ABSTRACT
Background: Nontuberculous mycobacterium is a recognized cause of hypercalcemia, particularly in patients with acquired immunodeficiency syndrome (AIDS). Here we describe a case of severe hypercalcemia secondary to Mycobacterium abscessus (M. abscessus) in a patient with AIDS. To the best of our knowledge this is the first case report describing a case of M. abscessus presenting as retroperitoneal lymphadenopathy and severe hypercalcemia.
Case description: A 56-year-old man with AIDS presented with altered mental status and somnolence for four days. Laboratory investigations were significant for calcium 16.49 mg/dL (RI 8.9–10.3 mg/dL), 1,25 dihydroxyvitamin D level 44.1 pg/ml (RI 19.9–79.3 pg/ml) and parathyroid hormone (PTH) 4 pg/mL (RI 15–65 pg/mL). CT scan of Abdomen and Pelvis showed hepatosplenomegaly with large retroperitoneal, retrocrural, and mesenteric lymphadenopathy which had an intense focal uptake on Gallium scan. Bone marrow biopsy revealed mild plasmacytosis (5%) with no evidence of myelodysplasia, acute leukemia or lymphoma. A subsequent lymph node biopsy showed fragments of fibrous tissue with lymphohistiocytic infiltrate and many acid-fast bacilli. Pre-antibiotic blood cultures grew Mycobacterium which was identified later as M. abscessus at four weeks.
Conclusion: hypercalcemia in HIV-infected patients may suggest malignancy or infectious etiology, among other causes. Clinicians should be aware of the risk of hypercalcemia with nontuberculous mycobacterium (NTM) infection, whether as first manifestation or a late presenter in the disease course after initiating antiretroviral therapy (ART). We suggest careful monitoring of serum calcium level upon diagnosis of NTM infection and after initiation of ART, NTM therapy or vitamin D supplementation.
1. Introduction
Hypercalcemia has been well described in granulomatous diseases, sarcoidosis and tuberculosis being the most common causes. Both Tuberculous and nontuberculous mycobacterium (NTM) have been associated with hypercalcemia. NTM, commonly Mycobacterium avium intracellulare has been a recognized cause of hypercalcemia based on case reports, particularly those with acquired immunodeficiency syndrome (AIDS). We describe a case of severe hypercalcemia secondary to Mycobacterium abscessus (M. abscessus) subspecies abscessus in a patient with AIDS. To the best of our knowledge this is the first case report of severe hypercalcemia with retroperitoneal lymphadenopathy secondary to M. abscessus without pulmonary, skin or soft tissue infection.
2. Case description
A 56-year-old man with AIDS for four years, non-compliant with his antiretroviral therapy (ART) presented with altered mental status and somnolence for four days. His family reported progressive weakness affecting his ambulation over a period of three weeks. There was no history of sick contacts, recent travel, animal exposure, or illicit drug use. An unintentional weight loss of about twenty pounds over the past four months was also reported. Patient had been started on ART four weeks prior to his hospital admission. Patient’s home medications were elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide (fixed dose combination), azithromycin and dapsone.
On physical examination, he was cachectic and somnolent, temperature was 97.5 F, blood pressure 112/74 mm Hg, heart rate 95 bpm, respiratory rate 16 with oxygen saturation 98% on room air. EKG showed sinus rhythm with premature atrial complexes and shortened QT interval (corrected 376ms).
Laboratory investigations were significant for normocytic anemia with a hemoglobin of 9.8 g/dL, leukopenia 3.3 × 103/µL, thrombocytopenia 120 x 103/µL, BUN 43 mg/dL (RI 8-20mg/dL), creatinine 2.09 mg/dL (RI 0.4−1.3 mg/dl), corrected calcium 16.49 mg/dL (RI 8.9–10.3 mg/dL), ionized calcium 7.8 mg/dL (RI 4.5–5.6 mg/dL), phosphorus 4.4 mg/dL (RI 2.4–4.7 mg/dL), and albumin 2.6 g/dL (RI 3.5–4.8 g/dL). Other notable initial laboratory findings included 25-hydroxyvitamin D level 56 ng/ml (RI 30–100 ng/ml), 1,25 dihydroxyvitamin D level 44.1 pg/ml (RI 19.9–79.3 pg/ml), parathyroid hormone (PTH) 4 pg/mL (RI 15–65 pg/mL) with PTH-related peptide levels undetectable. Of note, CD4 count was 36/mm3 and viral load was 617,000 before initiation of antiretroviral therapy.
He received intravenous fluids and pamidronate with calcitonin. His serum calcium declined to 9.8 mg/dL (RI 8.9–10.3 mg/dL), kidney function improved with BUN 39mg/dL (RI 8-20mg/dL) and creatinine 1.26 mg/dL (RI 0.4−1.3 mg/dl) by hospital day three. There was improvement in patient’s mental status within one day of treatment initiation.
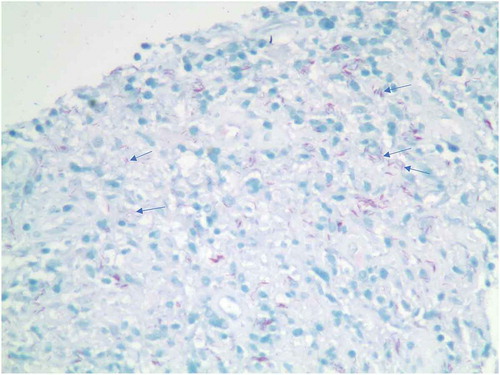
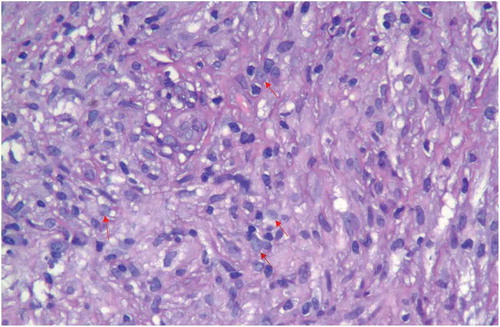
Serum protein electrophoresis revealed monoclonal gammopathy with Free Kappa/Lambda ratio of 1.31 (0.26–1.65) and serum Monoclonal Immunoglobulin (Ig) G was also elevated at 2359. Lactate dehydrogenase level (LDH) was 281 IU/L (RI 98–192 IU/L) and beta-2- microglobulin was 12 mg/L (RI 0.6–2.4mg/L). Whole body skeletal survey revealed no focal uptake. There was no evidence of parenchymal lung disease or mediastinal lymphadenopathy on Computerized Tomography (CT) scan of Chest (). CT scan of Abdomen and Pelvis revealed hepatosplenomegaly with large retroperitoneal, retrocrural, and mesenteric lymphadenopathy ((a,b)) which had an intense focal uptake on Gallium scan with no abnormal lung uptake (). The presence of Monoclonal IgG along with hepatosplenomegaly and retroperitoneal lymphadenopathy, elevated LDH were all strongly suggestive of initial presumptive diagnosis of a lymphoproliferative disease. Lymphoma was strongly suspected and he underwent a bone marrow biopsy and lymph node biopsies twice. Bone marrow biopsy revealed mild plasmacytosis (5%), normocellular marrow (50%) with mature trilineage, no evidence of myelodysplasia, acute leukemia or lymphoma. A subsequent biopsy of the lymph nodes showed fragments of fibrous tissue with lymphohistiocytic infiltrate () and many acid-fast bacilli on special stain (). Results of bone marrow biopsy and lymph node biopsy were not consistent with lymphoma which promoted investigation for other causes of hypercalcemia and lymphadenopathy. Mycobacterium tuberculosis and Mycobacterium avium complex Polymerase Chain Reaction (PCR) were also negative. Three sputum samples for acid fast bacilli (AFB) smear were negative.
Figure 1. Chest CT scan- Axial view: Normal parenchymal lung tissue without evidence of active chest disease or intrathoracic lymphadenopathy.
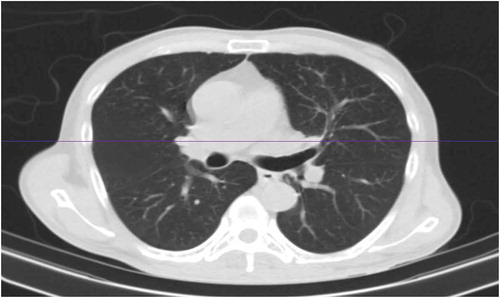
Figure 2. (a) Abdomen and pelvis CT scan: The liver is large measuring up to 24 cm (blue arrows). The spleen is large measuring 17.4 cm (red arrows), retrocrural lymphadenopathy (white arrows). (b) Abdomen and pelvis CT scan: Retroperitoneal lymph nodes (white arrows).
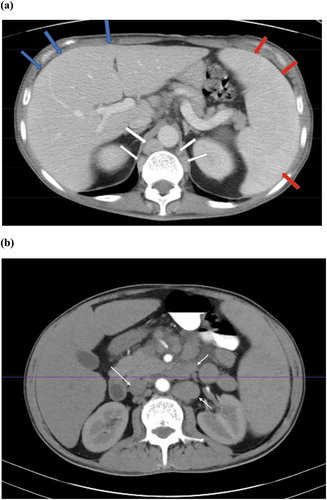
Figure 3. Gallium scan: Large region of intense focal uptake midline abdomen compatible with mesenteric (blue arrows) and retroperitoneal lymphadenopathy (white arrows). No abnormal lung uptake is seen.
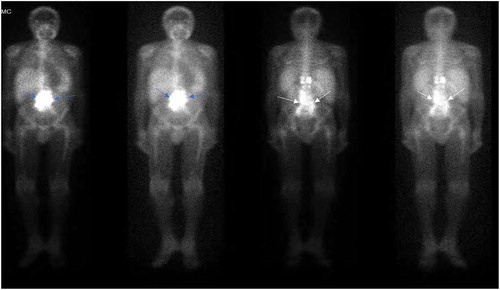
Figure 4. Lymph node biopsy: (hematoxylin and eosin stain) lymphohistiocytic infiltrate (red arrows).
Patient was initially started on Vancomycin and meropenem for presumed sepsis. As lymph node biopsy smear was positive for AFB; rifabutin, isoniazid, pyrazinamide and ethambutol were commenced as well as azithromycin for tuberculous and nontuberculous mycobacterium pending further identification. Calcium level remained within normal range and his medical condition improved. He was then discharged with medical follow up and continues to show sustained clinical improvement. However, pre-antibiotic blood cultures drawn in a sodium heparin tube subsequently grew Mycobacterium identified by genomic analysis as M. abscessus subspecies abscessus at four weeks. Bone marrow culture remained without any growth.
3. Discussion
Hypercalcemia occurs in many granulomatous diseases. Among them, sarcoidosis and tuberculosis are the most common causes. Other rare causes include berylliosis, coccidioidomycosis, histoplasmosis, Crohn’s disease, silicone-induced granulomas, cat-scratch disease, Wegener’s granulomatosis and Pneumocystis carinii pneumonia.
It has only recently been recognized that patients with AIDS and NTM colonization or infection may also present with hypercalcemia. The exact mechanism of hypercalcemia in NTM is not fully understood. It may be related to granuloma formation, which results in continuous production of 1,25-dihydroxyvitamin D3 [1,25(OH)2D3] despite high level of serum calcium. Macrophages in granulomatous tissue independently produce one alpha hydroxylase, leading to increased 1,25(OH)2D3 [Citation1–Citation5].
Hypercalcemia with elevated 1,25(OH)2D3 has also been described in a patient with hypersensitivity pneumonitis secondary to Mycobacterium avium-intracellulare (MAI) [Citation6].
Shrayyef et al. described a patient with HIV infection and hypocalcemia who was treated with Ergocalciferol 50,000 units po weekly, who subsequently developed hypercalcemia with corrected calcium of 13.7mg/dL. Chest and abdomen CT scan showed mediastinal and paraaortic lymphadenopathy and MAI was diagnosed by fine needle aspiration of lymph nodes [Citation7].
1,25(OH)2D3 produced by macrophages probably has only a local effect in enhancing cell-mediated immunity to NTM and should not normally affect calcium metabolism. However, large quantities of 1,25(OH)2D3 may result in hypercalcemia. Of interest, abnormal calcium metabolism against mycobacterial granuloma does not always correlate with the serum level of 1,25(OH)2D3, the type of infection, the extent of granulomatous destruction, or the duration of chemotherapeutic treatment [Citation8]. There are reported cases of hypercalcemia in NTM infection with normal levels of 1,25(OH)2D3 which might suggest a different mechanism for hypercalcemia [Citation9,Citation10].
In immunocompromised patients with disseminated granulomatous disorders, hypercalcemia might be explained by the restoration of the immune system after starting ART treatment. [Citation11–Citation14] Immune reconstitution inflammatory syndrome (IRIS) results from recovery of cellular and humoral immune system function in response to ART; symptoms result from immune responses to opportunistic pathogens. In IRIS, there is rebound production of IFN-γ and hence enhance granuloma formation to facilitate the eradication of infection. [Citation15] Tsao et al. described hypercalcemia as part of IRIS in patients with AIDS and NTM colonization who started on antiretroviral treatment [Citation8].
There are five reported cases of hypercalcemia in patients who were undergoing treatment for MAI and/or HIV, soon after starting or changing therapy. [Citation16–Citation18]
Hypercalcemia with low level of vitamin D also has been described in a case of cutaneous granulomatous disease caused by Mycobacterium marinum four weeks after starting ART. PTH and both 25 Hydroxyvitamin D and 1,25(OH)2D3 were all suppressed [Citation19]. Hypercalcemia has been also described in an immunocompetent patient with normal vitamin D3 level and MAI infection of the lung [Citation9].
Our patient was started on ART four weeks prior to manifestation of severe hypercalcemia and this is most likely the trigger. describes reported cases of hypercalcemia in NTM infection and their presumed triggers.
Table 1. Reported cases of hypercalcemia in NTM infection. [Citation18].
M. abscessus classified as one of the rapidly growing mycobacteria (RGM), it is the third most common NTM infection in the USA and causes about 80% of pulmonary infections due to RGM. M. abscessus can cause both pulmonary and extra pulmonary diseases.
Pulmonary infection is usually seen in nonsmoking white women who have no predisposing conditions. The usual clinical presentation is similar to that of other NTM pulmonary infections and includes cough and easy fatigability. For most patients without predisposing conditions, the chest radiograph usually shows multilobar, patchy, reticulonodular or mixed reticulonodular alveolar opacities. [Citation20] In our case chest CT scan revealed normal lung parenchyma without evidence of active chest disease or intrathoracic lymphadenopathy.
Extra-pulmonary disease most commonly involves skin and soft tissue infection, which usually occur after medical procedures or traumatic injuries [Citation21,Citation22]. Recently, postsurgical and post-procedure outbreaks of skin and soft tissue infections caused by M. abscessus or Mycobacterium massiliense (M. massiliense) have occurred in several countries. [Citation23–Citation27] Bone and joint infection have been also reported in the form of septic arthritis after medical procedures [Citation28]. However, isolated bone infection with M. abscessus is rare and only one case of vertebral osteomyelitis has been reported [Citation29]. Ocular infections can occur after medical interventions, trauma or implant and M. abscessus accounts for about 10% of NTM ocular infections [Citation30]. M. abscessus bacteremia has been reported after prostate biopsy, disseminated form in a peritoneal dialysis patient, glossitis and in a case of native valve endocarditis [Citation31–Citation34].
M. abscessus is typically resistant in vitro to most of the medications used to treat tuberculosis and has demonstrated in vitro activity to only a few antimicrobial agents. Cure can be elusive for many patients with M. abscessus lung disease with medical therapy alone [Citation35]. The guidelines of the American Thoracic Society and Infectious Diseases Society of America recommend macrolide-based antibiotic therapy combined with intravenous amikacin and cefoxitin or imipenem, based on the results of drug susceptibility testing (DST) for the treatment of M. abscessus infections of the lung. However, the guidelines recommend different approaches for the treatment of extrapulmonary and pulmonary M. abscessus infections. For extrapulmonary M. abscessus infections, such as skin, soft tissue, and bone infections, a total of 4–6 months of antibiotic therapy with at least 2 weeks of an initial combination of parenteral antibiotics is recommended, with a high likelihood of cure. However, pulmonary M. abscessus disease is regarded as a chronic, incurable infection for most patients, even with the recommended 2–4 months of parenteral antibiotics followed by long-term macrolide-based antibiotic therapy. The exact reasons for these different treatment outcomes are largely unknown. Serious infections should be treated with a regimen similar to that used for pulmonary disease. Skin and soft tissue infections should be treated for a minimum of 4 months and bone infections for 6 months. Surgery is generally indicated for extensive disease, for abscesses, or when drug therapy is difficult [Citation36].
Glucocorticoids are an effective treatment for NTM associated hypercalcemia. They suppress both the inflammatory process involved in granuloma formation and 1 -α hydroxylase activity [Citation6].
Bisphosphonates have been used to treat hypercalcemia secondary to NTM, however hemodialysis was required in some refractory cases. Our patient was treated with calcitonin and pamidronate which resulted in reduction in calcium level to normal range in few days.
In conclusion, hypercalcemia in HIV-infected patients may suggest malignancy or infectious etiology, among other causes. Clinicians should be aware of the risk of hypercalcemia with NTM infection, whether as the first manifestation or a late presenter in the disease course after initiating ART. We suggest careful monitoring of serum calcium level upon diagnosis of NTM infection and after initiation of ART, NTM therapy or vitamin D supplementation.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Hamzeh N. Sarcoidosis. Med Clin North Am. 2011 Nov;95(6):1223–1234. PubMed PMID: 22032436.
- Zhang JT, Chan C, Kwun SY, et al. A case of severe 1,25-dihydroxyvitamin D-mediated hypercalcemia due to a granulomatous disorder. J Clin Endocrinol Metab. 2012 Aug;97(8):2579–2583. PubMed PMID: 22639294.
- Mukhopadhyay S, Gal AA. Granulomatous lung disease: an approach to the differential diagnosis. Arch Pathol Lab Med. 2010 May;134(5):667–690. PubMed PMID: 20441499.
- Khoor A, Leslie KO, Tazelaar HD, et al. Diffuse pulmonary disease caused by nontuberculous mycobacteria in immunocompetent people (hot tub lung). Am J Clin Pathol. 2001 May;115(5):755–762. PubMed PMID: 11345841.
- Gardner DG. Hypercalcemia and sarcoidosis–another piece of the puzzle falls into place. Am J Med. 2001 Jun 15;110(9):736–737. PubMed PMID: 11403760.
- Donato J, Phillips CT, Gaffney AW, et al. A case of hypercalcemia secondary to hot tub lung. Chest. 2014 Dec;146(6):e186–e189. PubMed PMID: 25451359.
- Shrayyef MZ, DePapp Z, Cave WT, et al. Hypercalcemia in two patients with sarcoidosis and Mycobacterium avium intracellulare not mediated by elevated vitamin D metabolites. Am J Med Sci. 2011 Oct;342(4):336–340. PubMed PMID: 21760475.
- Tsao YT, Wu CC, Chu P. Immune reconstitution syndrome-induced hypercalcemic crisis. Am J Emerg Med. 2011 Feb;29(2):244 e3–6. PubMed PMID: 20825906.
- Parsons CE, Singh S, Geyer HL. A case of hypercalcaemia in an immunocompetent patient with Mycobacterium avium intracellulare. JRSM Open. 2017 Jul;8(7):2054270417716614. PubMed PMID: 28748100; PubMed Central PMCID: PMCPMC5507386.
- Delahunt JW, Romeril KE. Hypercalcemia in a patient with the acquired immunodeficiency syndrome and Mycobacterium avium intracellulare infection. J Acquir Immune Defic Syndr. 1994 Aug;7(8):871–872. PubMed PMID: 8021822.
- Lin JH, Chen W, Lee JY, et al. Disseminated cutaneous Mycobacterium haemophilum infection with severe hypercalcaemia in a failed renal transplant recipient. Br J Dermatol. 2003 Jul;149(1):200–202. PubMed PMID: 12890222.
- Ryzen E, Rea TH, Singer FR. Hypercalcemia and abnormal 1,25-dihydroxyvitamin D concentrations in leprosy. Am J Med. 1988 Feb;84(2):325–329. PubMed PMID: 2841852.
- Lawn SD, Macallan DC. Hypercalcemia: a manifestation of immune reconstitution complicating tuberculosis in an HIV-infected person. Clin Infect Dis. 2004 Jan 1;38(1):154–155. PubMed PMID: 14679464.
- Jenny-Avital ER, Abadi M. Immune reconstitution cryptococcosis after initiation of successful highly active antiretroviral therapy. Clin Infect Dis. 2002 Dec 15;35(12):e128–e133. PubMed PMID: 12471589.
- Monkawa T, Yoshida T, Hayashi M, et al. Identification of 25-hydroxyvitamin D3 1alpha-hydroxylase gene expression in macrophages. Kidney Int. 2000 Aug;58(2):559–568. PubMed PMID: 10916079.
- Choudhary M, Rose F. Posterior reversible encephalopathic syndrome due to severe hypercalcemia in AIDS. Scand J Infect Dis. 2005;37(6–7):524–526. PubMed PMID: 16012020.
- Playford EG, Bansal AS, Looke DF, et al. Hypercalcaemia and elevated 1,25(OH)(2)D(3) levels associated with disseminated Mycobacterium avium infection in AIDS. J Infect. 2001 Feb;42(2):157–158. PubMed PMID: 11531324.
- Ayoubieh H, Alkhalili E. Mycobacterium avium-intracellulare and the unpredictable course of hypercalcemia in an AIDS patient. Braz J Infect Dis. 2017 Jan-Feb;21(1):116–118. PubMed PMID: 27620657.
- Nielsen CT, Andersen AB. Hypercalcemia and renal failure in a case of disseminated Mycobacterium marinum infection. Eur J Intern Med. 2009 Mar;20(2):e29–e31. PubMed PMID: 19327592.
- Griffith DE, Girard WM, Wallace RJ Jr. Clinical features of pulmonary disease caused by rapidly growing mycobacteria. An analysis of 154 patients. Am Rev Respir Dis. 1993 May;147(5):1271–1278. PubMed PMID: 8484642.
- Piersimoni C, Scarparo C. Extrapulmonary infections associated with nontuberculous mycobacteria in immunocompetent persons. Emerg Infect Dis. 2009 Sep;15(9):1351–8; quiz 1544. PubMed PMID: 19788801; PubMed Central PMCID: PMCPMC2819852.
- Kasperbauer S, Huitt G. Management of extrapulmonary nontuberculous mycobacterial infections. Semin Respir Crit Care Med. 2013 Feb;34(1):143–150. PubMed PMID: 23460014.
- Cheng A, Liu YC, Chen ML, et al. Extrapulmonary infections caused by a dominant strain of Mycobacterium massiliense (Mycobacterium abscessus subspecies bolletii). Clin Microbiol Infect. 2013 Oct;19(10):E473–E482. PubMed PMID: 23718188.
- Koh SJ, Song T, Kang YA, et al. An outbreak of skin and soft tissue infection caused by Mycobacterium abscessus following acupuncture. Clin Microbiol Infect. 2010 Jul;16(7):895–901. PubMed PMID: 19694761.
- Leao SC, Viana-Niero C, Matsumoto CK, et al. Epidemic of surgical-site infections by a single clone of rapidly growing mycobacteria in Brazil. Future Microbiol. 2010 Jun;5(6):971–980. PubMed PMID: 20521940.
- Kim HY, Yun YJ, Park CG, et al. Outbreak of Mycobacterium massiliense infection associated with intramuscular injections. J Clin Microbiol. 2007 Sep;45(9):3127–3130. PubMed PMID: 17626174; PubMed Central PMCID: PMCPMC2045247.
- Song JY, Son JB, Lee MK, et al. Case series of mycobacterium abscessus infections associated with a trigger point injection and epidural block at a rural clinic. Epidemiol Health. 2012;34:e2012001. PubMed PMID: 22323979; PubMed Central PMCID: PMCPMC3272546.
- Jung SY, Kim BG, Kwon D, et al. An outbreak of joint and cutaneous infections caused by non-tuberculous mycobacteria after corticosteroid injection. Int J Infect Dis. 2015 Jul;36:62–69. PubMed PMID: 26026822.
- Garcia DC, Sandoval-Sus J, Razzaq K, et al. Vertebral osteomyelitis caused by Mycobacterium abscessus. BMJ Case Rep. 2013 Aug 7;2013. PubMed PMID: 23925676; PubMed Central PMCID: PMCPMC3761664. DOI: 10.1136/bcr-2013-009597
- Kheir WJ, Sheheitli H, Abdul Fattah M, et al. Nontuberculous mycobacterial ocular infections: a systematic review of the literature. Biomed Res Int. 2015;2015:164989. PubMed PMID: 26106601; PubMed Central PMCID: PMCPMC4461732.
- Chen CH, Lin J, Js L, et al. Mycobacterium abscessus complex bacteremia due to prostatitis after prostate biopsy. Indian J Tuberc. 2016 Oct;63(4):273–275. PubMed PMID: 27998503.
- Mooren V, Bleeker MWP, van Ingen J, et al. Disseminated Mycobacterium abscessus infection in a peritoneal dialysis patient. IDCases. 2017;9:6–7. PubMed PMID: 28529886; PubMed Central PMCID: PMCPMC5430147.
- Ko JH, Kang CI, Cho SY, et al. Mycobacterium abscessus glossitis. Lancet Infect Dis. 2017 Oct;17(10):1098. PubMed PMID: 28948933.
- Rodge G, Nagvekar V, Jhala D, et al. Mycobacterium abscessus causing native valve endocarditis due to peripherally inserted central catheter line. J Clin Tuberculosis Other Mycobacterial Dis. 2017;9:19–20. .
- Jeon K, Kwon OJ, Lee NY, et al. Antibiotic treatment of Mycobacterium abscessus lung disease: a retrospective analysis of 65 patients. Am J Respir Crit Care Med. 2009 Nov 1;180(9):896–902. PubMed PMID: 19661243.
- Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007 Feb 15;175(4):367–416. PubMed PMID: 17277290.
- Aly ES, Baig M, Khanna D, et al. Hypercalcaemia: a clue to Mycobacterium avium intracellulare infection in a patient with AIDS. Int J Clin Pract. 1999 Apr-May;53(3):227–228. PubMed PMID: 10665139.
- Newell A, Nelson MR. Hypercalcaemia in a patient with AIDS and Mycobacterium avium intracellulare infection. Int J STD AIDS. 1997 Jun;8(6):405. PubMed PMID: 9179654.