ABSTRACT
Background: Despite enthusiasm for inpatient ward redesign, coordinated models require high effort with uncertain return on investment.
Objective: We aimed to reduce mortality and achieve a benchmark of zero preventable deaths by committing to an interprofessional model, including partnered nurse-physician unit leadership, geographic localization, and structured interdisciplinary bedside rounds (SIBR).
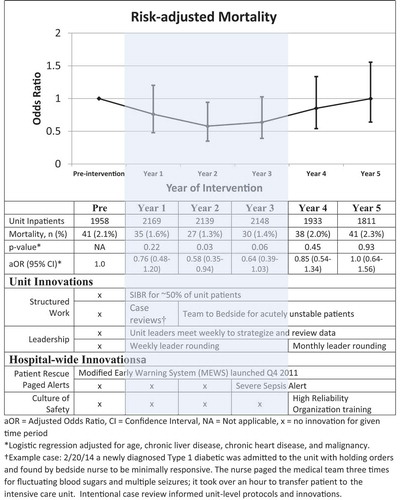
Methods: An observational pre-post design with 5-year follow-up studied the transition of a medical unit to an Accountable Care Unit (ACU). This geographic model enables partnered nurse-physician leadership and patient-centered workflows, including daily interdisciplinary bedside rounds. Potentially additive or confounding hospital-wide safety initiatives were tracked. Yearly mortality was compared using multivariable logistic regression and reported as odds ratio (OR). For the pre-specified goal of no preventable deaths, we report unexpected deaths, defined as those occurring without documentation of comfort as the goal of care.
Results: 12,158 inpatients (55.1% female, mean [sd] age 62.2 [19.7]) were observed over 6 years. Reduction in the risk-adjusted mortality was observed following ACU implementation, with Year 2 significantly lower than the pre-implementation year (adjusted odds ratio [aOR] = 0.58 [0.35–0.94]). Risk-adjusted mortality was similar in Year 3 (aOR = 0.64 [0.39–1.0]) but returned to baseline for Years 4 and 5. Unexpected deaths reached zero in Year 3 and plateaued in Years 4 and 5 at a rate below pre-implementation year (~0.1% vs. 0.38%).
Conclusions: A geographic ACU with nurse-physician partnered leadership and daily structured interdisciplinary bedside rounds can reduce total and unexpected mortality. However, maintenance requires constant effort and, in the real world, multiple confounders complicate study.
1. Introduction
Geographic localization and interdisciplinary team rounding are appealing yet require significant investment without guaranteed returns. Preparatory work, continued surveillance, and participant orientation are required from hospital administration, bed control, nursing, hospitalists, graduate medical education, pharmacy, and care management. Time and energy must be committed for interdisciplinary bedside rounds as well as unit leadership meetings. Coordinated models may improve patient experience, physician-staff communication, patient safety [Citation1,Citation2] and length of stay [Citation3]. However, these inter-professional designs, which vary in intensity and resources, have not gained universal provider acceptance nor consistently achieved robust clinical outcomes on general medical wards [Citation4,Citation5].
Despite patient, provider, and trainee enthusiasm for coordinated interdisciplinary models, many units experience ‘growing pains’ and scale back innovations after initial implementation [Citation6,Citation7]. Change or added complexity in hospital design without stakeholder buy-in or meaningful improvement may unintentionally compound waste. A path forward requires identifying interventions where the effort achieves authentic benefits. We committed to geographic localization and structured interdisciplinary bedside rounds for 5 years with strong nurse-physician leadership. We aimed to reduce mortality and achieve a benchmark of zero preventable deaths.
2. Materials and methods
On 26 August 2013, a single 29-bed medical unit transitioned to a geographic model designed as an Accountable Care Unit (ACU) [Citation8] with nurse-physician partnered leadership and daily (365 days/year) Structured Interdisciplinary Bedside Rounds (SIBR), including a quality-safety checklist. Dedicated nurse care managers and pharmacists rounded with the team Monday through Friday while the patient, patient contact, bedside nurse, physician team, and charge nurse rounded daily. Approximately half of the unit’s patients were assigned to a geographic physician team with SIBR. We used an observational pre-post design comparing risk-adjusted inpatient mortality before and for 5 years after model implementation.
Key safety workflows and their timeline of implementation are shown (). A physician medical director and/or nurse unit manager rounded with the multidisciplinary team weekly for Years 1–3, supporting SIBR, emphasizing key safety messages, and promoting multidisciplinary communication. This leader rounding shifted to monthly in Years 4–5. The physician medical director and nurse unit manager regularly assessed key measures, collected feedback on barriers, solicited improvement suggestions, and modified workflows.
Figure 1. Risk-adjusted yearly inpatient mortality odds-ratio versus pre-intervention for 5 years on an accountable care unit. Shaded area denotes the period of most intensive unit-level innovation and corresponding risk-adjusted mortality reduction
During the first 6 months, multidisciplinary review of patient safety events led to development of safety messages including a ‘Team to Bedside’ protocol for acutely deteriorating patients. A ‘Team to Bedside’ prompt resulted in immediate in-person assessment from both the physician and nurse. The protocol ended with a clear explanation and appropriate orders, engagement of the rapid response team, or escalation to a higher level of care. In Years 4–5, hospital-wide initiatives to improve patient safety were launched, such as a severe sepsis alert and High Reliability Organization training for all employees.
Unit data were obtained from the electronic medical record database for inpatient encounters 1 year pre- and 5 years post-implementation. No data were missing. Yearly in-unit mortality was compared using multivariable logistic regression, adjusted for age and comorbidities, and reported as odds ratio. For the pre-specified goal of no preventable deaths, we also report unexpected deaths, defined as those occurring without documentation of comfort as the goal of care. A computer query for comfort care orders was supplemented by physician review.
This study, protocol number STUDY2017000168, was granted full approval by the Providence Health and Services Institutional Review Board.
3. Results
Over 6 years 12,158 inpatients (55.1% female, mean [sd] age 62.2 [19.7]) were discharged from the ACU. No inpatients were excluded. Compared to pre-implementation year, mortality, crude or risk-adjusted, showed decline in Years 1, 2 and 3, reaching statistical significance in Year 2 (risk-adjusted odds ratio [aOR] = 0.58 [0.35–0.94]). Mortality rebounded to baseline over Years 4 and 5 (). The unit innovations ‘Team to bedside for acutely unstable patients’ and ‘Weekly leader rounding’ were associated with the lowest mortality Years 1–3. The hospital-wide innovations of ‘Severe sepsis alert’ and ‘Highly Reliable Organization’ training were not associated with mortality reductions on our unit. Unexpected mortality declined to zero in Year 3 and plateaued at a level below that of the pre-intervention year (). Because of the small number of unexpected deaths, no further risk-adjustment was attempted.
4. Discussion
Despite enthusiasm for inpatient ward redesign, coordinated models require high effort with uncertain return on investment. This study showed mortality reduction 2 years after the implementation of an ACU with a return to baseline by Year 5. A systematic review of interdisciplinary team care interventions on general medical wards found mortality reduction in only 1 of 15 studies, and the benefit did not persist beyond 6 months. The author highlights that team practices as opposed to the specific interdisciplinary team composition appeared most influential on mortality [Citation4]. As unit medical co-directors, we posit that the ACU may be beneficial in reducing mortality, but only with intense focus, weekly leadership presence, and constant unit-level case review, collaboration, and innovation. Hospital-wide efforts, also well-intentioned and also aimed at mortality reduction, inevitably compete for the limited resource of innovation energy among both leaders and caregivers. In fact, early success on the ACU led hospital executives to request our help in spreading the model, diluting our focus on the original unit and making study challenging by modifying workflows on what would have been a natural comparator unit. We hypothesize that gains achieved through a strong culture of collaboration and innovation are highly sensitive to local leadership and maintained enthusiasm.
Unexpected deaths reached the zero benchmark at Year 3 and remained below baseline. Authentic unit ownership and accountability for cohesive patient-centered care plans likely contributed, along with excellent nurse-physician rapport and a shared expectation that any acutely unstable patient would be seen by the entire team immediately. On a busy internal medicine ward, not all deaths are preventable; however, we noted that scheduled daily bedside rounding helped the team ensure patient and family understanding of their illness, which in turn may have facilitated earlier appropriate transition to comfort care. Despite the rebound in the overall mortality by Years 4 and 5, reduction in unanticipated deaths was sustained. The pre-specified and concrete goal of ‘zero unexpected deaths’ helped the team maintain focus and purpose in the face of change and challenges.
This study has limitations. The nonrandomized design is subject to confounding by other workflow changes and patient selection. Our care delivery model was implemented on a teaching service, which may not be generalizable to other settings. Randomized trials of care delivery models would be ideal; however, their scope and complexity may impede completion. We join Stein’s call [Citation8] for studies to highlight the specific practices or initiatives at local versus systemic levels that achieve clinically meaningful outcomes.
A geographic ACU with nurse-physician partnered leadership and daily structured interdisciplinary bedside rounds can reduce total and unexpected mortality. We theorize that sustained commitment by local leadership to unit-based culture and protocols is one key to maintained improvement.
List of abbreviations
Acknowledgments
Michael Goldstein, MD. Tanisha Perry, RN.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- O’Leary KJ, Haviley C, Slade ME, et al. Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit. J Hosp Med. 2011;6(2):88–93. .
- Williams A, DeMott C, Whicker S, et al. The impact of resident geographic rounding on rapid responses. J Gen Intern Med. 2019;34(7):1077–1078. .
- Kara A, Johnson CS, Nicley A, et al. Redesigning inpatient care: testing the effectiveness of an accountable care team model. J Hosp Med. 2015;10(12):773–779. .
- Pannick S, Davis R, Ashrafian H, et al. Effects of interdisciplinary team care interventions on general medical wards: a systematic review. JAMA Intern Med. 2015;175(8):1288–1298. .
- Reeves S, Pelone F, Harrison R, et al. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;6:CD000072.
- Kara A, Johnson CS, Hui SL, et al. Hospital-based clinicians’ perceptions of geographic cohorting: identifying opportunities for improvement. Am J Med Qual. 2018;33(3):303–312. .
- Pannick S, Wachter RM, Vincent C, et al. Rethinking medical ward quality. BMJ. 2016;355:i5417.
- Stein J, Shapiro S. Web exclusives. annals for hospitalists inpatient notes – modernizing rounds-why it’s time to redesign our hospital practice. Ann Intern Med. 2018;168(2):HO2–HO3.