ABSTRACT
Tuberculosis of the central nervous system (CNS-TB) is a critical disease with poor prognosis if not diagnosed and treated early. A regimen of drugs with good CNS penetration is required for treatment. Treatment options are limited in case of hypersensitivity reaction of the recommended regimen. We are reporting a rare instance where a patient developed hypersensitivity to both first line agents (isoniazid and rifampin) for CNS-TB and was successfully desensitized against both these medications to complete the treatment course using the rapid desensitization process. There have been reported cases of desensitization to anti tuberculous medications in cases with pulmonary tuberculosis and hypersensitivity reaction. In this review article we discuss the prior used methods of slow and rapid desensitization in case on non-CNS tuberculosis infections. This is the first reported case to use similar method of rapid desensitization in treatment of central nervous system infection.
1. Case presentation
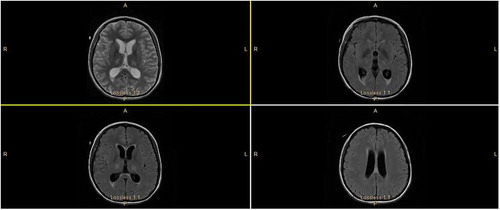
A 19-year old foreign exchange college student from Myanmar, with history of pulmonary tuberculosis presented with a three day history of fever, headache, photophobia and phonophobia. She arrived from Burma to the USA approximately 6 months prior to the presentation. She was taken to a local hospital, underwent a computed tomography of brain that showed findings consistent with hydrocephalus and leptomeningeal enhancement. Patient was transferred to our facility for neurosurgery intervention. She underwent an external ventricular drain placement for acute communicating hydrocephalus and was started on empirical bacterial meningitis coverage with Vancomycin, Ceftriaxone, Ampicillin and Acyclovir. Initial CSF sample during drain placement showed lymphocytic pleocytosis. Patient continued to spike fever the next day while on antimicrobial coverage and repeat MRI was performed. Repeat imaging demonstrated diffuse leptomeningeal enhancement most prominent in basilar cisterns, ventricles, brainstem and cerebellar fossa, consistent with meningoencephalitis as shown in . She had prior history of pulmonary tuberculosis for which she was treated for six months in Myanmar at the age of three. She denied any shortness of breath, hemoptysis or chronic cough. There was no history of tuberculosis in other family members. Patient denied smoking, alcohol use or use of other illicit drugs. Vital signs on presentation were significant for sinus tachycardia and fever of 102.5 degrees Fahrenheit (39.2 degrees Celsius). On physical examination patient had limited range of motion of neck on forward flexion, was oriented to self only, pupils bilaterally were equal and reactive, deep tendon reflexes were ¾ symmetrically in all extremities and clonus was noted in bilateral lower extremity.
2. Investigations
Complete blood count on admission showed no leukocytosis and basic metabolic profile was in normal range as well. CT and MRI report was followed by a cerebrospinal fluid analysis with test results as mentioned in . Further work-up revealed positive Quantiferon TB test (interferon gamma release assay). CSF cultures later grew Mycobacterium tuberculosis, sensitive to all first-line medications. CSF cryptococcal antigen, HSV PCR and serum HIV testing were negative.
Table 1. Cerebrospinal fluid analysis result.
3. Treatment
Antibacterial and antiviral coverage was discontinued after CSF analysis was obtained. In light of history, MRI imaging and CSF analysis, she was empirically started on Isoniazid 300 mg once daily(INH), Rifampin 600 mg once daily (RIF), Pyrazinamide 1000 mg once daily (PZA), Ethambutol 800 mg once daily(EMB), and pyridoxine 50 mg once daily along with dexamethasone taper over 2 weeks. Patient’s mental status improved. Due to hydrocephalus noted on initial head CT, a right extra-ventricular drain was placed, which was later removed and patient underwent weekly lumbar punctures during hospitalization.
4. Follow up
She was admitted to the inpatient rehabilitation unit 5 days after discharge due to cognitive issues which were not amenable to management on an outpatient basis. On regular blood tests she was noted to have elevated liver enzymes, neutropenia and development of generalized pruritic rash. Anti-tuberculous therapy was held. Four days later, she was started on ethambutol and levofloxacin (LVF). When liver enzymes trended down, isoniazid(INH) was restarted 14 days later. She developed a rash immediately and INH was again stopped. RIF was re-introduced 3 days later and patient developed a rash immediately and rifampin had to be discontinued as well. Five days later, PZA was restarted but this resulted in worsening of liver enzymes, necessitating cessation of pyrazinamide within 72 hours. Given the nature of the disease, it was decided to desensitize the patient to both isoniazid and rifampin in rapid succession to ensure continuation of an optimal antimicrobial regimen. Patient was transferred to ICU and started on desensitization protocol for RIF and INH ( and ). She tolerated desensitization without any issues and continued with a 4-drug regimen of EMB, RIF, INH and LVF with no new issues. She was discharged home 1 week later but was readmitted in 3 days with development of generalized seizures. MRI was repeated that confirmed worsening hydrocephalus, obstruction at level of fourth ventricle, associated debris obstructing foramen of Lushka and Magendie greater on left due to tuberculoma formation, requiring ventriculoperitoneal shunt (VP shunt) placement. She also developed steroid induced acne and herpes zoster which resolved with gradual steroid taper and oral acyclovir respectively.
Table 2. Isoniazid desensitization.
Table 3. Rifampin desensitization.
5. Outcome
The patient tolerated rapid oral desensitization and was able to continue a 4-drug regimen (INH, RIF, EMB, LVF) for two months which was subsequently simplified to a 2-drug regimen (INH and RIF) for total of 24 months. She rejoined college 1 year after last hospitalization. Follow up MRI one year showed residual nodule in inferior margin of fourth ventricle, reduced in size.
6. Discussion
Hypersensitivity to multiple anti-tuberculous agents presents a challenge and has been reported in few medical literature. Discontinuing the first-line agents in the event of hypersensitivity may significantly compromise the cure rate of tuberculosis. For pulmonary tuberculosis, patients who develop hypersensitivity to first line drug can be switched to second line therapy such as streptomycin and levofloxacin. In CNS infection, treatment options remain limited due to need for good CSF penetration. Drug desensitization can be an effective method allowing continued use of the first-line agents and achieving successful cure of tuberculosis.
American academy of allergy, asthma and immunology recommends against desensitization in severe drug reactions [Citation1]. In rare circumstances, with severe underlying disease and limited treatment options available, desensitization process may be necessary. Krittaecho et al in their recent study studied the outcome with drug desentization, and even in prior severe drug reaction, the success rate was 62.5% [Citation2]. Though they used a low dose for initiation of desensitization and also slower increase in dose as compared Thong et al [Citation3] There have been several other case reports of drug desensitization for antituberculous therapy [Citation4–Citation8]. Interestingly, there have been reported cases of resistance during desensitization process as well [Citation8].
With multi drug regimen for treatment of infection such as tuberculosis, identifying the ‘culprit’ drug is a challenge, as in our case. A patch test has been used for suspected drug reaction due to one drug but a negative test result cannot be completely relied on as the spectrum of allergic reaction due to the drugs remain variable and broad [Citation9,Citation10]. Another method, lymphocyte transformation test that measures the proliferation of T cells to a drug in vitro, can be useful but has limited availability and low sensitivity [Citation11]. Clinical correlation with detailed history and monitoring on reintroduction of each drug gradually is most commonly used. Since our patient developed skin rash, neutropenia and elevated liver enzymes on 4-drug regimen all medications had to be stopped transiently. Gradual introduction of medication based on known side effect profile is the next best step in cases such as ours when antimicrobial treatment cannot be held.
Drug reactions have been classified into non immediate and immediate based on occurrence of symptoms within one hour of exposure versus greater than one hour of exposure to the drug [Citation12]. The reactions are IgE mediated and T cell mediated respectively. Sherer et al provided a comprehensive review of different types of drug reaction and defined desensitization as a ‘procedure describing the induction of a clinical tolerance to a drug responsible for previous allergic reaction’. ‘Treating through’ was another term used by Scherer et al to describe mild allergic reaction to the drug during desensitization process that would resolve without stopping the medication.
There have been reported studies to support slower protocol versus rapid desensitization protocol of desensitization. The process should be in a stepwise manner in either case. The benefits of restarting the medication should be weighed against the risk. The adverse reaction should have resolved or atleast stabilized prior to the process. In our patient with severe CNS-TB, we waited for stabilization of liver enzymes and resolution of rash before rapid desensitization process under close supervision in intensive care unit. The rapid protocol with gradual increment in dose over few hours have advantage of faster desensitization but have shown to have higher failure rate in drug reaction. Holland et al and Kim et al reported use of rapid oral desensitization process to more than one anti tuberculous drugs with positive results. [5,7] In our patient a rapid protocol was chosen due severity of illness and need to start anti tuberculous therapy as soon as possible. Protocol followed is shown in and . Also, premedication with antihistamines and steroids is commonly used but there is no consensus regarding use of these medication in delayed hypersensitivity reactions [Citation13,Citation14]. Recent studies by Sasaki et al and Akduman et al support the use of rapid protocol as well [Citation15,Citation16]. Slower protocol can tend to be more effective than rapid protocols, but no clinical trials comparing the two exist, and clinical need for restarting therapy in severely ill patients may warrant trying the rapid protocol in such cases to improve patient outcome.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Joint Task Force on Practice P, American Academy of Allergy A, Immunology, American College of Allergy A, Immunology, Joint Council of Allergy A, et al. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol. 2010;105:259–273.
- Siripassorn K, Ruxrungtham K, Manosuthi W. Successful drug desensitization in patients with delayed-type allergic reactions to anti-tuberculosis drugs. Int J Infect Dis. 2018 Feb 1. DOI:10.1016/j.ijid.2018.01.006 pii: S1201-9712(18)30006-7.
- Thong BY, Chia FL, Tan SC, et al. A retrospective study on sequential desensitization-rechallenge for antituberculosis drug allergy. Asia Pac Allergy. 2014;4:156–163.
- Buergin S, Scherer K, Hausermann P, et al. Immediate hypersensitivity to rifampicin in 3 patients: diagnostic procedures and induction of clinical tolerance. Int Arch Allergy Immunol. 2006;140:20–26.
- Holland CL, Malasky C, Ogunkoya A, et al. Rapid oral desensitization to isoniazid and rifampin. Chest. 1990;98:1518–1519.
- Kura MM, Hira SK. Reintroducing antituberculosis therapy after Stevens-Johnson syndrome in human immunodeficiency virus-infected patients with tuberculosis: role of desensitization. Int J Dermatol. 2001;40:481–484.
- Kim JH, Kim HB, Kim BS, et al. Rapid oral desensitization to isoniazid, rifampin, and ethambutol. Allergy. 2003;58:540–541.
- Horne NW, Grant IW. Development of drug resistance to isoniazid during desensitization: a report of two cases. Tubercle. 1963;44:180–182.
- Arruti N, Villarreal O, Bernedo N, et al. Positive allergy study (Intradermal, Patch, and Lymphocyte Transformation Tests) in a case of isoniazid-induced DRESS. J Investig Allergol Clin Immunol. 2016;26:119–120.
- Rebollo S, Sanchez P, Vega JM, et al. Hypersensitivity syndrome from isoniazid with positive patch test. Contact Dermatitis. 2001;45:306.
- Schreiber J, Zissel G, Greinert U, et al. Lymphocyte transformation test for the evaluation of adverse effects of antituberculous drugs. Eur J Med Res. 1999;4:67–71.
- Demoly P, Pichler W, Pirmohamed M, et al. Important questions in Allergy: 1–drug allergy/hypersensitivity. Allergy. 2008;63:616–619.
- Scherer K, Brockow K, Aberer W, et al. Desensitization in delayed drug hypersensitivity reactions – an EAACI position paper of the drug allergy interest group. Allergy. 2013;68:844–852.
- Romano A, Artesani M, Andriolo M, et al. Effective prophylactic protocol in delayed hypersensitivity to contrast media: report of a case involving lymphocyte transformation studies with different compounds. Radiology. 2002;225:466–470.
- Sasaki Y, Kurashima A, Morimoto K, et al. Experience of rapid drug desensitization therapy in the treatment of mycobacterial disease. Kekkaku:[Tuberculosis]. 2014 Nov;89(11):797–802.
- Akduman AE, Sarıman N, Yaman G, et al. A case of rib tuberculosis and chest wall abscess with multi-drug hypersensitivity reactions. Mikrobiyol Bul. 2015 Jul;49(3):454–460.