ABSTRACT
Rhabdomyosarcoma (RMS) is a malignant soft tissue tumor of the pediatric population which is  rarely seen in adults. Metastatic rhabdomyosarcoma is even rarer. We present an unusual case of a 49 year old female presenting with palpitations and uterine bleeding. An Echo-cardiogram revealed a large oval mass on the posterior mitral leaflet and a Computerized Tomography (CT) scan of the abdomen revealed a uterine growth. Surgical excision of the cardiac mass was done and histological analysis of cardiac lesion confirmed it to be rhabdomyosarcoma with a primary source in the uterus. The patient became asymptomatic from a cardiac standpoint after excision of the mass and was scheduled for chemo/radiation therapy for the primary uterine malignancy. Metastatic cardiac rhabdomyosarcoma can be confused with a myxoma or any other primary or secondary cardiac tumors resulting in delayed diagnosis. However, its aggressive nature makes it a life-threatening tumor that requires an early diagnosis to prevent fatal consequences.
1. Summary
Rhabdomyosarcoma(RMS) is a malignant soft tissue tumor of the pediatric population which is rarely seen in adults. Metastatic rhabdomyosarcoma is even rarer. We present an unusual case of a 49 year old female presenting with palpitations and uterine bleeding. An Echocardiogram revealed a large oval mass on the posterior mitral leaflet and a Computerized Tomography(CT) scan of the abdomen revealed a uterine growth. Surgical excision of the cardiac mass was done and histological analysis of cardiac lesion confirmed it to be rhabdomyosarcoma with a primary source in the uterus. The patient became asymptomatic from a cardiac standpoint after excision of the mass and was scheduled for chemo/radiation therapy for the primary uterine malignancy. Metastatic cardiac rhabdomyosarcoma can be confused with a myxoma or any other primary or secondary cardiac tumors resulting in delayed diagnosis. However, its aggressive nature makes it a life-threatening tumor that requires an early diagnosis to prevent fatal consequences.
2. Background
Rhabdomyosarcoma (RMS) is a very rare and heterogeneous group of malignancies, found most commonly in the childhood. Its appearance among adults is rare, accounting for 2% to 5% of all the adult soft tissue sarcomas. Diagnosing a case of metastatic cardiac rhabdomyosarcoma is challenging for a physician because of its vague clinical features. The presentation of a cardiac mass highly depends on the location of tumor rather than the histological subtype. Therefore, classifying a cardiac tumor into a particular histological type can be very difficult and requires extensive workup. According to multiple sources, it has been established that median survival time is typically 6 to 12 months. Here, we discuss a case of a cardiac neoplasm that presented with symptoms mimicking any other cardiac mass and a provisional diagnosis of a cardiac myxoma was made. Excision of the mass, histological analysis and its comparison with the biopsy of uterine mass confirmed it to be a rhabdomyosarcoma and helped us in excluding the possibility of all other primary and secondary cardiac tumors. The purpose of writing up this case is to urge physicians to consider metastatic cardiac rhabdomyosarcoma in one of the ‘exclusion diagnosis’ of a cardiac mass so that it can be diagnosed and managed promptly since misdiagnosis or delayed diagnosis only worsens its already poor prognosis.
3. Case presentation
A 47-year-old female presented to the emergency department (ED) with palpitations for the past 3 days. She denied chest pain, nausea, diaphoresis or syncope associated with palpitations. She reported a history of microcytic anemia, menorrhagia and progressive weakness for the past 1 month. The anemia improved minimally with oral iron supplementation. Personal history included insomnia, smoking and alcohol intake. Family history was positive for hemochromatosis in maternal grandmother.
On physical examination, the patient was in no acute distress. Her vital signs were a blood pressure of 118/57 mm Hg, pulse rate of 110 bpm, temperature 99 F, respiratory rate 20 bpm and oxygen saturation of 98% on room air. Cardiovascular and respiratory examination revealed raced but regular first and second heart sounds with no added sound or murmur and bilaterally clear lungs with equal air entry. Pertinent laboratory findings revealed microcytic anemia with Hb 8 g/dL with MCV 74.4.
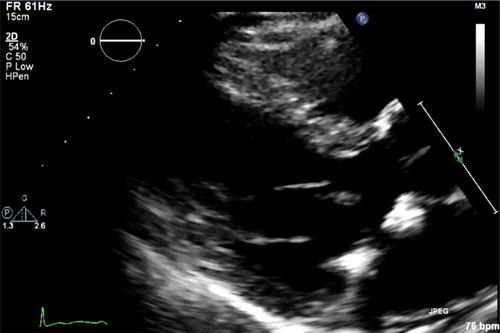
EKG revealed sinus tachycardia with heart rate of 110 bpm but was unremarkable for ischemia or other rhythm abnormalities. Trans-thoracic echocardiogram (TTE) was done to rule out any structural heart disease or tachycardia induced cardiomyopathy in the setting of Hb of 8 g/dL. TTE revealed normal right and left ventricular function, an ejection fraction of 55% and a mass on the left atrial side of the posterior mitral leaflet with mitral prolapse and mild mitral regurgitation. Trans-esophageal Echocardiography (TEE) was done to further delineate the mass which revealed that left atrium was normal in size. There was a large immobile, heterogenous mass on the posterior leaflet of mitral valve. The base was broad measuring 1.5 cm with no obvious stalk. The largest dimensions on imaging were 2.9 cm x 2.8 cm. There was no calcification of the mass ().
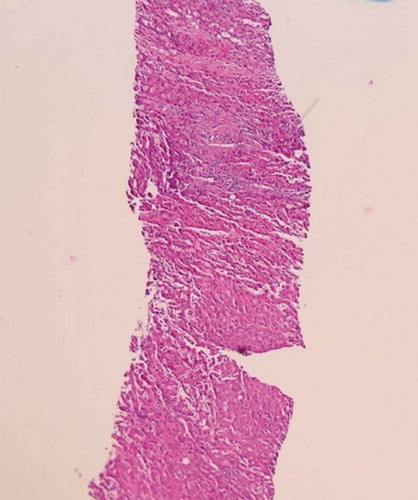
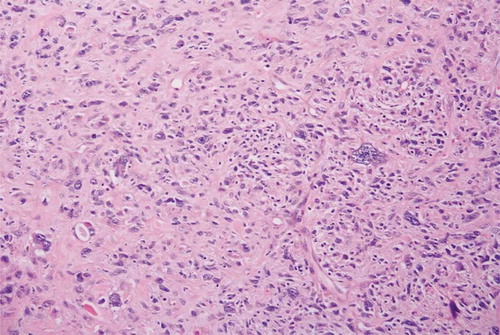
Cardiology Department was consulted. Initially, a presumptive diagnosis of atrial myxoma was made. Computed Tomography (CT) scan of the abdomen & pelvis revealed a 3 cm mass in the uterus. Biopsy of the uterine mass revealed it to be a rhabdomyosarcoma resembling an undifferentiated pleomorphic sarcoma (). Pleomorphic cells with abundant mitosis and areas of necrosis were seen. At this point, atrial mass was presumed to be a myxoma and the cause of palpitations. As per Cardiology recommendation, It was excised and the mitral valve was repaired. Histological analysis of the atrial mass was consistent with the diagnosis of rhabdomyosarcoma (). Histology of both atrial and uterine mass revealed a cellular malignant neoplasm composed of round to elongated markedly atypical cells enlarged with hyperchromatic nuclei and some cells with eosinophilic cytoplasm. Desmin positivity was observed on immunohistochemistry testing of uterine as well as the atrial mass. These findings, along with the patient’s clinical history, were consistent with the diagnosis of the rhabdomyosarcoma. After the surgical excision of the cardiac mass, the patient was scheduled for chemo/radiation therapy for uterine pathology. The patient stayed in the hospital for five days. She was discharged home and regular follow up was advised in the clinic with Gynecologic-Oncology, Cardiac Surgery, and Primary care Physician.
Figure 1. Trans-esophageal echocardiogram revealing a mass on the posterior leaflet of mitral valve.
3.1. Investigations if relevant
4. OUTCOME AND FOLLOW-UP
Her palpitations resolved following excision of left atrial mass via right Thoracotomy. To exclude metastasis in other organs, screening mammography and MRI Brain with contrast were performed which were negative for any mass. She was advised to follow up regularly with her primary care physician, cardiologist as well as gynecologic/oncology for further management of uterine rhabdomyosarcoma as an outpatient. PET scan of Abd/Pelvis were advised at scheduled intervals to look for any recurrence of tumor.
4.1. Discussion include a very brief review of similar published cases
Sarcomas are very uncommon malignant soft tissue tumors, consisting of fewer than 1% of adult malignancies and 12% of paediatric malignancies [Citation1]. It has been estimated that sarcomas constitute about 1% of all cancers, and approximately 12,000 people in the USA are diagnosed with sarcoma every year [Citation2]. Sarcomas have a wide variety of histopathological types that may be primary or metastatic. One type of sarcoma called Rhabdomyosarcoma is a malignant tumor of mesenchymal origin which is very aggressive in nature and has high metastatic potential. It is made up of striated muscle cells, which have failed to fully differentiate. It is most commonly seen in the paediatric population and is described as ‘small, blue, round cell tumors in the childhood’ due to its appearance in H&E staining [Citation3]. It has a fairly low incidence in adults, therefore, the study of this disease in the adult is quite challenging. The site of origin of RMS can be variable but is predominantly found in the head, neck, orbit, genitourinary tract, genitals, and extremities [Citation4]. The presenting symptoms also strongly correlate with the primary site, as there are no defined symptoms of the disorder itself. There are no specific risk factors linked with RMS however, associations with certain congenital malformations have been made [Citation5]. There are a variety of classification systems or defined histological types of RMS, including Embryonal, Alveolar, Botryoid and Pleomorphic rhabdomyosarcoma. Embryonal rhabdomyosarcoma is the most common type of rhabdomyosarcoma found in the children whereas pleomorphic rhabdomyosarcoma is usually found in adults [Citation6]. Our case also exhibited histological evidence and immune profile of pleomorphic rhabdomyosarcoma.
Primary cardiac tumors are remarkably rare and RMS makes up 20% of the primary cardiac tumors [Citation7].
The tumor frequently arises from the ventricular walls and may hinder valvular motion. However, in adults, it may stem from the atria and mimic numerous cardiac and non-cardiac ailments [Citation8]. However, RMS as metastatic disease to the heart is a unique existence. In our patient, cardiac mass was originally found in the left atrium attached to the mitral valve. Because of its location, it was misinterpreted to be a cardiac myxoma. However, further investigations revealed it to be a metastatic RMS primarily originating from the uterus.
Presenting symptoms in adults can be quite variable and there are no known definite symptoms. The location of the tumor has a dominant effect on the presentation. It can present as palpitations, acute heart failure, regurgitation murmurs, heart block, and pericardial effusion with or without tamponade. It has been proposed that tumor fragments may get dislodged and present with symptoms mimicking those of pulmonary embolus. The tumor can invade the adjacent lung resulting in pulmonary symptoms and simulate bronchogenic carcinoma. Other than the cardiac symptoms, some constitutional and systemic symptoms are also seen. However, in some cases, symptoms never appear and they are discovered incidentally on a regular check-up. Sarcomas are extremely fast-growing tumors with high recurrence rate.
Our patient presented with palpitations and EKG revealed sinus tachycardia. This prompted the physicians to perform TTE which discovered mass as an incidental finding and TEE was performed to further evaluate the mass. TTE is by far the most extensively used tool for initial evaluation but it can only identify the size, shape, attachment, and mobility of a mass [Citation9]. In contrast, a Cardiac computed tomography (CT) scan is an increasingly utilized modality in identifying malignancy and discovering the source of origin, which aids in confirming whether the cardiac mass is primary or metastatic. CT scan is also used as an imaging modality for evaluating other adjacent organs for metastasis [Citation10].
Fluorodeoxyglucose-positron emission tomography (FDG-PET-CT) is very useful in diagnosis as it differentiates between a benign and a malignant lesion with a 100% sensitivity and about 86% specificity [Citation11]. Immunohistochemistry is very helpful in the identification of a particular sarcoma and is the concluding diagnostic step in classifying the type of tumor. For the identification of RMS, desmin positivity is particularly valuable [Citation1]. In this case, the final diagnosis of Cardiac RMS with primary origin from the uterus was made after immunohistochemistry analysis showed desmin positivity in both the uterine and cardiac mass. Over 99% of RMS stain positive for polyclonal desmin [Citation4].
RMS is rare but a lethal disease in adults and the literature regarding its management is very limited. Distant disease is proportional to poor prognosis. The prognosis of cardiac sarcoma remains to be very poor. Survival rates for adolescents and adults with RMS are significantly poor compared to younger children. The standard care includes multimodality treatment with or without surgical resection. Chemoradiation combined with radical surgery is a promising protocol in patients with resectable disease. Complete resection improves survival output [].
However, there are many unanswered questions regarding the treatment options in the adult population as literature is limited in this regard.
Our patient was counselled regarding the overall poor prognosis of this disease. Cardiac metastatic lesions primarily originating from the uterus were found on imaging, and further metastatic workup was negative. Cardiac mass was symptomatic, causing distress to the patient. As a result, a decision was made to remove the cardiac mass. Palpitations resolved after excision and the patient was scheduled for chemo/radiation therapy for the primary lesion in the uterus.
In our case, cardiac RMS presented as a metastatic lesion from uterine RMS. It is a highly rare presentation and in our literature review, it is the second reported case of uterine RMS metastasizing to heart and the patient became asymptomatic from a cardiac standpoint after excision of the mass. From one case previously reported, the patient died within a year.
An approach tailored specifically to every individual case is extremely important to explore early diagnostic methods, treatment therapies, and better survival rates.
4.2. Learning points/take home messages 3-5 bullet points
After our comprehensive literature review, we have established the fact that it is a very rare presentation with very little published data, so more research is required to further investigate it.
The possibility of a cardiac RMS should be considered when someone presents with symptoms of palpitations and arrhythmias and a cardiac mass is detected on echocardiogram.
Radiological investigations, histological analysis, and immunohistochemistry can help in pinpointing the primary as well as the metastatic lesions.
A mass in the uterus can metastasize to the heart so vigilant follow-up and prompt screening methods should be encouraged in order to prevent fatal consequences.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Ryan CW, Meyer J, Maki R, et al. Clinical presentation, histopathology, diagnostic evaluation, and staging of soft tissue sarcoma. Waltham, MA: UpToDate; 2012. ( Up To Date).
- Different A View of Sarcoma Statistics [Internet]. Liddy Shriver Sarcoma Initiative. 2019 [cited 2019 Nov 4]. Available from: http://sarcomahelp.org/articles/sarcoma-statistics.html
- Arndt C, Crist W. Common Musculoskeletal Tumors of Childhood and Adolescence. N Engl J Med. 1999;341(5):342–352.
- Okcu F, Hicks J, Horowitz M Rhabdomyosarcoma in childhood and adolescence: epidemiology, pathology, and molecular pathogenesis.
- Pappo A, Shapiro D, Crist W, et al. Biology and therapy of pediatric rhabdomyosarcoma. J Clin Oncol. 1995;13(8):2123–2139.
- Newton W, Gehan E, Webber B. et al. Classification of rhabdomyosarcomas and related sarcomas. Pathologic aspects and proposal for a new classification-an intergroup rhabdomyosarcoma study. Cancer. 1995;76(6):1073–1085..
- SILVERMAN N. Surgical Progress. Ann Surg. 1980;191(2):127–138.
- Villasenor HR, Fuentes F, Walker WE. Left atrial rhabdomyosarcoma mimicking mitral valve stenosis. Tex Heart Inst J. 1985 Mar;12(1):107.
- Foster E Echocardiographic evaluation of the atria and appendages. UpToDate, accessed online at www. uptodate. com. 2014.
- Simpson L, Kumar SK, Okuno SH, et al. Malignant primary cardiac tumors: review of a single institution experience. Cancer: Interdiscip Int J Am Cancer Soc. 2008 Jun 1;112(11):2440–2446.
- Guazzaroni M, Lacchè A, Nardone V, et al. Evaluation of a cardiac sarcoma with CT multislice contrast-enhanced and 18FDG-PET/TC. Radiol Case Rep. 2019 Mar 1;14(3):368–371.