ABSTRACT
Background/Objective: This study evaluated emergency department (ED) visit trends, subsequent inpatient admissions for patients with inflammatory bowel disease (IBD) diagnosis and IBD-related abdominal pain (AP), and hospital-level variation in inpatient admission rates in the USA (US).
Methods: This population-based, cross-sectional study included data from Nationwide Emergency Department Sample (NEDS, 2006─2013) database. Patients ≥18 years of age with primary ED diagnosis of IBD/IBD-related AP were included. Variables included demographics, insurance information, household income, Quan-Charlson comorbidity score, ED discharge disposition, and length of hospital stay (2006, 2010, and 2013). Variation between hospitals using risk-adjusted admission ratio was estimated.
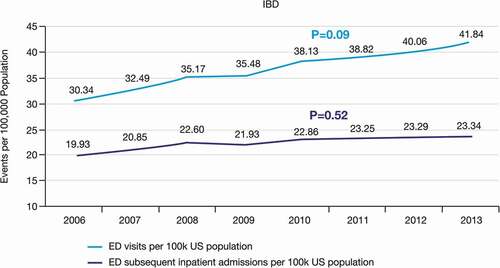
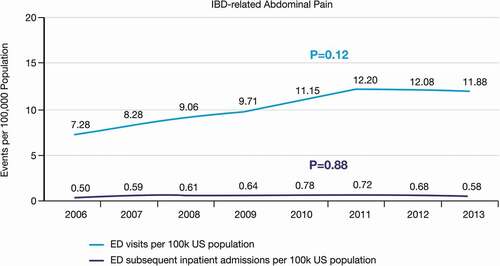
Results: Annual ED visits for IBD/100,000 US population increased (30 in 2006 vs 42 in 2013, p = 0.09), subsequent admissions remained stable (20 in 2006 vs 23 in 2013, p = 0.52). ED visits for IBD-related AP increased by 71% (7 in 2006 vs 12 in 2013; p = 0.12), subsequent admissions were stable (0.50 in 2006 vs 0.58 in 2013; p = 0.88). Proportion of patients with subsequent hospitalization decreased (IBD: 65.7% to 55.7%; IBD-related AP: 6.9% to 4.9%). Variation in subsequent inpatient admissions was 1.42 (IBD) and 1.96 (IBD-related AP).
Conclusions: An increase in annual ED visits was observed for patients with IBD and IBD-related AP; however, subsequent inpatient admission rate remained stable.
Introduction
According to a 2019 estimate from the Centers for Disease Control (CDC), approximately 1.3 million patients suffer from Inflammatory Bowel Disease (IBD) in the USA (US) [Citation1]. Emergency department (ED) visits for patients with IBD are quite common and contribute to approximately 0.09% of all ED visits in the US, about 109,392 annually [Citation2,Citation3].
Overall treatment costs for patients with IBD are 3-fold higher than for similar patients without IBD [Citation4]. Although healthcare utilization varies significantly across the globe owing to differences in sociodemographic characteristics and availability of healthcare facilities, studies have demonstrated that the overall treatment costs for IBD are 2–4 times higher in the US as compared with other Western countries [Citation5,Citation6]. The healthcare costs due to ED visits for IBD have also tripled in the US in <10 years ($194,773,824 in 2006 to 598,961,532 USD in 2014) [Citation7,Citation8].
Studies have shown a linear increase in ED visits for patients with IBD, however; the proportion of subsequent hospitalization in patients with IBD has decreased overtime [Citation2,Citation3]. This phenomenon has been driven by accessing alternative outpatient pathways, such as observation care and expedited clinic follow up for patients presenting to the ED with non-specific symptoms [Citation9,Citation10]. Abdominal pain (AP) is an early manifestation of inflammation and 50–70% patients with IBD experience AP during initial onset of an IBD flare [Citation11]. Non-specific AP has also been ranked as the second most common reason for ED visits among all adults in the US and the most common reason for ED visits among patients with IBD [Citation3,Citation11].
Lack of standardized treatment algorithms for IBD contributes to varied decision-making for the treatment of patients with IBD presenting to the ED with AP. Approximately 40% of patients with IBD are hospitalized and most physicians believe that IBD-related hospitalizations occur due to ineffective disease management in the outpatient setting [Citation12,Citation13]. Optimizing treatment practices requires an understanding of the overall ED and hospitalization utilization pattern in patients with IBD.
Data illustrating national trends in the US population for ED visits and subsequent inpatient admissions among patients with IBD and especially in patients with IBD-related AP are scarce. The objective of the current study was to investigate trends in ED visits and subsequent inpatient admissions for patients with IBD and IBD-related AP. The study further evaluated ED encounters by patient characteristics and examined hospital-level variation in inpatient admission rates from the ED.
Methods
Data source
We obtained data from the Nationwide Emergency Department Sample (NEDS), the largest all-payer ED database in the US. NEDS is a Health Insurance Portability and Accountability Act compliant, statistically certified database sponsored by the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality (http://www.hcup-us.ahrq.gov/). NEDS comprises >30 million ED visits of patients from >900 hospitals representing roughly 20% of hospital-based ED data across the US. The database contains information regarding geographical region of ED visit, hospital and patient characteristics, and the nature of visits. It also contains the ED charge information for 87% of ED visits, regardless of the payer. NEDS promotes comparative studies of healthcare services, healthcare policy, and research across various areas including the use of and charges for ED services, medical treatment effectiveness, quality of ED care, impact of health policy changes, access to care, and utilization of health services by special populations.
According to the available data, NEDS contained 135 million ED visit related data in the year 2013. Data records available in NEDS are de-identified for public use and are protected through data use agreements. Therefore, analysis and publication by obtaining information from NEDS is exempt from institutional review board review.
Study design and study population
This US population-based cross-sectional study investigated ED visits and subsequent inpatient admissions among patients with IBD or IBD-related AP between Jan 2006 and Dec 2013.
We included patients of either sex, who were ≥18 years of age with a primary ED discharge diagnosis of IBD according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM codes for Crohn’s Disease [CD]: 555.0, 555.1, 555.2, 555.9 and Ulcerative Colitis [UC]: 556.0, 556.1, 556.2, 556.3, 556.4, 556.5, 556.6, 556.8, 556.9). ICD-10 codes were not part of the NEDS dataset during the study time period.
We identified patients with IBD-related AP by a primary diagnosis of AP (ICD-9-CM: 789.0) and secondary diagnosis (DX2-DX15) of IBD (ICD-9-CM codes for CD and UC mentioned above), similar to previous studies [Citation14,Citation15]. In addition, we excluded patients if they had a secondary discharge diagnoses (DX2-DX15) of non-IBD outcomes that could have also correlated with a complaint of AP, including gall bladder disorders (ICD-9-CM: 575), cholelithiasis (ICD-9-CM: 574), acute and subacute necrosis of liver (ICD-9-CM: 570), chronic liver disease and cirrhosis (ICD-9-CM: 571), liver abscess and sequelae of chronic liver disease (ICD-9-CM: 572), other disorders of liver (ICD-9-CM: 573), other disorders of biliary tract (ICD-9-CM: 576), diseases of pancreas (ICD-9-CM: 577), gastrointestinal hemorrhage (ICD-9-CM: 578), appendicitis (ICD-9-CM: 540–543), hernia of abdominal cavity (ICD-9-CM: 550–553), intestinal obstruction without mention of hernia (ICD-9-CM: 560), diverticula of intestine (ICD-9-CM: 562), peritonitis and retroperitoneal infections (ICD-9-CM: 567), diseases of esophagus (ICD-9-CM: 530), gastric ulcer (ICD-9-CM: 531), duodenal ulcer (ICD-9-CM: 532), peptic ulcer site unspecified (ICD-9-CM: 533), gastrojejunal ulcer (ICD-9-CM: 534), gastritis and duodenitis (ICD-9-CM: 535), disorders of function of stomach (ICD-9-CM: 536), and complications of bariatric procedures (ICD-9-CM: 539).
Outcome measures
We collected demographic characteristics including age, sex, insurance information, household income, Quan-Charlson comorbidities index (CCI) score defined by all secondary discharge diagnoses, ED discharge disposition, and length of hospital stay (LOS) for the years 2006, 2010, and 2013. We report patient and hospital characteristics at the encounter level.
Statistical analysis
Patients with clinical and symptomatic conditions were categorized as per their demographic and clinical characteristics for the years 2006, 2010, and 2013. Outcomes such as the number of annual ED visits and inpatient admissions were weighted to reflect national estimates from 2006 to 2013. We utilized a generalized linear regression model with a Poisson distribution and a Wald test to analyze the trend associated with ED visits and subsequent inpatient admissions over time, accounting for the US census population. We performed our analyses using SAS Enterprise Guide, version 7 (SAS Institute., Cary, NC) and considered two-tail p values <0.05 to be statistically significant.
Variation in subsequent admission rate was assessed with a hospital-based risk-standardized admission ratio (RSAR), i.e., the ratio of the number of predicted admissions to the number of expected admissions at a given hospital for each clinical outcome or symptom. We reported the ratio in RSAR as the ratio of the 75th percentile hospital to the 25th percentile hospital. A generalized linear mixed model that accounted for correlations among hospital encounters was used to estimate the RSAR for every hospital with ≥25 ED visits for each clinical outcome or symptom. The analytical model was adjusted for sex, household income, age, patient comorbidities (based on CCI), and insurance status. The coefficient of variation – defined as the ratio of the standard deviation to the mean – was also calculated.
Results
Baseline characteristics in patients with IBD
The mean age of patients who visited the ED was 40 years and the mean age of patients with subsequent inpatient admissions was 43 years. More than half of the patients in the study were women. Private insurance was most common among both patients with ED visits and those with subsequent inpatient admissions. A considerable proportion of patients with ED visits (2006: 16.8% and 2013: 20.0%) and subsequent inpatient admissions (13.8% and 16.0%) were uninsured. The proportion of ED visits and subsequent inpatient admissions did not vary significantly with household income across the three selected years. The regional distribution of ED visits and hospitalizations remained constant for the years 2006, 2010, and 2013. The CCI score remained mostly similar in patients who visited the ED (0.3 and 0.4) and in patients with subsequent inpatient admissions (0.4 and 0.5). The hospital length of stay was mostly similar over the study period (5.6 days and 4.9 days). The proportion of ED patients who were subsequently hospitalized reduced from 65.7% in 2006 to 55.7% in 2013 and most of the admitted patients were discharged home (85.4% and 84.6%) ().
Table 1a. Selected baseline demographic and clinical characteristics in patients with inflammatory bowel disease (IBD) visiting the ED in 2006, 2010, 2013
Table 1b. Selected baseline demographic and clinical characteristics in patients with inflammatory bowel disease (IBD) admitted to the hospital in 2006, 2010, 2013
Baseline characteristics in patients with IBD-related AP
The mean age of patients who were subsequently admitted was slightly greater than the patients who had visited the ED (). Patients with ED visits (37.2 years and 36.9 years, in 2006 and 2013, respectively) were comparatively younger than patients with subsequent inpatient admissions (40.6 years and 39.5 years, in 2006 and 2013, respectively). The majority of the ED visits(~60%) and subsequent inpatient admissions(~62%) for IBD-related AP were women. A greater proportion of patients with ED visits and those with subsequent inpatient admissions were privately insured. A considerable proportion of patients with ED visits (19.6% and 22.2%) and subsequent inpatient admissions (15.7% and 18.1%) were uninsured. Household income did not show an association with the extent of ED visits and subsequent inpatient admissions, however; ED visits increased in 2013 for patients with least household income (30.9%). The regional distribution of ED visits and hospitalizations remained constant for the years 2006, 2010, and 2013. The CCI score mostly remained the same for ED visits (0.1 and 0.2) and subsequent inpatient admissions (0.3 and 0.4) across the three selected years with a slight increase in 2013. Hospital length of stay mostly remained stable throughout the three selected years of the study (3.1 days and 3.0 days). The proportion of ED visits among patients with IBD-related AP who were subsequently hospitalized decreased from 6.9% in 2006 to 4.9% in 2013 and most of the admitted patients were discharged home (85.3% and 91.6%) ().
Table 2a. Selected baseline demographic and clinical characteristics in patients with IBD-related abdominal pain visiting the ED in 2006, 2010, and 2013
Table 2b. Selected baseline demographic and clinical characteristics in patients with IBD-related abdominal pain admitted to the hospital in 2006, 2010, and 2013
Trend Analysis of ED visits among patients with IBD
After accounting for US census population, annual ED visits among patients with IBD increased from 30.34 per 100,000 population in 2006 to 41.84 per 100,000 population in 2013 (p = 0.09). Annual subsequent inpatient admission from ED visits among patients with IBD were 19.93 per 100,000 population in 2006 and remained mostly stable with a minimal rise to 23.34 admissions per 100,000 population in 2013 (p = 0.52) ().
Trend analysis of ED visits for IBD-related AP
After accounting for US census population, annual ED visits among patients with IBD-related AP increased from 7.28 per 100,000 population to 11.88 per 100,000 population in 2013 (p = 0.12) (). For patients with IBD-related AP, the annual subsequent inpatient admissions remained stable between 2006 (0.50 per 100,000 population) and 2013 (0.58 per 100,000 population) with minimal rise (p = 0.88) ().
Hospital-based risk standardized admission ratio
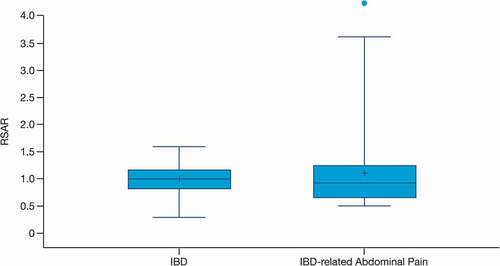
Based on the 398 hospitals with ≥25 ED visits for IBD, the ratio in RSAR between the 75th and 25th percentile hospitals was 1.42, with a coefficient of variation of 0.25, suggesting a notable variation in hospital admissions for IBD across hospitals. Similarly, based on the 81 hospitals with ≥25 ED visits for IBD-related AP, the ratio of RSAR for 75th-25th percentile hospitals was 1.96, with a coefficient of variation of 1.04, suggesting greater variation across hospitals in the rate of hospital admission for these type of visits ().
Discussion
While patients with IBD showed an increase in ED visits during the study period, the rate of subsequent inpatient admissions remained stable. A similar trend was noted in patients with IBD-related AP for ED visits and subsequent inpatient admissions. The overall rate in ED visits and subsequent inpatient admissions across different hospitals was similar for patients presenting with IBD-related issues, however; the rate of ED visits and subsequent inpatient admissions for patients specifically with IBD-related AP showed a greater variation.
A retrospective study evaluating the epidemiology of non-specific AP in patients with IBD reported that 31.5% of the ED visits among IBD patients were due to non-specific AP [Citation16]. The present study showed that the ratio of patients visiting ED with IBD vs. IBD-related AP was approximately 3:1 to 4:1. The national-level numbers of ED visits and subsequent inpatient admissions by patients with IBD-related AP reported by the current study fill a data gap in the literature. We believe the current study captured a more complete picture of ED resource utilization by patients with IBD and its related symptom of AP. The percentage of subsequent inpatient admissions among patients who visited the ED was much higher (55.7%) when compared with patients visiting the ED for IBD-related AP (4.9%).
AP occurs due to sub-clinical inflammation, overgrowth of bacteria in the small intestine, food intolerances, and bowel dysmotility [Citation17]. Weight loss, abdominal tenderness, depression, and nocturnal stools are significant predictors of IBD-related abdominal pain [Citation18]. As such, AP is often left unresolved due to lack of effective treatment. Treatment of AP with analgesics and opioids provides pain relief without any improvement in disease course. Optimum therapy for patients must include pain management combined with effective IBD therapy [Citation17].
An increasing prevalence of IBD is responsible for the rising direct and indirect treatment costs of the disease [Citation8]. The aggregate national cost of ED visits has shown a substantial rise of 207.5% and the cost of individual ED visits increased by 102.5% from 2006 to 2014 in the US [Citation7]. Although evidence evaluating the ED visit pattern in patients diagnosed with IBD is scarce, our findings were consistent with those in a recent study evaluating the ED utilization in US patients with IBD which reported 75.7 IBD-related ED visits per 100,000 ED visits in 2006 which increased to 100.1 IBD-related ED visits per 100,000 ED visits in 2014 [Citation7]. In addition, our results showing a decrease in the proportion of inpatient admissions subsequent to IBD-related ED visits (65.7% in 2006 to 55.7% in 2013) were consistent with Huh. et al, who reported a decrease in hospitalization rates for IBD subsequent to an ED visit between 2007 (65.2%) and 2014 (51.6%) [Citation3]. Regarding the possibility that these trends of decreasing hospital admission subsequent to ED visits were not specific to IBD patients, a similar study using NEDS data from the same time period in contrast reported a decrease in both the rate of ED visits and subsequent hospital admissions among patients with coronary artery disease [Citation14].
A significant variation in the rate of subsequent inpatient admissions was observed for patients with IBD (RSAR: 1.42) and for patients with IBD-related AP (RSAR: 1.96) [Citation18]. Use of different treatment modalities, variation in demographic characteristics of the patients across geographies, and differences in hospital infrastructure have been associated with variation in hospitalization rates [Citation19]. In particular, poor adherence to clinical practice guidelines has been reported as a contributing factor in high RSARs [Citation20]. Consistent with this, a retrospective study reported that implementation of specialty inpatient IBD care can reduce the chance of disease remission [Citation21]. Studies also report that implementation of a standardized treatment algorithm for patients with IBD can help reduce over-utilization of ED services and hospital length of stay [Citation22]. Incorporating biologic agents into treatment algorithms for patients with IBD has also been shown to optimize patient outcomes, quality of life, and decrease healthcare costs [Citation21,Citation23,Citation24].
Understanding the factors responsible for increased ED visits in patients with IBD is vital for optimizing management strategies among patients with IBD. Studies suggest that presence of psychiatric illness, low hemoglobin levels, age, and lack of access to gastroenterologists were significantly associated with higher rates of ED visits among patients with IBD [Citation22,Citation25]. The rise of ED visits among patients with IBD not only suggests an increase in the cost of overall IBD treatment, but also imply that the incidence of IBD has increased. Improving the quality of care for patients with IBD can reduce repeat ED visits. Although adequate clinical practice guidelines are available for the management of IBD, large variations in treatment patterns among practicing gastroenterologists/physicians have led to a gap in IBD management [Citation26–28]. Translation of recommended best practices into the care patients with IBD actually receive is needed to achieve optimal control of the disease.
The gap in IBD management could be due to the lack of a widely accepted standard treatment algorithm in the ED and outpatient clinic settings. Disease complexity coupled with non-specific symptoms such as AP demand a patient centered treatment approach. Although AP is one of the most common symptoms of IBD, it is under-researched and often inappropriately managed [Citation13]. Access to hospitals equipped adequately for the management of IBD is essential to achieve treatment goals. Studies have shown that lack of early gastroenterology care in patients with IBD has impacted hospitalization rates for IBD and overall clinical outcomes associated with the treatment of IBD [Citation29].
One of the prime strengths of this study was the utilization of the NEDS database, which is the most representative US sample of ED visits consisting of data from a wide geographical area and a large sample size for diverse disorders [Citation30]. Subgroup estimates such as different age groups or different hospital settings were possible because this database offers detailed information regarding geographical, hospital and patient characteristics, nature of ED visits, and clinical and resource use in inpatient care. Furthermore, several factors potentially confounding the estimates of ED visit rates and inpatient admissions such as the patient and hospital characteristics were controlled in the present analysis.
Our findings are subject to several limitations. First, our approach was vulnerable to the possibility of coding bias, misclassification of diagnosis codes, and lack of coding heterogeneity. IBD-related AP was identified using ICD-9-CM codes in the NEDS database rather than laboratory-confirmed diagnoses. Considering that the ICD-9-CM codes for IBD were not validated, misclassification or error in coding of IBD-related AP as a primary diagnosis with IBD as a secondary diagnosis may have contributed to a greater variation in hospital-based RSAR across different hospitals. Secondly, capture of data at encounter level rather than patient level might have presented a challenge to identify multiple visits by the same patient. Lack of data regarding covariates that potentially influence hospitalization such as prior hospitalization, concomitant medications, and clinical data to define disease severity (including comorbidities) may also be considered as limitations. Lastly, conducting the trend test without adjusting for potential confounding factors was also a limitation of the study.
In conclusion, the present study detected a trend towards increased annual ED visits from 2006 to 2013 for IBD and for IBD-related abdominal pain. However, the rise in rate of subsequent inpatient admissions for both ED visit types was lower than the rise in visit rate, suggesting increasing use of outpatient alternatives to care in the study population. The decision to admit a patient to the hospital was more variable for IBD-related AP, indicating a potential need for evidence-based research to improve translation of clinical practice guidelines into standard care.
Author contributions
ZD, AP, JI, CDP, JHL, and CWB were involved in study design. AP, ZD, JI, CDP, JHL, and CWB were involved in the interpretation of the results. ZD and JHL were responsible for the statistical analyses. All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors meet International Committee of Medical Journal Editor (ICMJE) criteria, and all those who fulfilled those criteria are listed as authors. All authors provided direction and comments on the manuscript, made the final decision about where to publish these data, and approved submission to this journal.
Disclosure statement
ZD, AP, JI, and CDP are employees of Janssen Pharmaceuticals (a Johnson & Johnson company) and hold stock in Johnson & Johnson. JHL is a former employee of Janssen Pharmaceuticals and was employed by Janssen Pharmaceuticals during study design, data interpretation and drafting of the manuscript. CWB has worked as a consultant and advisory board member for Janssen Pharmaceuticals, Salix Pharmaceuticals and Vapotherm; has previously received research funding from Janssen Pharmaceuticals and Boehringer Ingelheim; and has also served as an advisory board member and as a paid speaker for Roche Diagnostics.
Data Availability Statement
Please refer the NEDS database website (https://www.hcup-us.ahrq.gov/) for data included in the present study.
Additional information
Funding
References
- Park KT, Ehrlich OG, Allen JI, et al. The cost of inflammatory bowel disease: an initiative from the Crohn’s & Colitis Foundation. Inflamm Bowel Dis. 2020;26:1–10.
- Gajendran M, Umapathy C, Loganathan P, et al. Analysis of hospital-based emergency department visits for inflammatory bowel disease in the USA. Dig Dis Sci. 2016;61(2):389–399.
- Huh G, Yoon H, Choi YJ, et al. Trends in emergency department visits and hospitalization rates for inflammatory bowel disease in the era of biologics. PLoS One. 2019;14(1):e0210703.
- Park KT, Ehrlich OG, Allen JI, et al. The cost of inflammatory bowel disease: an initiative from the Crohn’s & Colitis Foundation. Inflamm Bowel Dis. 2020 Jan 1;26(1):1–10.
- Mehta F. Report: economic implications of inflammatory bowel disease and its management. Am J Manag Care. 2016;22(3 Suppl):s51–60.
- Gibson TB, Ng E, Ozminkowski RJ, et al. The direct and indirect cost burden of Crohn’s disease and ulcerative colitis. J Occup Environ Med. 2008;50(11):1261–1272.
- Ballou S, Hirsch W, Singh P, et al. Emergency department utilisation for inflammatory bowel disease in the USA from 2006 to 2014. Aliment Pharmacol Ther. 2018;47(7):913–921. .
- M’Koma AE. Inflammatory bowel disease: an expanding global health problem. Clin Med Insights Gastroenterol. 2013;6:33–47.
- Sabbatini AK, Wright B. Excluding observation stays from readmission rates - what quality measures are missing. N Engl J Med. 2018;378(22):2062–2065.
- Weiss AJ, Wier LM, Stocks C, et al. Overview of emergency department visits in the USA, 2011: statistical brief #174. Rockville (MD): Healthcare Cost and Utilization Project (HCUP) Statistical Briefs; 2006.
- Bielefeldt K, Davis B, Binion DG. Pain and inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:778–788.
- Altschuler A, Collins B, Lewis JD, et al. Gastroenterologists’ attitudes and self-reported practices regarding inflammatory bowel disease. Inflamm Bowel Dis. 2008;14:992–999.
- Carter MJ, Lobo AJ, Travis SPL. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004;53(suppl_5):v1–v16.
- Eichelberger C, Patel A, Ding Z; Eichelberger C, Patel A, Ding Z, et al. Emergency department visits and subsequent hospital admission trends for patients with chest pain and a history of coronary artery disease. Cardiol Ther. 2020;9:153–165.
- Yiadom M, Baugh CW, Jenkins CA, et al. Change in care transition practice for patients with nonspecific chest pain after emergency department evaluation 2006 to 2012. Acad Emerg Med. 2017;24(12):1527–1530.
- Cervellin G, Mora R, Ticinesi A, et al. Epidemiology and outcomes of acute abdominal pain in a large urban emergency department: retrospective analysis of 5,340 cases. Ann Transl Med. 2016;4(19):362.
- Norton C, Czuber-Dochan W, Artom M, et al. Systematic review: interventions for abdominal pain management in inflammatory bowel disease. Aliment Pharmacol Ther. 2017;46(2):115–125.
- Srinath AI, Goyal A, Zimmerman LA, et al. Predictors of abdominal pain in depressed pediatric inflammatory bowel disease patients. Inflamm Bowel Dis. 2014;20(8):1329–1340.
- Venkatesh AK, Dai Y, Ross JS, et al. Variation in US hospital emergency department admission rates by clinical condition. Med Care. 2015;53(3):237–244.
- Capp R, Ross JS, Fox JP, et al. Hospital variation in risk-standardized hospital admission rates from US EDs among adults. Am J Emerg Med. 2014;32(8):837–843.
- Law CC, Sasidharan S, Rodrigues R, et al. Impact of specialized inpatient IBD care on outcomes of IBD hospitalizations: a cohort study. Inflamm Bowel Dis. 2016;22(9):2149–2157.
- Nguyen GC, Bouchard S, Diong C, et al. Access to specialists and emergency department visits in inflammatory bowel disease: a population-based study. J Crohns Colitis. 2019;13(3):330–336.
- Taks M, Pijls PA, Derijks LJ, et al. Short article: the effect of implementation of a treatment algorithm for infliximab on remission rates and drug costs in inflammatory bowel disease patients. Eur J Gastroenterol Hepatol. 2017;29(2):169–173.
- Glassner K, Gajula P, Euers L, et al. Sa1860 – risk factors for repeated visits to the emergency department in patients with inflammatory bowel disease. Gastroenterology. 2019;156(6):S–431.
- Limsrivilai J, Stidham RW, Govani SM, et al. Factors that predict high health care utilization and costs for patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2017;15(3):385–392 e382.
- Strohl M, Gonczi L, Kurt Z, et al. Quality of care in inflammatory bowel diseases: what is the best way to better outcomes? World J Gastroenterol. 2018;24(22):2363–2372.
- Lichtenstein GR, Hanauer SB, Sandborn WJ, et al. Management of Crohn’s disease in adults. Am J Gastroenterol. 2009;104(2):465–483. quiz 464, 484.
- Pena-Sanchez JN, Lix LM, Teare GF, et al. Impact of an integrated model of care on outcomes of patients with inflammatory bowel diseases: evidence from a population-based study. J Crohns Colitis. 2017;11(12):1471–1479.
- Habashi P, Bouchard S, Nguyen GC, et al. Transforming access to specialist care for inflammatory bowel disease: the PACE telemedicine program. J Can Assoc Gastroenterol. 2018;2(4):186–194.
- Agency for Healthcare Research and Quality R, MD. NEDS Database Documentation. Healthcare cost and utilization project (HCUP). June 2019. 2019 Aug 23. Available from: www.hcup-us.ahrq.gov/db/nation/neds/nedsdbdocumentation.jsp.