ABSTRACT
Inadvertent removal of percutaneous endoscopic gastrostomy (PEG) tube shortly after placement creates the potential for gastric perforation and requires immediate attention. This problem has been addressed in the past with either observation or surgery. We describe our experience with the alternative approach of semi-urgent ‘re-PEGing’. Our results in seven patients were favorable.
1. Definitions used in this paper
Gastro-cutaneous Tract: The channel established between the gastric lumen and the skin created by the PEG placement. The tube traverses the abdominal wall, placing the visceral and parietal peritoneum in apposition.
Direct tube replacement: placement of balloon-based Foley-like catheter after PEG removal, directly into the gastro-cutaneous tract, usually at the bedside, without endoscopy or imaging guidance.
Early removal of PEG tube: removal within 4 weeks of PEG placement, a period during which the gastro-cutaneous tract may not be mature, and direct tube replacement may be unsafe.
Late removal of PEG tube: removal more than 4 weeks after PEG placement, by which time the gastro-cutaneous tract is likely to be mature, and allow safe direct tube replacement.
Violation of the peritoneal cavity: indicated by one or more of the following:
Clinical signs of peritonitis
Intraperitoneal air.
A catheter from a direct tube replacement attempt present outside the gastric lumen, on imaging studies.
2. Introduction
Percutaneous endoscopic gastrostomy (PEG) is the modality of choice for long-term enteral feeding access, with over 200,000 PEG procedures performed annually in the USA [Citation1]. While generally safe, complications do occur. Inadvertent PEG tube removal is a common problem and happens in as many as 12.8% of patients [Citation2]. Management of this problem depends on the time elapsed since placement. If it has been long enough to allow maturation of the gastro-cutaneous tract, direct tube replacement can usually be done easily and safely. If the withdrawal of the tube occurs early, the gastro-cutaneous tract is not well established, and the stomach is not well attached to the abdominal wall. Separation of the stomach from the abdominal wall may occur upon removal of the PEG tube, or as a result of attempted direct tube replacement. This separation creates the anatomic equivalent of acute gastric perforation.
The literature reports a range of 1–4 weeks for the gastro-cutaneous tract to mature [Citation3] – thus allowing safe direct tube replacement. We chose the more conservative time frame of 4 weeks, and used this to distinguish between early and late removal of PEG tube.
The standard approach to early removal of PEG tube, with the associated potential of gastric perforation, has been either observation with nasogastric tube decompression, or surgical exploration with closure of the gastric wall defect [Citation3,Citation4]. In 1990, Galat [Citation5] reported good results treating Early removal of PEG tube with immediate placement of a new PEG, ‘re-PEGing’. We report our experience with this approach.
2.1. Methods
The records of 352 patients who underwent PEG placement in a 34-month period (June 2015 to March 2018) at Rochester General Hospital, a 528-bed tertiary care hospital, were reviewed. Seven patients, 1.9% of this population, with semi-urgent PEG replacement after early removal of PEG tube, were identified. All procedures were performed by one of the authors (AK).
The PEG kit used was the 20 F Entake PEG Safety System (ConMed Corporation; Utica, New York) ().
Figure 1. Entake PEG safety system (Commed, Utica, NY). The tube dome is collapsible upon pulling allowing passage of the tube through the gastrocutaneous tract.
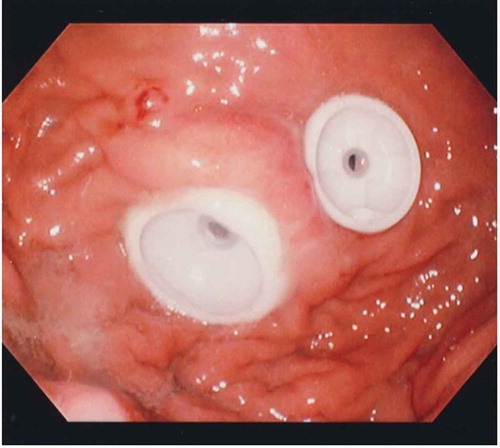
The endoscopic technique was modified to minimize gas insufflation and scope trauma. The duodenum was not intubated, and no retroflexion of the gastroscope was done. The gastric wall defect was visualized, and typically appeared partially sealed (). The percutaneous needle was placed at the previous entry site at the skin level, aiming to enter the stomach as close to the gastric wall defect as possible. If this distance was more than an inch, raising concern about completeness of sealing of the gastric perforation, an additional PEG tube was placed with the intention of improving the patching effect between the stomach and the abdominal wall (‘double-PEG’) (). Early tube feeding was started in most patients, with frequent residual checks.
2.2. Clinical data
summarizes individual patient characteristics. All re-PEGing was done within 24 hours of early removal of PEG tube. Our typical patients were elderly with multiple comorbidities. Five of the patients had violation of the peritoneal cavity; three of these five were asymptomatic; the other two were acutely ill with clinical picture of sepsis or peritonitis. In two of the asymptomatic patients the violation of the peritoneal cavity was iatrogenic, created by a failed attempt at direct tube replacement at 10 and 14 days. Two additional asymptomatic patients had no evidence of violation of the peritoneal cavity. In two patients, we placed a double PEG. All patients recovered uneventfully; no peritoneal abscess developed in any of them.
Table 1. Clinical data (*indicates time from attempted direct tube replacement [DTR]).
3. Discussion
The Early removal of PEG tube rate in our PEG patients is 1.9%, similar to that of Galat [Citation5]. This is frequent enough that it is likely that any endoscopist performing PEGs will face this problem at some point.
The re-PEGing approach to this problem is appealing because of its minimally invasive nature and the immediate reestablishment of enteral feeding access. Most significantly, the newly placed PEG tube, by patching the site of the perforation to the abdominal wall, prevents leak of gastric contents, and accomplishes early ‘damage control’.
The standard approach to early removal of PEG tube has been either nasogastric decompression with observation, or surgery, in patients with peritoneal signs. Galat’s [Citation5] innovative approach, re-PEGing, is the endoscopic equivalent of surgical repair of the gastric perforation, using a less invasive technique, sealing the perforation by pulling the stomach to the anterior abdominal wall. Additional case studies [Citation6,Citation7] also reported successful outcomes. However, the approach did not gain acceptance.
The maturation of the gastro-cutaneous tract created by the PEG placement is a gradual process, and the time at which direct tube replacement is safe is not clearly established. The recommendations in the literature range from one to 4 weeks [Citation3]. As we implemented the re-PEGing concept, it became clear to us that it is a safer alternative to direct tube replacement in patients with Early removal of PEG tube. Accordingly, there is a good argument against early attempts of direct tube replacement, and we chose to accept the longer time interval of 4 weeks from PEG placement as a safe one. Thus, we define early removal of PEG tube as occurring within 4 weeks. Unlike Galat [Citation5], who chose a time interval in 1 week.
In our study, the two Direct tube replacements leading to Violation of the peritoneal cavity and then re-PEGing, occurred at 10 and 14 days from original placement. While the numbers are small, it supports the recommendation of not attempting Direct tube replacement before 4 weeks thus avoiding this major complication.
Galat’s [Citation5] inclusion criteria for Re-PEGing allowed only patients without peritoneal signs. As we adopted the concept, we took it a step further and used the technique in all of our patients, with a wide variety of clinical and radiological findings, with positive outcomes.
In contrast to Galat’s conservative recommendation to wait 48 hours before starting feeding, we allowed early use of the PEG tube, with frequent checks of residual volume to ensure adequate gastric emptying.
None of our patients with violation of the peritoneal cavity developed abdominal abscess. Had that occurred, it could have been diagnosed by CT scan, and drained percutaneously by interventional radiology, still avoiding surgery.
Additional arguments in favor of re-PEGing rather than surgery, are the following:
Endoscopy under sedation is safer and less invasive than surgery, open or laparoscopic, that requires general anesthesia. Also, in most institutions, scheduling an endoscopic procedure is quicker and easier than scheduling surgery.
The perforated gastric site was previously brought to the abdominal wall during the original PEG procedure, so it can be done again, and endoscopic patching and sealing of the perforation is usually anatomically feasible.
With the universal use of CO2 for endoscopic insufflation, the gas that may leak into the peritoneal cavity is quickly absorbed. This weakens the argument against endoscopy in the face of perforation.
Immediate access for feeding and medication is obtained.
There is potential for significant cost saving by avoiding operating room expenses and shortening hospital stay.
So, why has not this appealing technique been widely accepted? The answer probably relates to the gastroenterologists’ ‘gestalt’ that perforation is a surgical problem, and the belief that gastroscopy is contra-indicated in patients with a perforated stomach. Informal polling of colleagues in gastroenterology and surgery revealed that a surgical approach would be their standard choice in the case of early removal of PEG tube, especially in the presence of peritoneal signs and free air.
We recommend the following approach to patients with Early removal of PEG tube:
Evaluate clinically; consider CT scan.
Avoid direct tube replacement.
If violation of the peritoneal cavity has occurred, use a short course of antibiotics.
Perform urgent endoscopic PEG replacement in most, if not all, of these patients, including those with violation of the peritoneal cavity.
Consider second PEG if needed to improve the patching and the sealing of the gastric perforation.
Start early feeding.
In summary, re-PEGing for Early removal of PEG tube is simple, safe, effective, and potentially cost saving, compared to observation or surgery. It controls the gastric leak and provides immediate feeding access. The ease of this approach is an additional argument against direct tube replacement attempts earlier than 4 weeks.
Author contributions
Soliman: Data acquisition, chart review, manuscript preparation, technical support
Kurchin: Manuscript preparation, supervisory role, study concept and design
Devgun: Data acquisition, supervisory role
Disclosure statement
No potential conflict of interest was reported by the author.
References
- Mendiratta P, Tilford JM, Prodhan P, et al. Trends in percutaneous endoscopic gastrostomy placement in the elderly from 1993 to 2003. Am J Alzheimer’s Dis Dementias. 2012;27(8):609–613.
- Rosenberger LH, Guidry CA, Davis JP, et al. Reducing accidental dislodgement of the percutaneous endoscopic gastrostomy: A prospective trial of the “SafetyBreak” device. Surg Innov. 2016;23(1):62–69.
- Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, et al. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014;20(24):7739–7751.
- Schrag SP, Sharma R, Jaik NP, et al. Complications related to percutaneous endoscopic gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis. 2007;16(4):407–418.
- Galat SA, Gerig KD, Porter JA, et al. Management of premature removal of the percutaneous gastrostomy. Am Surg. 1990;56(11):733–736.
- Gaines DI, Delegge MH. Semiurgent endoscopic PEG tube replacement as a treatment for early initial PEG tube dislodgement in the immune-compromised patient. Dig Dis Sci. 2005;50(12):2248–2250.
- Mincheff TV. Early dislodgement of percutaneous and endoscopic gastrostomy tube. J S C Med Assoc. 2007;103(1):13–15.