ABSTRACT
Background: Hospitalized patients with diabetes are at risk of complications and longer length of stay (LOS). Inpatient Diabetes Management Services (IDMS) are known to be beneficial; however, their impact on patient care measures in community, non-teaching hospitals, is unknown.
Objectives: To evaluate whether co-managing patients with diabetes by the IDMS team reduces LOS and 30-day readmission rate (30DR).
Methods: This retrospective quality improvement cohort study analyzed LOS and 30DR among patients with diabetes admitted to a community hospital. The IDMS medical team consisted of an endocrinologist, nurse practitioner, and diabetes educator. The comparison group consisted of hospitalized patients with diabetes under standard care of attending physicians (mostly internal medicine-trained hospitalists). The relationship between study groups and outcome variables was assessed using Generalized Estimating Equation models.
Results: 4,654 patients with diabetes (70.8 ± 0.2 years old) were admitted between January 2016 and May 2017. The IDMS team co-managed 18.3% of patients, mostly with higher severity of illness scores (p < 0.0001). Mean LOS in patients co-managed by the IDMS team decreased by 27%. Median LOS decreased over time in the IDMS group (p = 0.046), while no significant decrease was seen in the comparison group. Mean 30DR in patients co-managed by the IDMS decreased by 10.71%. Median 30DR decreased among patients co-managed by the IDMS (p = 0.048).
Conclusions: In a community hospital setting, LOS and 30DR significantly decreased in patients co-managed by a specialized diabetes team. These changes may be translated into considerable cost savings.
1. Introduction
Diabetes mellitus is a common disease that is prevalent in 9.4% of the USA population, or about 30.3 million people [Citation1], while many remain undiagnosed [Citation1,Citation2]. Most affected people have type 2 diabetes (90–95%), and there is a higher prevalence of diabetes in elderly and obese patients [Citation2,Citation3]. The high prevalence of diabetes and its complications make it a common comorbid condition in hospitalized patients [Citation2]. Uncontrolled glycemia due to diabetes is associated with adverse outcomes including death [Citation4–Citation6]. Compared to patients without diabetes, those with diabetes may require more hospitalizations per year, have a longer length of stay (LOS), and have more hospital complications and mortality rates [Citation2,Citation7].
Diabetes is an expensive disease. The estimated cost of diagnosed diabetes care in the U.S. was $327 billion in 2017 [Citation8,Citation9], and a major proportion of this expense was from hospitalizations and medications [Citation10]. Thus, hospitals may be under pressure to cut healthcare costs given limited resources. The Centers of Medicare and Medicaid Services (CMS) in collaboration with a number of U.S. states is implementing initiatives which would ‘incentivize hospitals to reduce avoidable readmissions by linking rewards and penalties to improvements in readmissions rates, and to the attainment of relatively low readmission rates’ [Citation11]. On January 1st 2014, the State of Maryland started a new All-Payer Model demonstration contract with the CMS Innovation Center, called the Readmission Reduction Incentive Program [Citation11]. This may create financial incentives for hospitals to reduce readmissions and hospital utilization [Citation12].
The Disease Management Association of America identifies diabetes as one of the chronic conditions with the greatest potential for management [Citation3]. A number of studies have evaluated the impact of a specialized endocrinology/diabetes team on the glycemic control of hospitalized patients and their LOS [Citation13-Citation15], and some found that such teams decrease of LOS [Citation16,Citation17].
To our knowledge, however, no study has evaluated the effects of implementing such a team at a community, non-teaching hospital. While non-teaching hospitals greatly outnumber teaching hospitals in the US, it has been suggested that patient outcomes in non-teaching hospitals are worse [Citation18]. One possibly for this discrepancy may be that innovative and effective practices enacted at major academic centers are slower to be implemented at smaller non-teaching hospitals. However, as scope, staffing, and resources are often significantly smaller at non-teaching community hospitals as compared to major academic centers, it is vital to evaluate which strategies deemed effective at the university level can be successfully implemented, efficacious, and cost-effective in the community hospital setting.
Suburban Hospital, a 240-bed community hospital in suburban Maryland, implemented an Inpatient Diabetes Management Service (IDMS) at the end of 2015, designed after a successful model at Johns Hopkins Hospital in Baltimore, Maryland [Citation19].
This retrospective quality improvement cohort study investigated the impact of the IDMS on LOS and 30-day readmission rates (30DR) for patients with diabetes admitted to Suburban Hospital over a 17-month period. The hypothesis was that patients co-managed by providers from the IDMS team would have reduced LOS and 30DR.
2. Materials and methods
2.1. Study population
Diabetes mellitus was defined as any medical International Statistical Classification of Diseases and Related Health Problems (ICD-10) listed as discharge diagnosis (primary or secondary), based on the provider’s documentation. The following ICD-10 codes were used: E08 (Diabetes mellitus due to underlying condition), E09 (Drug or chemical induced diabetes mellitus), E10 (Type 1 diabetes), E11 (Type 2 diabetes), or E13 (Other specified diabetes). De-identified hospitalized patient data were extracted from the electronic medical records between 1 January 2016, and 31 May 2017.
2.2. Exposure: Inpatient Diabetes Management Service (IDMS)
2.2.1. Implementation of the IDMS
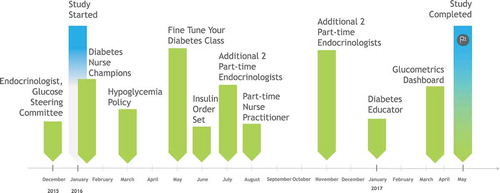
The IDMS at the study hospital was implemented at the end of 2015. A detailed timeline of the IDMS implementation is presented in . The IDMS model had three goals: (1) using structured knowledge dissemination, engage and educate hospital staff on the methods and importance of best practice inpatient glycemic management; (2) develop policies and clinical decision aids from evidence-based inpatient glucose management studies, and (3) assess process measures, as well as glucometric, clinical, and economic outcomes to determine intervention effectiveness.
2.2.1.1. A team of medical providers
A main component of the IDMS was creating a team of providers that specialized in diabetes treatment and provided direct care to the study group. Initially, it consisted of one full-time board-certified inpatient endocrinologist. Six months into the study period, two part-time ‘moonlighter’ endocrinologists joined the team, as the volume of consultations had gradually increased. The service expanded from 5 days per week to 6 days per week. By the end of the study period, the IDMS team consisted of one full-time endocrinologist, four part-time endocrinologists and one part-time nurse practitioner.
2.2.1.2. Glucose steering committee
A Glucose Steering Committee at Suburban Hospital was created at the end of 2015. It was comprised of multidisciplinary health care providers and a member of the Patient and Family Advisory Council to address various aspect of diabetes management. They developed diabetes policies, safety monitoring, and educational materials.
2.2.1.3. Diabetes nurse champions
A Diabetes Nurse Champions committee, modelled after a similar initiative at Johns Hopkins Hospital [Citation19,Citation20], was established in January 2016. It incorporated nursing staff from most hospital units. This active group of ‘diabetes champions’ provided one-on-one and group education sessions for all other nurses using a ‘train-the-trainer’ approach to increase nurses’ exposure to this information. Every nursing unit was supplied with ‘diabetes education kits’ that contain the tools needed for teaching patients to monitor and track their blood glucose.
2.2.1.4. Hypoglycemia policy
A formal evidence-based hypoglycemia protocol and nurse-driven treatment algorithm were developed to provide safe and effective management of hypoglycemia throughout the hospital.
2.2.1.5. Targeted education and clinical decision support
Hospital-wide glucose policies were coupled with targeted education and clinical decision support to facilitate policy acceptance and uptake by staff.
Medical providers from the IDMS team provided 48 interactive educational lectures, ‘lunch-n-learns’ and ‘in-services’ for medical and nursing staff during the study period. Examples of the topics include: basal-bolus insulin therapy, hypoglycemia and steroid-induced hyperglycemia treatment, perioperative glycemic management, diabetes ketoacidosis, transitioning of patients from intravenous insulin infusion to subcutaneous injections, discharge instructions for patients with diabetes, and managing patients on insulin pumps. iPad tablets preloaded with diabetes information have also been made available to patients and hospital staff.
2.2.1.6. Fine tune your diabetes class
The Suburban Hospital Community Health and Wellness Department created an educational program in May 2016, in which selected patients could be ‘prescribed’ a ‘Fine Tune Your Diabetes’ class that they would attend after being discharged. During this one-time session, certified diabetes educators and pharmacists discussed important components of diabetes care such as exercise, proper nutrition, and emotional and physical concerns. One-on-one sessions were offered, where each patient set his or her diabetes goals and learned to properly track their glucose levels.
2.2.1.7. Uniform subcutaneous insulin order set
The uniform subcutaneous insulin order set was updated and made available for all medical providers.
2.2.1.8. Certified diabetes educator
An inpatient Certified Diabetes Educator (CDE) joined the IDMS team in January 2017. The CDE educated and supported patients to understand and live well with diabetes. The nurse educator assisted patients with diabetes by walking them through reviewed their personalized treatment plan for diabetes and educated them about components of diabetes such as nutrition, exercise, and medications.
2.2.1.9. Glucometrics dashboard
The IDMS at Johns Hopkins Hospital in collaboration with the Johns Hopkins Armstrong Institute for Patient Safety and Quality and Diabetes Clincal Communities developed a glucometrics dashboard – a readily accessible online platform which assessed a number of glycemic-related metrics in the five hospitals of the Johns Hopkins Health System in Maryland and Washington, DC [Citation19,Citation21].
2.2.2. Identification of patients co-managed by the IDMS team
Patients co-managed by the IDMS medical providers were identified by the ‘type’ of endocrinology consultation note placed by one of the IDMS medical providers and unique billing area code. The following ‘consultation trigger’ guidelines were given to medical staff to request diabetes consultation from the medical IDMS team: (1) uncontrolled glycemia (glucose < 60 mg/dL, or glucose > 250 mg/dL); (2) uncontrolled diabetes in patients who recently underwent cardiac surgery; (3) high dose of glucocorticoids therapy; (3) newly diagnosed type 1 diabetes mellitus, admitted with diabetic ketoacidosis; (4) newly diagnosed uncontrolled type 2 diabetes; (5) patients on an insulin pump. The majority of consultations were requested via an electronic medical record order system, while some were requested in person and/or over the phone/paging system.
2.2.3. Identification of comparison study group
The comparison group was hospitalized patients with diabetes who were not co-managed by the medical providers from the IDMS team. These patients were under standard care of attending physicians (mostly Internal Medicine-trained hospitalists).
2.3. Outcomes: length of stay and 30-day readmission rates
The Premier Quality Advisor™ Platform was used to perform the initial analysis. The arithmetic LOS was calculated from the admission and discharge date of each patient. 30DR were calculated by determining the number of patients who returned exclusively to the study hospital within 30 days, using a similar methodology as the CMS [Citation22]. This rate excludes patients who expired on their first admission, were transferred to another facility or left against medical advice. The readmission rate includes only acute inpatients. Psychiatric, oncology and all observation patients were excluded. A 30-day cutoff for readmissions was chosen because it is conventionally referenced in existing readmission reports and is a publicly reported metric [Citation22], and it is also the cutoff used by the State of Maryland to measure financials and reimbursements [Citation11].
2.4. Calculation of potential cost savings
Potential cost savings based on LOS reduction were calculated using the following formula: Cost savings = ((LOS baseline-LOS month1) × N co-managed patients × Cost per one day of admission)month1 + ((LOS baseline-LOS month2) × N co-managed patients × Cost per one day of admission)month2 +… Average variable direct cost per admission ($3,500) and average LOS data (4.24 days during the period July-April 2017) were provided by the hospital’s administration.
2.5. The severity of illness score
The All Patient Refined Severity Levels are proprietary to 3M Health Information Systems. This methodology assigns a severity of illness score (minor, moderate, severe, or extreme) based on information specific to the patient population, as previously described [Citation23].
2.6. Statistical analysis
Data are described as frequencies and percentages or mean ± SD, unless otherwise indicated. The Kolmogorov-Smirnov test was used to test normality in continuous variables. In addition, histograms, stem-and-leaf plots, probability-probability plots, and quantile-quantile plots were generated to evaluate the variable’s distribution. Data were compared between the groups of patients (co-managed by the IDMS versus comparison group) using Chi-square tests for categorical variables, independent two sample T-test for normally distributed continuous variables, and Wilcoxon Rank Sum Test for continuous variables with non-normal distribution.
Generalized estimating equation models (GEE) were used to determine the significance of the data for LOS and 30DR, the relationship between patient consultation and outcome variables, and to account for multiple patient visits within the timeframe. Missing values were investigated and considered missing at random. Observations with missing values are automatically excluded from the GEE. Binomial distribution with a logit link function was used for readmission models. LOS was modelled with a negative binomial distribution. Percentage change in LOS and 30DR was computed based on the change from mean baseline to the last study month.
Three statistical models were used for this study. Each model analyzed the interaction between LOS and 30DR by factoring in different variables with the study group (patients co-managed by the IDMS team). Model 1 included study group, study month, and an interaction term between study group and study month only; Model 2 included Model 1 data plus sex, age, race, and ethnicity; Model 3 included Model 2 plus number of comorbidities, diabetes type, and disease severity. These models were used to assess the significance of a decrease in LOS and 30DR for the IDMS team. Results were tested against a comparison group, which was the patients with diabetes who were not co-managed by the IDMS team during the study period. Statistical analyses were performed using PROC FREQ (Chi-Square Tests), PROC NPAR1WAY (Wilcoxon Rank Sum Tests), PROC UNIVARIATE (Normality Tests and plots), and PROC GENMOD (GEE analysis) in SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA). Figures were generated using PROC SGPLOT and Microsoft PowerPoint.
3. Results
3.1. Demographics
Overall, the study population consisted of an elderly (median age 72 years), majority white (53.7%) population of patients with type 2 diabetes (94.7%) (). These patients had a significant number of comorbidities. The most prevalent were hypertension (51.8%), chronic kidney disease (31.6%), and heart failure (25.9%). Accordingly, the severity of illness was found to be major in 41.2% and extreme in 12.2%. The overall mortality rate was 3.5%.
Table 1. Characteristics of study patients.
There were several notable differences when comparing patients in the experimental group, co-managed by the IDMS team versus the control group. Patients in the experimental group were younger (median 67 vs. 73 years, p < 0.001), more likely to be male (55.8% vs. 50.8%, p = 0.02), more likely to have type 1 diabetes (9.3% vs. 1.5%, p < 0.0001), and had higher severity of illness scores (51% vs. 39.9% had major illness score, p < 0.0001). Mortality was lower in the IDMS patients (1.6% vs. 4%, p = 0.001).
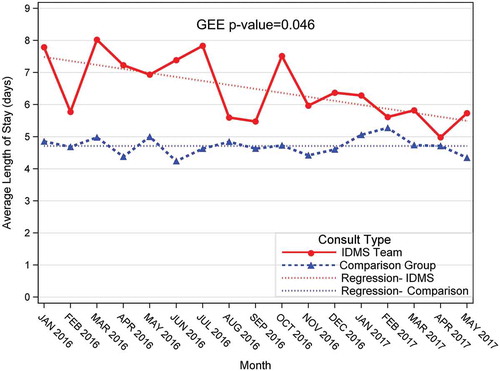
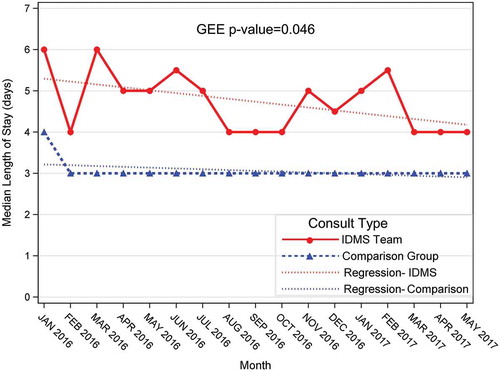
3.2. Length of stay
Patients cared for by the IDMS team had a longer LOS than the comparison group [median 5 days (interquartile range [IQR] = 5) versus median 3 days (IQR = 3); p < 0.0001] (). Over time, however, a statistically significant decrease in LOS was seen in the IDMS group, compared to the non-IDMS group (p = 0.046) (-Model 3). There was no significant change in LOS in the non-IDMS group. Mean LOS in patients co-managed by the IDMS team decreased from 7.8 days to 5.7 days over time (27% reduction) (). Median LOS over the study period in patients co-managed by the IDMS team decreased as well (p = 0.046) ().
Table 2. Analysis of length of stay.
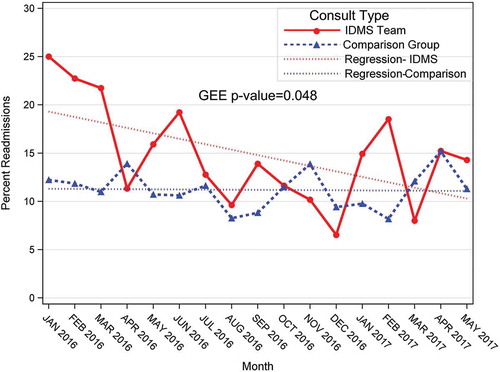
3.3. 30-day readmission rates
The 30DR in patients cared for by the IDMS team were higher (14.8% versus 11.2%; p = 0.005) (); however, there was an observed significant decrease in readmissions for patients co-managed by the IDMS team versus non-IDMS patients (p = 0.048) (-Model 3). No statistical significance was found in the readmission rate of the comparison group. Mean 30DR in patients co-managed by the IDMS team decreased over time from 25% to 14.29% (10.71% reduction) ().
Table 3. Analysis of 30-day readmissions.
3.4. The cost of care savings
Based on LOS decrease over time, the hospital had an estimated potential cost of care savings of $953,578.56 during the study period.
4. Discussion
This study found that despite higher LOS and 30DR among patients co-managed by a specialized IDMS team, reductions in both of these metrics were observed in patients co-managed by a specialized IDMS team in a community non-teaching hospital. The higher LOS and 30DR can likely be explained by the higher severity of illness in patients co-managed by the IDMS, as well as a greater proportion of patients with type 1 diabetes.
Our findings are consistent with other studies on trends in LOS and 30DR in hospitalized patients with diabetes. A number of studies have found that patients with diabetes have overall higher LOS and/or 30DR [Citation24–Citation32] when compared to patients who do not have diabetes. Comino, et al. reported that readmission rates in 23,779 study patients with diabetes were between 2–6 times higher than those who did not have diabetes [Citation24]. Mean LOS in patients admitted for over one day were 8.2 days in patients with diabetes and 7.1 days in those without. Additionally, patients with diabetes were found to be 24% more likely to be readmitted to a hospital in a yearlong period versus those without [Citation24]. Drincic and colleagues studied 66,518 patient records and found that 30-day readmission rates for patients with diabetes were 20.1%, which was higher than the overall hospital readmission rate (14.6%) [Citation26].
Another study analyzed data from all 1,502 patients admitted to an acute medical unit in a hospital in the UK emphasized the relationship between dysglycemia, LOS, and 28-day readmissions regardless of the diagnosis of diabetes [Citation33]. They found that high blood glucose levels in hospitalized patients were associated with worse outcomes concerning LOS, 28-day mortality, and 28-day readmission rates. Patients with blood glucose levels > 6.5 mmol/l (117.12 mg/dL) on admission had a significant difference in LOS when compared to those with blood glucose of < 6.5 mmol/l (117.12 mg/dL) on admission, where mean LOS was 10.8 days and 8.8 days, respectively [Citation33]. Our findings are also consistent with the published literature, where about a quarter of all admitted hospital patients that have diabetes are more likely to originate from emergency departments [Citation26,Citation34], rather than planned admissions (e.g., planned surgery).
Studies that evaluated specialized healthcare teams to manage patients with diabetes found that multidisciplinary and interactive teams were effective in providing improved care for patients with diabetes [Citation8,Citation25,Citation26,Citation34,Citation35]. Increased diabetes education for healthcare providers and/or increased nursing training may be especially effective [Citation8,Citation25,Citation36,Citation37]. When diabetes-related educational policies were targeted at nurses, medical providers, and patients, a decrease in LOS was observed [Citation17–Citation38]. Most, but not all, studies have found associations between the presence of IDMS teams and reduced LOS and 30DR [Citation8,Citation16,Citation24–Citation26,Citation33,Citation34,Citation39]. Horton and colleagues evaluated the effects of a guideline-derived physician resident educational program on LOS and observed a decrease in LOS after the guidelines were implemented (5.03 days vs 6.98 days; P = 0.042) [Citation16].
Another study of 169 inpatients with diabetes found the adjusted LOS decreased by 25% (95% CI, 9%-44%) after a detailed subcutaneous insulin protocol and an admission order set was implemented [Citation17]. Healy, et al emphasized the effect of patient diabetes education on decreasing 30-day readmission rates among patients with diabetes who received inpatient diabetes education consults versus those who did not (33 vs. 44%; p = 0.0001; unadjusted OR 0.62 [95% CI 0.48–0.80]; p = 0.0001) [Citation39]. Bansal, et al., found that 30DR in non-critical medical units was reduced around 30% in diabetes patients when a specialized diabetes team was involved in inpatient diabetes care, and they found that a consultation from a specialized diabetes team within 24 hours of patient admission was associated with a significantly shorter LOS [Citation34].
Does better diabetes care translate into potential healthcare savings? Healthcare systems and providers already recognize the importance of decreasing the costs spent on diabetes care and comorbid complications. However, it is not often clear how much a hospital could save by decreasing the LOS and/or 30DR, given that multiple factors are used to calculate the cost of care for one patient, and the ‘Global budget’ initiative in Maryland [Citation8]. Bansal et al estimated $2.9-$3.5 million in savings in 2011–2012 due to a decrease in 30DR after deployment of the specialized diabetes team [Citation34]. This study estimated that decreasing diabetes patient LOS may have saved the case-hospital almost a million U.S. dollars.
Our study has limitations. As with all before-after study designs, it was not possible to make inferences regarding causation with respect to the implementation of the IDMS and the outcomes of interest, since other confounders may have been present during the study period and were not accounted for. Both study groups have been exposed to the implementation of hospital-wide glucose policies and educational initiatives. Our study may have a selection bias, as providers from the IDMS team were consulted on more sick and complex patients with diabetes. No information was available about the study patients being admitted to any other hospital.
5. Conclusions
Implementation of an IDMS team at a community non-teaching hospital significantly correlated with a decrease over time in LOS and 30DR for patients with diabetes co-managed by the IDMS team. Inpatient glucose management remains an important area for patient safety, quality improvement, and clinical research, and the implementation model should guide other community hospitals in their glucose management initiatives. Implementing programs like the IDMS may result in better patient care, shorter LOS, reduced 30DR, and potential health care cost savings.
Acknowledgments
Authors thank Diane Cooper and the NIH Library for assistance in writing this manuscript. Authors are grateful for the assistance of Christina Wilson for providing support with the data collection. Authors also thank members of the Glucose Steering Committee at Suburban Hospital (Barbara Kahl, Cora Abundo, Eileen Peters, Gwendolyn Cain, Iniuboho Akpandak, Joyce Wedler, Lee Ann Alexander, Leni Barry, Lulu Fulda, Mahsa Motevalli, Margie Hackett, Mary Flynn, Patricia Rios and Roliette Gooding) for investing their time in developing diabetes initiatives. Authors thank Atul Rohatgi and Eric Park for assistance and support in developing the Inpatient Diabetes Management Service. Authors thank Jacky Schultz, LeighAnn Sidone, Eric Dobkin, Sunil Vasudevan, Thomas Stewart, Joseph Linstrom, and the rest of Suburban Hospital’s leadership for providing endless support for the inpatient diabetes initiative. Authors thank Robert Rothstein for providing continuous support and sharing his vision for the program.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2017. Available from: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
- Ostling S, Wyckoff J, Ciarkowski SL, et al. The relationship between diabetes mellitus and 30-day readmission rates. Clin Diabetes Endocrinol. 2017 March 22;3(1):3.
- Dalal MR, Robinson SB, Sullivan SD. Real-world evaluation of the effects of counseling and education in diabetes management. Diabetes Spectr. 2014 Nov;27(4):235–243. PubMed PMID: 25647045; PubMed Central PMCID: PMCPMC4231931.
- American Diabetes A. 14. Diabetes care in the hospital. Diabetes Care. 2017 Jan;40(Suppl 1):S120–S127. PubMed PMID: 27979901.
- Clement S, Braithwaite SS, Magee MF, et al. Management of diabetes and hyperglycemia in hospitals. Diabetes Care. 2004;27(2):553–591.
- Moghissi ES, Korytkowski MT, DiNardo M, et al. American association of clinical endocrinologists and American diabetes association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32(6):1119–1131.
- Umpierrez GE, Hellman R, Korytkowski MT, et al. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012 Jan;97(1):16–38. PubMed PMID: 22223765.
- Golden SH, Maruthur N, Mathioudakis N, et al. The case for diabetes population health improvement: evidence-based programming for population outcomes in diabetes. Curr Diab Rep. 2017 Jul;17(7):51. PubMed PMID: 28567711; PubMed Central PMCID: PMCPMC5553206.
- American Diabetes A. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018 May;41(5):917–928. PubMed PMID: 29567642; PubMed Central PMCID: PMCPMC5911784.
- Ozieh MN, Bishu KG, Dismuke CE, et al. Trends in health care expenditure in U.S. adults with diabetes: 2002–2011. Diabetes Care. 2015;38(10):1844–1851.
- Comission TMHSCR. Readmission reduction incentive program. 2018 [cited 2018 Dec 06]. Available from: http://www.hscrc.state.md.us/Pages/init-readm-rip.aspx
- Roberts ET, McWilliams J, Hatfield LA, et al. Changes in health care use associated with the introduction of hospital global budgets in maryland. JAMA Intern Med. 2018;178(2):260–268.
- Levetan CS, Salas JR, Wilets IF, et al. Impact of endocrine and diabetes team consultation on hospital length of stay for patients with diabetes. Am J Med. 1995 Jul;99(1):22–28. PubMed PMID: 7598138.
- Koproski J, Pretto Z, Poretsky L. Effects of an intervention by a diabetes team in hospitalized patients with diabetes. Diabetes Care. 1997 Oct;20(10):1553–1555. PubMed PMID: 9314634.
- Simmons D, Hartnell S, Watts J, et al. Effectiveness of a multidisciplinary team approach to the prevention of readmission for acute glycaemic events. Diabet Med. 2015 Oct;32(10):1361–1367. PubMed PMID: 25865087.
- Horton WB, Weeks AQ, Rhinewalt JM, et al. Analysis of a guideline-derived resident educational program on inpatient glycemic control. South Med J. 2015 Oct;108(10):596–598. PubMed PMID: 26437188.
- Schnipper JL, Ndumele CD, Liang CL, et al. Effects of a subcutaneous insulin protocol, clinical education, and computerized order set on the quality of inpatient management of hyperglycemia: results of a clinical trial. J Hosp Med. 2009 Jan;4(1):16–27. PubMed PMID: 19140191.
- Burke LG, Frakt AB, Khullar D, et al. Association between teaching status and mortality in US hospitals. JAMA. 2017 May 23;317(20):2105–2113. PubMed PMID: 28535236; PubMed Central PMCID: PMCPMC5815039.
- Munoz M, Pronovost P, Dintzis J, et al. Implementing and evaluating a multicomponent inpatient diabetes management program: putting research into practice. Jt Comm J Qual Patient Saf/Jt Comm Resour. 2012 May;38(5):195–206. PubMed PMID: 22649859; PubMed Central PMCID: PMC3697928.
- Kemmerer T, Bashura H, Dintzis J, et al. The impact of nursing and advanced practice clinicians on the implementation and outcomes of an inpatient glucose management program. AADE Pract. 2015;3(5):16–25.
- Golden SH, Hager D, Gould LJ, et al. A gap analysis needs assessment tool to drive a care delivery and research agenda for integration of care and sharing of best practices across a health system. Jt Comm J Qual Patient Saf. 2017 Jan;43(1):18–28. PubMed PMID: 28334581.
- McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015 May 19;131(20):1796–1803. PubMed PMID: 25986448; PubMed Central PMCID: PMCPMC4439931.
- Magee G, Zaloga GP, Turpin RS, et al. A retrospective, observational study of patient outcomes for critically ill patients receiving parenteral nutrition. Value Health. 2014 Jun;17(4):328–333. PubMed PMID: 24968991.
- Comino EJ, Harris MF, Islam MD, et al. Impact of diabetes on hospital admission and length of stay among a general population aged 45 year or more: a record linkage study. BMC Health Serv Res. 2015 Jan 22;(15):12. PubMed PMID: 25609196; PubMed Central PMCID: PMCPMC4310177.
- Dungan KM. The effect of diabetes on hospital readmissions. J Diabetes Sci Technol. 2012 Sep 1;6(5):1045–1052. PubMed PMID: 23063030; PubMed Central PMCID: PMCPMC3570838.
- Drincic A, Pfeffer E, Luo J, et al. The effect of diabetes case management and diabetes resource nurse program on readmissions of patients with diabetes mellitus. J Clin Transl Endocrinol. 2017 Jun;8:29–34. PubMed PMID: 29067256; PubMed Central PMCID: PMCPMC5651336.
- Cromarty J, Parikh S, Lim WK, et al. Effects of hospital-acquired conditions on length of stay for patients with diabetes. Intern Med J. 2014 Nov;44(11):1109–1116. PubMed PMID: 25070621.
- Valent F, Tonutti L, Grimaldi F. Does diabetes mellitus comorbidity affect in-hospital mortality and length of stay? Analysis of administrative data in an Italian academic hospital. Acta Diabetol. 2017 Dec;54(12):1081–1090. . PubMed PMID: 28916936.
- Martin WG, Galligan J, Simpson S Jr., et al. Admission blood glucose predicts mortality and length of stay in patients admitted through the emergency department. Intern Med J. 2015 Sep;45(9):916–924. PubMed PMID: 26109328.
- Gregory NS, Seley JJ, Dargar SK, et al. Strategies to prevent readmission in high-risk patients with diabetes: the importance of an interdisciplinary approach. Curr Diab Rep. 2018 Jun 21;18(8):54. PubMed PMID: 29931547.
- Thomas MC. Perspective review: type 2 diabetes and readmission for heart failure. Clin Med Insights Cardiol. 2018;12:1179546818779588. PubMed PMID: 29899670; PubMed Central PMCID: PMCPMC5992798.
- Krall JS, Donihi AC, Hatam M, et al. The Nurse Education and Transition (NEAT) model: educating the hospitalized patient with diabetes. Clin Diabetes Endocrinol. 2016;2:1. PubMed PMID: 28702237; PubMed Central PMCID: PMCPMC5471889.
- Evans NR, Dhatariya KK. Assessing the relationship between admission glucose levels, subsequent length of hospital stay, readmission and mortality. Clin Med (Lond). 2012 Apr;12(2):137–139. PubMed PMID: 22586788.
- Bansal V, Mottalib A, Pawar TK, et al. Inpatient diabetes management by specialized diabetes team versus primary service team in non-critical care units: impact on 30-day readmission rate and hospital cost. BMJ Open Diabetes Res Care. 2018;6(1):e000460. PubMed PMID: 29657719; PubMed Central PMCID: PMCPMC5892752.
- Black RL, Duval C. Diabetes discharge planning and transitions of care: a focused review. Curr Diabetes Rev. 2018 Jul 11. DOI:10.2174/1573399814666180711120830. PubMed PMID: 29992890.
- Rajendran R, Kerry C, Round RM, et al. Impact of the Diabetes Inpatient Care and Education (DICE) project and the DICE care pathway on patient outcomes and trainee doctor’s knowledge and confidence. Diabet Med. 2015 Jul;32(7):920–924. PubMed PMID: 25819323.
- Kangas S, Rintala TM, Jaatinen P, An integrative systematic review of interprofessional education on diabetes. J Interprof Care. 2018 Jul 24:1–13. PubMed PMID: 30040507. DOI:10.1080/13561820.2018.1500453.
- Feddersen E, Lockwood DH. An inpatient diabetes educator’s impact on length of hospital stay. Diabetes Educ. 1994 Mar-Apr;20(2):125–128. PubMed PMID: 7851225.
- Healy SJ, Black D, Harris C, et al. Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care. 2013 Oct;36(10):2960–2967. PubMed PMID: 23835695; PubMed Central PMCID: PMCPMC3781555.