ABSTRACT
Background: Pain management in emergency departments is a complex objective. The absence of a care pathway or a high level of activity complicates diagnostic or analgesic therapeutic strategies. Medical innovation can impact both individual practices and the functioning of an emergency department.
Objective: We then wanted to understand how medico-economic studies on pain were carried out in an emergency department.
Study design: We reviewed the literature of the last 20 years (between 1998 and 2018).
Setting: Of 846 titles screened, a total of 268 abstracts qualified for further screening, and 578 titles were excluded. A total of 14 studies qualified for inclusion in the review. Studies on medico-economics in an emergency department are very diverse. None of the methods used are identical; the studies differ in their very nature (prospective, retrospective, cost-effectiveness, etc.) and the determination of emergency room costs differs according to the part of the world studied. In addition, organizational impact is rarely measured, although it is an essential dimension for choosing or not a medical innovation.
Introduction
Emergency departments play an important role in the functioning of hospitals, but also as first contact care providers. This is a priority reception place for unscheduled activity. The activity is not only important but is constantly increasing.
The need for care of patients in emergency departments combined with the economic context requires hospitals to make rapid decisions and to optimize the use of material and human resources. The objective is to maintain the fluidity of the patient’s journey without compromising the quality of care.
An emergency department is very diverse, with serious cases as well as benign ambulatory medicine. Pain calls for the involvement of all categories of consultants: in an emergency room, 60% of patients experience acute pain. This leads to waiting times for a number of patients, which can be very long before they receive an analgesic treatment, when they are not prioritized. For 85% of them, pain is the main reason for seeking medical care [Citation1]. Chest pain is a frequently non-specific symptom that raises the problem of its varied etiology and potential severity.
Pain management is then a key quality indicator of organizational relevance in emergencies. The absence of a care system and too high a level of activity complicate diagnostic or analgesic therapeutic strategies. The introduction of a medical innovation gives hope for a positive impact both on individual practices and on the organizational level [Citation2].
The objective of our work is to review the literature on medico-economic studies conducted on the theme of therapeutic management or pain diagnosis in an emergency department.
Methods
A targeted literature review was conducted to assess medico-economic studies of pain in an emergency department
The MEDLINE database was searched for English-language studies using search terms related to ‘program evaluation’, ‘cost’, ‘emergency’ and ‘pain’.
The medline equation was: (‘Program Evaluation’[Mesh] OR ‘Costs and Cost Analysis’[Mesh] OR Cost OR ‘Healthcare Financing’[Mesh] OR ‘Economics’[Mesh]) AND (‘Emergency Service, Hospital’[Mesh] OR ‘Emergency Medical Services’[Mesh] OR emergency) AND (‘Pain’[Mesh] OR ‘Pain Management’[Mesh])
The search was limited to the following: studies published from 1998 to 2018 to capture the most up-to-date studies; in the English language; related to the economic evaluation of pain in a medical emergency department; and peer-reviewed journals. The bibliography of reviewed articles identified as part of this search was further screened for relevant articles not identified in the original search.
The resulting titles and abstracts were screened methodically and exported to Microsoft excel for an additional review. An article was retrieved for full review when its abstract met each of the including criteria. Articles were excluded from full review when its abstract met any of the following criteria: the study does not report economic study, case series, editorial or commentary.
From full-text reviews, study details including ‘country’, ‘type of study’, ‘population’ size’, ‘method’, ‘costs evaluation’ and ‘results’ were extracted.
Results
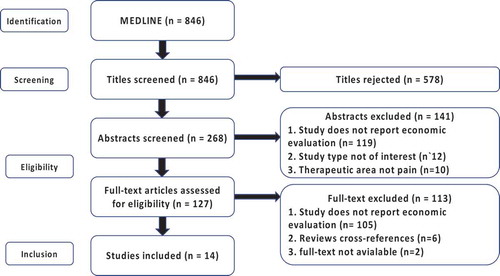
Medical-economic studies on pain treatment in an emergency department are few and heterogenous. Of 846 titles screened, a total of 268 abstracts qualified for further screening, and 578 titles were excluded. A total of 14 studies qualified for inclusion in the review.
A flow chart summarizing the study selection and inclusion is reported in .
The specific characteristics of each of the fourteen studies are summarized in .
Table 1. Specific characteristics of the fourteen studies.
The publications identified are based on two major themes in emergency departments: the assessment of diagnostic costs in the context of chest pain and the drug based analgesic strategy
Assessment of diagnostic costs in the context of chest pain
This first theme is over-represented in the literature since it is a field with a high economic stake in terms of the necessary investments.
Chest pain is one of the most frequent causes of emergency room visits. These are managed and usually classified into three categories: low, medium or high risk.
Eight million patients per year in the United States are treated by emergency departments for these pains compatible with cardiac ischemia. When investigated by non-invasive imaging, only 30% of them suffer from coronary artery disease, resulting in $10 billion in overly cautious spending.
In a 2015 study, these figures are explained by Culled et al. [Citation3]: the 67.2% of patients with non-heart chest pain each incur $3,331 in expenses. Much work has therefore focused on improving diagnostic techniques that can be used to send patients home who do not need care as quickly as possible.
Coronary computed tomography angiography (CCTA) allows coronary artery disease to be excluded quickly and non-invasively. The ROMICAT study is being launched, among other things, to ensure that this method does not increase costs compared to conventional techniques [Citation4]. This 2013 study is innovative in that it uses a sophisticated cost calculation calculator that is, according to Hulten et al., more accurate than a simple approach based on Medicare reimbursement values. It shows that the CCTA could have reduced total hospital costs by 23%.
CCTA is a less traumatic method than Coronary angiography, the conventional method.
This study is formative in two ways, since it shows that a single parameter can produce radically different results, if you take the time to study it. Indeed, when stenosis increases to more than 50%. As a result, the costs increase so much that the use of CCTA is ultimately more expensive than the traditional method.
CCTA is less traumatic than the reference method of invasive coronary angiography, but is nephrotoxic and has X-ray toxicity.
The more expensive BPCA contrast agents have a higher molecular weight, so they are less nephrotoxic [Citation5]. Espinosa et al. attract our attention because it brings a progress in the medico-economic approach. In addition to the cost studied traditionally, it focuses on cost-effectiveness through an indicator: QALY which is an indicator to estimate the value of life (a healthy year of life corresponds to a QALY score of 1).
Not surprisingly, this method, although more expensive to purchase, is more cost-effective than conventional CCTA because it results in less toxicity.
Another alternative method to CCTA in the diagnosis of chest pain without evidence ischemia on ECG is single-photon emission computed tomography (SPECT) with technetium-99m. This method is considered more discriminatory than CCTA, resulting in lower costs and fewer adverse effects.
To evaluate this method from an economic point of view, Stowers et al. and Wong et al. took an interest in it.
American study shows a lower median cost of $1843 with SPECT compared to the conventional protocol and a median length of stay of 2 days [Citation6].
Wong et al. show a saving of $566 (at the current Singapore dollar rate) and a reduced stay of 2.9 days [Citation7].
These two studies, carried out 10 years apart and on two different continents, show similar results but are sufficiently different to question the relevance of cost-effectiveness studies because they depend on many factors: the population studied, the diagnostic protocol, the statistical method, the data processing or the different sources of cost documentation (literature, patient invoice, health insurance data).
Another difficulty for conducting medico-economic studies in emergency departments is the diversity of possible questions, almost as important as the number of existing protocols.
In the management of chest pain, we have seen CCTA, CCTA with BPCA and SPECT. To continue in the exhaustiveness, Wyrick et al. armed with computer software took an interest in contrast echocardiography (CCE) [Citation8]. This method showed a good negative predictive value compared to the usual method, saving as much as $900 per patient.
In the same vein and with the same calculator, Priest et al., an American-Australian collective, wanted to compare multiple diagnostic strategies: stress ECG, stress echocardiography with stress or pharmacological, SPECT, CCTA alone and confirmed CCTA with SPECT [Citation9].
CCTA strategies are less expensive than other strategies and the one combining SPECT also increases the patients’ QALY indicator. Indeed, with a reduction in re-hospitalization due to false positives, patients have a more pleasant life.
We have previously seen that certain biases, such as the existence of thrombosis or stenosis, could modify the results of studies. In this context, Peitz et al. have shown the significant increase in the costs associated with a high body mass index in the management of chest pain and dyspnea in emergency departments [Citation10].
The questioning of scientific work must therefore remain a rule and as many parameters as possible must be included in future medical and economic considerations in order to discriminate as much as possible against biases.
After constant improvement in the ‘ultratechnological’ diagnostic methods of patients with chest pain, the latest international recommendations are moving towards the use of simple risk scores. Nieuwets et al. have studied two of them: the predictive score of the degree of thrombosis in myocardial infarction (TIMI) and the HEART score (History, ECG, Age, Risk factors and Troponin) [Citation11].
The use of these simple scores would save almost €80,000 out of 680 patients by discriminating against low-risk patients.
With regard to the international recommendations, Cakir et al. urge us to comply with them. Indeed, in this study, savings seems possible of up to $10 per patient treated in the emergency room for chest pain, simply by respecting some of the profitability rules dictated in the guidelines [Citation12].
Drug analgesic strategy in emergency medicine
Pain in pre-hospital emergencies is an infrequent topic of study due to a lack of education of health care staff, fear of adverse effects due to opiates and the fact that analgesia is costly in terms of resources. Hubert et al. tried to demonstrate that the work overload related to analgesia could lead SMUR teams to abandon it [Citation13]. Recording two useful scores to measure workload: the CCMS (Classification Clinique des Malades du SMUR) and the SECSISMUR (Système d’Evaluation de la Charge en SoIns du SMUR) they showed that under analgesic, the duration of medical treatment is identical with an increase in workload and its intensity. This is a proposed reason for oligoanalgesia rooted in the mentalities of pre-hospital emergency teams: The time lost for analgesia would represent, at the end of the day, missed interventions.
Casamayor et al., using guidelines from five European countries, estimate the costs associated with the management of IV morphine by an emergency room nurse [Citation14]. These costs include the cost of morphine, labor time, equipment, cost of adverse events, administration complications, including treatment costs, labor time and equipment for them.
This study is indicative of the distribution of costs since it shows that 73% are attributable to adverse events and complications and that the remaining three quarters are due to nurses’ working time, while the cost of morphine is very low.
Conducting a medico-economic study solely on the price of a drug therefore does not seem relevant.
A good way to save on labour costs related to the administration of drugs and morphine, in particular, could be the use of Patient Controlled Analgesia (PCA). Its clinical advantages are no longer to be demonstrated in the treatment of post-operative pain, which is why the idea of using PCA in emergency departments appeared, with scores comparable to intermittent IV boluses. Doleman et al. and Pritchard et al. compare PCA to standard treatment by studying not only the pain experienced but also the cost necessary to avoid moderate to severe pain [Citation15,Citation16]. Taking into account the different costs, PCA is about twice as expensive as conventional morphine administration.
Discussion
Studies on medico-economics in an emergency department are very diverse. It is important to be cautious about their results. Indeed, none of the methods used are identical, the nature of the studies differs in their very nature (prospective, retrospective, cost-effectiveness, etc.) and the determination of emergency department costs differs according to the part of the world studied. The publications identified in our study focus on two main areas: the assessment of diagnostic costs in the context of chest pain and the drug analgesic strategy.
For cost-effectiveness or cost-usefulness evaluations as presented above, the bulk of the costs studied are direct costs.
However, for the medico-economic evaluation of a therapeutic innovation in the field of acute pain management, quality indicators should be taken into account, in addition to direct costs. When measuring quality, the six quality dimensions defined by The Institute of Medicine should be appraised. Haugland et al. [Citation17] argue that this multidimensional approach to quality measurement seems particularly reasonable for services with a highly heterogenic patient population and complex operational contexts, like emergency medical services:
Patient satisfaction:/patient centeredness
Safety
Effectiveness
Efficiency
Equity
Timeliness
In addition, emergency services face, more or less frequently, peaks in activity and experience steady growth in their activity, requiring a highly structured organization likely to adapt to situations of high tension. The organizational variability of emergency departments, the variability in the typology of patients, the disparity in activity according to time of day, day, week or season associated with the complexity of the funding model make any non-systemic medico-economic study extremely delicate.
In view of these ways of operating an emergency service, the organizational impact should also be taken into account. To date, this dimension has not yet been assessed. The possible organizational impact of an innovation could be addressed from the perspective of the internal and external consequences of the organization.
Conclusion
In the field of pain management in an emergency department, the evaluation of diagnostic or therapeutic innovations is currently conducted on the basis of clinical and medico-economic studies. However, the implementation of an analgesic patient management strategy in an emergency department is a complex decision-making process that requires taking into account other dimensions such as organizational impact. New multi-criteria systemic methodologies must be proposed for new assessments.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Cordell WH, Keene KK, Giles BK, et al. The high prevalence of pain in emergency medical care. Am J Emerg Med. 2002;20:165–7.
- Coffey F, Wright J, Hartshorn S, et al. STOP!: a randomised, double-blind, placebo-controlled study of the efficacy and safety of methoxyflurane for the treatment of acute pain. Emerg Med J. 2014;31:613–618.
- Cullen L, Greenslade J, Merollini K, et al. Cost and outcomes of assessing patients with chest pain in an Australian emergency department. Med J Aust. 2015;202(8):427–432.
- Hulten E, Goehler A, Bittencourt MS, et al. Cost and resource utilization associated with use of computed tomography to evaluate chest pain in the emergency department: the Rule Out Myocardial Infarction using Computer Assisted Tomography (ROMICAT) study. Circ Cardiovasc Qual Outcomes. 2013;6(5):514–524.
- Espinosa G, Annapragada A. Cost-effectiveness of a novel blood-pool contrast agent in the setting of chest pain evaluation in an emergency department. Am J Roentgenol. 2013;2014:710–719.
- Stowers SA, Eisenstein EL, Wackers FJ, et al. An economic analysis of an aggressive diagnostic strategy with single photon emission computed tomography myocardial perfusion imaging and early exercise stress testing in emergency department patients who present with chest pain but nondiagnostic electrocardiograms: results from a randomized trial. Ann Emerg Med. 2000;35:17–25.
- Wong RC, Sinha AK, Mahadevan M, et al. Diagnostic utility, safety, and cost-effectiveness of emergency department-initiated early scheduled technetium-99m single photon emission computed tomography imaging followed by expedited outpatient cardiac clinic visits in acute chest pain syndromes. Emerg Radiol. 2010;17:375–380.
- Wyrick JJ, Kalvaitis S, McConnell KJ, et al. Cost-efficiency of myocardial contrast echocardiography in patients presenting to the emergency department with chest pain of suspected cardiac origin and a nondiagnostic electrocardiogram. Am J Cardiol. 2008;102:649–652.
- Priest VL, Scuffham PA, Hachamovitch R, et al. Cost-effectiveness of coronary computed tomography and cardiac stress imaging in the emergency department: a decision analytic model comparing diagnostic strategies for chest pain in patients at low risk of acute coronary syndromes. JACC Cardiovasc Imaging. 2011;4(5):549–556.
- Peitz GW, Troyer J, Jones AE, et al. Association of body mass index with increased cost of care and length of stay for emergency department patients with chest pain and dyspnea. Circulation Cardiovasc Qual Outcomes. 2014;7(2):292–298.
- Nieuwets A, Poldervaart JM, Reitsma JB, et al. Medical consumption compared for TIMI and HEART score in chest pain patients at the emergency department: a retrospective cost analysis. Br Med J. 2016;6:e010694.
- Cakir Z, Saritas A, Aslan S, et al. Acute nontraumatic chest pain in emergency department and cost-effectiveness evaluation. Eurasian J Med. 2008;40(3):119–123.
- Hubert H, Guinhouya C, Ricard-Hibon A, et al. Prehospital pain treatment: an economic productivity factor in emergency medicine? J Eval Clin Pract. 2009;15:152–157.
- Casamayor M, Didonato K, Hennebert M, et al. Administration of intravenous morphine for acute pain in the emergency department inflicts an economic burden in Europe. Drugs Context. 2018;7:212524.
- Doleman B, Williams JP. Patient controlled analgesia: effective and cost-effective management of acute pain within the emergency Department? Anaesthesia. 2017;72(8):935–939.
- Pritchard C, Smith JE, Creanor S, et al. PASTIES writing group. The cost‐effectiveness of patient‐controlled analgesia vs. standard care in patients presenting to the Emergency Department in pain, who are subsequently admitted to hospital. Anaesthesia. 2017;72(8):953–960.
- Haugland H, Rehn M, Klepstad P, et al.,EQUIPE-collaboration group. Developing quality indicators for physician- staffed emergency medical services: a consensus process. Scand J Trauma Resusc Emerg Med. 2017 Feb 15;25(1):14. DOI:10.1186/s13049-017-0362-4