ABSTRACT
A patient with recent thoracic outlet decompression surgery presented with acute dyspnea and was found by point-of-care ultrasound to have diaphragm dysfunction. This case highlights an unexpected cause of respiratory complaints in the outpatient setting discovered at the bedside, utilizing point-of-care ultrasound protocol.
1. Case
A 45-year-old female with history of Protein C deficiency and recent right thoracic outlet decompression surgery and first right first rib resection 3 weeks prior presented to an internal medicine clinic with dyspnea on exertion of one day duration. The patient was in good health up until 8 months before presentation when she developed recurrent transient ichemic attacks (TIAs). She underwent extensive evaluation at several hospitals and eventually was found to have thoracic outlet syndrome of the left upper extremity and possible thrombus at the subclavian artery. She successfully underwent left-sided thoracic outlet decompression and left first rib resection 7 months prior to presentation. Her post-op period was complicated by a subocclusive left external iliac deep vein thrombosis (DVT), and she was treated with apixaban. She recovered over the next several months and continued anticoagulation for her prior TIAsand DVT in the setting of Protein C deficiency. Two months prior to presentation, she developed right arm symptoms consistent with thoracic artery outlet syndrome on the contralateral side. She ultimately underwent thoracic outlet decompression surgery and right first rib resection 3 weeks prior to presentation, only missing full anticoagulation for 2 days. She was recovering as expected until she began to notice dyspnea on exertion 1 day prior to presentation.
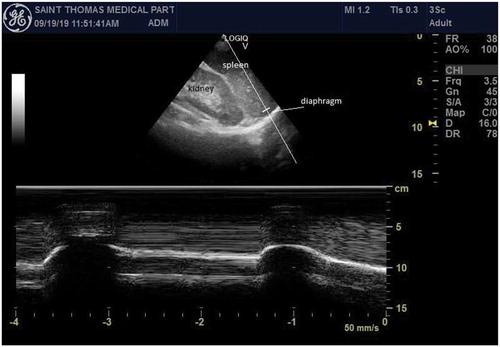
Her vitals were within normal limits. Her physical exam was notable for decreased breath sounds and dullness to percussion in the right lung base. To evaluate her complaints further, a Cardiac Limited Ultrasound Exam (CLUE) was performed with the phased array probe and revealed the right hemidiaphragm had decreased movement compared to the left hemidiaphragm with a normal CLUE exam otherwise ( and ; Supplement Videos 1 and 2) [Citation1].
Figure 1. Point-of-care ultrasound of the right hemi-diaphragm in the posterolateral axillary line at the level of the costophrenic angle. A phased array probe was used, and M-mode is utilized to show lack of excursion of the diaphragm during deep breaths
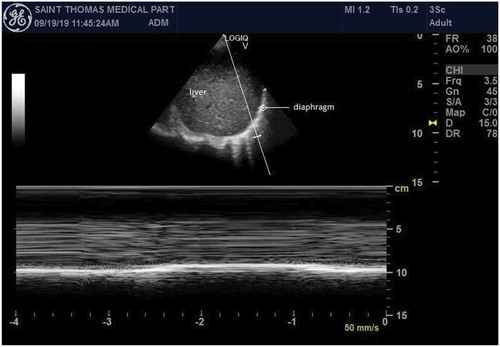
Figure 2. Point-of-care ultrasound of the left hemi-diaphragm in the posterolateral axillary line at the level of the costophrenic angle. A phased array probe is used, and M-mode shows normal excursion of the diaphragm during normal breaths
Labwork including troponin was normal, and electrocardigram revealed a new right bundle branch block but no evidence of ischemia. CT angiography of the chest was pursued due to her high risk of venous thromboembolism after surgery but did not show pulmonary embolism. It did confirm marked right hemidiaphragm elevation with associated compressive atelectasis. Sniff test confirmed abnormal motion during normal respiration of the right hemidiaphragm and abnormal paradoxical movement during sniff. She was diagnosed with postoperative unilateral diaphragm dysfunction that was initially found by point-of-care ultrasound during her clinic visit.
2. Discussion
Unilateral diaphragmatic paralysis or weakness following injury to the phrenic nerve results can be a rare complication after thoracic outlet surgery [Citation2,Citation3]. Patients with unilateral diaphragmatic dysfunction are usually asymptomatic at rest but may have exertional dyspnea and decreased exercise performance [Citation4]. Patients may also note a worsening in supine position [Citation5]. Workup of patients with diaphragm dysfunction may consist of chest radiographs, computed tomography, fluoroscopy, pulmonary function testing, phrenic nerve conduction studies, and transdiaphragmatic pressure measurements. These diagnostic tests have variable sensitivity and specificity, and some are invasive or uncomfortable examinations as well as expose patients to radiation [Citation4]. Point-of-care ultrasound is non-invasive and has been shown to have similar accuracy to most other modalities to evaluate for diaphragm dysfunction [Citation5–7]. For example, a prospective study of 82 patients with dyspnea referred to the EMG laboratory for evaluation of neuromuscular respiratory failure found ultrasound to be 93% sensitive and 100% specific for the diagnosis of neuromuscular diaphragmatic dysfunction [Citation7].
Diaphragm excursion is typically evaluated with the patient in the supine position in the following described views: the anterior subcostal view (transducer underneath the anterior costal margin at the mid-clavicular line), the posterior subcostal view (transducer at the posterior costal margin at the mid-clavicular line) and/or the subxiphoid view (transducer is in the subxiphoid region with the transducer directed cephalad) [Citation5]. The anterior subcostal view is preferred, and M-mode is utilized in this view to determine diaphragmatic excursion [Citation5].
This case was interesting because the diaphragm was evaluated using the posterolateral axillary line at the level of the costophrenic angle during the CLUE protocol. While the use of this view for evaluation of diaphragm dysfunction has not been studied, this view clearly showed a decreased excursion of the diaphragm and aided in the diagnosis. This view is used in protocols, such as CLUE, to evaluate respiratory complaints, and we believe it may also be valuable for evaluation of the diaphragm. Further study of this view and its use in evaluation of diaphragm excursion is warranted. This case is also reported because diagnosing diaphragm dysfunction using point-of-care ultrasound protocol in ambulatory patients presenting with respiratory complaints has not been published to our knowledge.
Supplemental Material
Download Zip (2.2 MB)Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Kimura BJ, Shaw DJ, Amundson SA, et al. Cardiac limited ultrasound examination techniques to augment the bedside cardiac physical examination. J Ultrasound Med. 2015 Sep;34(9):1683–1690. Epub 2015 Aug 12. PMID: 26269293.
- Kothari MJ. Unilateral diaphragmatic paralysis following thoracic outlet surgery: a case report. Electromyogr Clin Neurophysiol. 2004 Sep;44(6):375–378. PMID: 15473351.
- Heine MF, Asher EF, Roy TM, et al. Phrenic nerve injury following scalenectomy in a patient with thoracic outlet obstruction. J Clin Anesth. 1995 Feb;7(1):75–79. PMID: 7772364. DOI:10.1016/0952-8180(94)00021-u
- Hart N, Nickol AH, Cramer D, et al. Effect of severe isolated unilateral and bilateral diaphragm weakness on exercise performance. Am J Respir Crit Care Med. 2002 May 1;165(9):1265–1270. PMID: 11991876.
- Sarwal A, Walker FO, Cartwright MS. Neuromuscular ultrasound for evaluation of the diaphragm. Muscle Nerve. 2013 Mar;47(3):319–329. Epub 2013 Feb 4. PMID: 23382111; PMCID: PMC3581727.
- Houston JG, Fleet M, Cowan MD, et al. Comparison of ultrasound with fluoroscopy in the assessment of suspected hemidiaphragmatic movement abnormality. Clin Radiol. 1995 Feb;50(2):95–98. PMID: 7867276.
- Boon AJ, Sekiguchi H, Harper CJ, et al. Sensitivity and specificity of diagnostic ultrasound in the diagnosis of phrenic neuropathy. Neurology. 2014 Sep 30;83(14):1264–1270. Epub 2014 Aug 27. PMID: 25165390; PMCID: PMC4180486.
