ABSTRACT
Patients with atrial fibrillation are at an increased risk for stroke, and many benefits from anticoagulation. Despite the emergence of direct oral anticoagulants, many patients continue to rely on warfarin for their anticoagulation due to logistical, pharmacokinetic, clinical, or patient preference issues. Previous work has suggested that outcomes of warfarin therapy are related to patient education/knowledge. We assessed knowledge of indications, benefits, and complications of warfarin therapy in 99 randomly selected patients enrolled in the Warfarin Anticoagulation Clinic at the Mayo Clinic in Florida who were taking warfarin for non-valvular atrial fibrillation. Patients were labeled as ‘knowledgeable’ or ‘not knowledgeable’ regarding warfarin therapy according to the results of a cross-sectional questionnaire. The majority of patients in both the knowledgeable and not knowledgeable groups displayed understanding that they were taking warfarin for atrial fibrillation (valvular vs non-valvular atrial fibrillation was not an included answer choice). However, there was a clear lack of knowledge amongst patients with atrial fibrillation in both groups about their stroke risk while on and off warfarin, and their risk of major bleeding or adverse events related to their warfarin therapy. There was only a significant difference between the two groups regarding their knowledge of what increases or decreases the risk of bleeding while on warfarin. There was no major difference between the groups with regards to demographic and medical characteristics, except that ‘not knowledgeable’ patients tended to have more peripheral vascular disease, ulcer disease, and moderate-severe renal disease compared to ‘knowledgeable’ patients.
1. Introduction
Patients with atrial fibrillation are at increased risk for stroke, and many benefits from anticoagulation with warfarin. Warfarin has been shown to decrease the risk of stroke by two-thirds in patients with atrial fibrillation [Citation1]. Multiple large-scale studies, such as the Stroke Prevention in Atrial Fibrillation Study (SPAF) [Citation2], the Boston Area Anticoagulation Trial for Atrial Fibrillation (BAATAF) [Citation3], and Stroke Prevention in Nonrheumatic Atrial Fibrillation (SPINAF) trial [Citation4], have shown the benefit in stroke reduction amongst anticoagulated patients with atrial fibrillation. In non-valvular atrial fibrillation, the target goal for INR is 2.0–3.0 [Citation5]. INR levels below 2.0 do not adequately decrease a patient’s stroke risk, while INR values greater than 3.0, are associated with an increased risk of bleeding. Therefore, it is important to keep patients within the therapeutic range for as much time as possible in order to maximize the risk–benefit ratio. Many factors play a role in a patient achieving maximum time in the therapeutic range (TTR) including various pharmacologic interactions, patient adherence, adequate laboratory monitoring, and timely dose-adjustments. In a meta-analysis performed by Oake et al [Citation6], increased TTR conferred the lowest absolute risk of hemorrhage and thromboemboli in patients treated with warfarin for non-valvular atrial fibrillation. Time spent above the therapeutic range with an INR between 3 and 5 was associated with an increased risk of hemorrhage (relative risk = 2.7; 95% confidence interval 1.8–3.9; p < 0.01). An INR greater than 5 was associated with even greater risk (relative risk = 21.8; 95% confidence interval 12.1–39.4; p < 0.01). Time spent below the TTR led to an increased risk of thromboemboli with a relative risk of 2.4 (1.9–3.1; p < 0.01) [Citation6].
Several studies have examined elements of patient understanding of their anticoagulation therapy, many of which highlighted deficiencies. McCabe et al. found that 15% of patients could not state the name of their medication and only 41% of patients knew the indication for their warfarin therapy [Citation7]. Tang et al. reported that 75% of patients could not identify possible side effects and that 82% of patients were uncertain of the significance of discontinuation of warfarin therapy [Citation8]. The risks associated with warfarin use are also well documented. As such, informed patient consent prior to the initiation of anticoagulation is of paramount importance. Patients should be educated about the risks and benefits of anticoagulation with warfarin for stroke prevention. In this study, we aimed to evaluate patients’ understanding of their warfarin therapy.
2. Material and methods
A cross-sectional study was performed of patients actively taking warfarin for non-valvular atrial fibrillation in order to assess the knowledge regarding their therapy. A questionnaire about warfarin (), assessing knowledge of indications, benefits, and risks, was distributed to patients at the Warfarin Anticoagulation Clinic at Mayo Clinic Florida, between March 2014 and August 2016. A total of 99 patients on warfarin therapy for non-valvular atrial fibrillation were included in the study. Patients’ baseline knowledge of warfarin therapy, demographics, and clinical characteristics were collected at the time of the survey (). CHADS2 score, HAS-BLED score, and the Charlson Comorbidity Indexes were calculated for each patient through review of their medical records and were compared to their answers on the questionnaire to determine if their responses were correct. Patients who answered six or more questions correctly were labeled as ‘Knowledgeable’, while those who answered fewer than six questions correctly were labeled as ‘Not Knowledgeable’. While at the time of this study, the CHA2DS2-VASc score was available for use, at our institution, the CHADS2 was still primarily in use, and thus the CHADS2 was recorded as opposed to the CHA2DS2-VASc.
Table 1. Patient knowledge questions stratified by how knowledgeable a patient is.
Table 2. Baseline and medical characteristics stratified by how knowledgeable a patient is.
3. Statistical analysis
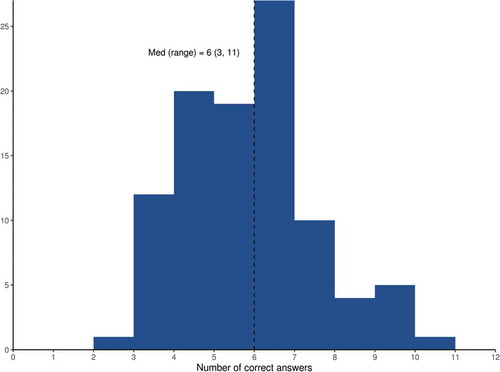
shows a Histogram of the number of correct answers. Data were summarized with the mean (SD), median, Q1, Q3, and range for numeric variables and number (percent) for categorical variables. Fisher’s exact test was used to compare categorical variables and the Kruskal–Wallis test was used to compare continuous variables between knowledgeable and not knowledgeable patients. All tests were two sided and performed at the 0.05 significance level.
4. Results
Sixty-six of 99 (66.7%) patients were classified as knowledgeable and 33 (33.3%) were classified as not. There were no significant differences between the ‘Knowledgeable’ and ‘Not Knowledgeable’ groups in their demographics and clinical characteristics. Fifty-one (77.3%) of knowledgeable patients and 23 (69.7%) of not knowledgeable patients understood that they were taking warfarin because of atrial fibrillation. The majority of patients from both knowledgeable and not knowledgeable groups were unable to answer the following questions (): ‘What is your risk of stroke within a given year if you do not take warfarin?’, ‘Warfarin decreases your risk of stroke by … ?’, and ’Your risk of significant bleeding while on warfarin within a given year is … ?’. The patients listed as ‘Knowledgeable’ were able to correctly answer the questions: ‘Which of the following increases your risk of bleeding if taken while treated with warfarin’? and ‘Which of the following decreases your risk of bleeding if taken while treated with warfarin?’ while the ‘Not Knowledgeable’ patients mostly answered ‘I don’t Know’. There was no statistical significance between ‘knowledgeable’ and ‘not knowledgeable’ patients in regards to how long they had been on warfarin (Figure 3) nor there was a significant difference between the two groups’ time in the therapeutic range.
5. Discussion
The risks and benefits of warfarin therapy for non-valvular atrial fibrillation are well established. Providers have a multitude of tools to calculate a particular patient’s specific risk profile in regards to warfarin therapy, but these can be complex and difficult for many patients to fully understand. Patients who are knowledgeable of their medications, and in particular the benefit they gain from proper adherence to their regimens, are more likely to have positive outcomes [Citation9]. Our study suggests that most patients do not understand their warfarin therapy in detail, highlighting a lack of effective education on the part of the prescribers. Our patients, even those in the ‘Knowledgeable’ group, were unable to report their risk of stroke while on and off warfarin, and were unable to report their risk of significant bleeding while on warfarin. The patients determined to be ‘Knowledgeable’ were aware of what would increase and what would decrease their risk of bleeding while on warfarin; indeed, these are the answers that set them apart from the ‘Not Knowledgeable’ group. This could suggest that patients are more likely to remember what will affect their medication than they are to remember the intricate details regarding the indications for the medication. This could also suggest that providers spend more time telling patients what will affect their medication and do not spend as much time discussing the indications surrounding the medication. As discussed by Bartoli-Abdou et al. [Citation10], patients with more understanding of warfarin demonstrate improved adherence and are more likely to have a consistently therapeutic INR. Specifically, patient beliefs regarding the severity of their illness and their beliefs surround medication efficacy led to increased TTR.
Other patient considerations must be accounted for when planning patient education on warfarin therapy. Studies of patients’ educational achievement have yielded mixed results. Smith et al. [Citation11] found that neither education level nor duration of therapy correlates with a patient’s knowledge of warfarin. On the contrary, Hernandez et al. [Citation9] found that patients with an 8th grade education or below had more difficulty with proper warfarin adherence than those with a college/university level of education. Patients with lower education levels were more likely to have subtherapeutic or supratherapeutic INRs (5.1% vs 2.8%, p < 0.05). Their investigation suggests patients with lower education levels also had more frequent bleeding events and strokes (2.6% vs 0.71%, p < 0.05), despite similar familiarity with the indication for their warfarin therapy. In our study, there was no difference in education level between the two groups. Our population was generally well educated with over 80% participating in more than high school education.
We did investigate if there would be any difference between our two groups of patients in their TTR. Here, we defined TTR as the percentage of therapeutic INRs (2.0–3.0) divided by the total number of INRs collected. There was no difference between our ‘knowledgeable’ and ‘not knowledgeable’ patient groups in relation to their TTR. We hypothesize that a similar number of total INRs in both groups, meaning similar compliance in INR checks, led to similar TTR for both groups ().
The geriatric population is particularly vulnerable to harm from warfarin therapy. Yiu and Bajorek [Citation12] reported that patients over age 65 have worse compliance, leading to decreased TTR, and an increased risk of adverse bleeding events. The majority of these patients had no follow-up education over the course of 1 to 5 years of warfarin therapy. Ongoing education is important, as many aspects of warfarin knowledge have a retention time as short as 28 to 56 days [Citation13].
Education and materials provided to patients must be easy to understand and readily accessible. Relying on the FDA medication guide for warfarin often leads to unsatisfactory patient knowledge and outcomes [Citation14]. Several approaches have been successful in leading to a better understanding of warfarin therapy such as one-on-one education [Citation15], video education from a pharmacist [Citation16], post-hospital discharge education [Citation17], and nurse-led anticoagulation clinics [Citation18].
An Australian study focused on redesigning warfarin educational materials emphasized five key elements, health professional/patient communication and partnerships; warfarin compliance; simple, easy-to-read warfarin information; improved continuity of care between hospital and community settings; and patient follow-up [Citation19]. Such changes led to improved patient outcomes which were particularly pronounced in ‘at risk’ groups including the elderly, those with low-literacy, and patients whose first language was not English.
We believe that utilizing the CHA2DS2-VASc score in patient education would increase patients’ understanding of their risk of stroke while on and off warfarin. Sharing the score with them would encourage patient participation and increase compliance and TTR. We also believe a follow-up, prospective study could address this issue.
6. Conclusions
While most of our patients understood that they were taking warfarin because of their atrial fibrillation, the majority could not quantify their risk of stroke while on and off warfarin, and their risk of bleeding while on warfarin. Risk scores for these events (e.g., CHADS2score and Has-Bled score) in patients with non-valvular atrial fibrillation treated with warfarin are readily available and widely utilized by the medical community but not commonly emphasized in patient education at our institution. Consequently, a large proportion of our patients were found to have a low understanding of the risks and benefits of anticoagulation.
This study was conducted at a specialized anticoagulation clinic at an academic tertiary care medical facility that serves a generally affluent and well-educated population and utilizes standardized educational materials and counseling by specialized nursing staff. Despite these advantages, most patients were unable to accurately articulate their risks with and without warfarin therapy. This knowledge deficit may relate in part to our failure to include teaching focused on well-established clinical risk scores that can place thrombotic and bleeding risks into perspective. We have proposed that each patient treated with warfarin for atrial fibrillation be provided with their individualized risk estimates based on the CHA2DS2-VASc and HAS-BLED scores along with other routine educational materials and that this education be repeated annually by the anticoagulation clinic staff. Future research will focus on the impact of such an intervention not only on patient knowledge but clinical outcomes, as well.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994;154:1449.
- Stroke Prevention in Atrial Fibrillation Study. Final results. Circulation. 1991;84:527–539.
- The Boston Area Anticoagulation Trial for Atrial Fibrillation Investigators. The effect of low-dose warfarin on the risk of stroke in patients with nonrheumatic atrial fibrillation. N Engl J Med. 1990;323(22):1505–1511.
- Ezekowitz MD, Bridgers SL, James KE, et al. The veterans affairs stroke prevention in nonrheumatic atrial fibrillation investigators warfarin in the prevention of stroke associated with nonrheumatic atrial fibrillation. N Engl J Med. 1992;327(20):1406–1412. Erratum. N Engl J Med. 1993; 328:148.
- Wann LS, Curtis AB, January CT, et al. ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (updating the 2006 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2011;57:223–242.
- Oake N, Jennings a, Forster AJ, et al. Anticoagulation intensity and outcomes among patients prescribed oral anticoagulant therapy: a systematic review and meta-analysis. CMAJ. 2008;179(3):235–244.
- Tang EO, Lai CS, Lee KK, et al. Relationship between patients’ warfarin knowledge and anticoagulation control. Ann Pharmacother. 2003;37(1):34–39.
- McCabe PJ, Schad S, Hampton a, et al. Knowledge and self-management behaviors of patients with recently detected atrial fibrillation. Heart Lung. 2008;37(2):79–90.
- Madrid AH, Potpara TS, Dagres N, et al. Differences in attitude, education, and knowledge about oral anticoagulation therapy among patients with atrial fibrillation in Europe: result of a self-assessment patient survey conducted by the European Heart Rhythm Association. EP Europace. 2016 Mar 1;18(3):463–467.
- Bartoli-Abdou JK, Patel JP, Xie R, et al. Associations between illness beliefs, medication beliefs, anticoagulation-related quality of life, and INR control: insights from the switching study. Res Pract Thromb Haemost. 2018;2(3):497–507. Published 2018 Jun 7.
- Smith M, Christensen N, Wang S, et al. Warfarin knowledge in patients with atrial fibrillation: implications for safety, efficacy, and education strategies. Cardiology. 2010;116(1):61–69.
- Yiu AW, Bajorek BV. Health literacy and knowledge in a cohort of Australian patients taking warfarin. Pharm Pract (Granada). 2018 Jan-Mar;16(1):1080.
- Collins S, Barber a, Sahm LJ. Pharmacist’s counselling improves patient knowledge regarding warfarin, irrespective of health literacy level. Pharmacy. 2014;2(1):114–123.
- Schwartz L, Mazzola N, Hoffman RS, et al. Evaluating patients’ understanding of printed warfarin medication information. J Pharm Pract. 2015;28(6):518–522.
- Baysal E, Midilli TS. Effects of structured patient education on knowledge level and INR control of patients receiving warfarin: randomized controlled trial. Pak J Med Sci. 2018;34(2):240–246.
- Moore SJ, Blair EA, Steeb DR, et al. Impact of video technology on efficiency of pharmacist-provided anticoagulation counseling and patient comprehension. Ann Pharmacother. 2015;49(6):631–638.
- Brunetti L, Lee SM, Doherty N, et al. 721. Int J Clin Pharm. 2018;40. DOI:10.1007/s11096-018-0631-y
- Salinero M, Hyman T. Reducing warfarin ADR’s with a nurse led anticoagulation clinic: a new model of patientcare. All Publications. 2095. Mullan: Judy; 2017.
- Mullan J. To develop and trial a new warfarin education program [PhD thesis]. Graduate School of Public Health, University of Wollongong; 2005. Available from: http://ro.uow.edu.au/theses/561