ABSTRACT
Background: Actinic keratosis (AK) is characterized by the occurrence of thick and scaly skin areas caused by damage from ultraviolet radiation. The management of AK aims to reduce lesions and prevent their recurrence by regular monitoring. French guidelines, last updated in 2009, reflect European guidelines for the management of face and scalp AK. However, they do not address all current, available options.
Objective: To assess the management of face and scalp AK in French clinical practice.
Methods: A two-part online questionnaire comprising a survey among French dermatologists and an analysis of patient medical records was performed to describe AK patients treated with topical therapy, patients’ profiles, and characteristics of the affected lesion areas.
Results: Decisions for topical treatments for face and scalp AK made by dermatologists were mainly driven by the lesion size. According to the last 10 patients they have seen, dermatologists were prescribing physical therapy in 53% of the cases, a combination of topical and physical therapy in 27% and topical only in 20%. Patient records revealed the average surface area targeted for treatment was 139 ± 113cm2.
Conclusions: Discrepancies between the guidelines on the treatment of face and scalp AK and clinical practice exist. Further research may help to standardize the treatment.
Introduction
Actinic keratosis (AK), also known as solar keratosis, is a disease characterized by the occurrence of thick, scaly, or crusty areas on the skin caused by damage from exposure to ultraviolet (UV) radiation [Citation1]. Its prevalence rises with age with a peek between the ages of 70 and 80 [Citation2]. AK is considered potentially pre-cancerous and when left untreated, may transform into squamous cell skin cancer [Citation3]. Diagnosing AK takes more than 10% of overall visits to dermatologists, making it one of the most common conditions seen in the outpatient setting [Citation4]. In France, AK of the face and scalp is a fairly common condition affecting up to 2.7 million people [Citation5].
According to the guidelines for the diagnosis and treatment of cutaneous squamous cell carcinoma and precursor lesions, the guidelines for the treatment of AK of the International League of Dermatological Societies in cooperation with the European Dermatology Forum, and the guidelines of Haute Autorité de Santé (HAS), the management of AK aims to reduce lesions and to prevent their recurrence by regular monitoring after treatment [Citation5–Citation8]. The standard treatment for AK is based on cryotherapy especially in cases with single or few skin lesions.
As an alternative, photodynamic therapy (PDT) either with red light or daylight, may be used particularly for the treatment of multiple lesions of the face and balding scalp, which are the predominant locations of lesions.
PDT with methyl aminolevulinate is recommended among others, as a first-line active photosensitizer. Yet, it is the only one currently available in France [Citation2,Citation5]. With multiple lesions, the second-line therapy is the use of topical treatments including fluorouracil, imiquimod, ingenol mebutate, and diclofenac [Citation5]. For patients presenting with multiple AKs, treatment is often targeted to the area of cancerization and the decision for specific treatment is determined by the size of this field and patient characteristics [Citation8].
In France, the most recent guidelines on the treatment of AK were published in 2009 [Citation6] and are in line with the European guidelines [Citation5,Citation7]. However, they do not address all currently available treatment options as like as methyl aminolevulinate recommended as a first-line treatment and ingenol mebutate, fluorouracil, and imiquimod as a second-line treatment. In order to have a clearer understanding of the treatment recommendations for AKs, these guidelines must be updated according to the French health technology assessment organization: HAS (Haute Authorité de Santé) to evaluate the latest treatment options.
French recommendations for first-line treatment options for face and scalp lesions are cryotherapy in case of few lesions and PDT with methyl aminolevulinate for the treatment of multiple lesions [Citation2,Citation6,Citation9,Citation10]. As second-line therapy options, local application of diclofenac, imiquimod, ingenol mebutate, or fluorouracil (5-FU) are recommended [Citation2,Citation6,Citation9].
Little is known about the treatment of AK in French clinical practice. To the authors’ knowledge, no study has been conducted to assess whether the management of AK is in line with French recommendations. Also, the profile of AK patients and their management regarding lesion characteristics has not been explored.
The objective of this study was to evaluate the management of AK provided by dermatologists in clinical practice. Additionally, the study aimed to describe the population of patients with face and scalp AK treated with topical therapy and to characterize their skin lesions.
Methodology
Study design
This study consisted of a two-part online questionnaire for dermatologists working in France and treating patients with AK. The survey was conducted between the 12th and 19th of October 2018 and data were collected online.
The first part of the questionnaire addressed clinical practice and was conducted to collect information on treatment preferences in the management of multiple AK from the dermatologist perspective.
The second part of the questionnaire aimed to collect data on current clinical practice within the study population from patient medical records.
Study populations
On the 120 dermatologists who were randomly selected from a representative panel of dermatologists in France (Onekey database) [Citation11], 40 accepted to participate. Dermatologists working in a hospital setting were excluded because AK is almost exclusively treated in outpatient clinics. Enrolled dermatologists were asked to answer questions on the treatment of AK.
Also, dermatologists were asked to identify their last five patients with multiple AKs of the face and scalp treated with topical therapies. The following data were extracted from the medical records: patient profile, characteristics of lesions, and prescribed treatment.
Questionnaire
A 2-section multiple-choice online questionnaire was developed for this survey.
In the first section, dermatologists were asked to describe their clinical practice in the management of face and scalp AK and provide information on the mean number of patients seen monthly, the overall proportion of AK patients and this with AK of the face and scalp, the type of treatment, topical treatment prescribed by area, first- and second-line treatment, the rationale behind treatment choices, areas treated per one pack of prescribed medication, and their definition of cancerization zone. The questionnaire addressing clinical practice is presented in the supplementary materials.
In the second part of the questionnaire, dermatologists were asked to perform a chart abstraction (based on the standardized questionnaire) for the last five patients that met inclusion criteria.
The questionnaire allowed collecting information on patients’ age, sex, last visit date, time from onset for each lesion, history of transplantation, and lesion location. The dermatologists were asked to determine the specific face and scalp location of lesioned areas (e.g., chin or cheek) in total and this targeted for treatment. The surface of the area treated was expressed as the percentage of the lesioned area in relation to the area of the specific location of the lesion. For example, if a lesion subjected to treatment was located on the chin, the percentage of the surface of the chin under treatment was reported. Additionally, the dermatologists collected information on the treatment prescribed at the last consultation and treatments used previously.
Statistical analysis
The population was weighted by the number of patients treated by each dermatologist to ensure better representativeness of the results.
Differences in topical treatments in terms of reasons for selecting a given therapeutic option and the usual size of the area treated per pack were compared. Student test was used to compare the topical treatments 2 by 2 according to the item response. The threshold for significance was set at p = 0.1.
The average size of the lesion area targeted for treatment was converted to square centimeter using the following standardized surface conversions reported by Calzavara-Pinton et al. [Citation8]: scalp: 200cm2, forehead: 150cm2, cheek: 100 cm2, and chin, ear, and nose: 25cm2 each.
Results
Survey of dermatologists’ general practice
Dermatologists reported that they consulted an average of 56 AK patients per month, which represents 19% of the total number of patients seen monthly. Among AK patients, 78% (n = 43) had face and/or scalp AK, which accounted for 15% of the total number of patients.
The most commonly reported treatments prescribed for face and/or scalp AKs were physical therapies in 53% of cases and the combination of physical and topical treatments in 27% of cases, while topical treatments alone were used in 20% of cases.
Most dermatologists (61%) declared that they usually prescribe topical treatments when the patient has 5 or more face and/or scalp AKs, while 31% prescribe it when the patient has at least 10 AKs and 8% when there are less than 5 AKs.
The most frequently reported first-choice topical treatment of face and/or scalp AKs was ingenol mebutate (60%), followed by methyl aminolevulinate daylight PDT (13%), imiquimod (13%), fluorouracil (13%), and diclofenac (2%).
As a second-choice topical treatment, methyl aminolevulinate daylight PDT was the most commonly reported treatment (32%), followed by imiquimod (25%), fluorouracil (17%), ingenol mebutate (15%), and methyl aminolevulinate red light PDT (10%).
Overall, ingenol mebutate was the most commonly reported topical treatment used (75%) followed by methyl aminolevulinate daylight PDT (45%). Diclofenac was reported as the first-choice topical treatment by only one dermatologist. First and second-choice treatment for face and/or scalp AKs details are depicted in Figure S1.
The most commonly reported reasons for prescribing ingenol mebutate were its short-term use (90%), its capacity to treat AK lesions (83%), and its efficacy (67%) (Figure S2). For methyl aminolevulinate daylight PDT, the reasons included its capacity to treat AK lesions (72%), its short-term use (67%), and its suitability to the lesion location (67%) (Figure S2). The short-term use was significantly more often reported as a reason for choosing ingenol mebutate than other treatments. The good tolerability of methyl aminolevulinate daylight PDT was also often reported as a reason for prescription compared to other treatments (Figure S2).
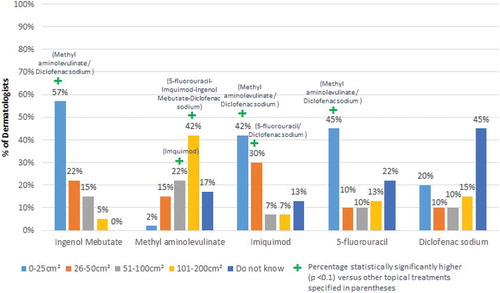
Methyl aminolevulinate PDTday light and red light were identified as the treatment preferred for the largest AK lesion areas (42% for 101–200cm2), while imiquimod, fluorouracil, and ingenol mebutate were generally used to treat smaller areas ranging from 0cm2 to 25cm2 (42%, 45%, and 57%, respectively). In respect to diclofenac, 45% of dermatologists reported that they do not know which surface area it is used for ().
Survey of patients’ record extraction by physician
AK patient profiles
A sample of 202 AK patients for whom a topical treatment was prescribed for face and/or scalp AKs at their last visit were included in the study. Two dermatologists selected six patients instead of five to be included in the analysis. The average time between data collection and the last visit was 7 weeks with standard deviation of 67.7 days. The average age of multiple actinic keratosis lesions of face and scalp currently treated was 4 years and 11 months.
Most of AK patients were men (80%) and the average age was 74 ± 9.64 years. The mean duration of face and/or scalp AK lesions was 4 years and 11 months with standard deviation of 65.15 months. Overall, 95% of patients were immunocompetent and 5% received an organ transplant.
Lesion locations and size
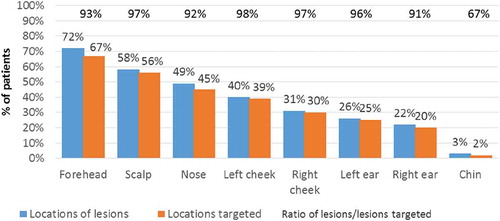
At the last visit, most lesions reported were located on the forehead (73%), scalp (64%), and nose (45%). Not all lesions were targeted for treatment. The ratio of lesions to lesions targeted for treatment ranged from 66% to 98% ().
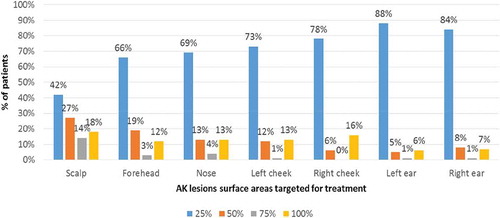
The majority of dermatologists reported treating only 25% of the surface of each targeted lesion of the scalp, forehead nose, both cheeks, and both ears. However, the results were more heterogeneous for the forehead ().
The average surface area of the lesion targeted for treatment was 139 ± 113cm2. It was less than 25cm2 in 8% of cases, between 25cm2 and 50cm2 in 15% of cases, between 50cm2 and 100cm2 in 26% of cases, and above 100cm2 in 50% of cases.
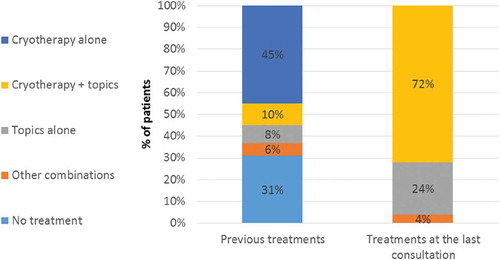
Treatment pattern
In almost 70% of cases, the lesion surface was previously treated (). The treatments used were mostly cryotherapy alone (65%), a combination of cryotherapy and topical treatments (14%), topical treatment alone (11%), surgery (6%), and others (1%). The most prescribed topical treatments were ingenol mebutate (64%), fluorouracil (29%), methyl aminolevulinate daylight PDT (20%), imiquimod (14%), methyl aminolevulinate red light PDT (6%), and diclofenac (2%).
At the last visit, the dermatologist prescribed only topical treatments (as per inclusion criteria). Seventy-two percent (72%) of patients received a topical treatment combined with cryotherapy, 24% received a topical treatment alone, and 4% received other combinations. Ingenol mebutate was the most commonly prescribed topical treatment (43%), followed by fluorouracil (20%), and methyl aminolevulinate daylight PDT (14%).
Cryotherapy was mostly used in combination with ingenol mebutate (33%), followed by fluorouracil (13%), methyl aminolevulinate daylight PDT (10%), and imiquimod (9%).
Discussion
To the authors’ knowledge, this is the first study which provides details on the management of face and scalp AK in the French population including the location and size of lesions as well as describes the topical therapies used for the treatment and the rationale behind the prescription.
The present study has several limitations. First, as the survey was related to the selection of the 5 last seen patients, this process is known to over-represent the patients that may have more than one visit, therefore, may be more difficult to treat. It is believed that this would be not critical for the study population as face and/or scalp AK patients are seen regularly, which is considered independent of the size and number of lesions.
The weighted results adjustment of the study population ensures a better external validity of the results. These results might be extrapolated based on the dermatologists’ selection of the patients. The exclusion of hospital-only based dermatologists was reasonable for this study as patients with AK are rarely hospitalized.
The survey revealed inconsistency in the indication of the lesion surface but showed a high correlation between the treatment used and the actual practice based on the patients’ chart.
The key feature of this study is that 202 patients were included, which is a robust sample size to characterize AK lesions.
The study showed that most of AK lesions were located on the forehead, scalp, and nose. However, only 25% of these lesioned areas were targeted for treatment during the last visit to the dermatologist. The mean surface of the area targeted for treatment was 139 ± 113 cm2. Only 8% of AK patients had the surface targeted for treatment of 25cm2 or less. This raises the question of the adequacy of some products (imiquimod, fluorouracil, and ingenol mebutate) which should be used to treat a maximum threshold of surface areas of 25cm2 according to their summary of product characteristics (SmPC), in the treatment of areas of >25cm2. However, when asked, most of the dermatologists identified that they can use imiquimod, fluorouracil, and ingenol mebutate to treat less than 25cm2 AK lesion areas and methyl aminolevulinate PDT to treat greater lesions. But in practice, the market shares and the usage pattern of imiquimod, fluorouracil, and ingenol mebutate in clinical practice clearly support their usage in the treatment of surface areas greater than 25cm2.
This study suggests data gaps between the management of AK patients in the real-life practice and the clinical guidelines. Cryotherapy is recommended as the first-line treatment for AK in dermatological practice according to the guidelines, but the results indicated that 31% of patients received a topical treatment as a first-line therapy (). Considering that contraindications to cryosurgery are very rare, the findings suggest that cryotherapy may be underused conversely to recommendations from the guidelines.
Due to the small sample size of dermatologists participating in this study, some of the French regions were not represented (e.g., Normandy, Center, and Corsica). Nevertheless, gender distribution within the respondents was representative of all dermatologists (3,109 dermatologists). Sixty-eight percent (68%) were women and 32% were men within the respondents; however, overall, 70% were women and 30% were men. Regardless of the limitations, this study brings exclusive information related to the location and size of lesions as well as the prescribed treatments for face and/or scalp AK patients.
The use of first-line topical therapy in France does not follow the guidelines, as more than 60% of first-line therapies are being used off label. This result is consistent with the market share of topical treatments in France which are dominated by second-line therapies, suggesting their higher use as first-line therapies.
Regarding the rationale for prescription, the efficacy was not considered as a differentiating factor. The key drivers were the size of lesions to be treated, treatment duration, tolerability, and compliance with the use of conventional red light PDT red light.
The prescription of different treatments according to the size of lesions is very interesting especially as methyl aminolevulinate PDT happens to be widely channeled to patients with larger surfaces to treat. Therefore, this may suggest a higher volume of products used per patient and eventually higher costs. Yet, it might be the opposite as methyl aminolevulinate PDT is recommended for large size lesions due to its packaging which could be cheaper for the patients.
Conclusion
Overall, dermatologists appear to be aware of their practice but with the exception towards the size of the lesion they treat. It is interesting to notice that guidelines and HAS recommendations were not followed, especially for first- and second-line treatments. There is a need to develop new guidelines integrating all the knowledge and the most recent opinions of HAS. The current practice ignores the limit of SmPCs recommendations on the size of the lesions to be treated. Thus, the level of off-label use is quite common. Furthermore, it is noticeable that size of the lesion is driving the choice of the product, which is likely due to the package size of the product. This has induced a channeling for the indication towards methyl aminolevulinate PDT is often chosen and, which happens to be used in patients with the largest lesions to be treated sub-optimally, suggesting that higher volumes may be needed when using other products.
This is the first study addressing the size of lesions and the therapies in relation to other multiple criteria. Further studies using multivariate analysis to assess drivers for prescription of treatments in AK patients are recommended. Replication studies on a larger sample would also be highly informative.
Supplemental Material
Download MS Word (1.3 MB)Acknowledgments
The authors would like to acknowledge Monique Dabbous and Nawel Jaafar for their contribution to editing the final manuscript.
Disclosure statement
This article was funded by Galderma. Dr Jacques Savary and Marie Christelle Tine are employees of Galderma. Julie Dorey and Anne-Caroline Weber are employees of Creativ-Ceutical, who received funding from Galderma. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in, or financial conflict with, the subject matter or materials discussed in the manuscript. No writing assistance was used in the production of this manuscript.
Supplementary material
supplemental data for this article can be accessed here.
Additional information
Funding
References
- Poulin Y, Lynde CW, Barber K, et al. Non-melanoma skin cancer in Canada chapter 3: management of actinic keratoses. J Cutan Med Surg. 2015;19(3):227–7.
- HAS. Transparency committee opinion: METVIXIA 168 mg. 2014.
- Quaedvlieg PJ, Tirsi E, Thissen MR, et al. Actinic keratosis: how to differentiate the good from the bad ones? Eur J Dermatol. 2006;16(4):335–339.
- Bickers DR, Lim HW, Margolis D, et al. The burden of skin diseases: 2004 a joint project of the American academy of dermatology association and the society for investigative dermatology. J Am Acad Dermatol. 2006;55(3):490–500.
- HAS. Transparency committee opinion: METVIXIA 168 mg. 2017.
- Dermatologie Sfd. [Guidelines for the diagnosis and treatment of cutaneous squamous cell carcinoma and precursor lesions. Guidelines]. Revue de stomatologie et de chirurgie maxillo-faciale. 2010;111(4):228–237.
- Werner RN, Stockfleth E, Connolly SM, et al. Evidence- and consensus-based (S3) guidelines for the treatment of actinic keratosis - International League of Dermatological Societies in cooperation with the European Dermatology Forum - short version. J Eur Acad Dermatol Venereol. 2015;29(11):2069–2079.
- Calzavara-Pinton P, Haedersdal M, Barber K, et al. Structured expert consensus on actinic keratosis: treatment algorithm focusing on daylight PDT. J Cutan Med Surg. 2017;21(Suppl. 1):3S-16S. 1203475417702994.
- HAS. Avis de la Commission de la Transparence Ameluz. 2016.
- Girard C, Adamski H, Basset-Seguin N, et al. [Procedure for daylight methyl aminolevulinate photodynamic therapy to treat actinic keratoses]. Annales de dermatologie et de venereologie. 2016;143(4):257–263.
- Database O. OneKey Santé database – IQVIA. [cited 2019 Mar 21]. Available from: https://www.smartdataforlead.com/fichiers-prospection-btob/fichier-prospection-medicale-onekey/