ABSTRACT
Mycoplasma pneumoniae is a common bacterial pathogen that causes atypical community-acquired pneumonia. Illness onset can be gradual and progressive over weeks. Patients typically have cough, pharyngitis, malaise, and tracheobronchitis. Although symptoms are frequently mild, the initial presentation can be severe with numerous complications. We present a case of a 28-year-old male who presented with 1 day of significant hemoptysis. He was intubated for airway protection and underwent bronchoscopy, which showed multiple blood clots in several lung lobes, consistent with diffuse alveolar hemorrhage (DAH). His workup was negative for pulmonary embolism, coagulopathy, and vasculitis. He tested positive for rhinovirus and mycoplasma pneumoniae IgM (negative IgG). He was ultimately discharged home with oral doxycycline to complete a 10-day course. DAH is a rare presentation and life-threatening complication of mycoplasma pneumonia. Although there is a reported association between DAH and rhinovirus, our patient improved with antibiotics making mycoplasma pneumoniae the likely culprit. When encountering hemoptysis or alveolar bleeding, clinicians should have low suspicion for atypical infections and start appropriate antibiotics early in the clinical course.
1. Introduction
Mycoplasma pneumoniae (M. pneumoniae) infection usually causes upper respiratory tract disease, but it is also the second most common cause of community-acquired pneumonia. Infection typically involves the trachea, bronchi, bronchioles, and peri-bronchial tissues and may extend to the alveoli and alveolar walls [Citation1]. Symptoms of M. pneumoniae pneumonia are typically milder than other bacterial pneumonias and include a non-productive cough, headache, fever, and malaise. Diagnosis can be made via PCR analysis of respiratory tract secretions with up to 90% sensitivity and 100% specificity [Citation2]. Appropriate antimicrobial treatment significantly shortens the duration of illness and M.pneumoniae pneumonia rarely causes death. However, extrapulmonary complications including hematologic manifestations, skin eruptions, and neurologic manifestations have been reported [Citation2].
We present a case of a 28-year-old male with 1 day of severe hemoptysis and positive mycoplasma pneumoniae testing. He was emergently intubated for airway protection and underwent bronchoscopy with findings consistent with diffuse alveolar hemorrhage. This case demonstrates a rare presentation and severe complication of mycoplasma pneumonia in a young immunocompetent patient.
2. Case Presentation
A 28-year-old wheelchair-bound man with cerebral palsy presented to the emergency department with 1 day of hemoptysis. The patient’s caretaker reported that the patient had an episode of intense coughing that was followed by expectoration of bright red blood. About a week prior, the patient had a mechanical fall onto his back while boarding a vehicle. At that time they did not seek medical care. The patient had no chest pain, dyspnea, fevers, chills, night sweats, nausea, hematemesis, or melena. Additionally, there was no recent travel outside their state of residence. The patient had a past medical history significant for cerebral palsy with a ventriculoperitoneal shunt for hydrocephalus. There was no family history of malignancy. He did not use tobacco products, drink alcohol, or use illicit drugs. He lived at home and was cared for solely by his mother. He was not prescribed any anticoagulants and did not use non-steroidal anti-inflammatory drugs (NSAIDs). He had never been incarcerated.
On presentation, the patient was afebrile, tachycardic, and saturating 95% on room air. He did not appear to be in respiratory distress. His pupils were equal, round, and reactive to light. Blood was noted in his oral cavity. His chest did not show signs of trauma and he had symmetric chest wall expansion with inspiration. Breath sounds were diminished on the right side, without wheezes or rales. The cardiovascular exam was unremarkable and the abdomen was soft, non-distended, non-tender, with no organomegaly, and bowel sounds were present. Radial pulses were present bilaterally and minimal edema was noted in both legs. The patient was awake and alert, and at baseline, he was fully oriented. Multiple neurological deficits were noted, all of which were unchanged from baseline. Chest x-ray showed diffuse mixed nodular and patchy opacities in the right middle and lower lung zones. Laboratory testing revealed hemoglobin of 12.9 g/dL, normal comprehensive chemistry panel, negative D-dimer, and normal PTT and prothrombin time. An initial CT angiogram of the chest (, row A) demonstrated no pulmonary embolism but revealed hazy opacities in the right upper and lower lobes.
Figure 1. (a) CT angiogram of the chest at the time of presentation showing right upper and lower lobe opacities. (b) 12 h repeat CT angiogram showing worsening of the opacities of right upper and lower lobes, with new left lower lobe opacity
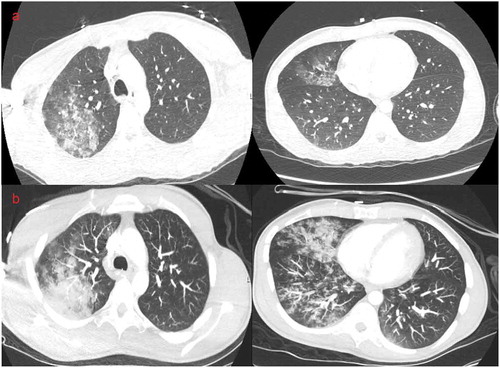
During his evaluation, the patient continued to have large volume hemoptysis, which consisted of more than 200cc of blood. Due to aspiration risk, he was subsequently intubated for airway protection and was admitted to the intensive care unit. A repeat CT angiogram of the chest (, row B) performed 12 hours after the initial study again demonstrated no pulmonary embolism, but showed interval progression of the opacities in both the right upper and lower lobes, as well as a new left lower lobe opacity. Emergent bronchoscopy was performed, which demonstrated dark-colored clotted blood in both lungs (right side greater than left side), with no active bleeding. Evaluation of the upper gastrointestinal tract at this time showed normal appearing esophagus and no signs of bleeding in the stomach, but the stomach contained swallowed blood.
Due to the patient’s rapid clinical decline, a broad workup was initiated including infectious and rheumatologic testing. Additional history revealed that during the week after the fall, both the patient and his mother experienced coughing. He was subsequently started on vancomycin, piperacillin/tazobactam, and azithromycin for empiric coverage of pulmonary infections. Blood cultures, sputum smear and cultures, respiratory viral panel, legionella antigen, and mycoplasma IgM/IgG were ordered. Additionally, antinuclear antibodies (ANA), perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA), antineutrophil cytoplasmic antibodies (c-ANCA), rheumatoid factor, and anti-glomerular basement membrane antibodies (anti-GBM) were ordered.
Overnight, he remained clinically stable on mechanical ventilation and continued to be afebrile. His hemoglobin dropped to 10.7 g/dL. Sputum smear showed no organisms and no acid-fast bacilli. Sputum and blood cultures showed no growth. Mycoplasma pneumoniae IgM was positive, with a negative IgG. Respiratory viral panel was positive for rhinovirus. Antibiotics were narrowed to IV doxycycline due to concern for macrolide resistance, and possible post-viral complication from staphylococcus aureus.
Rheumatoid factors, ANA, c-ANCA, p-ANCA, and anti-GBM, were all negative. He was monitored for 36 h after the initiation of antibiotics. Serial chest x-rays showed improvement of the right lung infiltrate. The amount of blood drained by endotracheal suctioning decreased to a trace amount. On hospital day 3, the patient was extubated to a nasal cannula and then transitioned to room air. He was transitioned to oral doxycycline 100 mg twice daily. He was transferred out of ICU and continued to be afebrile without hemoptysis or breathing difficulties. He was discharged home on hospital day 5 with a course of oral doxycycline to complete a total of 10 days.
3. Discussion
Diffuse alveolar hemorrhage, the extravasation of red blood cells into pulmonary alveolar spaces occurs in conjunction with many diseases. Symptoms range from fever, dyspnea, cough, and chest pain to severe life-threatening respiratory failure. One-third of patients will not have hemoptysis [Citation3].
The diagnosis should be suspected when a patient presents with hemoptysis, diffuse pulmonary infiltrates, anemia, and manifestations of systemic disease. Bronchoalveolar lavage showing progressively more blood with serial aspiration is considered diagnostic. Pulmonary infections are rarely associated with DAH, but an infectious workup must be considered given the treatment implications [Citation4].
Our patient underwent an extensive workup for hemoptysis; trauma, infection, coagulopathy, malignancy, and autoimmune causes were all considered. The mechanical fall raised initial concerns for a pulmonary contusion. Given that the patient was non-mobile, there was also a concern for pulmonary embolism. An infectious etiology was not suspected initially given a lack of fever and leukocytosis and was not considered until further history and additional work-up. Studies have shown that delay in the initiation of antibiotics is associated with the development of fulminant M. pneumoniae and that early recognition and treatment can be lifesaving [Citation5]. Because M. pneumoniae lacks a cell wall, it does not appear on gram stain and does not grow in routine cultures. Although Mycoplasma is known to cause hemolytic anemia, our patient’s clinical presentation was more consistent with an acute bleed given that his hemoglobin stabilized after hemostasis. Mycoplasma has also been reported to cause CNS infection [Citation6], which would be concerning as this patient had a VP shunt. However, our patient had no neurological changes and his mental status was at baseline prior to presentation and after extubation. Another complication of Mycoplasma infection is cold agglutinin cryogloblinemia, which can cause pulmonary hemorrhage [Citation7]. Although this complication was a possibility in our case, the lack of renal failure, a purpuric rash, or petechiae on the skin made it less likely [Citation4].
Mycoplasma pneumoniae is a frequent cause of atypical community-acquired pneumonia and infection in many cases is mild, and sometimes even asymptomatic. It is atypical for an immunocompetent 28-year-old male to have significant hemoptysis due to Mycoplasma pneumonia and then rapidly improve with antibiotics. DAH associated with M. pneumoniae is very rare; to our knowledge, there are only four other published cases [Citation8–11]. Our patient had a full recovery, similar to a prior case report involving a 24-year old woman [Citation11]. However, a 74-year old woman with comorbidities had many complications due to DAH including cardiac arrest and death [Citation8]. DAH has been reported with other pulmonary infections, such as rhinovirus [Citation12,Citation13], which our patient tested positive for, however, the rapid clinical improvement after the initiation of antibiotics suggests that Mycoplasma pneumoniae was the culprit rather than rhinovirus. Clinicians should be aware of the association between M. pneumoniae and DAH so that appropriate antibiotics can be started early to prevent disease progression and adverse outcomes.
Disclosure statement
All authors contributed to the drafting and editing of this manuscript and approve the submission of the final draft for publication.
The authors disclose no conflict of interest.
References
- Ryan KJ. Mycoplasma. In: Sherris medical microbiology [Internet]. New York, NY: McGraw-Hill Education; 2017. P. 7e.
- Jameson JL, Fauci AS, Kasper DL, et al. Mycoplasma pneumoniae, legionella species, and chlamydia pneumoniae. In: Harrison’s manual of medicine. New York, NY: McGraw-Hill Education; 2020. P. 20e.
- Benson A, Albert RK. Massive hemoptysis. In: Hall JB, Schmidt GA, Kress JP, editors. Principles of critical care. New York, NY: McGraw-Hill Education; 2015. P. 4e.
- Von Ranke FM, Zanetti G, Hochhegger B, et al. Infectious diseases causing diffuse alveolar hemorrhage in immunocompetent patients: a state-of-the-art review. Lung. 2013;191(1):9–18.
- Izumikawa K. Clinical features of severe or fatal mycoplasma pneumoniae pneumonia. Front Microbiol. 2016;7:800.
- Parrott GL, Kinjo T, Fujita J. A compendium for mycoplasma pneumoniae. Front Microbiol. 2016;7:513.
- Amital H, Rubinow A, Naparstek Y. Alveolar hemorrhage in cryoglobulinemia–an indicator of poor prognosis. Clin Exp Rheumatol. 2005;23(5):616–620.
- Mishra R, Cano E, Venkatram S, et al. An interesting case of mycoplasma pneumonia associated multisystem involvement and diffuse alveolar hemorrhage. Respir Med Case Rep. 2017;21:78–81.
- Patel K, Ali N, Nazir H, et al. Mycoplasma pneumonia as cause of acute respiratory distress syndrome (ARDS) and diffuse alveolar hemorrhage (DAH) requiring veno-venous extra corporeal membrane oxygenation (VV-ECMO). Chest. 2014;146(4):163A.
- Wang’ondu RW, Long T. An atypical case of hemoptysis. Conn Med. 2016 Mar;80(3):153–157.
- Choi N, Lederer P, Prieto-Centurion V, et al. Diffuse alveolar hemorrhage and acute respiratory distress syndrome secondary to mycoplasma pneumoniae infection in a young immunocompetent patient. Am Thorac Soc. 2016;A6998–A6998.
- Kane JR, Shenep JL, Krance RA, et al. Diffuse alveolar hemorrhage associated with mycoplasma hominis respiratory tract infection in a bone marrow transplant recipient. Chest. 1994 Jun;105(6):1891–1892.
- Grover K, Zainah H, Bhatnagar S, et al. A rare case of diffuse alveolar hemorrhage secondary to acute pulmonary histoplasmosis. Case Rep Infect Dis. 2015;2015:821749.
