ABSTRACT
Takotsubo Cardiomyopathy (TCM) is characterized by a transient but reversible ventricular dysfunction in post-menopausal females following, but not always, a recent emotional or physical stress. Typically, chest pain is reported as a presenting symptom in the majority of patients. The severe diarrheal illness secondary to acute viral gastroenteritis is not commonly reported as the stressor event prior to TCM. We report a unique case of a middle-aged male presented with syncope shortly after loose bowel movements. He was diagnosed with TCM and was successfully managed with supportive care. The purpose of this case is to make clinicians aware of this rare association.
1. Introduction
Takotsubo cardiomyopathy (TCM), stress-induced cardiomyopathy, apical ballooning syndrome, or broken heart syndrome is characterized by acute reversible left ventricular systolic dysfunction (LVSD) mimicking myocardial infarction, but with clean coronaries on angiography [Citation1]. The term ‘Takotsubo’ is derived from the Japanese name for an octopus trap, which has a similar shape to the systolic apical ballooning appearance of the LV in stress-induced cardiomyopathy [Citation2]. TCM predominantly occurs in post-menopausal females following, but not always, a recent emotional or physically stressful event [Citation3]. It is unusual for acute viral gastroenteritis (AVG) to precipitate a TCM. Herein, we report a case of a middle-aged male patient with a recent episode of AVG who presented with syncope and was found to have elevated troponin levels, clean coronaries on angiography and evidence of apical ballooning on left ventriculogram. Our case highlights that in patients who present with diarrhea and new-onset heart failure symptoms or syncope and elevated troponins should be evaluated with angiography to rule out acute coronary syndrome or rule in TCM if there is no evidence of obstructive coronary artery disease on angiography.
2. Case presentation
A 58-year-old male with a past medical history of chronic obstructive pulmonary disease (COPD) and hypertension presented to the emergency department (ED) after being found unresponsive in the restroom. He had 5–6 loose watery diarrheal episodes associated with nausea and vomiting for the past 24 hours. The family denied that the patient complained of any chest pain or prior hospitalization or any travel very recently. On arrival to the ED, his vitals demonstrated a blood pressure of 132/99 mmHg, a heart rate of 131/min, a temperature of 98.2 F, and a respiratory rate of 29/min with oxygen saturation of 98% on bag-mask ventilation, started by EMS due to hypoxia. He was eventually intubated and started on mechanical ventilation due to resistant hypoxemia. His cardiopulmonary examinations did not reveal any murmurs, rubs, or gallops but were significant for mild crackles in the lung bases bilaterally. Subsequently, an arterial blood gas (ABGs) demonstrated a pH of 7.28, pCO2: 52.5 mmHg, pO2: 123.7 mmHg, HCO3: 24.5 mmol/L while on mechanical ventilation with 100% FiO2. The ventilator settings were titrated based on oxygen saturation and pCO2.
The serial electrocardiograms (EKGs) were not suggestive of ischemic changes but did show some premature ventricular contractions. His initial cardiac troponin was less than 0.1 ng/mL but the second troponin came back elevated at 2.74 ng/ml. His initial laboratory workup was as follows; Hemoglobin: 14.9 g/dL, white blood cell count: 23.6 k/UL, Platelets: 420 k/UL, serum sodium: 140 milliequivalent per liter (mEq/L), potassium: 5.1 mEq/L, chloride: 101 mEq/L, lactic acid: 2.2 mEq/L, anion gap: 20, blood glucose: 259 milligrams per deciliter (mg/dL), blood urea nitrogen: 25 mg/dL, and serum creatinine: 1.68 mg/dL.The blood and urine cultures, influenza swab, stool samples for clostridium difficile (C. Diff), and Shigella toxin were collected and the patient was initially treated with intravenous fluids, cefepime, and metronidazole for a possible sepsis syndrome related to bacterial enterocolitis. However, antibiotics were stopped after negative results were obtained on blood, stool and urine cultures. The cardiac b-type natriuretic peptide (BNP) was elevated at 544 pg/mL, and D-Dimer was 5250 ng/ml. An urgent Computed Tomography scan chest ruled out pulmonary embolism.
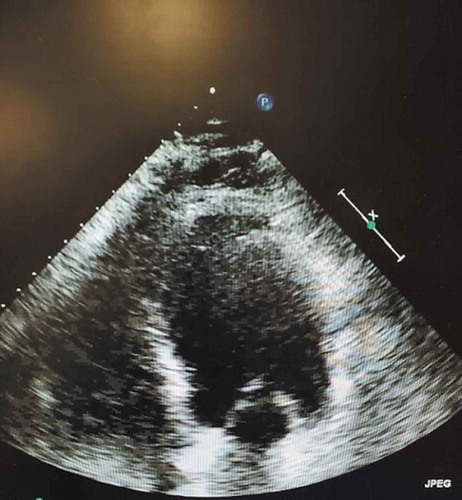
Transthoracic echocardiography was done, which was suggestive of decreased ejection fraction (EF) of 20–25% with diffuse apical hypokinesis (). He was started on heparin for the suspicion of NSTEMI. The urgent coronary catheterization did not reveal any significant obstructive coronary artery disease. However, the ventriculogram showed apical hypokinesis and ballooning, consistent with TCM ().
He was started on a low dose of beta-blocker and an ACE inhibitor. Over the next two days, his diarrhea resolved, and his overall condition improved. He was eventually extubated and was stable in room air. Over the next few days, he was deemed stable and was downgraded to the general medical floor and discharged home on a beta-blocker and life vest.
On follow up after two months, he had a cardiac magnetic resonance imaging (C-MRI) done which showed an average ejection fraction with no infiltrative or other myocardial diseases. ().
3. Discussion
Takotsubo cardiomyopathy (TCM) is characterized by transient but reversible left ventricular systolic dysfunction which resolves within a few days to weeks. Chest pain is reported as a typical presenting symptom (70% of cases) which mimics acute coronary syndrome. However, a small number of cases may be asymptomatic [Citation4]. TCM has been identified in 1–2% of troponin positive patients suspected as having an acute myocardial infarction [Citation5]. Acute viral gastroenteritis (AVG) is the viral-induced inflammation of the gastrointestinal tract causing vomiting, diarrhea and abdominal pain with or without fever. It usually is self-limiting and does not lead to complications. TCM predominantly occurs in post-menopausal females following, but not always, a recent emotional or physically stressful event [Citation3]. Given the benign nature, it is rare for AVG to be associated with Takotsubo syndromes, like in our case. A literature search using different medical subject headings (MeSH) on PubMed identified only three cases of gastroenteritis-related Takotsubo syndrome [Citation6–Citation8]. Interestingly, patients were at the both extreme of their ages, with two elderly patients (72 and 65-year-old) and the other one only 15 months old. One of the previously reported elderly patients was male and one was female. All patients presented with diarrhea predominantly. Two reported cases had C. Diff related gastroenteritis and one had viral gastroenteritis, similar to our case. All patients had classic findings of Takotsubo syndrome, defined as apical ballooning with reduced ejection fraction. One patient with C. Diff-induced TCM expired, while the patient with AVG had a successful recovery. Our patient also has had a successful recovery with supportive management only. All cases, including our case, are summarized in .
Table 1. Characteristics of previously published gastroenteritis-induced TCM.
The exact pathophysiology of TCM is yet to be fully understood. However, it is postulated to result from one of the following mechanisms: catecholamine-mediated cardiac toxicity, left ventricular (LV) outflow tract obstruction, multivessel coronary spasm, or microvascular dysfunction [Citation4]. The sustained beta-receptor stimulation secondary to stress-related catecholamines surge is believed to cause beta 1 and beta 2-adrenergic receptor down regulation. This can result in a blunted myocardial adrenergic stimulation, hence, resulting in LV apex stunning or ballooning [Citation9]. Since beta-adrenergic receptors are densely located in the LV apex than in the base, thus the apical myocardium being more susceptible, particularly to epinephrine than the basal segments [Citation10]. Wittstein et al. first reported the significantly raised catecholamines levels during an acute episode of TCM [Citation11]. Hence it is plausible that AVG, as in our case, can cause a release of inflammatory markers and increase catecholamine levels in the blood which could have led to TCM.
The diagnosis of TCM can be made by meeting the Mayo Clinic diagnostic criteria [Citation12]. Our patient met the criteria by having transient LV systolic dysfunction (LVSD) with a decreased EF in hospital and normalization of EF on repeat imaging after two months, absence of obstructive coronary artery disease on angiography and absence of myocarditis as seen on repeat MRI. The fourth criteria are new EKG abnormalities or elevation in cardiac troponin. Interestingly, our patient did not show any of the EKG changes, he, however, did meet the diagnostic criteria for TCM. Our patient had a mildly elevated troponin. It is important to note that the diagnosis of TCM does not require the presence of stressors and can happen in the absence of an identifiable cause [Citation3].
The treatment of TCM is mainly supportive. It is advised to start all patients on a beta-blockers (to inhibit catecholamines induced beta receptors stimulation in myocytes) and angiotensin-converting enzyme inhibitors as they improve the recovery of Takotsubo syndrome [Citation4]. In our patient, other indications for these medications were hypertension. Since the treatment of AVG is mainly supportive so we monitored it. Management should also be individualized depending upon the TCM-related complications. For example, diuretics would be given for LVSD while anticoagulation would be started for ventricular thrombi. However, careful volume management should be undertaken in left ventricular outflow obstruction.
Patients with Takotsubo syndrome usually have a good prognosis and the heart function returns to normal over the course of a few months, however, the risk of severe complications in the hospital are similar to patients with CAD.
Takotsubo syndrome is reversible if the stressor is managed appropriately, and regular follow up is indicated. Takotsubo syndrome should be considered in the setting of major stressors but it can be caused by a trivial event such as AVG or without an identified stressor. Our case highlights that TCM should be suspected in patients presenting with diarrhea and symptoms of new-onset heart failure. Furthermore, EKG changes most commonly seen can be suggestive of ischemic changes and it is imperative to do coronary angiography to rule out acute coronary syndrome.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Bybee KA, Kara T, Prasad A, et al. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med. 2004 Dec 7;141(11):858–865.
- Yoshikawa T. Takotsubo cardiomyopathy, a new concept of cardiomyopathy: clinical features and pathophysiology. Int J Cardiol. 2015 March 1;182:297–303. .
- Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006 May 23;27(13):1523–1529.
- Roshanzamir S, Showkathali R. Takotsubo cardiomyopathy a short review. Curr Cardiol Rev. 2013 August 1;9(3):191–196.
- Kurowski V, Kaiser A, von Hof K, et al. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest. 2007;132(3):809.
- Virk HU, Inayat F. Clostridium difficile infection and Takotsubo cardiomyopathy: is there a relation? N Am J Med Sci. 2016 Jul;8(7):316.
- Okada S, Azuma Y, Kaneyasu H, et al. (stress) cardiomyopathy and obstructive renal stones in an infant with norovirus gastroenteritis. Int J Cardiol. 2015 May;1(186):233–235.
- Elikowski WA, Małek-Elikowska MA, Lisiecka MO, et al. Fatal course of takotsubo cardiomyopathy in a female with recurrent clostridium difficile infection. Pol Merkur Lekarski. 2017 Jun 23;42(252):256–259.
- Lyon AR, Rees PS, Prasad S, et al. Stress (Takotsubo) cardiomyopathy—a novel pathophysiological hypothesis to explain catecholamine-induced acute myocardial stunning. Nat Rev Cardiol. 2008 January;5(1):22. .
- Mori H, Ishikawa S, Kojima S, et al. Increased responsiveness of left ventricular apical myocardium to adrenergic stimuli. Cardiovasc Res. 1993 February 1;27(2):192–198.
- Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005 February 10;352(6):539–548.
- Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008 Mar 1;155(3):408–417.