ABSTRACT
Lemierre’s syndrome also termed post-anginal septicemia, is a disease characterized by internal jugular septic thrombophlebitis leading to Fusobacterium septicemia with multiple metastatic foci following an oropharyngeal infection. Diagnosis and management is challenging and can result in fatal consequences due to potential multisystem involvement and multiple complications. We describe here a case of Lemierre’s syndrome with multifocal pneumonia, acute renal failure and protracted course of illness over forty days with successful recovery. A brief overview of literature is also presented.
KEYWORDS:
Background
Lemierre’s syndrome is a rare disease that was often fatal in the pre-antibiotic era, with a mortality rate approaching approximately 90%Citation[1]. It used to be named ‘a forgotten disease’ due to its rarity. There was not a single case reported between 1950’s and 1960’s but has been more overlooked than forgotten in recent years. According to a systematic review by Karkos et al Citation[2]., its incidence has been steadily increasing since the 1980’s, there were six online reported cases from 1980–1990 which rose to 121 from 2000 to 2008. It may be due to the emergence of resistant strains of causative pathogens, more emphasis on the judicious use of antibiotics or simply less clinical suspicion in the minds of physicians.
Case Presentation
A 33-year-old otherwise healthy male presented to emergency room after referral from an urgent care unit after his chest X-ray showed multifocal pneumonia. His symptoms started with high grade-fever and rigors for the last 9 days. He later developed sore throat, difficulty swallowing, productive cough and progressive dyspnea. He denied any sick contacts, romantic relationships, recent travel, tuberculosis exposure, recent dental procedure or exposure to animals.
On presentation, his vitals included a temperature of 104°F, pulse-140/min, blood pressure −104/53 mmHg, respiratory rate-33/min and oxygen saturation-89% on ambient air.
On physical examination, he appeared toxic and scleral icterus was noticed. The oropharynx examination showed right tonsillar swelling with erythema but without exudates. A firm immobile non-tender right submandibular swelling was present. No tongue swelling, dental caries/abscesses were identified. Axillary and cervical lymph nodes were not appreciated. No skin rash, joint swelling, needle or track marks were noticed. Chest examination showed bilateral rhonchi. Central nervous, cardiovascular and gastrointestinal systems were unremarkable.
Initial laboratory evaluation showed elevated white blood count (WBC) 21k/µl (neutrophils 81%, lymphocytes 4%, bands 13%), hemoglobin 16.1 mg/dl, platelet count of 41 k/µl, blood urea nitrogen 46 mg/dl, creatinine 2.12 mg/dl (baseline normal), total bilirubin 5 mg/dl (direct bilirubin 2.4 mg/dl) and alkaline phosphatase 261 U/L. Arterial blood gas revealed marked hypoxia requiring high flow nasal cannula.
Chest X-ray showed bilateral airspace opacities and patchy ground glass opacities consistent with multifocal pneumonia ().
He was resuscitated aggressively with intravenous fluids for septic shock from possibly pulmonary source and started empirically on vancomycin, cefepime, and levofloxacin. Bedside ultrasound of submandibular swelling revealed a clot in right internal jugular vein followed by an urgent CT scan of neck which revealed 3.3 × 2.7 × 3.1 cm fluid collection representing an abscess in the right palatine tonsil with a phlegmon and non-occlusive thrombus in the right internal jugular vein consistent with the diagnosis of Lemierre’s syndrome (, )).
Figure 2. (a, b): CT neck coronal section (a) abscess in the right palatine tonsil. (b) Non-occluding thrombus in the right internal jugular vein.

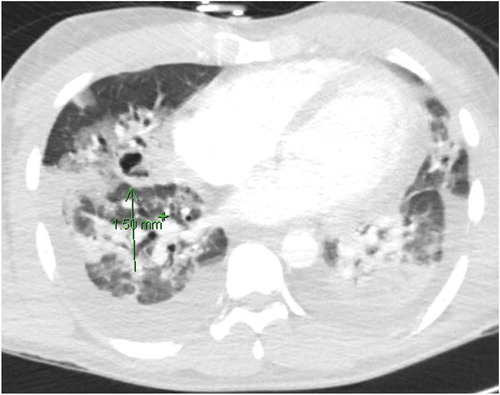
CT chest showed several hypodense foci of the lower lobes worrisome for phlegmon or early abscess formation and cavitary lesions in the right upper lobe (). Infectious disease and ENT were consulted and antibiotics were broadened to include clindamycin due to possible lung abscesses and cefepime was changed to meropenem due to its increased efficacy against anaerobes. A repeat ultrasound of neck veins didn’t show extension of the clot so anticoagulation was held.
The patient’s respiratory status deteriorated and he had to be intubated for worsening hypoxia. Bed side incision and drainage of the peritonsillar abscess was done by ENT which grew group-C streptococci. Antibiotics were narrowed to ampicillin-sulbactam after blood cultures came back positive for gram negative rods which were later identified as Fusobacterium species. His hospitalization course was complicated by acute respiratory distress syndrome(ARDS) requiring bi-level ventilation, intermittent pressor support and chest tube placement for persistent pleural effusions. Later, his kidney function deteriorated requiring hemodialysis for fluid overload. Antibiotics were changed to levofloxacin and metronidazole on day 10 of hospitalization as the decline in renal function was attributed to either interstitial nephritis from penicillin or septic acute tubular necrosis from the overwhelming infection. He continued to have recurrent fevers which led to repeat CT chest on day 15 of admission showing worsening of interstitial opacities and increase in the number of pulmonary cavities. Repeat cultures of blood, urine, and sputum were done which were negative including stool studies, bronchoalveolar lavage, and pleural fluid analysis. Same antibiotics were continued and gradually his fever resolved. His respiratory status continued to improve with improvement of hypoxia. The patient was extubated on day 21 of hospitalization. He never underwent tracheostomy and percutaneous endoscopic gastrostomy (PEG). He was also found to have right upper extremity deep venous thrombosis diagnosed by ultrasound after he was noticed to have swelling of right upper extremity. He was started on heparin initially and later bridged to warfarin. His kidney function improved and dialysis wasn’t required anymore. Levofloxacin was discontinued after a month and metronidazole was continued for a total of 6 weeks of antibiotics. He did well post discharge and warfarin was discontinued after three months.
Discussion
Lemierre’s syndrome is a condition that can be clinically correlated as having septic emboli from an oropharyngeal source. It is diagnosed on history of recent oropharyngeal infection, thrombophlebitis of internal jugular vein and positive blood cultures confirming septicemia. The process may start with a sore throat, acute tonsillitis, peritonsillar abscess, otitis media, sinusitis or any other head and neck infection, but pharyngitis and tonsillitis are the most commonly reported preceding illnesses [Citation3,Citation4]. The classic signs of bacteremia such as lethargy, high-grade fevers with chills and rigors are the most common presenting complaints accompanied by neck swelling, odynophagia, and dysphagia. The infection can extend to the internal jugular vein and cause the classic internal jugular vein thrombophlebitis. The mechanism of internal jugular vein involvement is not entirely clear, however various theories have been put forward such as hematogenous/lymphatic spread or local invasion. Once thrombophlebitis sets in, it can lead to systemic bacteremia and distant metastasisCitation[5].
The most common pathogen involved is Fusobacterium Necrophorum, a gram-negative anaerobe of the oral cavity. It is a frequent cause of sore throat, tonsillitis and peritonsillar abscessesCitation[6]. Other microorganisms causing Lemierre’s syndrome include Staphylococcus aureus including MRSA, Bacteroides, Peptostreptococcus and rarely Klebsiella pneumoniae [Citation7,Citation8]. The most common site of septic embolus is the lungs causing pneumonia, pleural effusions, abscess formation, cavitation and scarring of lung parenchyma [Citation4,Citation9,Citation10]. The septic metastases can involve any region of the body including joints, soft tissues, bones, and the meninges [Citation4,Citation10–Citation16].
The diagnosis when suspected should be confirmed with contrast enhanced CT scan as it leads to confirmation of thrombus in the internal jugular vein and can also detect septic emboli and other complications in the lungs. Doppler ultrasound should be used with caution to diagnose Lemierre’s syndrome as it has low sensitivity and can easily miss clots underneath the bones such as clavicle and mandible or the ones that are newly formed.
Early initiation of broad spectrum antibiotics shows favorable response and delay can lead to a worse outcome with mortality rate reaching as high as ~17% in untreated patientsCitation[17]. Antibiotics should be continued for a total of 3–6 weeks. Even in the presence of appropriate antibiotics fever might take 8–9 days to defervesce which doesn’t necessarily indicate resistanceCitation[18]. Prolonged course of antibiotics is required as antibiotics penetration is poor in abscess and fibrin clot which is the most likely explanation for recurrent fevers in this disease. Initial antibiotic choices are a combination of beta-lactamase resistant beta-lactams with metronidazole or monotherapy with clindamycin/carbapenem. The role of anticoagulation for the thrombophlebitis is controversial and is not unreasonable to consider it when there is an extensive clot or retrograde progression of the clot to cavernous sinusCitation[19].
The clinical course of the disease can get complicated due to multisystem involvement leading to increased mortality. Mild elevation of blood urea nitrogen and creatinine with hematuria is not uncommon but acute renal failure is rare and the possible etiology include either septic emboli to kidneys or acute septic tubular necrosis. Our patient also developed acute renal insufficiency requiring hemodialysis. The etiology of renal failure hasn’t been well documented in the available literature. Dreadful complications such as disseminated intravascular coagulation (DIC) due to sepsis can also occur [Citation20,Citation21].Lemierre’s syndrome is a treatable disease of young adults which can be fatal. In young adults, sore throat or any sign of oropharyngeal and head/neck infection should be dealt with more caution. Any suspicious swelling in the neck should be evaluated with sonographyCitation[22]. The patient should be closely followed up and on any sign of distress, antibiotics should be initiated soon after sending the cultures. Intensive level care should be given with a multi-specialty team involved to improve outcome and avoid complications.
Learning Points
Lemierre’s Syndrome is a treatable disease which otherwise can lead to a variety of complications including death. High index of suspicion in the minds of primary care and emergency physicians and early identification can result in favorable outcome.
Cases of sore throat in young adults should be followed up more closely as the incidence of Lemierre’s syndrome is on the rise.
Any head and neck infection not responding adequately to treatment should be screened for Lemierre’s syndrome and any neck swelling with history of sore throat should be subjected to radiological imaging.
Early initiation of antibiotic therapy and a multidisciplinary team should be employed in the care.
Disclosure statement
potential conflict of interest was reported by the authors.
References
- Noy D, Rachmiel A, Levy-Faber D, et al. Lemierre’s syndrome from odontogenic infection: review of the literature and case description. Ann Maxillofac Surg. 2015;5(2):219–225.
- Karkos PD, Asrani S, Karkos CD, et al. Lemierre’s syndrome: A systematic review. Laryngoscope. 2009;119(8):1552–1559.
- Te BN, Cocker D, Cullis P, et al. Lemierre’s disease: a case with bilateral iliopsoas abscesses and a literature review. World J Emerg Surg. 2014;9:38.
- Chirinos JA, Lichtstein DM, Garcia J, et al. The evolution of Lemierre syndrome: report of 2 cases and review of the literature. Medicine (Baltimore). 2002;81(6):458–465.
- Kuppalli K, Livorsi D, Talati NJ, et al. Lemierre’s syndrome due to Fusobacterium necrophorum. Lancet Infect Dis. 2012;12(10):808–815.
- Centor RM, Atkinson TP, Ratliff AE, et al. The clinical presentation of Fusobacterium - positive and streptococcal-positive pharyngitis in a University Health Clinic. Ann Intern Med. 2015;162(4):241.
- Chuncharunee A, Khawcharoenporn T. Lemierre’s syndrome caused by Klebsiella pneumoniae in a diabetic patient: a case report and review of the literature. Hawaii J Med Public Health. 2015;74(8):260–266.
- Stauffer C, Josiah AF, Fortes M, et al. Lemierre syndrome secondary to community-acquired methicillin-resistant Staphylococcus aureus infection associated with cavernous sinus thromboses. J Emerg Med. 2013;44(2):e177–82.
- Croft DP, Philippo SM, Prasad P. A case of Lemierre’s syndrome with septic shock and complicated parapneumonic effusions requiring intrapleural fibrinolysis. Respir Med Case Reports. 2015;16:86–88.
- Armstrong, Spooner, Sanders. Lemierre’s Syndrome. Curr Infect Dis Rep. 2000;2(2):168–173
- Bentham JR, Pollard AJ, Milford CA, et al. Cerebral infarct and meningitis secondary to Lemierre’s syndrome. Pediatr Neurol. 2004;30(4):281–283.
- Crum-Cianflone N, Mayer R, Malczynski J, et al. An unusual case of Lemierre’s syndrome presenting as pyomyositis. Am J Med Sci. 2008;335(6):499–501.
- Lustig LR, Cusick BC, Cheung SW, et al. Lemierre’s syndrome: two cases of postanginal sepsis. Otolaryngol Head Neck Surg. 1995;112(6):767–772.
- Hannoodi F, Sabbagh H, Kulairi Z, et al. A rare case of fusobacterium necrophorum liver abscesses. Clin Pract. 2017;7(1):928.
- Smith GR, Barton SA, Wallace LM. Further observations on enhancement of the infectivity of Fusobacterium necrophorum by other bacteria. Epidemiol Infect. 1991;106(2):305–310.
- Sinave CP, Hardy GJ, Fardy PW. The Lemierre syndrome: suppurative thrombophlebitis of the internal jugular vein secondary to oropharyngeal infection. Medicine (Baltimore). 1989;68(2):85–94.
- Shook J, Trigger C. Lemierre’s syndrome. West J Emerg Med. 2014;15(2):125–126.
- Hagelskjær LH, Prag J, Malczynski J, et al. Incidence and clinical epidemiology of necrobacillosis, including Lemierre’s syndrome, in Denmark 1990–1995. Eur J Clin Microbiol Infect Dis. 1998;17(8):561–565.
- Phua CK, Chadachan VM, Acharya R. Lemierre syndrome-should we anticoagulate? A case report and review of the literature. Int J Angiol. 2013;22(2):137–142.
- Iwamoto Y, Kawakami H, Kishi F, et al. Lemierre’s syndrome with acute renal failure. Nihon Naika Gakkai Zasshi. 2007;96(12):2792–2793.
- Georgopoulos S, Korres S, Riga M, et al. Lemierre’s syndrome associated with consumption coagulopathy and acute renal failure: a case report. J Laryngol Otol. 2008;122(5):527–530.
- Nadir N-A, Stone MB, Chao J. Diagnosis of Lemierre’s syndrome by bedside sonography. Acad Emerg Med. 2010;17(2):E9–E10.