ABSTRACT
Pneumatosis intestinalis is a radiographic finding that represents a spectrum of conditions ranging from benign disease to abdominal sepsis and death. Along with portal venous gas, it is generally considered an ominous sign prompting emergency operative intervention. We report a rare case showing that nonoperative therapy can be considered in a seriously ill patient with esophageal, gastric and portal venous air.
1. Introduction
Pneumatosis of the gastrointestinal (GI) tract is a well-known phenomenon characterized by air-filled spaces in the mucosa and the submucosa. It can extend from the esophagus to the rectum with the small bowel being most commonly affected [Citation1]. With improvement in diagnostics there has been increased documentation of pneumatosis on computerized tomography (CT) scans [Citation2] of the abdomen.
Some causes that may lead to pneumatosis (depends upon the age of the patient) include: inflammatory bowel disease, bowel distention, diverticulitis, chronic obstructive pulmonary disease, connective tissue disease, AIDS, steroids, chemotherapy, pyloric stenosis, gastric outlet obstruction, duodenal stenosis, duodenal ulcers, or tumors. The most commonly attributed reason has been ischemia [Citation3–Citation5].
Traditionally pneumatosis of any part of the bowel meant an ominous sign. In this case report, we present a unique incident of gastric pneumatosis extending to the esophagus treated conservatively, with the latter being reported only seven times before in medical literature ().
Table 1. Cases of esophageal pneumatosis reported.
2. Case report
A 78-year-old male presented in the emergency department with altered mental status. According to family, the patient was in normal state of health in the morning, talking with his grandchildren, but became progressively less responsive.
His medical history included Alzheimer’s disease and hypertension. He had no known drug allergies and was taking no medications. Social history was significant for heavy alcohol use in the past but quit many years ago, and no tobacco use. The family denied any past surgeries.
Upon arrival to the ED he immediately began vomiting large volumes of coffee ground emesis, total output was over one liter. After rapid intubation and nasogastric tube placement, an additional 500 mL of coffee ground emesis was collected. Physical exam revealed tachycardia, clear lung fields, soft and nontender abdomen, and warm dry skin. Central line was placed and IV Levophed maintained the patient’s blood pressure at 105/60 mmHg, pulse at 95 bpm.
The workup included clear chest x-ray and non-contrast computed tomography, which revealed extensive portal venous gas essentially filling the superior mesenteric vein, splenic vein, and entire portal venous tree (). Extensive intramural gas was seen in the stomach and portions of the visualized esophagus, however there was no intramural gas pattern noted in the small bowel and no free air (). This pattern combined with metabolic acidosis on arterial blood gas with a pH of 7.16 and lactic acid level of 12.9 lead to the diagnosis of septic shock due to ischemic bowel.
Figure 1. Computed tomogram of the abdomen shows gastric pneumatosis and hepatic portal venous gas extending the entire venous tree and to the liver margins. Intramural gas in the stomach.
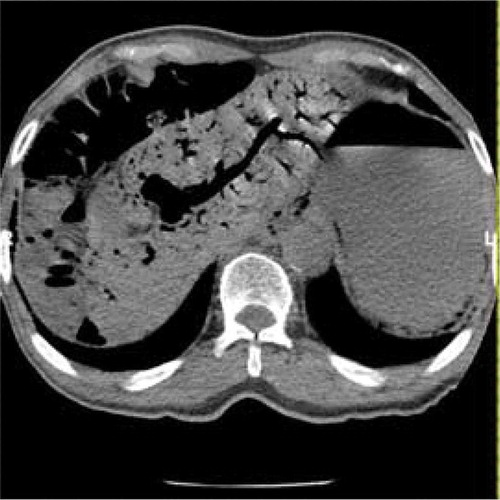
Figure 2. Computed tomogram of the abdomen revealing intramural gas in the stomach extending to the visualized esophagus. The small bowel is diffusely gas distended, but there is no intramural gas noted.
The patient was started on aggressive IV hydration, broad spectrum IV antibiotics, and pressors. In view of the presence of septic shock and unstable condition, a family meeting was held.
Despite the ominous signs of gastric and esophageal pneumatosis and portal venous gas, the decision was made to treat the patient nonoperatively. He recovered well on fluid resuscitation; lactic acid decreased to 4.0, hemoglobin was stable at 12.1 the following morning. His blood pressure stabilized and pressors were gradually withdrawn and stopped. A CT scan with oral contrast was done on hospital day 2, which showed near total resolution of pneumatosis of esophagus, stomach, and no evidence of portal venous gas. There was diffuse mural thickening of the stomach wall with no obstruction or extravasation of gastrografin (). Hospital day 5 the patient underwent esophagoduodenoscopy which revealed a healing Mallory-Weiss tear in the lower third of the esophagus with a small hiatal hernia and diffuse gastritis.
3. Discussion
The first description of pneumatosis was documented in medical literature in 1730 by Thorpe and Du Vernoi in a cadaver [Citation12]. Since then there have been many cases of gastric and intestinal pneumatosis and a few esophageal pneumatosis have been documented. They can affect a wide age, ranging from neonates to elderly patients. Pneumatosis is just a sign; it is for the physician to decide whether to perform surgery or treat conservatively based on likely presence of ischemia or infarction. Mclaughlin [Citation10] suggests the use of ‘non-gangrenous’ or ‘gangrenous’ for any pneumatosis intestinalis lesion of the GI tract.
Although the pathogenesis of pneumatosis isn’t very clear, four theories have been proposed: (1) bacterial – intramucosal gas is generated by gas-forming bacilli; (2) mechanical – increased intraluminal pressure during endoscopy or obstruction; (3) mucosal damage – air enters through disrupted mucosa due to, e.g., gastric ulcer: (4) pulmonary disease – alveolar air dissects down through the mediastinum within the gastric wall [Citation13].
Some examples of gangrenous pneumatosis are ischemia (most common), necrotizing enterocolitis, and caustic injury. The resulting mucosal injury gives way for gas forming bacteria like E. coli, Pseudomonas, Enterobacter, and Clostridium [Citation8]. These bacteria can also embolize to the portal system and cause hepatic-portal venous gas (HPVG). Pulmonary, mechanical, and traumatic are examples of non-gangrenous pneumatosis.
Various modalities have been utilized based on the underlying etiology of the pneumatosis. The most commonly used diagnostic modality is a CT scan, which is extremely sensitive [Citation14,Citation15]. Endoscopy can be used to confirm air in the lamina propria of the tissue, as well as to rule out the non-gangrenous causes of pneumatosis. According to Greenstein [Citation16], surgery was most likely to occur in patients with WBC >12 c/mmCitation3 and/or emesis in the >60-year-old age group.
4. Conclusion
A radiologic finding of pneumatosis does not necessarily indicate a severe underlying pathology. It has always been considered an indicator of bad prognosis and is associated with a high mortality rate. It is not by itself a surgical indication and treatment depends mainly on the underlying disease. The prognosis is related to the pathology itself and is not influenced by the presence of HPVG.
We believe that our patient had non-gangrenous esophageal and gastric pneumatosis. However, we are unsure of the exact mechanism that caused it. A small mucosal abrasion had occurred during the vomiting which was a Mallory–Weiss tear. The transient ischemia possibly involving the celiac plexus root compounded with the vomiting may have resulted in the pneumatosis involving the stomach, esophagus, and portal gas.
Although there have been few published reports on this condition, we believe that conservative supportive care in a critical care unit, with antibiotic coverage, may be the safest approach to management of non-gangrenous esophageal and gastric pneumatosis.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Boerner RM, Fried DB, Warshauer DM, et al. Pneumatosis intestinalis. Two case reports and a retrospective review of the literature from 1985 to 1995. Dig Dis Sci. 1996;41(11):2272–2285.
- Wayne E, Ough M, Wu A, et al. Management algorithm for pneumatosis intestinalis and portal venous gas: treatment and outcome of 88 consecutive cases j gastrointest. 2010;14(3):437–448.
- Luncă S, Rikkers A, Stănescu A. Acute massive gastric dilatation: severe ischemia and gastric necrosis without perforation. Rom J Gastroenterol. 2005;14(3):279–283.
- Kataria R, Bhatnagar V, Wadhwa S, et al. Gastric pneumatosis associated with preduodenal portal vein, duodenal atresia, and asplenia. Pediatr Surg Int. 1998;14(1–2):100–101.
- Kawano S, Tanaka H, Daimon Y, et al. Gastric pneumatosis associated with duodenal stenosis and malrotation. Pediatr Radiol. 2001;31(9):656–658.
- Vanasin B, Wright JR, Schuster MM. Pneumatosis cystoides esophagi. Case report supporting theory of submucosal spread. JAMA. 1971;217: 76–77. [PubMed].
- Katz D, Cano R, Antonelle M. Benign air dissection of the esophagus and stomach at fiber esophagoscopy. Gastrointest Endosc. 1972;19: 72–74. [PubMed].
- McKelvie PA, Fink MA. A fatal case of emphysematous gastritis and esophagitis. Pathology. 1994;26: 490–492. [PubMed].
- Tixedor N, Taourel P, Adell JF, et al. Extensive esophageal pneumatosis after acute dilatation of the stomach. AJR Am J Roentgenol. 1998;171: 272–273. [PubMed].
- Mclaughlin SA, Nguyen JH. Conservative management of nongangrenous esophageal and gastric pneumatosis. Am Surg. 2007;73: 862–864. [PubMed].
- Yahng SA, Kim HJ. Fortuitous detection of esophageal pneumatosis in a neutropenic patient. Korean J Hematol. 2011;46:151.
- Thorpe GJ. Pneumatosis cystoides intestinalis associated with abdominal carcinomatosis. Postgrad Med J. 1965;41:41–42.
- Johnson PT, Horton KM, Edil BH, et al. Gastric pneumatosis: the role of CT in diagnosis and patient management. Emerg Radiol. 2011;18(1):65–73.
- Monneuse O, Pilleul F, Barth X, et al. Portal venous gas detected on computed tomography in emergency situations: surgery is still necessary. World J Surg. 2007;31:1065–1071.
- Chan SC, Wan YL, Cheung YC, et al. Computed tomography findings in fatal cases of enormous hepatic portal venous gas. World J Gastroenterol. 2005;11:2953–2955.
- Greenstein AJ, Nguyen SQ, Berlin A, et al. Pneumatosis intestinalis in adults: management, surgical indications, and risk factors for mortality. Gastrointest Surg. 2007;11(10):1268–1274.