ABSTRACT
Introduction: Chronic obstructive pulmonary disease (COPD) contributes to impaired health-related quality of life (HRQoL). Patient education and smoking cessation programs are recommended to reduce the number of exacerbations and hospitalizations, but the effects of such programs have yet to be explored in larger samples.
Objective: The aim was to explore the longitudinal effects of patient education and smoking cessation programs on exacerbations and hospital admissions in patients with COPD.
Design: This is a register study where data from the Swedish National Airway Register, including 20,666 patients with COPD, were used. Baseline measures of demographic, disease-related, and patient-reported variables were compared with a follow-up, 10–30 months after baseline. Descriptive statistics and changes between baseline and follow-up were calculated.
Results: Comparing those not participating in education programs to those who did, HRQoL deteriorated significantly between baseline and follow-up in non-participants; there was no change in either exacerbations or hospitalizations in either group; there was a significant difference in baseline HRQoL between the two, and, when controlling for this, there was no significant change (p = 0.73). Patients who participated in smoking cessation programs were younger than the non-participants; mean 66.0 (standard deviations (SD) 7.8) vs. mean 68.1 (SD 8.8), p = 0.006. Among participants in smoking cessation programs, the proportion with continued smoking decreased significantly, from 76% to 66%, p < 0.001. Exacerbations at follow-up were predicted by FEV1% of predicted value and exacerbations at baseline. Hospital admissions at follow-up were predicted by baseline FEV1% of predicted value and exacerbations at baseline.
Conclusions: To prevent exacerbations and hospital admissions, treatment and prevention must be prioritized in COPD care. Patient education and smoking cessation programs are beneficial, but there is a need to combine them with other interventions.
Background
Chronic obstructive pulmonary disease (COPD) is a progressive and life-limiting disease which is predicted to be the third-leading cause of death by the year of 2020, globally [Citation1]. Recent GOLD guidelines recommend combined COPD assessment, where COPD first is classified into four spirometric stages and then severity grading due to successively increasing symptoms and exacerbations [Citation2,Citation3]. COPD creates a significant burden for the patient in terms of disability and impaired health-related quality of life (HRQoL) [Citation4,Citation5]. When adjusting for spirometric stage of COPD, deteriorated HRQoL was found to be predicted by increasing dyspnea, depression/anxiety, an increasing number of exacerbations, and decreased exercise capacity [Citation6]. Other signs of deteriorating COPD disease are disabling breathlessness [Citation7] and low body mass index [Citation8].
Preventive measures to reduce the impact of exacerbations are a priority [Citation9], including patient education [Citation10–Citation13]. Factors reducing urgent health care utilization for patients affected by COPD were found to be general education, exercise, and physical therapy [Citation10]. A specific COPD exacerbation action plan accompanied by a single short educational component along with ongoing support was found to reduce hospitalization and exacerbations [Citation11]. Other studies have shown that patient education have been shown to decrease the risk of hospitalization [Citation12], improve HRQoL [Citation12], and significantly lower exacerbation frequency [Citation12,Citation13].
Furthermore, among continuing smokers, smoking cessation has the highest priority. Cigarette smokers have a higher prevalence of respiratory symptoms and lung function abnormalities, a greater annual rate of decline in Forced Expiratory Volume (FEV1)%, increased exacerbations rate [Citation14], and a greater COPD mortality rate than non-smokers [Citation15]. Participation in a smoking cessation program compared to non-participation was shown to significantly decrease self-reported phlegm and significantly less number of days hospitalized for COPD [Citation16]. In a meta-analysis including four studies with 1,540 participants, it was found that a combination of behavioral treatment and pharmacotherapy is effective in helping smokers affected by COPD to quit smoking [Citation17].
In the Swedish national guidelines for patients affected by COPD [Citation18], it is recommended that these patients should be offered interprofessional patient education programs and support for smoking cessation. The patient education program could relate to activities of daily life, energy-saving techniques, coping with exacerbation, anxiety, and stress, dietary counseling, medication, smoking cessation, and education about the disease. Patients should be supported to be vigilant and heed incipient exacerbation. A written care plan gives the patient the opportunity to administer adequate medication for early onset of symptoms. A care plan could also include recommendations for diet and physical activity [Citation17]. Patient education and smoking cessation programs are recommended for patients with COPD to reduce the number of exacerbations and hospitalization, but the effect of the programs has yet to be explored in a larger sample. Therefore, the aim of the present study was to explore the longitudinal effect of patient education and smoking cessation programs on exacerbations and hospital admission in patients affected by COPD, and to explore what factors influence the number of exacerbations and the number of hospital admissions at follow-up. Primary outcome was the effect of patient education and smoking cessation program on exacerbations. Secondary outcome was the effect of patient education and smoking cessation program on hospitalizations. The study also explores the impact of various other baseline variables related to mortality and hospital admissions.
Methods
This is a longitudinal register study using data from the Swedish National Airway Register, which was introduced in 2009. In 2012, the model was expanded to also include asthma. The present study comprises data from the register both prior to and after expansion. From the cohort from 2012 until 2015 (Cohort 1), only data for the patients affected by COPD were extracted. All patients have been reported to the register based on their spirometry measurements fulfilling COPD requirements. The cohort collected from 2009 until 2012 was merged with the cohort collected between 2012 and 2015 (Cohort 2). The patients were registered at their visits at outpatient clinics, with one registration recorded per visit. During the expansion phase, some patients had been registered both in the earlier register and the expanded register. In the first cohort, there were 11,300 registrations of 7,800 patients, and the second cohort comprised 35,300 registrations for 15,100 patients. Duplicate registrations were identified and the two cohorts were merged. In the merged register (Cohorts 1 and 2), 20,666 unique patients were identified within a total of 46,628 registrations.
Follow-up registrations were identified for the patients who had more than one registration. In order to have a larger cohort at follow-up, the time frame for the follow-up was set to be between 10 and 30 months after the baseline visit. If the patient had more than one visit over 10–30 months, the most recent visit was used so as to have as long a period as possible between baseline and follow-up. Another criterion for choosing the most recent visit to use at follow-up was that the registration should include registration of FEV1% of predicted value. The number of exacerbations and hospitalizations were defined as number of exacerbations or hospitalizations due to COPD last 12 months and one registered exacerbation or hospitalization could therefore be included twice. Because of this, we chose to include and analyze the registrations of these variables at follow-up visits from more than 12 months after baseline visit, not to risk including an exacerbation or a hospitalization more than once.
Variables
Demographic variables were registered, e.g. age, sex, and social situation, that is whether the patient was living alone or cohabiting. Disease-related variables comprised spirometric stage of COPD, obstruction, measured by FEV1 as percentage of predicted value, oxygen saturation, number of exacerbations, and number of hospital admissions due to COPD in the last 12 months. All hospital admissions mentioned in the paper concern admission due to COPD. Patient-reported variables were smoking (non-smokers, quit smoking, or still smokers), and exercise capacity, that is number of reported days per week with physical activity.
In the first register, i. e. Cohort 1, and for some patients in the expanded register, i.e. Cohort 2, HRQoL was measured by the clinical COPD questionnaire (CCQ) [Citation19], a patient-rated questionnaire with 10 items, measuring: one item each of dyspnea at rest, dyspnea during physical activities, cough, and phlegm; two items about how concerned the patient is about the dyspnea; and four items about how the dyspnea had limited the patient’s activities, i.e. strenuous physical activities, moderate physical activities, daily activities, and social activities. All items are scored by the patient; from 0, ‘never,’ to 6, which corresponds to ‘almost all the time.’ The mean score of the items is used and the results are interpreted as follows: 4.0–6.0 means a large or very large impact on HRQoL/health status; 2.0–3.9 corresponds to moderate impact on HRQoL, and 0.0–1.9 means no or small impact on HRQoL. The minimal clinically important difference in the CCQ was found to be 0.4 [Citation20].
Functional dyspnea was measured by the Modified Medical Research Council (mMRC) dyspnea scale [Citation21]. The mMRC dyspnea scale is a patient-rated, single-item scale where severity of the dyspnea experience is reported, ranging from 0, corresponding to ‘Not troubled by breathlessness except on strenuous exercise,’ to 4, corresponding to ‘breathless when dressing or undressing.’ The wording of the items in mMRC is presented in . The results from the mMRC are presented both as continuous and categorical variables.
Table 1. Labels for the categorical steps in mMRC.
Patient education programs are not standardized but usually include, e.g. lectures to increase knowledge about COPD, medications, and infection prevention; advice about physical activity, breathing, and coughs; and relaxation techniques, energy conserving techniques and daily life aids. The patient education programs could also include advice on appropriate actions to take during exacerbations, as well as smoking prevention and smoking cessation. The smoking cessation programs were not standardized, but use to include both pharmacological and non-pharmacological components. Participation in either intervention was marked as participated or not for both variables, that is patient education and/or smoking cessation programs.
Procedure
The interventions in this report are categorized as participation in patient education and/or participation in smoking cessation programs. In the register, a registration at baseline that the patient had participated in either patient education or smoking cessation programs could not distinguish whether the patient had participated before their first registration in the register, or the specific visit when the first registration was made. Therefore, patients who had participated in the intervention at baseline were not included in the analysis of the effect of interventions. Patients who had participated at follow-up were compared with the patients who had not participated at either baseline or at follow-up. The strategy of excluding patients who were registered as participants at baseline was adopted to ensure that the intervention was new to the patient between baseline and follow-up, and could therefore be assumed to have an effect at follow-up. The register has no information about earlier unsuccessful participations in smoking cessation programs.
Data analysis
Descriptive statistics were used for providing a description of the sample and the registered treatments, with mean values and standard deviations (SD) calculated for continuous variables. The categorical variables were presented as numbers and percentages for the total sample. In , demographic, clinical and patient-reported variables are presented for baseline for the total sample. The comparisons between baseline and follow-up, presented in , relate to all patients for whom there was a follow-up, irrespective of their participation in patient education or smoking cessation programs. The comparisons between baseline and follow-up were made with paired statistics. Paired statistics were also used when comparing within the sample of participants in patient education or in smoking cessation program, and within the sample of non-participants ( and ). For comparisons between baseline and follow-up in continuous variables, paired sample t-test was used, and for categorical variables, the Sign test was used. When comparing differences between the samples of participants and non-participants, an independent sample t-test was used for continuous variables, and the Mantel–Haenszel chi-square test was used for ordered categorical variables. To control for baseline differences in HRQoL, an analysis of covariance was performed with baseline HRQoL as covariate. Spearman’s correlation coefficient (rs) was used for all correlation analysis.
Table 2. Differences between patients at baseline and at follow-up at a visit at 10–30 months later.
Table 3. Differences between participants and non-participants in patient education programs.
Table 4. Differences between participants and non-participants in smoking cessation program.
Two univariable logistic regression analyses were performed; one with patient education program and one with smoking cessation program as the dependent variable. Independent variables were: age; sex; social situation; FEV1% of predicted value; exacerbations in the last 12 months; hospital admissions due to COPD in the last 12 months; smoking, dichotomized into non-smokers, i.e. both never smokers and ex-smokers, and smokers; and dyspnea, measured by mMRC. Second, independent variables that significantly predicted the dependent variable with p < 0.20 in the univariable analyses were entered in the multivariable stepwise logistic regression analyses with the same dependent variables.
The primary outcome was number of exacerbations in the last 12 months and the secondary outcome was number of hospital admissions due to COPD in the last 12 months. These variables were not found to be normally distributed, with a Shapiro–Wilks test result <0.001. Therefore, generalized linear models with negative binomial distribution were performed with number of exacerbations in the last 12 months and number of hospital admissions due to COPD in the last 12 months as dependent variables, and age, sex, social situation, baseline registrations of FEV1% of predicted value, exacerbations per year, hospital admission due to COPD, smoking, and participation in patient education or smoking cessation program as independent variables. Second, independent variables that significantly predicted the dependent variable with p < 0.20 in the univariable analyses were entered into generalized linear models with negative binomial distribution with the same dependent variables. All significance tests were two-sided and were conducted at the 5% significance level.
The study was approved by the Ethics Committee at the Department of Medical Ethics in Gothenburg on 7 July 2015 (Dnr: 317-15).
Results
At baseline, 20,666 patients were included. One follow-up visit within the time span 10–30 months was identified for 3,497 patients. The mean number of days between baseline and follow-up was 561 (SD 175), and the median 537 days (range 300–900). Time between baseline and follow-up correlated significantly with change in dyspnea, measured by mMRC (rs = 0.11, p < 0.001), with change in exacerbations (rs = 0.06, p = 0.007), but not with change in number of hospitalizations due to COPD (rs = −0.01, p = 0.73), or with change in HRQoL, measured by CCQ (rs = 0.05, p = 0.079) (data not shown).
There was a significant deterioration between baseline and follow-up in HRQoL, with a mean of 0.10 (SD 0.89, p < 0.001), median of 0.1 (min −3.5, max 3.6) and in functional dyspnea, in that 772 patients (29.6%) deteriorated, the majority were unchanged (49.6%), and 542 (20.8%) improved (p < 0.001) (). The number of patients participating in patient education programs increased significantly from baseline to follow-up (from 31.3% to 47.5%, p < 0.001), but there was no significant difference between the proportion of patients who participated in smoking cessation programs at baseline and follow-up (30.5% vs. 29.3%, p = 0.17).
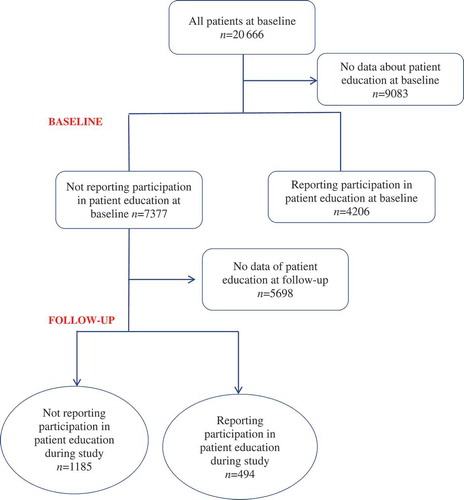
Patients who had not participated in patient education programs at baseline were identified (n = 7,347). At follow-up, they were divided into those who had not participated at follow-up (n = 1,185) and those who had (n = 494) (). shows a flowchart of the participants and non-participants in the patient education program. Comparisons in were made between the two categories represented by the ovals in . HRQoL and dyspnea differed significantly in the non-participation and the participation groups at baseline in that patients in the non-participant group had a mean CCQ of 1.58 (SD 1.03), and the participants’ mean value was 1.77 (SD 1.10), p < 0.001. In the non-participation group, HRQoL measured by CCQ deteriorated from baseline to follow-up with a mean value of 0.13 (SD 0.87, p < 0.001), but, in the participation group, HRQoL improved slightly with a mean value of 0.05 (SD 0.91, p = 0.019). A one-way analysis of covariance was conducted to compare the effectiveness of the patient education. The independent variable was change in HRQoL, measured by CCQ from baseline to follow-up, and the dependent variable consisted of the participation in patient education. Patient-reported CCQ at baseline was used as the covariate in the analysis. After adjusting for baseline CCQ, there was no significant difference in change in CCQ between the participants and non-participants in patient education (p = 0.73). There was a non-significant numerical difference in HRQoL between the groups participating and not participating in patient education at follow-up in that 27% of participators had an improvement of 0.4 or more, while 23% of non-participators had an improvement of 0.4 or more (data not shown). In the non-participating group, dyspnea improved for 205 patients (19.4%), was unchanged for 530 (50%) of the patients, and deteriorated for 324 (30.6%) of the patients between baseline and follow-up. There was a significant difference in baseline dyspnea between the participant group and the non-participant group. There were no significant differences between baseline and follow-up in the participation group. There was no significant difference in change of dyspnea between participants and non-participants.
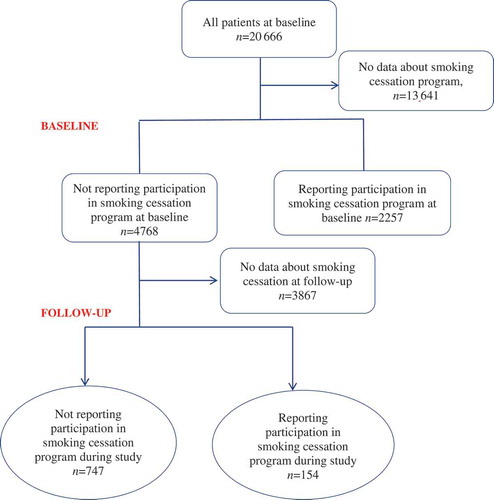
There were significant differences between baseline and follow-up for patients who participated in smoking cessation programs in that patients who participated in smoking cessation programs were significantly younger than the non-participants, with a mean value of 68.1 (SD 8.8) vs. a mean value of 66.0 (SD 7.8); p = 0.006. shows a flowchart of the participants and non-participants in the smoking cessation programs. Comparisons in were made between the categories illustrated in the ovals in . HRQoL, measured by CCQ, deteriorated in the non-participating group with a mean value of 0.09 (SD 0.8), p = 0.007, and in the participating group with a mean value of 0.06 (SD 0.9) p = 0.55. Dyspnea improved in 124 patients (18.1%) in the non-participating group, and in 38 patients (27.3%) in the participating group, and deteriorated in 215 patients (31.4%) in the non-participating group and in 39 of the participating patients (28.1%, p = 1.0). Thus, there was a significant deterioration in the non-participating group between baseline and follow-up (p < 0.001), but not in the participating group ().
There was a significant decrease in smoking prevalence, from 33.6% at baseline to 30.6% at follow-up (). There were significant changes in smoking from baseline to follow-up in both the group who participated in patient education and the group who did not participate. Among the non-participants, 7.5% decreased smoking (p < 0.001), and, among the participants, 8.4% decreased smoking (p = 0.03). There was no significant difference in changes between the participants and the non-participants (p = 0.28). In relation to smoking cessation, significantly more patients who participated in smoking cessation programs decreased their smoking compared to those who did not participate, 4% compared to 16%, p < 0.001. There was significant difference in change in smoking between the participants and non-participants in smoking cessation programs (p < 0.001).
Table 5. Smoking among the patients who participated and not participated in patient education and smoking cessation program.
A predictor of participation in patient education program at follow-up was an increased number of exacerbations at baseline, and the odds of participating in a patient education program were 31% lower for smokers compared to non-smokers (). Age was the only predictor of participation in a smoking cessation program, in that the odds of participating decreased with increasing age.
Table 6. Logistic regression with patient education program and smoking cessation programs as dependent variables. Patients were included if they had not participated in the intervention at baseline. The independent variables are from baseline.
In the generalized linear models, with negative binomial distribution with number of exacerbations at follow-up as dependent variable, FEV1% of predicted value and exacerbations at baseline were found to be predictors of exacerbations at follow-up (). The number of hospital admissions at follow-up was predicted by baseline FEV1% of predicted value and by exacerbations at baseline, but not with hospital admissions at baseline. However, when excluding non-smokers from the analysis, hospitalizations became an additional predictor (data not shown).
Table 7. Generalized linear models with negative binomial distribution analysis with number of exacerbations and hospital admissions as dependent variables, and with independent variables from baseline.
Discussion
There was no decrease in the number of exacerbations or hospitalizations among the patients who participated in patient education or in smoking cessation program, but the findings that the disabling symptom of dyspnea did not increase, and that the HRQoL did not deteriorate in the intervention group, could indicate that participating is of benefit to patients. Although the deterioration in HRQoL of the non-participants did not reach minimally clinical important difference of 0.4 [Citation20], it was found that the non-participants deteriorated while the participants improved. In a register study of patients affected by COPD, disabling breathlessness, defined as an mMRC score ≥2, was found in 54% of the patients, and predictors of disabling breathlessness were found to be higher age, lower FEV1% of predicted values, obesity, and depression [Citation7]. Dyspnea could be detrimental to well-being. Patients affected by COPD were, in an interview study, found to experience death anxiety related to fear of suffocation, awareness of death, fear of dying and separation anxiety [Citation22]. The patients also experienced life anxiety, which relates to the fear of living a life with disabling breathlessness, which gave them a fear of the future. In relation to the nature of dyspnea, it could be inferred that participation in patient education that results in a non-deterioration in COPD is beneficial for the patient [Citation23,Citation24]. The fact that dyspnea was significantly worse at baseline in the participation group compared to the non-participation group, could indicate that patients with more severe dyspnea were more inclined to participate in patient education.
Exacerbations at follow-up were predicted by FEV1% of predicted value and number of exacerbations at baseline. This indicates the importance of effective management of exacerbations and deterioration in patients affected by COPD. This finding is in-line with recent GOLD guidelines, that the best predictor of frequent exacerbations is a history of earlier treated events [Citation1,Citation25]. It is suggested that written negotiated action plans for worsening symptoms may lead to less respiratory-related hospitalization and all-cause hospitalizations as well as improved health status. Hospitalizations at follow-up were predicted by exacerbations and FEV1% of predicted value at baseline. Therefore, the treatment of exacerbations and their prevention must be prioritized areas in COPD care. When excluding non-smokers from the analysis, hospital admission became an additional predictor. This could be due to that the smokers are more impacted by the disease [Citation26].
Patient education could be an intervention that hinders deterioration and helps the patients to manage the disease. Other disease-management interventions for patients affected by COPD could be exercise, self-management of exacerbations, action plans for exacerbations, and education programs which, in a systematic review, were found to increase quality of life and improve the participants’ exercise tolerance after 12 months for those who participate in the programs [Citation27]. The review also found that, for the participants treated with such programs, the number of hospital admissions related to exacerbations decreased and the total number of days spent in hospital was reduced by 3 days. The Swedish national guidelines also emphasize that patients affected by COPD should be offered patient education to enable them to manage exacerbations and to avoid hospitalizations [Citation18]. However, in the present study, we could not show that participation in patient education either decreased the number of exacerbations or the number of hospitalization days due to COPD. In a study of 2,000 patients affected by COPD, it was found that one-third took a ‘wait and see’ approach to exacerbations; this indicates that it would be appropriate to educate patients about the proper actions to take to prevent an exacerbation [Citation28].
HRQoL deteriorated and dyspnea symptoms worsened significantly among patients who did not participate in a smoking cessation program, but not for patients who did. Although a decreased number of hospitalizations have earlier been found for patients who participated in smoking cessation programs [Citation16], the present study could not show this. Neither exacerbations nor hospital admissions were influenced by patient education or smoking cessation. The proportion of patients who participated in patient education increased significantly from baseline to follow-up, but the proportion of patients participating in smoking cessation programs did not (). The predictors of participation in patient education were a higher number of exacerbations at baseline, and, to a lesser extent, being a smoker. The reason for this could be that the smokers participated in smoking cessation programs instead of education or that the smokers were ashamed by their smoking and were not able to quit smoking, as described by Jonsdottir and Jonsdottir [Citation29]. The only predictor of participation in smoking cessation program was younger age. The reason for this might be that younger people are more inclined for lifestyle changes. In the present study, participating in a smoking cessation program was found to be effective in helping patients to quit smoking, and this could contribute to a lower number of exacerbations in the long run, therefore, a follow-up within 10–30 months might be too short to have any effect on exacerbations or hospital admissions. The patient education program includes education about how to identify exacerbations and about how to understand when it is necessary to seek hospital care. One explanation for why the number of exacerbations did not decrease after participation in the program could be that patients in the patient education program became more aware of the seriousness of an exacerbation.
Limitations
The results from the present study should be interpreted with caution first, because it is a retrospective register study and not a randomized controlled trial, and second because of some irregularities in the reporting of some variables. There were some registrations of smoking that did not seem to be accurate, in that a few patients were registered as non-smokers at baseline and as smokers or ex-smokers at follow-up and that smoking cessation program has been provided to ex-smokers. In the multivariable generalized linear model in , it was shown that smoking did not affect the number of exacerbations or hospitalizations. One reason for this could be that smoking was dichotomized into non-smokers, which included both never smokers and ex-smokers, and smokers. This division might not have been appropriate, as it is known that ex-smokers are affected by smoking also after smoking cessation.
One limitation is that there were differences in the number of patients for whom the items were completed, and in , it is apparent that about one-third of the patients were still smokers and that around one-third of the patients participated in smoking cessation programs. Thus, there could be a substantial number of patients for whom there were no data relating to whether they participated in smoking cessation or not.
The follow-up period of 10–30 months could be regarded as a wide time span. A follow-up period of 10–12 months could be considered too short to show any results after patient education, but at the median of time to follow-up of about 18 months, patient education would have the potential to influence the patients’ health.
Conclusions
Prevention of exacerbations and hospital admissions, treatment and prevention is prioritized in COPD care. Patient education and smoking cessation programs are beneficial, but need to combine with other interventions. Number of exacerbations at baseline predicted both number of exacerbations and number of hospitalizations at follow-up. Therefore, all measures to prevent exacerbations are beneficial for COPD patients’ well-being.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Notes on contributors
Ingela Henoch
Ingela Henoch is a registered nurse and associate professor in nursing at Sahlgrenska academy, Gothenburg, Sweden. This research was conducted at Angered Hospital where IH has a position as researcher.
Claes-Göran Löfdahl
Claes-Göran Löfdahl is a pulmonary physician and senior professor in medicine at Lund's University Sweden.
Ann Ekberg-Jansson
Ann Ekberg-Jansson is a pulmonary physician, associate Professor at Sahlgrenska academy and has a position as head of Research and Devlopment at Region Halland, Sweden.
References
- Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Respirology. 2017;22(3):575–13.
- Seamark DA, Seamark CJ, Halpin DM. Palliative care in chronic obstructive pulmonary disease: a review for clinicians. JRSM. 2007;100(5):225–233.
- Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365.
- Murray CJL, Barber RM, Foreman KJ, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386(10009):2145–2191.
- Ståhl E, Lindberg A, Jansson SA, et al. Health-related quality of life is related to COPD disease severity. Health Qual Life Outcomes. 2005;3:56.
- Henoch I, Strang S, Löfdahl CG, et al. Health-related quality of life in a nationwide cohort of patients with COPD related to other characteristics. Eur Clin Respir J. 2016;3(1):31459.
- Sundh J, Ekström M. Persistent disabling breathlessness in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2016;11:2805–2812.
- Sundh J, Montgomery S, Hasselgren M, et al. Change in health status in COPD: a seven-year follow-up cohort study. NPJ Prim Care Respir Med. 2016;26:16073.
- Soler-Cataluna JJ, Martinez-Garcia MA, Sanchez LS, et al. Severe exacerbations and BODE index: two independent risk factors for death in male COPD patients. Respir Med. 2009;103(5):692–699.
- Dickens C, Katon W, Blakemore A, et al. Complex interventions that reduce urgent care use in COPD: a systematic review with meta-regression. Respir Med. 2014;108(3):426–437.
- Howcroft M, Walters EH, Wood-Baker R, et al. Action plans with brief patient education for exacerbations in chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;12:CD005074.
- Peytremann-Bridevaux I, Staeger P, Bridevaux PO, et al. Effectiveness of chronic obstructive pulmonary disease-management programs: systematic review and meta-analysis. Am J Med. 2008;121(5):433–43.e4.
- Worth H, Dhein Y. Does patient education modify behaviour in the management of COPD? Patient Educ Couns. 2004;52(3):267–270.
- Kanner RE, Anthonisen NR, Connett JE. Lung Health Study Research Group. Lower respiratory illnesses promote FEV(1) decline in current smokers but not ex-smokers with mild chronic obstructive pulmonary disease: results from the lung health study. Am J Respir Crit Care Med. 2001;164(3):358–364).
- Chapman KR, Mannino DM, Soriano JB, et al. Epidemiology and costs of chronic obstructive pulmonary disease. Eur Respir J. 2006;27(1):188–207.
- Borglykke A, Pisinger C, Jorgensen T, et al. The effectiveness of smoking cessation groups offered to hospitalised patients with symptoms of exacerbations of chronic obstructive pulmonary disease (COPD). Clin Respir J. 2008;2(3):158–165.
- Van Eerd EA, Van Der Meer RM, Van Schayck OC, et al. Smoking cessation for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;8:CD010744.
- National Board of Health and Welfare. National guidelines for care of asthma and COPD. Support for management and administration. [Swedish: nationella riktlinjer för vård vid astma och KOL. Stöd för styrning och ledning] [Internet] 2015. [cited 2017 Oct 24]. Available from: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/19949/2015-11-3.pdf
- Van Der Molen T, Willemse BW, Schokker S, et al. Development, validity and responsiveness of the clinical COPD questionnaire. Health Qual Life Outcomes. 2003;1:13.
- Zhou Z, Zhou A, Zhao Y, et al. Evaluating the clinical COPD questionnaire: a systematic review. Respirology. 2017;22(2):251–262.
- Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586.
- Strang S, Ekberg-Jansson A, Henoch I. Experience of anxiety among patients with severe COPD: a qualitative, in-depth interview study. Palliat Support Care. 2013;12(6):1–8.
- Haughney J, Partridge MR, Vogelmeier C, et al. Exacerbations of COPD: quantifying the patient’s perspective using discrete choice modelling. Eur Respir J. 2005;26(4):623–629.
- Kessler R, Ståhl E, Vogelmeier C, et al. Patient understanding, detection, and experience of COPD exacerbations: an observational, interview-based study. Chest. 2006;130(1):133–142.
- Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138.
- Zhang J, Lin X-F, Bai C-X. Comparison of clinical features between non-smokers with COPD and smokers with COPD: a retrospective observational study. Int J Chron Obstruct Pulmon Dis. 2014;9:57–63.
- Kruis AL, Smidt N, Assendelft WJ, et al. Integrated disease management interventions for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;10:CD009437.
- Barnes N, Calverley PM, Kaplan A, et al. Chronic obstructive pulmonary disease and exacerbations: patient insights from the global hidden depths of COPD survey. BMC Pulm Med. 2013;13(1):54.
- Jonsdottir R, Jonsdottir H. The experience of women with advanced chronic obstructive pulmonary disease of repeatedly relapsing to smoking. Scand J Caring Sci. 2007;21(3):297–304.