ABSTRACT
Introduction
Gilteritinib is a FLT3 kinase inhibitor approved for FLT3-mutated acute myeloid leukemia (AML). We present a case of febrile neutropenia and neutrophilic dermatosis consistent with Sweet’s syndrome (SS).
Case history
A 55-year-old woman presented with fever and skin lesions after 4 weeks of initiation of Gilteritinib for AML. She was febrile, pancytopenic and neutropenic with absolute neutrophil count (ANC) of 0.1x10E3/UI. Examination revealed reddish and violaceous rashes on her extremities. Pathology showed superficial dermal edema, widespread epidermal spongiosis and multiple neutrophils in the dermal infiltrate. Rash improved with prednisone 60 mg daily and started to flare with taper. She was still on Gilteritinib all this time. Gilteritinib was finally stopped due to non-response and possible contribution in flaring her SS. Shortly after, the patient succumbed to progressive disease and complications of sepsis.
Discussion
There have been reports of SS in neutropenic patients although SS is typically a neutrophilic dermatosis. The pathogenesis of SS in neutropenia remains uncertain. Our study represents an additional medication-associated cutaneous complication of AML therapy. Clinicians need to be aware of potential neutrophilic dermatoses with FLT-3 inhibition, even with peripheral neutropenia.
1. Introduction
Sweet’s syndrome (SS), also known as acute febrile neutrophilic dermatosis, is characterized by fever, corticosteroid-responsive red painful skin lesions (papules, nodules, plaques) and histopathogical evidence of diffuse neutrophilic infiltration in the upper dermis sometimes with fragmented neutrophil nuclei (leukocytoclasia), dilated small blood vessels and swollen endothelial cells, without findings of ‘primary’ leukocytoclastic vasculitis [Citation1,Citation2]. Dr.Douglas Sweet originally reported SS in 1964, when he described 8 women aged 35 to 55 years with findings as mentioned above [Citation3]. Although SS is related to hematologic malignancy, it can be associated with infections, pregnancy and medications, most commonly reported being granulocyte-colony stimulating factor[Citation1]. In patients with hematologic disorders, SS may present in 3 settings: a paraneoplastic syndrome, drug-induced dermatosis or concurrently with leukemia cutis[Citation2]. The cutaneous manifestation may occur before, during or after the diagnosis of malignancy, and therefore could herald a new diagnosis or recurrence of underlying malignancy[Citation4].
The most commonly mutated gene in acute myeloblastic leukemia (AML) is the receptor tyrosine kinase FLT3, mutated in about 30% of patients. Gilteritinib is a highly potent and selective FLT3 kinase inhibitor approved as monotherapy for the treatment of relapsed and/or refractory FLT3-mutated AML[Citation5]. We present a 55-year-old woman who presented with febrile neutropenia and skin lesions consistent with neutrophilic dermatosis 4 weeks after being started on Gilteritinib for AML.
2. Case history
A 55-year-old woman presented to the hospital with fever and skin lesions of 1-day duration. Past medical history was notable for invasive ductal carcinoma of the right breast who developed Adriamycin-related myelodysblastic syndrome/myeloproliferative neoplasm and failed treatment with Azacitidine/Venetoclax with subsequent progression to AML with 60% blasts and FLT3 ITD mutation. She also developed transfusion-dependent pancytopenia. She had multiple recent hospital admissions for neutropenic fever. She was not considered a candidate for induction chemotherapy in the setting of repeated infections and was palliatively started on Gilteritinib 4 weeks prior to the current presentation.
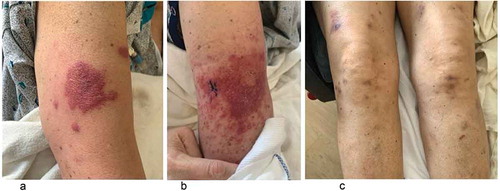
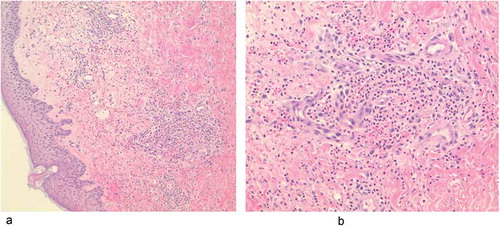
She noted initial painful lesion that appeared like an insect bite on her left arm and rapidly progressed to involve the right arm and bilateral legs. At presentation, she was febrile to 102 F but hemodynamically stable. Routine laboratory tests showed pancytopenia with white blood cells (WBC) count of 0.5 (ref- 4.8–10.8) 10E3/uL, 31% peripheral blasts, absolute neutrophil count (ANC) of 0.1 (ref- 2.0–8.0) 10E3/UI, platelet count of 14 (ref- 130 – 400) 10E3/uL and hemoglobin of 7.7 (12.0–16.0) g/dl. ANC range in the past month was 0–0.2 10E3/UI. She lacked infectious symptoms or signs and had no laboratory or radiographic evidence of infection. She was started on broad-spectrum antibiotics pending blood culture results. Examination revealed reddish and violaceous macular, papular and nodular rashes on her left arm and forearm, right forearm and on bilateral legs (). No treatment was initiated for the rash until final tissue diagnosis, which occurred 3 days later. Pathology of the left upper arm lesion showed ‘superficial dermal edema with a perivascular and interstitial cellular infiltrate, widespread spongiosis in the overlying epidermis along with multiple neutrophils and some leukocytoclasia noted in the dermal infiltrate’ (). Diagnosis of SS was made based on fever, suggestive skin lesions and pathological finding of neutrophilic dermatosis in the setting of an underlying hematologic malignancy.
The patient started to improve with prednisone 60 mg daily and was discharged on outpatient taper regimen. Skin lesions started to flare when prednisone dose was weaned to 10 mg daily, which was again increased (). She was still on Gilteritinib all this time. Blood examination showed persistent pancytopenia and neutropenia with ANC of 0.7 10E3/UI. Bone marrow study showed persistent blasts at 30-40% (a slight improvement from 60% but still signifying persistence of the neoplasm at a level consistent with AML). Gilteritinib was stopped due to non-response, worsening performance status and possible contribution in flaring her SS. At subsequent follow-up, her WBC was up to 13,000 with 75% blasts and she was started on hydroxyurea. Shortly after, the patient succumbed to progressive disease and complications of sepsis.
3. Discussion
The most consistent lab finding in SS is peripheral leukocytosis with neutrophilia[Citation6]. However, not all patients with biopsy-proven Sweet syndrome, especially those that are malignancy-associated, have an elevated white count, and may even have leukopenia or neutropenia [Citation7,Citation8]. Important differential diagnoses of neutrophilic dermatosis in a febrile and neutropenic patient may include infections (cellulitis, erysipelas), drug eruptions, leukemia cutis, erythema multiforme, thrombocytopenic purpura and leukocytoclastic vasculitis, among others [Citation1,Citation8].
Malignancy or drug-associated SS usually clears with successful management of cancer or cessation of the causative agent, respectively, and administration of corticosteroids [Citation1]. Recurrence of SS can occur, with more frequent recurrences being common in cancer patients [Citation2,Citation9]. Our patient had AML with FLT3 mutation and febrile neutropenia, was on FLT3 inhibitor Gilterinib and developed SS 4 weeks post-initiation. Our diagnosis of SS was made based on acute painful erythematous plaques and nodules with neutrophilic infiltration in the dermis with generalized malaise and fever and an underlying AML along with a good response to corticosteroids, which is in line with Su and Liu’s revised criteria for the diagnosis of SS [Citation10,Citation11].
There have been reports of SS in neutropenic patients although SS is typically a neutrophilic dermatosis. Probert et al. reported 3 cases of neutrophilic dermatoses in neutropenic patients after receiving chemotherapy. Studies also indicate that patients with hematological malignancy usually do not typically have neutrophilia at SS onset [Citation7,Citation11]. Fathi et al. reported 3 cases of neutrophilic dermatoses after treatment with FLT3 inhibitor for AML with the onset of lesion 2–8 weeks after therapy initiation[Citation12]. Varadarajan et al. described 2 cases of neutrophilic dermatoses with Gilteritinib after 2 months of therapy initiation[Citation13]. Oczelik et al. reported SS in a 24 year female with AML and severe neutropenia treated with several antibiotics and chemotherapeutic regimen[Citation14]. The pathogenesis of SS in neutropenia, however, remains uncertain. There has been a suggestion that neutrophils may be sequestrated into the skin as the peripheral neutrophil count is decreasing or that leukemic cells can differentiate into clonal neutrophils which then build up in the dermis regardless of peripheral neutrophil counts [Citation8,Citation11].
Our study represents an additional medication-associated cutaneous complication of AML therapy. Clinicians need to be aware of potential neutrophilic dermatoses with FLT-3 inhibition, even in patients with peripheral leukopenia and neutropenia. In a granulocytopenic patient, attention is primarily paid to infection and it is challenging to initiate steroids which may exacerbate infections. Early skin biopsy can be helpful in a febrile neutropenic patient with skin lesions, to prevent unnecessary antibiotic use and delay diagnosis.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Cohen PR. Sweet’s syndrome – a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;2:34.
- Cohen PR, Kurzrock R. Sweet’s syndrome revisited: a review of disease concepts. Int J Dermatol. 2003;42(10):761–778.
- Sweet RB. An acute febrile neutrophtlic dermatosts. Br J Dermatol. 1964;76(8–9):349–356.
- Kazmi SM, Pemmaraju N, Patel KP, et al. Characteristics of Sweet’s syndrome in patients with acute myeloid leukemia. Clin Lymphoma Myeloma Leuk. 2015;15(6):358–363.
- McMahon CM, Perl AE. Gilteritinib for the treatment of relapsed and/or refractory FLT3-mutated acute myeloid leukemia. Expert Rev Clin Pharmacol. 2019;12(9):841–849.
- Cohen PR, Kurzrock R. Sweet’s syndrome: a neutrophilic dermatosis classically associated with acute onset and fever. Clin Dermatol. 2000;18(3):265–282.
- Cohen PR, Talpaz M, Kurzrock R. Malignancy-associated Sweet’s syndrome: review of the world literature. J Clin Oncol Off J Am Soc Clin Oncol. 1988;6(12):1887–1897.
- Aractingi S, Mallet V, Pinquier L, et al. Neutrophilic dermatoses during granulocytopenia. Arch Dermatol. 1995;131(10):1141–1145.
- Cohen PR, Almeida L, Kurzrock R. Acute febrile neutrophilic dermatosis. Am Fam Physician. 1989;39(3):199–204.
- Su WP, Liu HN. Diagnostic criteria for Sweet’s syndrome. Cutis. 1986;37(3):167–174.
- Sweet’s syndrome without granulocytosis - Probert, MD - 1998 - international journal of dermatology - Wiley online library. [cited 2019 Nov 17]. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1365-4362.1998.00270.x
- Fathi AT, Le L, Hasserjian RP, et al. FLT3 inhibitor-induced neutrophilic dermatosis. Blood. 2013;122(2):239–242.
- Varadarajan N, Boni A, Elder DE, et al. FLT3 inhibitor-associated neutrophilic dermatoses. JAMA Dermatol. 2016;152(4):480–482.
- Ozcelik T, Ozkocaman V, Ali R, et al. Sweet’s syndrome: dilemma in febrile neutropenic patient with acute myeloid leukemia. Leuk Res. 2006;30(11):1466–1468.