ABSTRACT
Bile cast nephropathy (BCN) is a rare form of acute kidney injury (AKI) that occurs in the setting of hyperbilirubinemia. We present the case of a 67 year-old male with severe kidney injury who was found to have obstructive cholestasis. By way of this report, we aim to expand upon the existing literature and showcase the importance of timely endoscopic retrograde cholangio-pancreatography (ERCP) in this setting, in order to prevent irreversible kidney damage.
1. Introduction
Bile cast nephropathy (BCN), also known as biliary nephrosis, is a form of acute kidney injury (AKI) in the setting of hyperbilirubinemia. Patients typically present with jaundice, bilirubin levels greater than 20, and a rising creatinine in the setting of nonspecific symptomatology [Citation1]. Amongst the obscure causes of kidney injury, BCNs difficulty to diagnose, the lack of a standardized treatment regimen, and its under-representation in the literature add to its complexity [Citation2]. As such, this condition often requires a high index of clinical suspicion as well as a multi-disciplinary approach to accurately diagnose and manage [Citation1–3]. Herein, we present the case of a 67 year-old male with severe kidney injury who was found to have obstructive cholestasis. By way of this report, we aim to expand upon the existing literature and showcase the importance of timely endoscopic retrograde cholangio-pancreatography (ERCP) in this setting – in order to prevent disease progression and subsequent irreversible kidney damage.
2. Case presentation
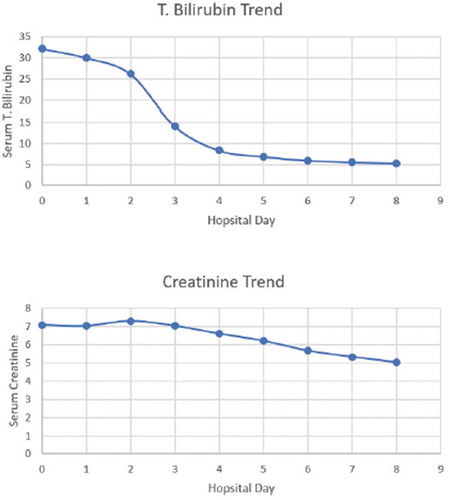
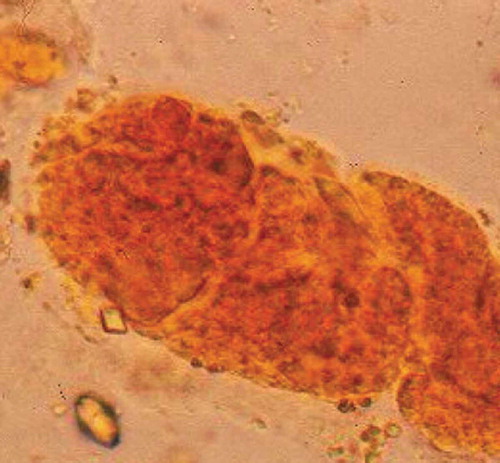
A 67-year-old Hispanic male with no known medical history presented to our emergency department complaining of decreased appetite and fatigue for the last 2 weeks. Family and social history were non-contributory. Upon physical examination, the patient had jaundice, scleral icterus, and right upper quadrant abdominal pain, while the remainder of the physical exam was unremarkable. Laboratory studies were significant for a cholestatic obstructive pattern seen by an aspartate transaminase/alanine transaminase (AST/ALT) of 170/134 U/L, direct bilirubin/total bilirubin of 22/32.2 mg/dL, alkaline phosphatase >763 U/L. The patient had a BUN/creatinine of 115/7.08 mg/dL and a urine analysis demonstrating dark-yellow urine with no proteinuria, dysmorphic red blood cells, or eosinophils. In addition, urobilinogen was elevated at 4 EU/dL. Upon microscopic examination of the urine sample, bilirubin-stained epithelial cells (bilirubin casts) were seen (). Renal ultrasound was performed and excluded other causes of obstructive uropathy. Ultrasound of the abdomen revealed gallbladder wall thickening and biliary ductal dilatation. Multi-disciplinary decision was made to pursue a magnetic resonance cholangiopancreatography, which subsequently confirmed the presence of a 1.1 cm distal common bile duct stone with proximal intra and extra-hepatic biliary ductal dilatation (). The patient underwent urgent ERCP with sphincterotomy and stent placement. Immediately following the ERCP, direct/total bilirubin and serum creatinine returned to near baseline levels. Within the next 24 hours, the patient was safely discharged home ().
Figure 1. Bilirubin-stained epithelial cells (bilirubin casts) was apparent upon microscopy of centrifuged urine sample
3. Discussion
While the exact pathophysiology of BCN remains unknown, it is presumed to be secondary to elevated bile acid levels causing oxidative injury to the renal tubules [Citation2]. An additional proposed mechanism is bile cast deposition leading to tubular obstruction at the level of the nephron [Citation2–4]. Finally, the last hypothesized cause involves direct toxic damage by sulfated bile salts [Citation2–4]. Recent studies have considered the extra-hepatic effects of bile salts on the myocardium, where it was shown that elevated levels of bile salts elicited a negative inotropic and chronotropic effect leading to renal hypo-perfusion [Citation2]. Interestingly, it has been suggested that bile casts may trigger the inflammasome signalling cascade via built up oxidative stress, hence leading to interstitial inflammation and driving bile cast nephropathy pathobiology [Citation5].
Although kidney biopsy is the solitary means of establishing definitive diagnosis, it is often too invasive, or not practical. As such, urine analysis, with characteristic bile‐stained granular casts, as seen in this case, is pathognomonic for BCN. As a simple and inexpensive method, it can reliably suggest this diagnosis, when kidney biopsy was not obtained.
Treatment should be targeted at improving hepatic dysfunction and relieving the biliary obstruction without delay. This may improve renal function, but the patient may still need temporary dialysis or plasmapheresis if renal function fails to improve following treatment directed at the underlying cause of hyperbilirubinemia [Citation1–3]. Conservative complementary modalities such as the use of steroids, or ursodeoxycholic acid, and lactulose have shown minimal benefit in studies [Citation6].
4. Conclusion
In conclusion, as under-representation of BCN in the literature adds to its variability in management, a multi-disciplinary approach is essential. As BCN is a plausible phenomenon in patients presenting with an AKI and hyperbilirubinemia, we hope to encourage clinicians to maintain a broad differential in similar scenarios. In addition, by way of this report, we highlight the prompt role of ERCP in this setting, in order to help prevent irreversible renal damage.
A statement of manuscript approval
We approve that the manuscript was read and approved by all of the Authors, and we believe that the manuscript represents honest work.
Informed consent
Informed consent was obtained for publication of the case details.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Krones E, Wagner M, Eller K, et al. Bile acid-induced cholemic nephropathy. Dig Dis. 2015;33(3):367–375.
- Patel J, Walayat S, Kalva N, et al. Bile cast nephropathy: A case report and review of the literature. World J Gastroenterol. 2016;22(27):6328–6334.
- Fisler A, Breidthardt T, Schmidlin N. Bile cast nephropathy: the unknown dangers of online shopping. Case Rep Nephrol Dial. 2018;8(2):98–102.
- Van Slambrouck CM, Salem F, Meehan SM, et al. Bile cast nephropathy is a common pathologic finding for kidney injury associated with severe liver dysfunction. Kidney Int. 2013;84(1):192–197.
- Giuliani KTK, Kassianos AJ, Kildey K, et al. Role of inflammation and inflammasome activation in human bile cast nephropathy. Nephrology (Carlton). 2020;25(6):502–506.
- Betjes MG, Bajema I. The pathology of jaundice-related renal insufficiency: cholemic nephrosis revisited. J Nephrol. 2006;19(2):229–233.