tutus, D., & Rosner, R. (2016). Effectiveness of trauma-focused cognitive behavioral therapy for children and adolescents: A randomized controlled trial in eight German mental health clinics. Psychotherapy and Psychosomatics, 85(3), 159–170. doi:10.1159/000442824
- Grist, R., Croker, A., Denne, M., & Stallard, P. (2019). Technology delivered interventions for depression and Anxiety in children and adolescents: A systematic review and meta-analysis. Clinical Child and Family Psychology Review, 22(2), 147–171. doi:10.1007/s10567-018-0271-8
- Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough?: An experiment with data saturation and variability. Field Methods, 18(1), 59–82. https://doi.org/10.1177/1525822X05279903
- Gulliver, A., Griffiths, K. M., & Christensen, H. (2010). Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry, 10(1), 1–9. doi:10.1186/1471-244X-10-113
- de Haas, S., Höing, M., & Schrieken, B. (2009). Internetbehandlung für jugendliche Opfer sexueller Gewalt: Eine Pilotstudie. Monatsmagazin. http://youth-of-today.wdfiles.com/local–files/artikel:jolien/Artikel_behandeling_via_het_internet_voor_jeugdige_slachtoffers_van_seksueel_geweld.docx
- de Haas, S., Hoing, M., Schrieken, B., Tsagana, A., Wijnker, C., & Michels, C. (2009). Behandeling via het internet voor jeugdige slachtoffers van seksueel geweld: Een pilotstudie [Online treatment of young victims of sexual violence: a pilot study]. MGV Maandblad Geestelijke Volksgezondheid, 64(11), 981–997. http://youth-of-today.wdfiles.com/local--files/artikel:jolien/Artikel_behandeling_via_het_internet_voor_jeugdige_slachtoffers_van_seksueel_geweld.docx
- Habetha, S., Bleich, S., Sievers, C., Marschall, U., Weidenhammer, J., & Fegert, J. M. (2012). Deutsche Traumafolgekostenstudie Kein Kind mehr-kein(e) Trauma(kosten) mehr? Schriftenreihe Band III. In dgfpi.de. https://www.dgfpi.de/tl_files/pdf/medien/2015-04-09_Publikat_Deutsche_Traumafolgekostenstudie_final_2.pdf
- Hautzinger, M., Keller, F., & Kühner, C. (2006). Beck depressions-inventar (BDI-II).
- Hedges, L., & Olkin, I. (1985). Statistical methods for meta-analysis. Academic Press. https://books.google.com/books?hl=de&lr=&id=7GviBQAAQBAJ&oi=fnd&pg=PP1&dq=Statistical+Methods+for+Meta-Analysis&ots=DxSSuP55dD&sig=ODipKj-0SLpVkPh5ZDZ4B4WzTe0
- Heim, E., & Kohrt, B. A. (2019). Cultural adaptation of scalable psychological interventions: A new conceptual framework. Clinical Psychology in Europe, 1(4), 1–22. doi:10.32872/cpe.v1i4.37679
- ISTSS Guidelines Committee. (2019). ISTSS PTSD prevention and treatment guidelines methodology and recommendations. https://istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-Treatment-Guidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- Jacobson, N. S., & Truax, P. (2004). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. In Methodological issues & strategies in clinical research (pp. 631–648). American Psychological Association. doi:10.1037/10109-042
- Kazlauskas, E., Javakhishvilli, J., Meewisse, M., Merecz-Kot, D., Şar, V., Schäfer, I., … Gersons, B. P. R. (2016). Trauma treatment across Europe: Where do we stand now from a perspective of seven countries. European Journal of Psychotraumatology, 7(1), doi:10.3402/ejpt.v7.29450
- Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi:10.1046/j.1525-1497.2001.016009606.x
- Kuckartz, U., Ebert, T., Rädiker, S., & Stefer, C. (2009). Evaluation online: internetgestützte Befragung in der Praxis. Verlag für Sozialwissenschaften. https://link.springer.com/content/pdf/10.1007/978-3-531-91317-9.pdf
- Kuester, A., Niemeyer, H., & Knaevelsrud, C. (2016). Internet-based interventions for posttraumatic stress: A meta-analysis of randomized controlled trials. In Clinical psychology review (Vol. 43, pp. 1–16). Elsevier Inc. doi:10.1016/j.cpr.2015.11.004
- Lancaster, G. A., & Thabane, L. (2019). Guidelines for reporting non-randomised pilot and feasibility studies. In Pilot and feasibility studies (Vol. 5, Issue 1, p. 114). BioMed Central Ltd. doi:10.1186/s40814-019-0499-1
- Lange, A., & Ruwaard, J. (2010). Ethical dilemmas in online research and treatment of sexually abused adolescents. Journal of Medical Internet Research, 12(5), e1455. doi:10.2196/jmir.1455
- Lilienfeld, S. O., Ritschel, L. A., Lynn, S. J., Cautin, R. L., & Latzman, R. D. (2013). Why many clinical psychologists are resistant to evidence-based practice: Root causes and constructive remedies. In Clinical psychology review (Vol. 33, Issue 7, pp. 883–900). Pergamon. doi:10.1016/j.cpr.2012.09.008
- Lin, J., Ebert, D. D., Lehr, D., Berking, M., & Baumeister, H. (2013). Internetbasierte kognitiv-behaviorale Behandlungsansätze: State of the Art und Einsatzmöglichkeiten in der Rehabilitation. Die Rehabilitation, 52(03), 155–163. doi:10.1055/s-0033-1343491
- Linehan, M. (2014). DBT skills training manual. Guilford Press. https://books.google.de/books?hl=de&lr=&id=VfMZBQAAQBAJ&oi=fnd&pg=PP1&dq=Linehan+MM+(2015a)+DBT+Skills+Training+Manual.+New+York,+Guilford+Press.&ots=CfkIHNGIST&sig=XdYXwiPX7H1YRFb3dI3UHu_b4rE&redir_esc=y#v=onepage&q&f=false
- Makley, A. T., & Falcone, R. A. (2010). Posttraumatic stress disorder in the pediatric trauma patient. Seminars in Pediatric Surgery, 19(4), 292–299. doi:10.1053/j.sempedsurg.2010.06.006
- Mavranezouli, I., Megnin-Viggars, O., Daly, C., Dias, S., Stockton, S., Meiser-Stedman, R., … Pilling, S. (2020). Research review: Psychological and psychosocial treatments for children and young people with post-traumatic stress disorder: A network meta-analysis. Journal of Child Psychology and Psychiatry, 61(1), 18–29. doi:10.1111/jcpp.13094
- Mayring, P. (2010). Qualitative Inhaltsanalyse. In G. Mey & K. Mruck (Eds.), Handbuch Qualitative Forschung in der Psychologie (pp. 601–613). Wiesbaden: VS Verlag für Sozialwissenschaften Springer.
- McKinnon, A., Smith, P., Bryant, R., Salmon, K., Yule, W., Dalgleish, T., … Meister-Stedman, R. (2016). An update on the clinical utility of the children’s posttraumatic cognitions inventory. Journal of Traumatic Stress, doi:10.1002/jts.22096
- Mezquita, L., Bravo, A. J., Pilatti, A., Ortet, G., & Ibáñez, M. I. (2022). Quantifying cannabis problems among college students from English and Spanish speaking countries: Cross-cultural validation of the Cannabis use disorders identification test-revised (CUDIT-R). Addictive Behaviors, 127, 107209. doi:10.1016/j.addbeh.2021.107209
- National Institute for Health and Care Excellence. (2018). Post- traumatic stress disorder (NICE guideline NG116): [B] Evidence reviews for psychological, psychosocial and other non-phar- macological interventions for the treatment of PTSD in children and young people. https://www.nice.org.uk/guidance/ng116/resources/posttraumatic-stress-disorder-pdf-66141601777861
- Nock, M. K., Holmberg, E. B., Photos, V. I., & Michel, B. D. (2007). Self-injurious thoughts and behaviors interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment, 19(3), 309–317. doi:10.1037/1040-3590.19.3.309
- Ogle, C. M., Rubin, D. C., & Siegler, I. C. (2013). The impact of the developmental timing of trauma exposure on PTSD symptoms and psychosocial functioning among older adults. Developmental Psychology, 49(11), 2191–2200. doi:10.1037/a0031985
- Orsmond, G. I., & Cohn, E. S. (2015). The distinctive features of a feasibility study: Objectives and guiding questions. OTJR: Occupation, Participation and Health, 35(3), 169–177. doi:10.1177/1539449215578649
- Perkonigg, A., Kessler, R. C., Storz, S., & Wittchen, H.-U. (2000). Traumatic events and post-traumatic stress disorder in the community: Prevalence, risk factors and comorbidity. Acta Psychiatrica Scandinavica, 101(1), 46–59. doi:10.1034/j.1600-0447.2000.101001046.x
- Phoenix Australia Centre for Posttraumatic Mental Health. (2020). Australian guidelines for the prevention and treatment of stress, disorder, posttraumatic stress disorder and complex PTSD.
- Pillhofer, M., Ziegenhain, U., Nandi, C., Fegert, J. M., & Goldbeck, L. (2011). Prävalenz von Kindesmisshandlung und -vernachlässigung in Deutschland. Kindheit Und Entwicklung, 20, 64–71. doi:10.1026/0942-5403/A000042
- Porche, M. V., Fortuna, L. R., Lin, J., & Alegria, M. (2011). Childhood trauma and psychiatric disorders as correlates of school dropout in a national sample of young adults. Child Development, 82(3), 982–998. doi:10.1111/j.1467-8624.2010.01534.x
- Pynoos, R. S., Weathers, F. W., Steinberg, A. M., Marx, B. P., Layne, C. M., Kaloupek, D. G., … Kriegler, J. A. (2015). Clinician-administered PTSD Scale for DSM-5 – child/adolescent version. In ptsd.va.gov. https://www.ptsd.va.gov/professional/assessment/documents/CAPS-CA-5.pdf
- R Core Team. (2009). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.r-project.org
- Ravens-Sieberer, U., Erhart, M., Rajmil, L., Herdman, M., Auquier, P., Bruil, J., … Kilroe, J. (2010). Reliability, construct and criterion validity of the KIDSCREEN-10 score: A short measure for children and adolescents’ well-being and health-related quality of life. Quality of Life Research, 19(10), 1487–1500. doi:10.1007/s11136-010-9706-5
- Rosner, R., Barke, A., Albrecht, B., Christiansen, H., Ebert, D. D., Lechner-Meichsner, F., … Steil, R. (2020). BEST FOR CAN – bringing empirically supported treatments to children and adolescents after child abuse and neglect: Study protocol. European Journal of Psychotraumatology, 11(1), 1837531. doi:10.1080/20008198.2020.1837531
- Rosner, R., König, H. H., Neuner, F., Schmidt, U., & Steil, R. (2014). Developmentally adapted cognitive processing therapy for adolescents and young adults with PTSD symptoms after physical and sexual abuse: Study protocol for a randomized controlled trial. Trials, 15(1), 1–9. doi:10.1186/1745-6215-15-195
- Rozental, A., Andersson, G., Boettcher, J., Ebert, D. D., Cuijpers, P., Knaevelsrud, C., … Carlbring, P. (2014). Consensus statement on defining and measuring negative effects of Internet interventions. In Internet Interventions (Vol. 1, Issue 1, pp. 12–19). Elsevier. doi:10.1016/j.invent.2014.02.001
- Rozental, A., Kottorp, A., Boettcher, J., Andersson, G., & Carlbring, P. (2016). Negative effects of psychological treatments: An exploratory factor analysis of the negative effects questionnaire for monitoring and reporting adverse and unwanted events. PLoS ONE, 11(6), doi:10.1371/journal.pone.0157503
- Rumpf, H.-J., Wohlert, T., Freyer-Adam, J., Grothues, J., & Bischof, G. (2013). Screening questionnaires for problem drinking in adolescents: Performance of AUDIT, AUDIT-C, CRAFFT and POSIT. European Addiction Research, 19(3), 121–127. doi:10.1159/000342331
- Sachser, C., Berliner, L., Holt, T., Jensen, T. K., Jungbluth, N., Risch, E., … Goldbeck, L. (2017). International development and psychometric properties of the Child and Adolescent Trauma Screen (CATS). Journal of Affective Disorders, 210, 189–195. doi:10.1016/j.jad.2016.12.040
- Saunders, J. B., Aasland, O. G., Babor, T. F., de la Fuente, J. R., & Grant, M. (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88(6), 791–804. doi:10.1111/j.1360-0443.1993.tb02093.x
- Schäfer, I., Gast, U., Hofmann, A., Knaevelsrud, C., Lampe, A., Liebermann, P., … Wöller, W. (2019). S3-Leitlinie Posttraumatische Belastungsstörung.
- Scheeringa, M. S., Zeanah, C. H., Myers, L., & Putnam, F. W. (2005). Predictive validity in a prospective follow-up of PTSD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry, 44(9), 899–906. doi:10.1097/01.chi.0000169013.81536.71
- Schneider, S., Pflug, V., In-Albon, T., & Margraf, J. (2017). Kinder-DIPS open access: Diagnostisches Interview bei psychischen Störungen im Kindes- und Jugendalter. In Forschungs- und Behandlungszentrum für psychische Gesundheit, Ruhr-Universität Bochum (Issue December). doi:10.13154/rub.101.90
- Schnyder, U., Ehlers, A., Elbert, T., Foa, E. B., Gersons, B. P. R., Resick, P. A., … Cloitre, M. (2015). Psychotherapies for PTSD: What do they have in common? European Journal of Psychotraumatology, 6, doi:10.3402/ejpt.v6.28186
- Schröder, J., Sautier, L., Kriston, L., Berger, T., Meyer, B., Späth, C., … Moritz, S. (2015). Development of a questionnaire measuring attitudes towards psychological online interventions-the APOI. Journal of Affective Disorders, 187, 136–141. doi:10.1016/j.jad.2015.08.044
- Seitz, D., Knaevelsrud, C., Duran, G., Waadt, S., & Goldbeck, L. (2014). Internet-based psychotherapy in young adult survivors of pediatric cancer: Feasibility and participants’ satisfaction. Cyberpsychology, Behavior, and Social Networking, 17(9), 624–629. doi:10.1089/cyber.2014.0066
- Seitz, D., Knaevelsrud, C., Duran, G., Waadt, S., Loos, S., & Goldbeck, L. (2014). Efficacy of an internet-based cognitive-behavioral intervention for long-term survivors of pediatric cancer: A pilot study. Supportive Care in Cancer, 22(8), 2075–2083. doi:10.1007/s00520-014-2193-4
- Sekhon, M., Cartwright, M., & Francis, J. J. (2017). Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Services Research, 17(1), 88. doi:10.1186/s12913-017-2031-8
- Sharma-Patel, K., & Brown, E. J. (2016). Emotion regulation and self blame as mediators and moderators of trauma-specific treatment. Psychology of Violence, 6(3), 400–409. doi:10.1037/vio0000044
- Sijbrandij, M., Kunovski, I., & Cuijpers, P. (2016). Effectiveness of internet-delivered cognitive behavioral therapy for posttraumatic stress disorder: A systematic review and meta-analysis. Depression and Anxiety, 33(9), 783–791. doi:10.1002/da.22533
- Sloan, D. M., & Marx, B. P. (2019). Written exposure therapy for PTSD: A brief treatment approach for mental health professionals. In Written exposure therapy for PTSD: A brief treatment approach for mental health professionals. American Psychological Association. doi:10.1037/0000139-000
- Spence, J., Titov, N., Dear, B. F., Johnston, L., Solley, K., Lorian, C., … Schwenke, G. (2011). Randomized controlled trial of internet-delivered cognitive behavioral therapy for posttraumatic stress disorder. Depression and Anxiety, 28(7), 541–550. doi:10.1002/da.20835
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. doi:10.1001/archinte.166.10.1092
- Steubl, L., Sachser, C., Baumeister, H., & Domhardt, M. (2021). Mechanisms of change in internet- and mobile-based interventions for PTSD: A systematic review and meta-analysis. European Journal of Psychotraumatology, 12(1), 1879551. doi:10.1080/20008198.2021.1879551
- UNICEF. (2017). Children in a digital world. In The state of the world’s children.
- van Minnen, A., Hendriks, L., & Olff, M. (2010). When do trauma experts choose exposure therapy for PTSD patients? A controlled study of therapist and patient factors. Behaviour Research and Therapy, 48(4), 312–320. doi:10.1016/j.brat.2009.12.003
- Vigerland, S., Lenhard, F., Bonnert, M., Lalouni, M., Hedman, E., Ahlen, J., … Ljótsson, B. (2016). Internet-delivered cognitive behavior therapy for children and adolescents: A systematic review and meta-analysis. Clinical Psychology Review, 50, 1–10. doi:10.1016/j.cpr.2016.09.005
- Weber, S., Jud, A., Landolt, M. A., & Goldbeck, L. (2017). Predictors of health-related quality of life in maltreated children and adolescents. Quality of Life Research, 26(10), 2717–2727. doi:10.1007/s11136-017-1615-4
- Williams, M. B., & Poijula, S. (2012). The PTSD Workbook. Simple, effective techniques for overcoming traumatic stress symptoms (Vol. 1). Probst, G.P. https://www.medimops.de/williams-mary-beth-das-ptbs-arbeitsbuch-wirksame-techniken-zur-ueberwindung-von-symptomen-traumatischer-belastung-broschiert-M03981338928.html?creative=&sitelink=&gclid=Cj0KCQjw0emHBhC1ARIsAL1QGNeQ5ktVVvE63VARUA4jvyG_GdSjsTVIIRtMWZ
- Yule, W., Bolton, D., Udwin, O., Boyle, S., O’Ryan, D., & Nurrish, J. (2000). The long-term psychological effects of a disaster experienced in adolescence: I: The incidence and course of PTSD. Journal of Child Psychology and Psychiatry, 41(4), 503–511. doi:10.1111/1469-7610.00635
- Zarski, A. C., Lehr, D., Berking, M., Riper, H., Cuijpers, P., & Ebert, D. D. (2016). Adherence to internet-based mobile-supported stress management: A pooled analysis of individual participant data from three randomized controlled trials. Journal of Medical Internet Research, 18(6), e146. doi:10.2196/jmir.4493