ABSTRACT
Background
The Brugada pattern is identified on the EKG by a coved ST-segment elevation accompanied by a negative T wave in the early precordial leads in the absence of a cardiac structural abnormality. Brugada pattern and Brugada syndrome should be differentiated, as the latter is associated with an increased risk of sudden cardiac death.
Methods
The literature was searched using multiple databases to identify all the articles on Brugada pattern. Data were screened and analyzed by independent authors.
Results
Sixty articles, comprising 71 patients, were included in the study. The mean age of patients was 42.6 years, with a higher prevalence of Brugada pattern in men (83%) than women (17%). The most frequent findings associated with Brugada pattern was fever (83%). Other less common presentations included cough (21%), sore throat (10%), syncope (18%), abdominal pain (8%), and chest pain (7%). Comorbidities included pneumonia (30%), upper respiratory tract infections (14%) and smoking (14%). Among treatment modalities, 39% of patients had ICD placement performed, 44% received antibiotics, while 14% had supportive care. Adenosine was given to 3% of patients, while other antiarrhythmics like milrinone, amiodarone, sotalol, procainamide, flecainide, and nitroglycerin were given to 1% of patients. Most patients with Brugada syndrome had a satisfactory outcome, with only 4% mortality rate(WHAT ABOUT THE OTHER 11%?). Out of the 71 patients, 3% had persistent Brugada patterns, while 86% of patients recovered completely. There was no significant effect of ICD on mortality or Brugada pattern resolution (p 0.37).
Conclusion
Our study shows that fever is the main reason for unmasking the Brugada pattern in patients with this channelopathy. ICD placement in such patients is not recommended as it has no mortality benefits.
1. Introduction
The Brugada pattern was first described in 1992 by Brugada, characterized by ST-segment elevation accompanied by a negative T wave in the early precordial leads without any cardiac structural abnormality [Citation1]. In 1996, Yan and Antzelevitch proposed that this ST-segment elevation and right bundle branch block (RBBB) appearance had a cellular basis for the development of life-threatening arrhythmias [Citation2]. This theory further confirmed by Kobayashi et al. and Miyazaki et al. [Citation3–Citation6] This review aims to summarize the known literature specifically on the Brugada pattern and also highlights the distinguishing features of Brugada pattern and Brugada syndrome.
2. Materials and methods
A literature search for relevant articles was performed using MEDLINE (PubMed, Ovid), Embase, and Cochrane databases. A total of 60 articles were selected after initial screening and duplicates removal. The authors extracted data into an excel sheet identifying presentation, risk factors, diagnostic modalities, management, and outcome of patients with Brugada pattern.
3. Results
A total of 71 patients were identified from the included 60 articles. The mean age was 42.6 years. Approximately 35% of the patients were 50 years or older. Of the reported cases, 83% were males, and 17% were females. Overall, the most common presentation was fever in 83% of patients. Upper respiratory symptoms were also reported frequently, including cough in 21%, sore throat in 10%. Besides these, syncope was present in 18%, abdominal pain in 8%, chest pain in 7%, arthralgia in 4%, nausea and vomiting in 4%, and pleuritic chest pain in 3%. The most common associated comorbidity was pneumonia, present in 30% of patients. An upper respiratory tract infection was present in 14% of the patients. Ventricular fibrillation was present in 8% and ventricular tachycardia in 4%. Other comorbidities are shown in
Table 1. This table depicts the epidemiology, most common presenting symptoms, and comorbidities associated with presentation of Brugada pattern.
Thirty nine percent of patients had an ICD placed for the Brugada pattern. Forty four percent of patients received antibiotics. As many of the patients presented with fever or an infection. One patient underwent defibrillation. Three percent received adenosine, and 1% received milrinone, amiodarone, sotalol, procainamide, flecainide or nitroglycerine. This is shown in
Table 2. Management of our patient population with Brugada syndrome.
Most of the patients with the Brugada pattern had a good outcome. 86% of the patients recovered, while 4% died and 3% had persistent brugada pattern, no outcome data was available in 7% patients.
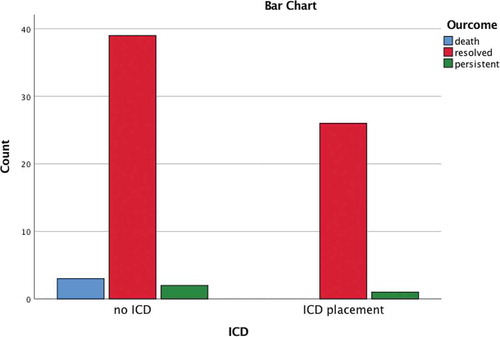
The clinical outcomes in these patients were further assessed based on presentation, comorbidities, and management. One important characteristic that was evaluated as if there was any association of ICD placement with better outcomes. A total of 27 patients had an ICD placed, and out of these patients, 26 (96%) recovered, while one patient had persistent Brugada pattern. There were no deaths recorded. On the other hand, in patients that did not receive an ICD, 3 (7%) of the patients died, 39 (88%) recovered, and 2 (5%) patients had persistent Brugada pattern. Even though the rate of death was much higher (6.8% vs. 0%) in patients who did not receive an ICD, this difference was not statistically significant (p = 0.372).
Figure 1. This figure depicts the outcomes in patients who received and those who did not receive an ICD.
The outcomes of patients with different presentations, associations, co-morbidities, and management options were analyzed, as depicted in . There was no statistically significant association, based on chi-square test, between different outcomes and any of the above-described feature.
Table 3. This table depicts the association between different outcomes and different patient characteristics.
4. Discussion
Our analysis indicates Brugada pattern is a relatively benign condition mostly unmasked by fever and has favourable outcomes if the underlying conditions are treated. These patients have channelopathy just like brugada syndrome patients but they do not have a history of sudden cardiac death in their family nor have been symptomatic in life, differentiating them from brugada syndrome. As per our study, patients with brugada pattern do not need ICD placement or antiarrhythmic medications. The brugada pattern resolves with the management of the underlying condition. Brigada pattern patients do not have symptoms, so they are usually unaware of their condition unless diagnosed incidentally on EKG.
5. Clinical presentation
Brugada pattern typically is unmasked by fever due to any cause, mostly in association with a chest infection. Our study found fever was associated with Brugada pattern in 83% of presenting patients. Further, we found the most frequent association was with pneumonia (30%) and upper respiratory tract infection (14%). Other findings associated with Brugada pattern included cough in 21% of the individuals, sore throat in 10%, syncope in 18%, abdominal pain in 8% and chest pain in 7%.
Brugada pattern typically presents during adulthood (42.6% in our study). A study of 384 patients showed its occurrence in men predominantly (70%) [Citation7]. Our study showed a higher prevalence in males (83%) compared to females (17%).
6. Molecular genetics and cellular mechanisms
Brugada syndrome shows an autosomal dominant mode of transmission. In 1998, Chen et al. demonstrated the link of Brugada syndrome to the alpha subunit of the cardiac sodium channel gene (SCN5A gene) [Citation8]. The loss of function of this gene can be caused by a failure of expression of the channel, accelerated inactivation of the pathway, inactivation of the channel to an intermediate state with a slow recovery, or a shift in voltage and time-dependent sodium channel activation, inactivation, or reactivation [Citation9]. It was observed that the accelerated inactivation of sodium channels occurred at temperatures above the physiologic range suggesting the possible mechanism for Brugada pattern in a febrile state [Citation10]. In 2002, Antzelevitch et al. identified patients of the Brugada pattern exhibiting fever-induced ventricular tachycardia (VT) [Citation11].
Various studies conducted to understand the cellular mechanisms of Brugada pattern suggest a rebalancing of active currents at the end of phase 1 causing the ST-segment elevation or J wave observed in the Brugada pattern [Citation12]. The accentuation of the J wave leads to a saddleback configuration of the repolarization waves. As the notch becomes more prominent due to the prolongation of an epicardial action potential, the direction of repolarization across the RV wall and transmural voltage gradient is reversed. This leads to a typical dome-like ST segment elevation and T wave inversion. ()
7. Diagnosis
Brugada pattern is characterized by three types of repolarization patterns in the right precordial ECG leads. Out of these three patterns, type 1 pattern is diagnostic of Brugada, and it consists of a coved ST-segment elevation of more than 2 mm (0.2 mV) followed by T wave inversion. Type 2 ECG pattern of Brugada typically shows a saddleback appearance with an ST-segment elevation of ≥2 mm, a trough showing ≥1 mm ST elevation, and a positive or biphasic T wave [Citation8]. In type 3, there is an ST-segment elevation of <1 mm with a saddleback or coved appearance. The definitive diagnosis in types 2 and 3 is made by the presence of type 1 ST-segment elevation in more than one right precordial lead (V1 to V3) in the presence or absence of a sodium channel blocking drug [Citation12]. The three types of Brugada patterns are illustrated in the figure below. ()
Figure 2. EKG of a patient with Brugada syndrome with three characteristic patterns. The left panel shows a type 1 ECG, whereas the middle and right panels show type 2 and 3 ECGs.
It is essential to exclude other factors that could lead to the these ECG abnormalities, such as atypical RBBB, left ventricular hypertrophy, acute pericarditis, dissecting aortic aneurysm, electrolyte abnormalities, or mechanical compression of the right ventricular outflow tract (RVOT) [Citation12].
8. Management
Over the past few years, a considerable amount of progress has been observed in the diagnosis and characterization of Brugada pattern and syndrome. However, the same cannot be said about its management. For Brugada syndrome, an ICD has proved to be the only definitive treatment [Citation13]. However, its use is riddled with limitations. It is not a feasible treatment option in infants and young children, and in some parts of the world, its implantation is extremely expensive. Patients with Brugada pattern, however, require supportive care and treatment of febrile illness. There was no significant benefit of ICD or pacemaker noted in our review on the Brugada pattern
Other options in Brugada syndrome are pharmacological therapy, including quinidine to restore the epicardial action potential dome, leading to normalization of the ST segment and preventing phase 2 reentry and development of VT [Citation14]. However, its use in the prevention of sudden death has not been established. Other antiarrhythmic drugs such as amiodarone and beta-blockers have been observed to be ineffective, whereas class IA antiarrhythmic such as procainamide and class IC antiarrhythmics such as flecainide and propafenone are contraindicated [Citation15]. Our study, however, focused on the management of the Brugada pattern only and revealed that 39% of patients had ICD placement performed for Brugada pattern due to other compelling indications (family history of sudden deaths, low ejection fraction). Most patients (44%) were started on antibiotics for the treatment of underlying febrile illness while supportive care was given to 14% of patients. Only a few patients had antiarrhythmic therapies, adenosine (3%) and milrinone, amiodarone, sotalol, procainamide, flecainide, and nitroglycerin were given to 1% of patients.
9. Outcome
According to our study, most patients with the Brugada pattern had a satisfactory outcome, with a mortality rate of only 4%. Out of the 71 patients, 3% had persistent Brugada patterns, while 86% of patients recovered completely. When the recovery pattern of the different treatment modalities was assessed, 96.3% of patients with ICD placement had a complete recovery, while in patients who underwent conservative treatment, 88.6% recovered completely, 4.5% had persistent Brugada pattern, and 6.8% (n = 3) patients died.
10. Conclusions
Brugada syndrome is associated with a high incidence of sudden deaths in adults with structurally healthy hearts and should be managed with ICD, pacemaker, or antiarrhythmic medications. Brugada pattern, on the other hand, is a benign condition usually unmasked by fever and can be reversed by alleviating the cause of illness. ICD has no mortality benefit in the Brugada pattern.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391–1396.
- Yan GX, Antzelevitch C. Cellular basis for the electrocardiographic J wave. Circulation. 1996;93:372–379.
- Kobayashi T, Shintani U, Yamamoto T, et al. Familial occurrence of electrocardiographic abnormalities of the Brugada-type. Intern Med. 1996;35:637–640.
- Miyazaki T, Mitamura H, Miyoshi S, et al. Autonomic and antiarrhythmic drug modulation of ST-segment elevation in patients with Brugada syndrome. J Am Coll Cardiol. 1996;27:1061–1070.
- Probst V, Wilde AA, Barc J, et al. SCN5A mutations and the role of genetic background in the pathophysiology of Brugada syndrome. Circ Cardiovasc Genet. 2009;2:552–557.
- Antzelevitch C, Brugada P, Brugada J, et al. Brugada syndrome: a decade of progress. Circ Res. 2002;91:1114–1118.
- Benito B, Sarkozy A, Mont L, et al. Gender differences in clinical manifestations of Brugada syndrome. J Am Coll Cardiol. 2008 Nov 4;52(19):1567–1573.
- Chen Q, Kirsch GE, Zhang D, et al. Genetic basis and molecular mechanisms for idiopathic ventricular fibrillation. Nature. 1998;392:293–296.
- Bezzina CR, Rook MB, Wilde AAM. Cardiac sodium channel and inherited arrhythmia syndromes. Cardiovasc Res. 2001;49:257–271.
- Dumaine R, Towbin JA, Brugada P, et al. Ionic mechanisms responsible for the electrocardiographic phenotype of the Brugada syndrome are temperature dependent. Circ Res. 1999;85:803–809.
- Antzelevitch C, Brugada R. Fever and the Brugada syndrome. Pacing Clin Electrophysiol. 2002;25:1537–1539.
- Wilde AA, Postema PG, Di Diego JM, et al. The pathophysiological mechanism underlying Brugada syndrome: depolarization versus repolarization. J Mol Cell Cardiol. 2010 Oct 1;49(4):543–553.
- Brugada J, Brugada R, Brugada P. Pharmacological and device approach to therapy of inherited cardiac diseases associated with cardiac arrhythmias and sudden death. J Electrocardiol. 2000;33(Suppl):41–47.
- Yan GX, Antzelevitch C. Cellular basis for the Brugada syndrome and other mechanisms of arrhythmogenesis associated with ST-segment elevation. Circulation. 1999;100:1660–1666.
- Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST-segment elevation in leads V1through V3. A marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998;97:457–460.
