ABSTRACT
Aortitis is an inflammation of the aorta that is linked to large vessel vasculitis and other rheumatologic cases. Less often, an infectious etiology of aortitis is diagnosed. Aortitis is associated with high mortality and morbidity and requires a high index of suspicion. Here we present a rare case of aortitis secondary to Salmonella Septicemia treated with six weeks of antibiotics in the hospital without and remained asymptomatic and inflammatory markers normalized at 2 weeks follow up (ESR, CRP, and WBCs).
1. Introduction
Aortitis is an inflammation of the aortic wall that can be seen in giant cell arteritis (GCA) and Takayasu arteritis [Citation1]. It can also be seen in some rheumatologic diseases such as systemic lupus erythematosus, rheumatoid arthritis, HLA-B27–associated spondyloarthropathies, anti-neutrophil cytoplasmic antibody-associated vasculitis, Behçet disease, and sarcoidosis. The infectious etiologies for aortitis include tuberculosis (TB), syphilis, salmonella, staph, and streptococcus species. Amongst infectious etiologies, salmonella, staph and strept are most common [Citation1,Citation2]. It is essential to identify the type of aortitis as the infectious cause is directly associated with mortality [Citation1].
2. Case report
A 76-year-old male with a past medical history of type 2 diabetes mellitus, hypertension, and coronary artery disease status post coronary artery bypass graft three months prior presented to the emergency department with a chief complaint of abdominal pain. The abdominal pain started seven days prior, originating in the suprapubic region, spreading diffusely to all quadrants and lower back, described as crushing in nature, not associated with food intake, and not relieved or exacerbated by anything. The pain was associated with fever, chills, and night sweats for seven days. The patient also endorsed seven days of chest pain and denied any headache, blood in urine or stool, trauma to the abdomen, dysuria, nausea, vomiting, any recent travel or sick contacts. On admission, the patient had a temperature of 101 F, blood pressure of 100/60 mmHg, respiratory rate of 18/min and pulse of 100 beats per minute. The physical exam was positive for sternal erythema, swelling and tenderness with deep palpation over the manubrium, tenderness over the 2nd, 3rd and 4th costochondral junction and suprapubic tenderness with deep palpation, but no guarding and rigidity. Routine labs showed: WBC: 31000, Bands: 20, Segments: 90%. Serum chemistry was within normal limits. ESR of 100 mm/hr, CRP: 150 mg/L, Computed tomography of the abdomen showed perineural fibrosis of the aorta just above the ostium of the inferior mesenteric artery that is associated with gas in the area of fibrosis, which raised our suspicion of infectious aortitis. On the basis of clinical examination, ESR, CRP and CT findings, the vascular team was consulted, however, the patient refused to proceed with surgery. Blood cultures were sent and the patient was started empirically on 1 gram of IV Cefepime every 12 hours, 600 mg of Linezolid every 12 hours, 100 mg of metronidazole every 8 hours.
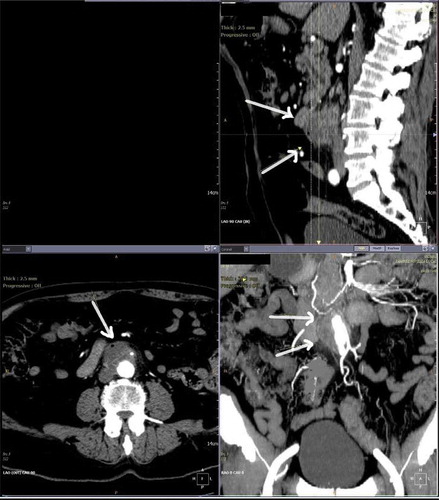
We suspected sternal osteomyelitis as an explanation for the patient’s chest pain. A subsequent bone scan was ordered and revealed increased uptake in the region of the manubrium and upper body of the sternum. (Appendix A) This was suspected to be secondary to chronic inflammatory changes associated with his prior sternotomy. CT angiogram showed peri aortitis with a small air bubble/locule of gas suggesting that this may be infectious etiology, thus confirming the diagnosis of aortitis [Appendix B]. The sternal biopsy was positive for osteomyelitis and blood cultures grew Salmonella Enteritidis. Antibiotics were switched to IV Ceftriaxone, and the patient was treated for six weeks inpatient. The patient responded positively to treatment with no further complications and remained asymptomatic and inflammatory markers normalized at 2 weeks follow up (ESR, CRP, and WBCs).
3. Discussion
Infectious aortitis requires specialized management different than non-infectious aortitis [Citation3]. The most common organisms involved in infectious aortitis are Salmonella, Staphylococcal species, and Streptococcus pneumonia [Citation2]. The proposed pathophysiology explaining infectious Aortitis is the hematogenous spread of micro-organisms to the vasa-vasorium of the blood vessel, which leads to the seeding of blood vessels [Citation4]. Infectious aortitis has a predisposition for blood vessels with preexisting underlying pathology such as atherosclerosis [Citation3].
Clinical presentation may vary from abdominal pain to cardiogenic or septic shock [Citation1]. Clinicians should have a high index of suspicion for aortitis, as timely recognition and treatment reduces morbidity and mortality [Citation1,Citation4]. Inflammation of the aorta can cause aortic dilation, resulting in aortic insufficiency [Citation4]. Furthermore, it can cause fibrous thickening and ostial stenosis of significant branches, resulting in reduced or absent pulses, low blood pressure in the arms and central hypertension due to renal artery stenosis [Citation3]. Depending on which other vessels are involved, ocular disturbances, neurological deficits, claudication, and other manifestations of vascular impairment may accompany this disorder [Citation3].
Salmonella aortitis carries very high mortality even with the available treatment options. Salmonella aortitis risk factors include; male sex, prior history of vascular pathologies, coronary artery disease, hypertension, diabetes, immunosuppression, long term steroids and immunosuppressive drug use, rheumatoid arthritis, rheumatological disease, and hematological malignancies [Citation5]. The standard of care for Infectious aortitis is surgical endovascular repair along with long-term antibiotics [Citation6]. Treatment with antibiotics alone is controversial [Citation1]. In a study by Soravia-Dunand et al. [Citation4], 10 patients with salmonella aortitis were reviewed from their databases including; antibiotic use, possible surgical procedure used, clinical outcome, and complications. From the 10 cases identified, 7 underwent a surgical procedure with antibiotic treatment and 3 just received antibiotic treatment. From the 7 that underwent surgery, only two survived greater than 3 months post-operatively. The surgeries used in these 10 cases were; axillofemoral graft, repair and in situ graft or just in situ graft placement. The two patients that survived surgery had an axillofemoral graft placement. The 3 patients that only received antibiotic treatment all died. In another case by Strahm et al. [Citation6], a resolution of the aortitis has been reported after EVAR and 12 months of antibiotic treatment. The correct surgery and duration of antibiotic use have yet to be determined. Some experts suggest lifelong therapy. In our case, the patient refused surgery and underwent antibiotic use only. Clinically and radiologically, the patient was in remission after 6 weeks of antibiotic coverage inpatient and remained asymptomatic at 2 weeks follow up (ESR, CRP, and WBCs).
Learning points
Aortitis is inflammation of the aorta with very high mortality and morbidity; prompt diagnosis is essential to ameliorate outcomes
Once aortitis is diagnosed, a proper surgical evaluation should be performed. Ideally, treatment would consist of both surgical intervention and long-term antibiotics.
Very few cases of aortitis have been successfully treated with antibiotics alone. If the patient declines surgery or Is not a surgical candidate, they should be treated with antibiotics and should be followed closely to prevent complications
Once aortitis is confirmed patient should be considered for endovascular surgery without delay.
Author contributions
All authors contributed to the work and approved the submission of this manuscript.
Informed consent
Informed consent was obtained from the patient for this case report.
Acknowledgments
We thank Dr. Patrick Michael (Program Director of the Internal Medicine Residency), Dr. Michael Agnelli (Associate Program Director of the Internal Medicine Residency), Dr. Monisha Singhal (Associate Program Director of the Internal Medicine Residency) and Dr. Robert Lahita (Chairman of the Department of Medicine) for their continuous support and guidance.
Disclosure statement
The authors declare that they have no conflicts of interest.
Additional information
Funding
References
- Gornik HL, Creager MA. Aortitis. Circulation. 2008;117(23):3039–3051.
- Molacek J, Treska V, Baxa J, et al. Acute conditions caused by infectious aortitis. Aorta (Stamford). 2014 Jun 1;2(3):93–99.
- Deipolyi AR, Czaplicki CD, Oklu R. Inflammatory and infectious aortic diseases. Cardiovasc Diagn Ther. 2018;8(Suppl1):S61–S70.
- Soravia-Dunand VA, Loo VG, Salit IE. Aortitis due to salmonella: report of 10 cases and comprehensive review of the literature. Clinl Infect Dis. 1999 August 15;29(4):862–868.
- Töpel I, Zorger N, Steinbauer M. Inflammatory diseases of the aorta: part 1: non-infectious aortitis. Gefasschirurgie. 2016;21(Suppl2):80–86.
- Strahm C, Lederer H, Schwarz EI, et al. Salmonella aortitis treated with endovascular aortic repair: a case report. J Med Case Rep. 2012;6:243.
Appendices
Appendix A.
Nuclear medicine imaging revealing enhanced activity at the sternum suspicious of inflammation.
Figure 1. Nuclear Medicine Imaging revealing enhanced activity at the sternum suspicious of inflammation

Appendix B.
CTA Aorta Runoff Angiogram: Peri aortitis with small air bubble/locule of gas suggesting that this may be an infectious etiology.