ABSTRACT
Introduction: Malignant thyroid nodules are clinically euthyroid and appear as cold nodules on scintigraphy. Malignancy in hyper-functioning thyroid nodule is rare.
Case report: A 48-year-old male with painless swelling on the right side of his neck for the last 4 months complained of feeling hot all the time, sweating and unintentionally losing about 20 pounds. On physical examination, there was a 3-cm mobile, non-tender mass on the right supra-clavicular area biopsy of which was consistent with metastatic papillary carcinoma of thyroid. Neck imaging showed a cystic mass in the right supra-clavicular fossa region, bilateral neck adenopathy and multiple thyroid nodules. Subsequent thyroid radionuclide scans showed three hyper-functioning nodules, which were later demonstrated to be a follicular variant of papillary microcarcinoma. He was treated with total thyroidectomy followed by radioactive iodine thyroid ablation therapy.
Conclusion: Physicians need to be aware and vigilant for the possibilities of malignancy in a hyper-functioning thyroid nodule when evaluating any thyroid nodule.
1. Introduction
Thyroid nodules are frequently encountered clinical entities, and tend to be benign in nearly 95% of the cases [Citation1]. However, certain features in history, physical examination, laboratory tests and imaging scans raise suspicion for malignancy. Nearly all the malignant thyroid nodules are clinically euthyroid and appear as cold nodules on scintigraphy [Citation2]. However, they are rarely associated with hyper-functioning thyroid glands [Citation3,Citation4]. Here we present a case of a young man with hyper-functioning thyroid nodules found to be harboring invasive papillary thyroid carcinoma with nodal metastasis. He had a markedly suppressed serum thyrotropin level with elevated free thyroxine level.
2. Case report
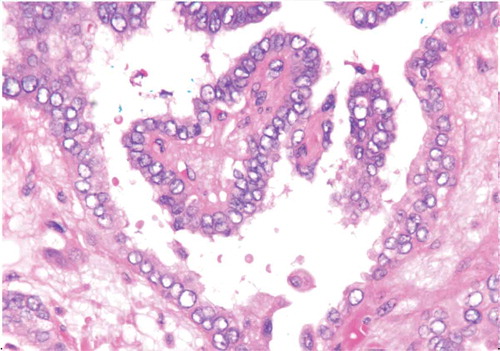
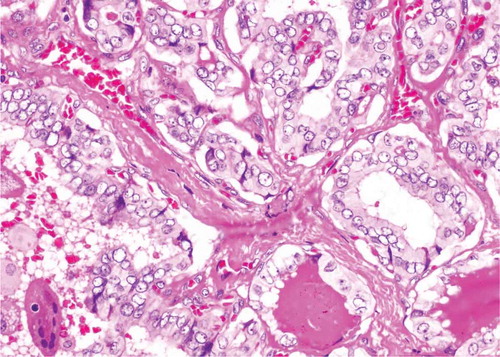
A 48-year-old African–American male presented for surgical removal of his recurrent keloid on left cheek. He was also complaining of painless swelling on the right side of his neck for the last 4 months. The swelling had been progressively increasing in size, but he denied any pain, discharge, redness, fever, sore throat, hoarseness or difficulty in swallowing. However, he reported feeling hot all the time, sweating and unintentionally losing about 20 pounds in the last 2 months. There was no change in his appetite, abdominal pain, bowel habit alteration, nausea or vomiting. The rest of the systemic review was negative. He had a past medical history of recurrent keloids and hypertension, but was not taking any medications. There was no previous history of neck irradiation. He had smoked about 10 cigarettes daily for the last 20 years. He did not drink alcohol or use recreational drugs. Family history was significant for pancreatic cancer and gastric cancer on his maternal side. Physical examination was significant for a pedunculated keloid on the left side of the face and a 3-cm mobile, non-tender mass on the right supra-clavicular area. His initial blood test was significant for thyroid-stimulating hormone (TSH) level of <0.005 µIU/mL (normal 0.450–4.50 µIU/mL), free T4 level of 2.93 ng/dL (0.9–2.4 ng/dL) and T3 level of 155 ng/dL (3.6–5.6 ng/dL). Neck imaging with computed tomography (CT) scan and thyroid ultrasonogram (USG) showed a cystic mass about 4.4 cm in the right supra-clavicular fossa region, bilateral neck adenopathy and multiple thyroid nodules. Thyroid USG showed a 1.5-cm nodule in superior pole of the right lobe, a 1.4-cm nodule in the lower pole of right lobe and a 0.7-cm nodule near the isthmus. Subsequent thyroid radionuclide scans with technetium 99 m pertechnetate showed hyperavid nodular foci in the lower pole of right lobe, middle portion of the right lobe and the isthmus (). Excisional biopsy of the right supra-clavicular mass was done and showed a lymph node consistent with metastatic papillary carcinoma of thyroid (). Immunohistochemistry testing was positive for TTF1 and CK20, and focally positive for Carcino Embryonic Antigen (CEA) monoclonal marker and thyroglobulin. He then underwent total thyroidectomy with right neck dissection. Microscopic examination of the surgical specimen revealed three foci of tumor – a 5.5-mm area in the lower portion of the right lobe with follicular variant of papillary microcarcinoma involving the thyroid capsule, a 1.4-mm area in the isthmus with circumscribed follicular variant of papillary microcarcinoma and a 0.5-mm area in mid portion of the right lobe with circumscribed follicular variant of papillary microcarcinoma (). Surgical margins were clear, and only 1 out of the 17 lymph nodes sampled was positive for metastatic carcinoma. The pathological stage of the tumor was T1aN1bMx. Subsequently, the patient underwent radioactive iodine (I-131) thyroid ablation therapy and was discharged. On follow up, his TSH was 55 µIU/mL (normal 0.36–3.7 µIU/mL), thyroglobulin level was 5.2 ng/mL and thyroglobulin antibody level was <1, while whole body I-131 scan showed mild focal areas of increased activity in the upper neck region and no evidence of distant metastasis.
3. Discussion
Thyroid nodules are a common clinical problem. While 4–7% of adult population in the United States have a palpable thyroid nodule, only 5% of these are malignant [Citation1]. All thyroid nodules more than 1 cm in size and those less than 1 cm in size with associated lymphadenopathy or suggestive clinical features require further evaluation to rule out malignancy [Citation5]. The initial step in the evaluation of a thyroid nodule is measurement of serum TSH followed by thyroid radionuclide scan if the TSH is subnormal. Malignant nodules are usually non-functioning [Citation2]. Hyper-functioning nodules are thought to only rarely harbor malignancy and, as such, do not necessitate cytological evaluation [Citation5].
Our patient had hyper-functioning nodules on thyroid radionuclide scan with overt hyperthyroidism as evidenced by clinical symptoms, suppressed serum thyrotropin and elevated thyroxine. However, in the presence of cervical lymphadenopathy, the possibility of thyroid malignancy was entertained. The subsequent excisional biopsy of the lymph node and thyroidectomy proved the presence of invasive papillary carcinoma of thyroid. Multiple other cases of hyper-functioning malignant thyroid nodules have been reported [Citation4,Citation6–Citation8]. In a review by Mirfakhraee et al., the prevalence of intra-nodular thyroid malignancy among hyper-functioning ‘hot’ nodules ranged from 0% to 12.5% in different case series with the weighted prevalence rate being 3.1% [Citation6]. Similarly, there are increasing number of reports of co-existence of thyroid malignancy and hyperthyroidism [Citation9–Citation12]. In a review by Gabriele et al., the prevalence of thyroid malignancy in hyperthyroid patients was 1.65% [Citation11]. Most of these malignancies were of the papillary carcinoma type [Citation6]. While the exact pathophysiological mechanism has not been elucidated, mutations in TSH receptors and Ki-RAS play an important role in the hyper-functioning of the thyroid tumor and its carcinogenetic process [Citation13,Citation14].
Further evaluation and characterization of this association between hyper-functioning thyroid nodule and malignancy is needed. Meanwhile, physicians need to be aware and vigilant for the possibilities of malignancy in a hyper-functioning thyroid nodule when evaluating any thyroid nodule.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Hegedüs L. Clinical practice. The thyroid nodule. N Engl J Med. 2004;351(17):1764–1771.
- Singer PA, Cooper DS, Daniels GH, et al. Treatment guidelines for patients with thyroid nodules and well-differentiated thyroid cancer. American Thyroid Association. Arch Intern Med. 1996;156(19):2165–2172.
- Haraj NE, Ahandar H, El Aziz S, et al. [Association of hyperthyroidism with differentiated thyroid cancer]. Pan Afr Med J. 2016;24:18.
- Salih AM, Kakamad FH, Nihad H. Hyperfunctioning papillary thyroid carcinoma: a case report with literature review. Int J Surg Case Rep. 2016;26:202–204.
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133.
- Mirfakhraee S, Mathews D, Peng L, et al. A solitary hyperfunctioning thyroid nodule harboring thyroid carcinoma: review of the literature. Thyroid Res. 2013;6(1):7.
- Harach HR, Sánchez SS, Williams ED. Pathology of the autonomously functioning (hot) thyroid nodule. Ann Diagn Pathol. 2002;6(1):10–19.
- De Rosa G, Testa A, Maurizi M, et al. Thyroid carcinoma mimicking a toxic adenoma. Eur J Nucl Med. 1990;17(3–4):179–184.
- Girelli ME, Casara D, Rubello D, et al. Severe hyperthyroidism due to metastatic papillary thyroid carcinoma with favorable outcome. J Endocrinol Invest. 1990;13(4):333–337.
- Manmadharao V, Kirankumar G, Jayaramudu YV, et al. A rare case of papillary carcinoma of thyroid with hyperthyroidism. J Evol Med Dent Sci. 2015;4(10):1694–1698.
- Gabriele R, Letizia C, Borghese M, et al. Thyroid cancer in patients with hyperthyroidism. Horm Res. 2003;60(2):79–83.
- Kinkel B, Bucerius J, Risse JH. [Graves’ disease and papillary thyroid cancer – coincidence or association?]. Dtsch Med Wochenschr. 2007;132(18):983–986.
- Niepomniszcze H, Suárez H, Pitoia F, et al. Follicular carcinoma presenting as autonomous functioning thyroid nodule and containing an activating mutation of the TSH receptor (T620I) and a mutation of the Ki-RAS (G12C) genes. Thyroid. 2006;16(5):497–503.
- Gozu H, Avsar M, Bircan R, et al. Does a Leu 512 Arg thyrotropin receptor mutation cause an autonomously functioning papillary carcinoma? Thyroid. 2004;14(11):975–980.