ABSTRACT
Background: Listening to music as a means of relieving anxiety before and during endoscopy has been examined in several studies but results so far are contradictory and inconclusive.
Aims: We aimed to determine whether listening to music could reduce anxiety prior to and during bronchoscopy, and whether it is influenced by the patient’s preference in music.
Methods: 300 patients undergoing bronchoscopy for suspected lung cancer were randomly assigned to: self-selected music, specially-designed music (MusiCureTM), or control (no sound). Spielberger’s State-Trait Anxiety Inventory (STAI) was administered three times: at admission, after 20 min with or without music (preceding bronchoscopy), and shortly before discharge. The primary outcome was STAI state score after 20 min, with or without exposure to music prior to bronchoscopy.
Results: On average, music reduced the STAI score by 2.5 points (95% CI, 1.1 to 4.0; p < 0.001) compared with the control group. This reduction was largest in the self-selected music group (3.4; 95% CI, 1.5 to 5.3; p < 0.001). In contrast, specially designed music did not significantly reduce STAI score (1.7; 95% CI, −0.3 to 3.6; p = 0.1).
Conclusion: Listening to music reduces anxiety in patients undergoing bronchoscopy, provided that the music complies with the patient’s preferences.
Introduction
Bronchoscopy is an important invasive tool in the diagnosis of lung cancer. Fear and anxiety related to bronchoscopy are quite common in patients, much like emotions observed in patients facing other invasive procedures [Citation1–Citation3]. Since anxiety is an unpleasant sensation, which negatively affects patients’ tolerance of the procedure, it is important that healthcare staff address and seek to relieve anxiety [Citation2]. With administration of sedatives comes an increased risk of respiratory depression [Citation4–Citation6].
In a previous randomised investigator-blinded study, we examined the effect of specially designed music (MusiCureTM), played for 10 min before bronchoscopy and throughout the procedure. Anxiety was measured by Spielberger’s State-Trait Anxiety Inventory (STAI) on arrival, after 10 min with or without music, and at discharge. We found no significant effect of music when adjusting for baseline anxiety and sex [Citation7].
Anxiety and music in relation to bronchoscopy have also been studied in a randomised controlled trial by Colt et al. Patients were exposed to pre-recorded piano improvisations versus no music during bronchoscopy, and STAI was used as primary outcome. It was concluded that there was no significant effect of music on anxiety [Citation8].
A major limitation in both studies is the use of investigator-selected music. While some evidence exists that music influences anxiety, further research is needed to establish the effect of patient-selected music in relation to investigator-selected music [Citation9,Citation10].
The aim of this study was to investigate the anxiety-reducing effect of self-selected and investigator-selected music, played for a period of 20 min prior to bronchoscopy.
Material and methods
Subjects
The study was approved by the Danish Ethics Committee (Protocol no. H-3–2014-065), and patients were consecutively included in the study among patients referred for examination for pulmonary nodules in the period between October 2016 and November 2017. In total, 1162 patients were assessed for eligibility, 671 patients were excluded, due to exclusion criteria, and a further 191 eligible patients refused to participate, leaving 300 patients to be included in the study and randomised to three groups (). Baseline characteristics were not significantly different between the three groups (), and no clinically significant differences were observed between those 266 who were analysed per protocol, and those 34 who were not. There is no difference in conclusions when analysing data as intention-to-treat and per-protocol analysis.
Figure 1. Flowchart of the trial (CONSORT flow diagram, www.consort-statement.org).
Table 1. Baseline characteristics.
However, there were significant differences in some baseline values between those who were excluded prior to randomisation and the 300 patients included in the study. The excluded patients were older, had lower weight and height and lower levels of lung function. There was, however, no significant difference regarding gender.
Study design
Randomisation was performed by block randomisation in blocks of 15 patients, using Statistical Package for the Social Sciences (SPSS) version 22.0. Patients were assigned to one of three treatment groups:
self-selected genre of music ()
specially-designed music (MusiCure™)
control (no sound)
Table 2. Track list for the categories in the group of self-selected music.
We employed a randomised design and did not consider baseline anxiety, aiming to include a clinically relevant ‘real-life’ study population rather than those most likely to benefit from an anxiety-reducing intervention, i.e. patients having a high baseline anxiety score
The sample size was set at 300, using estimates from study by Colt et al. [Citation8]. The standard deviation was set at 10.4 for STAI state, and a difference of five points was interpreted as clinically relevant. The significance level was set at 0.05, power at 0.90, and a 20% dropout was estimated.
The primary endpoint in the study was anxiety score after 20 min with or without music measured with Spielberger’s STAI (State, form Y). The inventory consists of 40 self-reported items including 20 assessing state anxiety and 20 assessing trait anxiety. The scores of each item vary from 1 to 4, and each inventory has a minimum score of 20 and a maximum score of 80. Higher scores indicate higher levels of anxiety [Citation11,Citation12].
Methods
Patients subjected to examination of pulmonary nodules were informed about the study when they were scheduled for bronchoscopy at the outpatient clinic at Bispebjerg University Hospital, Copenhagen. Written informed consent was obtained from the patients on admission. Subsequently, blood pressure, heart rate, respiratory rate, and oxygen saturation (SaO2) were recorded, and a blood sample was taken from the peripheral venous catheter for analysis of serum cortisol. Participants completed an electronic version of the STAI on a tablet device (iPad, Apple, Cupertino, CA, USA). A staff member not involved with the patient at any time opened the sealed envelope containing the randomised treatment: MusiCure™, self-selected music or control (no sound). The same staff member also fitted the in-ear earphones (Flying Tiger, Copenhagen, Denmark) into the patient’s ears and adjusted the volume on the mp3 player (SanDisk, Clip Sport, Milpitas, CA, USA). All patients, including the control group, wore earphones during the procedure, to ensure blinding of the staff. The patients were not blinded, and the written information stated that the aim of the study was to investigate if MusiCure™ could reduce anxiety.
After 20 min with or without music the second blood sample was collected from the peripheral venous catheter for analysis of s-cortisol. Blood pressure, heart rate, respiratory rate, and SaO2 were recorded, and the participants completed the State part of the STAI.
On admission to the operating theatre, blood pressure, heart rate, respiratory rate, and SaO2 were recorded again. An accelerometer (ActiGraph, GT3X+, Pensacola, FL, USA) was attached to the patient’s chest. The device recorded movement with epoch lengths of 10 seconds measured in hertz.
Afterwards, the patients were sedated with midazolam and fentanyl, with an initial standard dose of 5 mg midazolam and 50 microgram fentanyl, titrated until sedation. All patients underwent bronchoscopy lying in the supine position while being exposed, through earphones, to either specially-designed music (MusiCure™), self-selected music or no sound (control), and throughout the bronchoscopy blood pressure, heart rate, respiratory rate and SaO2 were recorded every 15 min.
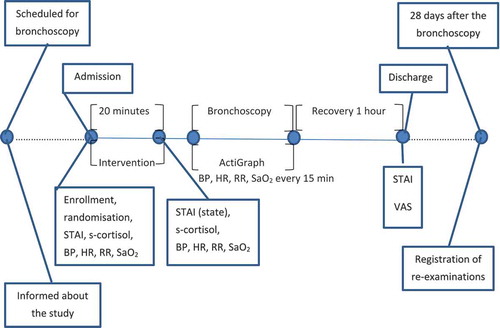
On discharge, approximately 60 min after bronchoscopy, patients completed the STAI and a visual analogue scale (VAS) indicating the overall perception of sound before and during bronchoscopy, ranging from very bad to very good. After 28 days, the number of re-examinations was registered ().
Figure 2. Timeline.
BP = blood pressure; HR = heart rate; RR = respiratory rate; SaO2 = oxygen saturation; STAI = Spielberger’s state trait anxiety inventory; VAS = visual analogue scale.
Plasma cortisol was analysed with competitive electrochemiluminescence immunoassay (ECLIA) (Cobas 8000, e801 module, Roche, Basel, Schweiz).
Analysis
Normally distributed continuous variables were compared using one-way ANOVA. When not normally distributed the Kruskal–Wallis test was used. The χ2-test was used for categorical variables. Statistical analyses were completed using SPSS version 22.0 (Chicago, IL, USA). Results are reported in intention-to-treat values. Missing values are replaced with last-observation-carried-forward regarding STAI and replaced by 0 regarding the VAS scale.
Results
There were no significant differences between the three groups on the absolute values of STAI state or STAI trait at the time of admission, nor after 20 min with or without music, or at discharge ().
Table 3. Comparison of STAI scores.
However, music did have a significant effect in reducing state anxiety when analysing the change (Δ-STAI) after 20 min [F (2, 297) = 8.68, p < 0.001, ω = .05]. On average, music reduced the STAI state score by 2.5 points (95% CI, 1.1 to 4.0; p < 0.001) compared with the control group. This reduction was greatest in the self-selected music group (3.4; 95% CI, 1.5 to 5.3; p < 0.001), whereas specially designed music showed a smaller and nonsignificant reduction in STAI state score (1.7; 95% CI, −0.3 to 3.6; p = 0.1).
Tukey-adjusted post-hoc comparisons indicated that the change in STAI state score was significant with self-selected music (mean±SD) (−6.3 ± 6.2) compared with that for the control group (no sound) (−2,9 ± 5.1) (p < 0.001; d 0.6). MusiCure™ (−4.6 ± 5.9) did not significantly differ from no music (p = 0.1) nor from self-selected music (p = 0.09) in terms of change in STAI state score ().
Figure 3. Mean difference of STAI state score (Δ-STAI) from admission to 20 min with or without music prior to bronchoscopy.
There was a significant effect of music on change of STAI score from admission to 20 min with or without music [F (2, 297) = 8.68, p < 0.001, ω = .05]. Tukey-adjusted post-hoc comparisons indicated that the change in STAI state score was significant with self-selected music (mean±SD) (−6.3 ± 6.2) compared with that for the control group (no sound) (−2,9 ± 5.1) (p < 0.001; d 0.6). MusiCure™ (−4.6 ± 5.9) did not significantly differ from no music (p = 0.1) nor from self-selected music (p = 0.09) in terms of change in STAI state score.
![Figure 3. Mean difference of STAI state score (Δ-STAI) from admission to 20 min with or without music prior to bronchoscopy.There was a significant effect of music on change of STAI score from admission to 20 min with or without music [F (2, 297) = 8.68, p < 0.001, ω = .05]. Tukey-adjusted post-hoc comparisons indicated that the change in STAI state score was significant with self-selected music (mean±SD) (−6.3 ± 6.2) compared with that for the control group (no sound) (−2,9 ± 5.1) (p < 0.001; d 0.6). MusiCure™ (−4.6 ± 5.9) did not significantly differ from no music (p = 0.1) nor from self-selected music (p = 0.09) in terms of change in STAI state score.](/cms/asset/4d31645f-48ee-49e9-8582-a921c7fb3e0f/zecr_a_1583517_f0003_b.gif)
Analysing the results of the VAS at discharge, reporting patients’ self-perception of the sound, there was a highly significant difference between the music groups and the control group [H (2) = 33.81, p < 0.001] (). When analysing the differences between the three treatments, the median VAS score of the control group (median (IQR); 4.5 mm (8.1)) compared with that for the group receiving MusiCure™ (8.3 mm (2.4); p < 0.001) and that of the group receiving self-selected music (8.1 mm (2.9); p < 0.001) was highly significant. No significant difference was found between MusiCure™ and self-selected music (p = 1.0).
Figure 4. Patients overall perception of the sound prior to and during bronchoscopy.
There was a highly significant difference between the music groups and the control group [H (2) = 33.81, p < 0.001]. When analysing the differences between the three treatments, the median VAS score of the control group (median (IQR); 4.5 mm (8.1)) compared with that for the group receiving MusiCure™ (8.3 mm (2.4); p < 0.001) and that of the group receiving self-selected music (8.1 mm (2.9); p < 0.001) was highly significant. No significant difference was found between MusiCure™ and self-selected music (p = 1.0).
![Figure 4. Patients overall perception of the sound prior to and during bronchoscopy.There was a highly significant difference between the music groups and the control group [H (2) = 33.81, p < 0.001]. When analysing the differences between the three treatments, the median VAS score of the control group (median (IQR); 4.5 mm (8.1)) compared with that for the group receiving MusiCure™ (8.3 mm (2.4); p < 0.001) and that of the group receiving self-selected music (8.1 mm (2.9); p < 0.001) was highly significant. No significant difference was found between MusiCure™ and self-selected music (p = 1.0).](/cms/asset/491e6fba-dfd1-40d5-b100-a031abff8670/zecr_a_1583517_f0004_b.gif)
When dividing the groups by VAS tertiles and looking at change in STAI state score, the significant change in STAI state is found in the top VAS tertile ().
Figure 5. STAI change from admission to after 20 min with or without music divided by how the patients appreciated the sound measured by VAS.
There is only a significant difference in STAI change in the upper tertile of VAS measuring how patients appreciated the sound. (Kruskal–Wallis test is used because of the very different sizes of the groups).
No significant differences were found in physiological variables, as blood pressure, heartrate, oxygen saturation, respiratory rate and s-cortisol. Nor were there any significant differences between the groups in duration of the bronchoscopy, amount of sedatives, movement during the bronchoscopy or number of re-examinations. Furthermore, there were no statistically significant differences between the groups in confounders like attending staff (nurses and doctors) and diagnostic procedures performed during bronchoscopy.
Discussion
In this RCT study, we were able to detect differences in anxiety score by STAI state when comparing the changes in anxiety from admission (baseline) to 20 min after exposure to self-selected music. We found a significant reduction in anxiety for those who listened to self-selected music compared to the control group. This reduction persisted after adjusting for sex and baseline anxiety.
Interestingly, patients in both music groups had similar perception ratings of the sound environment (VAS). It has been hypothesized that self-selected music reduces anxiety because it provides patients with a sense of control over their situation [Citation13,Citation14]. In a sub-analysis, the meaningful change in STAI state occurred when the patients responded in the top tertile of the self-perceptive VAS scale (). Those who either disliked the sound or were neutral did not experience any significant reduction in anxiety compared to the control group. It seems, therefore, that the possibility of selecting music is, in and of itself, not enough. Nor is it enough to be satisfied with the sound. It seems that the music must comply with the patient’s personal preference and that it is, perhaps, the element of familiarity that causes the positive effect on decreasing anxiety.
Brain research indicates that music is processed differently in the brain depending on an individual’s musical background and competence [Citation15,Citation16]. This might explain why patients in the two music groups are equally satisfied with the sound but vary in changes in anxiety.
There is no consensus on what a minimal clinically important difference in STAI state should be [Citation10]. A change of 6.3 points found in the present RCT study from admission to 20 min after listening to music is a small difference on a scale from 20 to 80 points, but in line with several other studies, which also study the effect of music on anxiety [Citation10,Citation17–Citation19]. One principle when calculating the minimal important difference is that the change should be greater than half the standard deviation at baseline [Citation20]. In this study, the standard deviation of STAI state baseline is 12.6, and 6.3 is just the half. Calculating the effect size the partial eta squared for the change is ranged as medium (η = .06), but the less biased omega squared is characterised as small, but close to medium (ω = .05). Another measure of effect size is Cohen’s d, and again the effect size is ranged as medium (d = 0.6).
It can be questioned whether a huge effect can be seen, when the mean of STAI state was 41.5 at admission. The STAI manual indicates a mean of working adults of 35.5 points [Citation11]. This is not far below the mean of participants in this study, though the mean in this study also corresponds with similar studies [Citation8–Citation10]. Patients who declined to participate commonly responded that they were too nervous to focus on anything other than the forthcoming bronchoscopy and therefore too nervous to concentrate on completing questionnaires. Regardless, we were able to show an effect in the present group with moderately increased STAI state score.
We found no significant differences between the groups regarding vital signs such as blood pressure, heartrate, respiration rate and s-cortisol. This might be due to the fact that moderate anxiety does not create physiological arousal, because the physical change is so small that it is impossible to detect, or due to physiological arousal not following the same pace as subjective changes in anxiety. In the current study, we did not control confounders such as antihypertensive and cardiac medications.
There are discrepancies in earlier studies regarding the effect of listening to music on vital signs. A recent meta-analysis about the effect of music during bronchoscopy concludes that music during bronchoscopy is an effective way of reducing patients´ blood pressure and heartrate [Citation21]. Whereas a review found only a small effect on physiological variables [Citation10] and another review found no effect of music [Citation9]. It can be questioned whether there is a cultural aspect in the findings because the conclusion of the meta-analysis is built on four Chinese studies and one European. Approximately half of the studies included in the review that finds a small difference in physiological parameters are Asian, in contrast to the review with no clear findings, which only includes a quarter of Asian studies.
In the present study, we found no significant differences in re-examinations of patients. In the present study, every patient with a history of bronchoscopy was excluded. The significant difference of re-examinations in our previous study is probably confounded by an uneven distribution of patients with a former history of bronchoscopy.
In the former study, we also questioned whether the exposure time of 10 min to MusiCure™ was long enough. In a recent RCT, the duration needed to reduce preoperative anxiety measured with STAI was investigated. Sessions of self-selected music for 15 and 30 min were investigated, and it appeared that as little as 15 min of listening to self-selected music provided a significant change in STAI state [Citation17].
Low-cost single-use earphones were chosen for reasons of hygiene. The impact of sound quality can be queried and seen as a limitation. Another limitation is that, during bronchoscopy, the music interventions were probably confounded by the sedatives, making it unlikely that the sensor recording chest movements, and every other measurement recorded during the bronchoscopy, truly reflected the music intervention.
In relation to the self-perceptive VAS, the difference between the intervention groups and the control group might be due to disappointment within the control group with not receiving music and could also be biased by the patients´ awareness of their participation in a study whose objective was to measure the effect of listening to music. Another bias in connection with that was that the patients were aware of that the aim of the study was to investigate the effect of MusiCure™ and this could impact their rating.
There were no group differences in re-examinations (diagnostic yield), amount of sedatives required and physiological parameters; however, the study was not powered to detect such differences in secondary outcomes.
Reduction of anxiety is certainly desirable, yet it is important that any adjunct intervention does not impact negatively on diagnostic yield [Citation22]. Optimal patient satisfaction and optimal diagnostic yield are however not mutually exclusive and both should be sought for the benefit of the patient.
Conclusion
Music prior to bronchoscopy reduces anxiety for patients undergoing bronchoscopy for suspected lung cancer if the music is consistent with the patient’s own preferences. There is, overall, more satisfaction among patients, with the sound environment before and during bronchoscopy, when listening to any type of music. Due to its low cost and safety, self-selected music pre-procedurally can reasonably be offered to patients undergoing bronchoscopy.
Acknowledgements
We thank composer Niels Eje for the music set-up, the management and staff at the Respiratory Department at Bispebjerg Hospital. The study was funded by Department of Respiratory Medicine, Bispebjerg Hospital, Department of Cardiothoracic Anaesthesiology, Rigshospitalet and Professor Vibeke Backer.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes on contributors
Elisabeth Jeppesen
Elisabeth Jeppesen is a registered nurse at the outpatient clinic in respiratory medicine at Bispebjerg Hospital, Copenhagen, Denmark. She has a special interest in preoperative anxiety and the effects of music on physical and psychological well-being.
Carsten M. Pedersen
Carsten M. Pedersen is a clinical nurse specialist at the department of Cardiothoracic Anaesthesiology, Copenhagen University Hospital. He has a Master of Science, MSc (Nursing) and educated as a CCN (Critical Care Nurse) and CRNA (certified registered nurse anesthetist). He has a special interest within preventing inadvertent perioperative hypothermia, endotracheal suctioning, PONV and preoperative anxiety
Klaus R. Larsen
Klaus R. Larsen is a medical doctor, PhD, and chief respiratory physician. Specialist in pulmonary and allergy diseases at Bispebjerg Hospital, Copenhagen Denmark. He has a special interest lung cancer, bronchoscopy, endoscopic ultrasound and transcutaneous biopsy. He is active in science.
Emil S. Walsted
Emil S. Walsted is a medical doctor, PhD, and is a trainee in respiratory medicine at Bispebjerg Hospital, Copenhagen Denmark. He has a special interest in the larynx, breathlessness and frontier technology.
Anne Rehl
Anne Rehl is a registered nurse at the outpatient clinic in respiratory medicine at Bispebjerg Hospital, Copenhagen, Denmark. She takes a special interest in the patient’s wellbeing during the procedures in the out-patient clinic.
Julie Ehrenreich
Julie Ehrenreich is a registered nurse at the outpatient clinic in respiratory medicine at Bispebjerg Hospital, Copenhagen, Denmark. She has a special interest in the calming effects of music.
Sascha Schnoor
Sascha Schnoor is a registered nurse at the outpatient clinic in respiratory medicine at Bispebjerg Hospital, Copenhagen, Denmark, as a patient coordinator. She works to ensure optimal clinical pathways for patients in the lung cancer examination process.
Vibeke Backer
Vibeke Backer is a chief respiratory physician and chair professor in respiratory medicine, Bispebejrg hospital, Copenhagen university, Denmark. Vibeke Backer have > 30 former PhD students and 2 doctor of medical science who have defended their thesis, 3 Master of Science. Opponent at 6 PhD-thesis and 3 DMSci. Furthermore, she has more than 325 publications in total: Citation 5501 & H-index 43. She developed a new Journal, called CRJ 2006 and was editor-in-chief until 1.1.2013, Impact raised from 0 to 1.2, Medline 2009. Together with the Nordic professor group, she developed a new Journal from 1.1.2014 called European Clinical respiratory Journal (ECRJ).
References
- Poi PJ, Chuah SY, Srinivas P, et al. Common fears of patients undergoing bronchoscopy. Eur Respir J. 1998;11:1147–9.
- Tetikkurt C, Yasar I, Tetikkurt S, et al. Role of anxiety on patient intolerance during bronchoscopy. Br J Med Med Res. 2014;4(11):2171–2180.
- Badner NH, Nielson WR, Munk S, et al. Preoperative anxiety: detection and contributing factors. Can J Anaesth. 1990 May;37:444–447.
- Putinati S, Ballerin L, Corbetta L, et al. Patient satisfaction with conscious sedation for bronchoscopy. Chest J. 1999;115:1437–1440.
- Matot I, Kramer M. Sedation in outpatient bronchoscopy. Respir Med. 2000;94:1145–1153.
- Mouchantaf FG, Shostak E, Lamb CR. Characteristics and financial costs of patients with respiratory failure at bronchoscopy. J Bronchology Interv Pulmonol. 2012;19:188–194.
- Jeppesen E, Pedersen CM, Larsen KR, et al. Music does not alter anxiety in patients with suspected lung cancer undergoing bronchoscopy: a randomised controlled trial. Eur Clin Respir J. 2016;3:33472.
- Colt HG, Powers A, Shanks TG. Effect of music on state anxiety scores in patients undergoing fiberoptic bronchoscopy. Chest J. 1999;116(3):819–824.
- Gillen E, Biley F, Allen D. Effects of music listening on adult patients’ pre‐procedural state anxiety in hospital. Int J Evid Based Healthc. 2008;6(1):24–49.
- Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. Cochrane Database Syst Rev. 2013;(6):CD006908. DOI:10.1002/14651858.CD006908.pub2
- Spielberger CD, Gorsuch RL, Vagg PR, et al. Manual for the State-Trait Anxiety Inventory STAI (form Y). Paolo Alto, CA: Consulting Psycologists Press, Inc; 1983.
- Spielberger CD, Gorsuch RL, Lushene RE. STAI manual for the State-Trait Anxiety Inventory. Paolo Alto, CA: Consulting Psychologists Press, Inc; 1970.
- Labbé E, Scmidt N, Babin J, et al. Coping with stress: the effectiveness of different types of music. Appl Psychophysiol Biofeedback. 2007;32:163–168.
- Chanda ML, Levitin DJ. The neurochemistry of music. Trends Cogn Sci. 2013 apr;17(4):179–193.
- Vuust P, Pallesen KJ, Bailey C, et al. To musicians, the message is in the meter pre-attentive neuronal responses to incongruent rhythm are left-lateralized in musicians. Neuroimage. 2005;15;24(2):560–564.
- Caldwell GN, Riby LM. The effects of music exposure and own genre preference on conscious and unconscious cognitive processes: a pilot ERP study. Conscious Cogn. 2007;16:992–996.
- McClurkin S, Smith C. The duration of self-selected music needed to reduce preoperative anxiety. J PeriAnesthesia Nurs. 2016;31(3):196–208.
- Hayes A, Buffum M, Lanier E, et al. A music intervention to reduce anxiety prior to gastrointestinal procedures. Gastroenterol Nurs. 2003;26(4):145–149.
- Bringman H, Giesecke K, Thörne A, et al. Relaxing music as pre-medication before surgery: a randomised controlled trial. Acta Anaesthesiol Scand. 2009;53:759–764.
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life. The remarkable Universality of half a standard deviation. Med care. 2003;41(5):582–592.
- Tam WW, Lo KK, Hui DS. The effect of music during bronchoscopy: a meta-analysis. Heart Lung. 2016;45:86–94.
- Metha AC. Don’t lose the forest for the trees. Satisfaction and success in bronchoscopy. Am J Res Crit Care Med. 2002;166:1306–1307.
