ABSTRACT
Sump syndrome – a collection of digested food, debris, stones, bile, and bacteria in a poorly drained, bile duct reservoir – occurs most commonly after a side-to-side choledochoduodenostomy. As choledochoduodenostomies are now less common, sump syndrome is more often characterized as a complication of Roux-en-Y hepaticojejunostomies; however, most cases occur at the hepaticojejunostomy anastomosis. We report a rare case of sump syndrome in the intra-pancreatic remnant common bile duct in a patient with primary sclerosing cholangitis following living donor liver transplant via Roux-en-Y hepaticojejunostomy. Our patient had a history of end-stage liver disease secondary to primary sclerosing cholangitis but presented with recurrent bacteremia and symptoms of acute cholangitis following her transplant. While this complication has not been reported in this population, we know that those with primary sclerosing cholangitis and those undergoing liver transplantation are at very high risk for biliary complications and strictures. Liver transplant is currently our only treatment for primary sclerosing cholangitis, and more than any other group, they are referred for living donor liver transplantation, preferably via Roux-en-Y hepaticojejunostomy. Thus, our patient’s clinical scenario is not uncommon and demonstrates a source of serious infection of which providers must be aware.
1. Introduction
Sump syndrome was initially described as digested food, debris, stones, bile, and/or bacteria accumulating in a poorly drained distal common bile duct (CBD) in patients undergoing choledochoduodenostomy[Citation1]. The presenting symptoms of sump syndrome include indigestion, abdominal pain, nausea, vomiting, postprandial discomfort, and jaundice[Citation1]. With the decline of choledochoduodenostomies in favor of endoscopic retrograde cholangiopancreatography (ERCP), sump syndrome is less prevalent and is now described mainly as a complication following Roux-en-Y hepaticojejunostomy for benign biliary disease[Citation2]. Biliary complications following a living donor liver transplant are common, but sump syndrome has yet to be described in the literature. We present a case of sump syndrome in a patient with living donor liver transplantation for primary sclerosing cholangitis (PSC).
2. Case presentation
A 38-year-old woman with a history of cirrhosis secondary to PSC status post-living donor liver transplantation 4 years prior with a Roux-en-Y hepaticojejunostomy presented with abdominal pain, fever, and recurrent Klebsiella pneumoniae bacteremia. Three months earlier, she was treated for K. pneumoniae bacteremia without an identified source. She had presented with fevers to 38.4°C and sharp right upper quadrant pain. Her transaminases, bilirubin, and alkaline phosphatase were mildly elevated at admission in the setting of a transient lapse in immunosuppression. A magnetic resonance cholangiopancreatography demonstrated trace intrahepatic dilation, which was unchanged from prior imaging, and edema with surrounding infiltration at the intra-pancreatic CBD remnant. Intervention at this time was deferred and transaminase levels decreased when immunosuppression was restarted. She was discharged on sulfamethoxazole-trimethoprim.
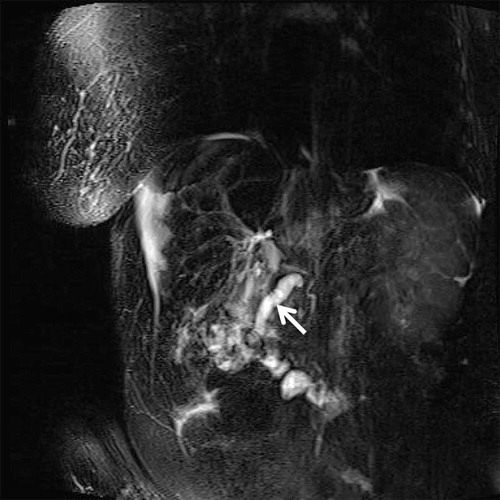
The patient returned 11 weeks later with sharp epigastric and right upper quadrant pain associated with emesis, fevers, chills, and poor appetite. Vital signs were normal. Transaminases and bilirubin were within the normal range, and repeat imaging was significant for persistent edema of the remnant CBD and increased diameter of the proximal segment of the remnant CBD (). An ERCP was performed and demonstrated a single 5 mm stenosis which was successfully dilated and swept with a balloon, expelling copious pus. Following the ERCP, a single balloon enteroscope was advanced to the hepaticojejunostomy site. The anastomosis was evaluated, and there were no strictures or signs of infection.
Figure 1. Magnetic resonance cholangiopancreatography
Following successful sphincterotomy and clearance of the remnant CBD, the patient’s abdominal pain resolved. She remained afebrile with normal liver function tests but was again discharged on sulfamethoxazole-trimethoprim to prevent recurrence. In a follow-up five months later, our patient remains without recurrence of infection at her remnant duct or further signs of sump syndrome.
3. Discussion
The prevalence of living donor liver transplantation is increasing, and biliary complication rates occur in 10–30% of the cases, with the two most common complications being anastomotic strictures and bile leaks[Citation3]. Additionally, PSC patients more often have biliary complications following liver transplants than others; however, PSC patients are still referred for living donor liver transplantation more than any other patient population[Citation4]. In transplants done for PSC, Roux-en-Y hepaticojejunostomy is usually performed in order to mitigate biliary complications or disease recurrence, but a remnant CBD is left within the head of the pancreas (). This distal remnant becomes a ‘sump,’ which is discontinuous from, and no longer drains the contents of the intrahepatic biliary tree. This poorly draining duct is prone to accumulating debris with loss of filling pressure and peristalsis. In our patient, her symptoms were resolved following sphincterotomy and stricture dilation.
Figure 2. Patient anatomy with CBD stricture
The case is unique and distinct from complications such as anastomotic strictures and non-anastomotic strictures, which can occur in the conjoined extra- or intrahepatic biliary system following living donor liver transplantation. Anastomotic strictures are usually associated with technical issues such as bile duct size mismatch, and non-anastomotic strictures can occur because of bile duct injury from ischemia or immune-mediated processes[Citation5]. Furthermore, anastomotic and non-anastomotic strictures are largely diagnosed through abnormal liver function tests (LFTs) because clinical presentations range from no symptoms to overt cholangitis [Citation6,Citation7]. Thus, infection in the remnant duct requires a high index of suspicion as liver enzymes are not elevated due to the lack of continuity with the biliary tree. As a result, treatment requires targeting the ERCP to the ‘default’ usual destination, i.e., the ampulla in the duodenum, rather than the destination that is typically targeted in post-transplant patients with a hepaticojejunostomy type biliary anastomosis, the hepaticojejunostomy site itself.
The clinical benefit from this case comes from recognizing the presence of sump syndrome in a patient with normal LFTs and performing ERCP at the correct location. Essentially, it is recognizing the intra-pancreatic remnant CBD as a possible nidus for infection. To our knowledge, we present the first case of sump syndrome in PSC and in a living donor liver transplant recipient. Sump syndrome has been reported in Roux-en-Y hepaticojejunostomy; however, this refers to cholangitis at the hepaticojejunostomy secondary to refluxing contents in the roux-limb. There is only one other case of infection documented at this location, which described a rare case of a fistula forming between this remnant portion of the bile duct and the patient’s jejunum, a very different scenario [Citation8]. While this can become a source of infection in any patient following Roux-en-Y hepaticojejunostomy, PSC patients will be even further predisposed as their native ducts are at high risk for ongoing strictures which likely caused an obstruction in our patient. This unique location along with the normal LFTs led our team to miss this source of infection during our patient’s first admission, and it was not until it became more obvious on repeat imaging, that we realized the intrapancreatic remnant duct needed to be drained. We hope this case will prevent a delay in similar patients’ care as postponed therapy can have dire results.
Authors’ Contribution
Gordon Robbins: Conceptualization, Data Curation, Project Administration, Writing – Review and Editing, Revision. Justin Brilliant: Data Curation, Writing – Original draft preparation and Revision. Yuting Huang: Visualization, Writing – Original draft preparation and Revision. Jonah Rubin: Conceptualization, Writing – Review and Editing. Eric Goldberg: Supervision, Writing – Review and Editing. Zurabi Lominadze: Supervision, Writing – Review and Editing and Revision.
Every author involved meets inclusion criteria as recommended by the International Committee of Medical Journal Editors. All authors have approved the final draft submitted.
Informed Consent:
Verbal patient consent was obtained for publication of the case details on 9 June 2020.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Abraham H, Thomas S, Srivastava A. Sump syndrome: a rare long-term complication of choledochoduodenostomy. Case Rep Gastroenterol. 2017;11:428–433.
- Marangoni G, Ali A, Faraj W, et al. Clinical features and treatment of sump syndrome following hepaticojejunostomy. Hepatobiliary Pancreat Dis Int. 2011;10(3):261–264.
- Chok KSH, Lo CM. Biliary complications in right lobe living donor liver transplantation. Hepatol Int. 2016;10:553–558.
- Shamsaeefar A, Shafiee M, Nikeghbalian S, et al. Biliary reconstruction in liver transplant patients with primary sclerosing cholangitis, duct-to-duct or Roux-en-Y? Clin Transplant. 2017;31(6):e12964. 10.1111/ctr.12964.
- Roos FJM, Poley J-W, Polak WG, et al. Biliary complications after liver transplantation; recent developments in etiology, diagnosis and endoscopic treatment. Best Pract Res Clin Gastroenterol. 2017;31(2):227–235.
- Tsujino T, Isayama H, Kogure H, et al. Endoscopic management of biliary strictures after living donor liver transplantation. Clin J Gastroenterol. 2017;10(4):297–311.
- Rao HB, Prakash A, Sudhindran S, et al.Biliary strictures complicating living donor liver transplantation: problems, novel insights and solutions. World J Gastroenterol. 2018;24(19):2061.
- Eshkenazy R, Inbal Y, Azoulay D. A new cause of cholangitis following Roux-en-Y hepaticojejunostomy. Gastroenterology. 2020;159:S0016-5085(20)30130–X.
