ABSTRACT
The incidence of spontaneous pneumothorax has been estimated to 7.4–18.0/100,000 for men and 1.2–6.0/100,000 for women. The most common symptoms are sudden chest pain and dyspnoea. Due to chest pain many patients have an electrocardiogram (ECG) done in the acute setting.
We present a case of unusual findings of electric alternans in the electrocardiogram (ECG) in a patient with a left-sided spontaneous pneumothorax. Reviewing the literature we found five former cases of pneumothoraxes with electric alternans in the ECG, all occurring in relation to left-sided pneumothorax.
Background
The incidence of spontaneous pneumothorax has been estimated to 7.4–18.0/100,000 for men and 1.2–6.0/100,000 for women [Citation1,Citation2]. Risk factors include smoking, previous pneumothorax, male sex and age between 10 and 30 year [Citation3–Citation5].
The most common symptoms are sudden chest pain and dyspnoea, and the diagnosis can be confirmed by chest x-ray, lung ultrasound, or computed tomography. Due to chest pain many patients also have an electrocardiogram (ECG) done in the acute setting. In the following we present a case of unusual findings of electric alternans in the ECG in a patient with spontaneous pneumothorax.
Case presentation
A 34 year old woman with a history of smoking and non-adherent asthma, presented with 8 h of dyspnoea with acute worsening of shortness of breath and mid-sternal chest pain radiating towards the back. The patient experienced increasing pain during inspiration, and was treated with inhaled beta 2 agonist and intravenous morphine by paramedics prior to arrival at the hospital.
Investigations
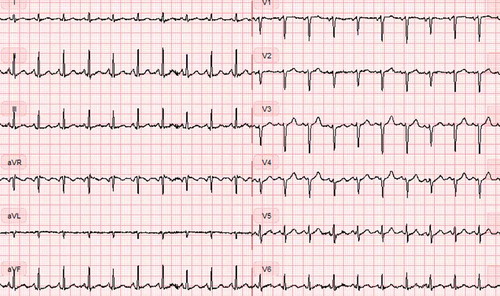
The patient was in moderate distress and was hypoxemic with a peripheral saturation of 97% on 8 L oxygen administered on a Hudson mask, with a heart rate of 124 b.p.m., blood pressure 110/76 mm Hg, and a respiratory rate of 20 breaths/min. Arterial blood gas analysis showed respiratory alkalosis with a pH value of 7.52, pCO2 3.8 kPa, pO2 11.2 kPa and lactate 1.2 mmol/L. Acute ECG revealed sinus tachycardia, heart rate 125 b.p.m., Q-waves in the first four precordial leads (V1-V4), normal axis (78 degrees), and an electric alternans with borderline low-voltage pattern, consistent with pericardial effusion (). Auscultation of the chest revealed decreased respiratory sounds on the left side, tachycardia and no murmurs. Lower extremities were without signs of deep venous thrombosis or edema. Acute chest x-ray confirmed tension pneumothorax with mediastinal displacement ().
Differential diagnosis
In general dyspnoea and chest pain could be symptoms of e.g. pulmonary embolism, acute coronary syndrome, pericarditis, and aortic dissection with pericardial effusion. A young female with a history of smoking and untreated asthma is at an increased risk for acute exacerbation of asthma.
Treatment
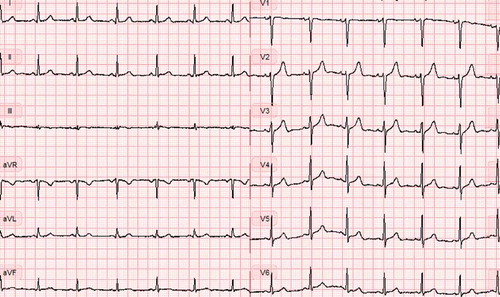
The patient was transferred directly from the radiology department to the department of orthopaedic surgery for chest tube insertion. An 18F chest tube was placed in the fourth intercostal space, in local anaesthesia with the patient in supine position. No rush of air or blood was recognized during the procedure. As the chest tube was fixed and connected to an electronic chest drain system, the symptoms resolved immediately. A subsequent chest x-ray revealed an expanded lung and a well placed chest tube (). The patient was transferred to the department of respiratory medicine. After 2 days there was no air leak from the chest tube and it was removed. A new ECG was recorded and showed no sign of electric alternans (). The patient was discharged with planned follow-up in the outpatient clinic.
Outcome and follow-up
In the outpatient clinic, the level of alpha-1 antitrypsin was analysed (1.63 g/L) and was in the normal range. A follow-up CT scan of the lungs showed bilateral centrilobular emphysema, highly concentrated to the upper lobes and the patient was encouraged to smoking cessation (). Spirometry showed FEV1 1.96 (66%), FVC 4.07 (120%) and FEV1/FVC 48.
Discussion
ECG is a fast and easy test for diagnosing cardiac ischemia in patients presenting with sudden onset dyspnoea and chest pain. Pneumothorax on the other hand can easily be distinguished from other causes of acute dyspnoea using a variety of radiological examinations including chest x-ray, lung ultrasound, or computed tomography. In a patient presenting with abnormal ECG, a diagnosis of pneumothorax can easily be delayed.
Few case presentations of ECG alterations has been published earlier all of them involving left-sided pneumothorax.
The first case of ECG changes were described by Kuritzky in 1976 where a 26-year-old woman with a spontaneous complete collapse of the left lung had phasic voltage alternation in the ECG and a shift of the P, QRS and T axis [Citation6]. Three years later Hallengren reported phasic voltage alternation in the ECG of a 37-year-old man with a left-sided pneumothorax [Citation7]. In 1997 Kozelj described a case of a 43-year-old man with a left-sided pneumothorax and an ECG that showed a frontal plane axis of 74 degrees and phasic voltage alternation [Citation8]. In 2009 Soltani presented a case of a 46-year-old man with a left-sided pneumothorax and an ECG with right axis deviation and phasic voltage alternation [Citation9]. The last case of a left-sided pneumothorax and ECG changes in a 53-year-old woman was described by Fei in 2015 [Citation10]. There have not been any cases of ECG changes due to a right-sided pneumothorax.
We present another case of left-sided pneumothorax in a young smoking woman with acute onset dyspnoea and alternating electric axis on ECG. The mechanism behind ECG variations in left-sided pneumothorax is thought to be related to the physical displacement of the heart in the mediastinum, with the heart possibly intermittently recoiling back to its normal position. In this context, a left-sided eventration of the diaphragm has also been reported to be able to cause electric alternans on ECG [Citation11].
As verified in earlier publications and in this case, left-sided pneumothorax can lead to an abnormal ECG and alternating electric axis and low voltage possibly mimicking pericardial effusion. A thorough assessment with auscultation and percussion, chest x-ray or lung ultrasound is therefore needed in the physical examination of patients with acute onset dyspnoea and chest pain.
The patient in this case had normal levels of alpha-1 antitrypsin and despite a young age, pronounced centrilobular emphysema predominantly located in the upper lobes, probably causing the pneumothorax. In the literature only few descriptions of abnormal ECG findings has been published but the incidence may be much higher than reported.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Notes on contributors
Diana Chabané Schmidt
Diana Schmidtis a resident in pulmonology with prior experience in general practice, internal medicine and ortopedics. She has a wide medical interest and a former position as a research fellow within the field of childhood acute lymfoblastic leukemia and immunotherapy.
Charlotte Andersson
Charlotte Andersson is a cardiology fellow at Herlev-Gentofte hospital. She has a long-standing research interest in various aspects of cardiovascular epidemiology, including pharmacoepidemiology, genomics, and clinical outcome studies. Outside her clinical work she mentors 4 PhD students focusing on various aspects of cardiovascular disease and its risk factors.
Hans Henrik Schultz
Hans Henrik Schultz is a specialist registrar in pulmonology, with combined 9 years of clinical and research experience in respiratory medicine and thoracic surgery. Main research areas are lung transplantation but also the connection between heart and lung, and the interplay between respiratory medicine and thoracic surgery.
References
- Bense L, Eklund G, Wiman L-G, Smoking and the increased risk of contracting spontaneous pneumothorax. Chest. 1987;92(6):1009–4. http://www.ncbi.nlm.nih.gov/pubmed/3677805. Accessed 2017 Dec 30.
- Melton LJ, Hepper NG, Offord KP. Incidence of spontaneous pneumothorax in Olmsted County, Minnesota: 1950 to 1974. Am Rev Respir Dis. 1979;120(6):1379–1382.
- Primrose WR. Spontaneous pneumothorax: a retrospective review of aetiology, pathogenesis and management. Scott Med J. 1984;29(1):15–20.
- Schramel FM, Postmus PE, Vanderschueren RG, Current aspects of spontaneous pneumothorax. Eur Respir J. 1997;10(6):1372–1379. http://www.ncbi.nlm.nih.gov/pubmed/9192946. Accessed 2017 Dec 30.
- Noppen M. Spontaneous pneumothorax: epidemiology, pathophysiology and cause. Eur Respir Rev. 2010;19(117):217–219.
- Kuritzky P, Goldfarb AL, Unusual electrocardiographic changes in spontaneous pneumothorax. Chest. 1976;70(4):535–537. http://www.ncbi.nlm.nih.gov/pubmed/975956. Accessed 2017 Dec 30.
- Hallengren B, Phasic voltage alternation in spontaneous left-sided pneumothorax. Acta Med Scand. 1979;205(1–2):143–144. http://www.ncbi.nlm.nih.gov/pubmed/760403. Accessed 2017 Dec 30.
- Koželj M, Rakovec P, Sok M, Unusual ECG variations in left-sided pneumothorax. J Electrocardiol. 1997;30(2):109–111. http://www.ncbi.nlm.nih.gov/pubmed/9141605. Accessed 2017 Dec 30.
- Soltani P, Malozzi CM, Abi Saleh B, et al. Electrocardiogram manifestation of spontaneous pneumothorax. Am J Emerg Med. 2009;27(6):750.e1-5.
- Fei J, Marill KA. ECG phasic voltage changes associated with spontaneous pneumothorax in a patient with vanishing lung syndrome. BMJ Case Rep;2015. DOI: 10.1136/bcr-2014-207498. (jan23 2): bcr2014207498-bcr2014207498
- Gul EE, Can I, Ozbek O. Displacement of the heart by diaphragm: is this heart alternating?. J Electrocardiol. 2011;44:465–466.