ABSTRACT
Background: Exacerbation in Chronic obstructive pulmonary disease (COPD) becomes more frequent with advancing disease severity and often the patients end up being hospitalized.
Objective: To evaluate the impact on exacerbations of establishing a cross-sectorial lung team (CLT) for patients with COPD at high risk of exacerbating.
Methods: In total, 49 patients with severe COPD were affiliated to a CLT for 6 months. On request from the participants, the CLT was available for telephone calls and home visits day and night to initiate treatment and give advice. Data regarding hospitalizations were collected 3 years prior to the intervention year to predict future numbers of admissions and length of stay. These predictions were compared with the observed data. COPD assessment test (CAT) was conducted before and after intervention.
Results: Observed risk of hospitalization (0.54 (95% CI 0.32; 0.90), p = 0.0192)) and length of hospital stay due to COPD (0.41 (95% CI 0.22; 0.76), p = 0.0046)) were significantly lower during the intervention period than predicted. A numerical but non-significant improvement in the total CAT score of 1.10 (95%CI: –0.71;2.91), p = 0.226)) was observed.
Conclusion: Affiliation to a CLT seemed to lower the burden of COPD exacerbations in a high-risk population.
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by airway obstruction due to inflammation and destruction of lung tissue. The disease leads to various degrees of breathlessness, cough, mucus and frequent respiratory infections as well as decreasing lung function.
In Denmark, 320,000 citizens are estimated to suffer from COPD [Citation1]. In 2018, the official number of hospital admissions due to COPD was 22,311 with a re-admission rate (within 30 days) of 19% and an overall 30-day mortality rate of 11% [Citation2,Citation3]. For several years, initiatives to improve continuity of care for patients with COPD across the primary and secondary healthcare sectors have been on the political agenda in Denmark [Citation1,Citation4]. Meanwhile, patients with COPD continue to be hospitalized and readmitted frequently [Citation1,Citation5].
Research points to the fact, that patients with COPD in general are not being offered an equal quality of treatment compared to patients with other chronic diseases [Citation6]. In addition, patients with COPD more frequently experience that they are not taken seriously by healthcare professionals, which might transform to insecurity [Citation6,Citation7]. Finally, among patients with COPD, a trend has been observed towards acting late in the symptom build-up resulting in acute worsening and hospitalization [Citation8].
Patients with COPD constitute a large group in both primary and secondary healthcare sectors. Collaboration based on patients’ preferences may have a number of positive outcomes. Patients with COPD emphasize the importance of having the possibility to contact a respiratory nurse night and day. Also, they prefer education close to home as transportation to hospital or community support center requires much mental and physical effort [Citation8]. Studies have demonstrated that home visits paid by a hospital or a community nurse can reduce hospital admissions and readmissions [Citation9–12]. Some of the interventions comprised treatment at home [Citation12,Citation13], others education regarding management, observation and prevention of exacerbations [Citation10,Citation11].
Patient-centered collaboration across healthcare sectors lies at the root of good patient management and may involve community nurses, general practitioners (GPs) [Citation9,Citation14,Citation15], and/or community nurses supervised by hospital-based respiratory specialist nurses [Citation9,Citation12].
To our knowledge, no study has yet investigated the effect of acute joint home visits (community nurses in close collaboration with hospital-based respiratory specialist nurses) on severe exacerbations measured as the total number of COPD-related hospital admissions and readmissions and as length of hospital stay. To improve continuity of care for patients with COPD across healthcare sectors, we established a cross-sectorial cooperation based on patients’ and relatives’ recommendations [Citation7].
We hypothesized, that affiliation with the cross-sectorial lung team (CLT) would reduce the number of COPD-related hospital admissions including readmissions, and would also reduce the length of hospital stay. Henceforth, admissions will include readmissions. Furthermore, we hypothesized that affiliation to the CLT is equal to usual care regarding safety. Therefore, the aim of the present study was to determine the feasibility and safety of establishing a CLT and the impact on exacerbations for patients at high risk of COPD exacerbations.
Methods
Study design
In this pilot study, a prospective follow-up design was used to evaluate the impact on severe exacerbations of establishing a CLT.
Patients
All patients were affiliated with the CLT for at least 6 months.
Inclusion criteria were (i) hospitalization due to COPD within the past year or forced expiratory volume in 1 s (FEV1) <50% and at least two acute exacerbations of COPD (AECOPD) treated with antibiotics and/or cortisone within the past year, (ii) citizens of the Municipality of Aarhus, Denmark, (iii) registered as patients at the Department of Respiratory Diseases and Allergy, Aarhus University Hospital (AUH) and (iv) age > 45 years. Patients were included from September 2015 to February 2016.
Consecutive patients were enrolled from the COPD outpatient clinic or when hospitalized at the Department of Respiratory Diseases and Allergy, AUH.
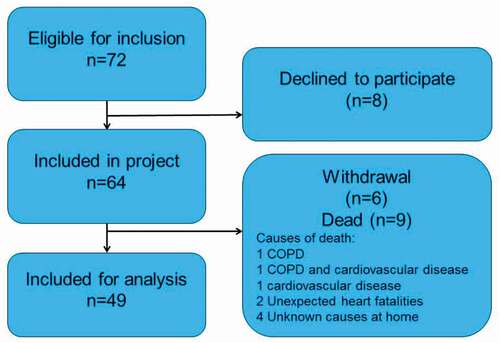
Seventy-two patients were eligible for inclusion of whom 49 patients were included in the final analyzes, as eight declined to participate, nine died and six withdrew from the project before 6 months of intervention ().
Intervention
The CLT constituted of a specialist nurse from the Department of Respiratory Diseases and Allergy at Aarhus University Hospital (AUH) with enhanced competences in respiratory medicine and community nurses from the Acute Team in the Municipality of Aarhus with minimum five years of vocational experience from the hospital.
During daytime, the specialist nurse coordinated the CLT’s activities, educated the community nurses in pulmonary nursing skills (often in the homes of the patients) such as inhaler technique, observation of symptoms related to AECOPD, breathing techniques for patients with dyspnea. The community nurses also visited the COPD outpatient clinic at AUH for one or 2 days where they were taught about medical treatment, inhaler technique and measuring lung function. In addition, the CLT performed joint home visits with the community nurses. In the evening, during night-time and weekends, the community nurses were CLT-coordinators.
The CLT was to improve patients´ ability to detect and handle on symptoms of AECOPD and appropriately as well to contact the CLT to discuss the need for treatment. The intervention was based on user-initiated contact to improve patient involvement. Thus patients contacted the CLT when needed to agree on home visits, telephone follow-up etc.
The CLT’s activities involved:
– Giving information and advice on request from patients, relatives and primary care staff.
– Initiating treatment and home visits depending on the patients’ needs. The medical treatment was guided by a respiratory specialist doctor from the hospital. The treatment options comprised oxygen therapy, nebulizer treatment, intravenous antibiotic therapy, intermittent CPAP (continuous positive airway pressure) treatment, and treatment with antibiotics and/or cortisone. Treatment was initiated in accordance with local and/or international guidelines [Citation16,Citation17].
– Drawing blood samples (infection counts, arterial blood gas, etc.), measuring blood pressure, oxygen saturation, lung function and collected sputum sampling
– Acute/subacute consultations at the Department of Respiratory Diseases and Allergy, if needed.
The GP was informed whenever additional treatment was commenced. If the patient contacted the CLT for reasons other than COPD, they were directed to their GP.
Data collection and measurements
Admissions and length of hospital stay
Data from February 2016 to August 2016 on hospital admissions and length of hospitalization were collected from the Electronic Patient Records in the Central Denmark Region (MidtEPJ). Data were compared with historical data from the same patient sample for the corresponding period (from February to August) in the three preceding years to get an estimate of disease development over time. These data were also collected at MidtEPJ. By monitoring number of admissions and length of stay during 3 years, we aimed at preventing deviations in a single year caused by fortuitous circumstances such as stable weather conditions. To avoid influence of seasonal variation, we chose historical data from February to August for comparison as it corresponds to the data collection period for the intervention [Citation18,Citation19]. The hospitalizations were categorized in three groups related to the patients´ treatments. Some of the patients received treatment for exacerbation of COPD. Other were treated for exacerbation of COPD and one or more comorbidities (cardiovascular diseases, diabetes, etc.) [Citation17]. The last category was related to treatments for all other causes (e.g. ileus, cerebral infarction due to thrombosis).
Quality of life
Quality of life (QoL) was used as an indirect parameter to assess safety for patients affiliated to the CLT. QoL was measured with the COPD Assessment Test (CAT) at the time of inclusion and straight after the end of the intervention. CAT is a self-assessment instrument with eight items. Each item span from 0 to 5; a low score indicates that COPD has little impact on daily life. The questionnaire measures level of cough, phlegm, chest tightness, breathlessness, activity limitations at home, confidence leaving home, sleep and energy [Citation20,Citation21].
Statistical analysis
Data were analyzed using STATA 15 (StataCorp LLC. 2017. College Station, TX: USA). Demographic data were analyzed with descriptive statistical analysis. Changes in the total CAT score were analyzed using paired t-test, and the eight subscales in CAT with categorical variables were analyzed using Wilcoxon’s rank test.
We performed Poisson regression analysis on admissions and length of hospitalization for comparable time periods (from February to August) in 2013, 2014 and 2015. We adjusted for sex, age, FEV1 and affiliation to the CLT. It results in intercept s and estimates for the independent variables. Based on the collected data from the preceding years we predicted the number of future admissions and the length of hospitalization for 2016 by extrapolating data for each patient based on the assumption that the combined trends for 2013, 2014 and 2015 continued in 2016.
Using Poisson Regression model with repeated measures; we compared the predicted estimations with the observed numbers of admission and length of hospitalization in 2016.
Ethical considerations
The patients received oral and written information about the study. Patients who agreed to participate gave written informed consent before inclusion. The Danish Data Protection Agency in the Central Denmark Region approved the study (reference 1–16-02-451-15). The study did not involve biomedical interventions, thereby the Central Denmark Committee on Health Research Ethics did not find the study obligation to notify (reference 1–10-72-323-15). All collected data were anonymized. The data were processed, analyzed and stored in accordance with the provisions of the Danish Data Protection Agency.
Results
Patient characteristics
The final sample comprised 49 patients with COPD living in the Municipality of Aarhus.
Patients´ characteristics are presented in . The mean age was 71.7 years. Patients were primarily females (63.3%). Mean FEV1 was 34.5% of predicted values. Most patients had severe or very severe COPD and they were all stratified to Global Initiative for Chronic Obstructive Lung Disease (GOLD) group D as the pre-intervention CAT scores were between 12 and 31, and they had at least one hospitalization due to COPD or two exacerbations within the past year. GOLD D indicates a CAT score > 10 and a history of minimum two moderate exacerbations and/or one admission due to COPD within the past year [Citation17].
Table 1. Characteristics of patients (n = 49)
Patients were primarily living in their own residence (95.9%), two patients were living at a nursing home. Approximately half of the patients lived alone (53.1%). Nineteen (38.8%) patients received long-term oxygen therapy (LTOT). Eleven (22.5%) patients were still smokers, 37 (75.5%) patients were ex-smokers and only one patient was never smoker (2.0%).
Effect on CAT score
Means and p-values before and after the intervention are presented in . The data are categorical and paired. No significant differences were observed regarding the subscales: cough, chest tightness, breathlessness, limitation in activities at home, confidence in leaving home, capability of sleep, and level of energy before and after the intervention. Only phlegm showed a significant difference (p-value = 0.024). However, the means for all subscales were numerically lower after intervention than at baseline.
Table 2. Means before and after the intervention for the eight subscales in CAT (n = 49)
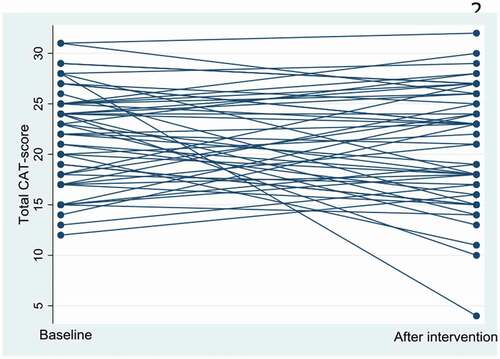
The results from the analysis of the total CAT score (continuous data) are shown in . shows the dispersion of the total CAT score before and after the intervention for each patient.
Table 3. Differences in total CAT score before and after the intervention
The mean difference in total CAT score before and after the intervention was 1.10 (95%CI −0.71; 2.91) and not statistically significant (p-value = 0.226, 95%CI −0.71; 2.91).
Effect on admission and contact to the CLT
The predicted admissions and length of hospital stays in 2016 were estimated for each patient using a Poisson regression model, including data from 2013 to 2015 and adjusted for age, gender, lung function and affiliation with the CLT as explanatory variables ().
Table 4. Observed and predicted numbers of admissions and length of hospital stay per patient
The observed number of admissions and length of hospitalization (mean days per admission) and the predicted number of admission and length of stay for 2016 are displayed in . A numerical trend for patients with COPD to be more hospitalized during the observation period was demonstrated, and the lengths of hospitalization to increase proportionally, except for the intervention period while patients were affiliated to the CLT in 2016.
Figure 3. Number of admissions and mean length of stay in days per admission
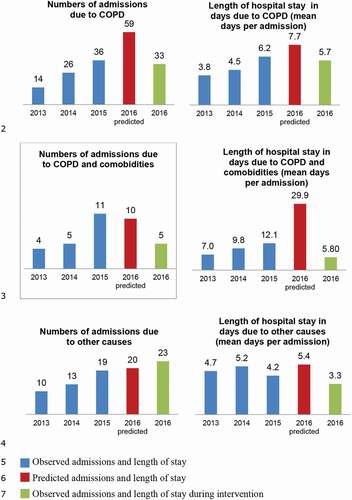
The results of the Poisson repeated analysis are presented in . The risk of being hospitalized based on the predicted number of admissions and length of stay was compared with the actual observed risk while affiliated to the CLT in 2016. While affiliated to the CLT, the actual observed risk of being hospitalized due to COPD was not statistically significantly lower than predicted (0.54 (95% CI 0.32; 0.90), p = 0.0192). The actual observed risk of a longer stay at the hospital due to COPD (0.41 (95% CI 0.22; 0.76), p = 0.0046) and COPD + comorbidities (0.10 (95% CI 0.03; 0.29), p < 0.0001) was statistically significantly lower than predicted.
Table 5. Number of observed admissions and length of hospitalizations versus predicted for 2016
Thirty-seven (76%) patients contacted the CLT during the intervention period. Twenty (61%) out of 33 hospital admissions due to COPD, happened in collaboration with the CLT. Four out of 5 admissions due to COPD and comorbidities occurred in collaboration with the CLT.
Discussion
To our knowledge, the present study is the first to evaluate the effects of a tailored CLT.
We hypothesized that affiliation with the CLT would reduce the number of COPD-related hospital admissions including readmissions and reduce the length of hospital stay. We found that affiliation to the CLT significantly reduced both the actual observed risk of being hospitalized due to COPD as well as the actual observed risk of a longer stay at the hospital when comparing with predicted values.
With usual care, the numbers of exacerbations and hospital admissions are expected to increase as time advances because COPD usually is a progressive disease [Citation22].
According to the National Danish COPD Registry (DRKOL), 23,334 Danish patients were hospitalized due to COPD exacerbation in 2016. The mean age was 73.3 years and 54% were women. Per patient, mean length of hospital stay per admission was 5.1 days. DRKOL represents all patients admitted with COPD nationwide and thus all degrees of disease severity from mild to very severe. For some patients it is their first admission while other patients have been hospitalized previously [Citation23].
The sample in this study had more severe COPD (GOLD group D) than in DRKOL on average. However, the observed mean length of hospital stay due to COPD was only 5.7 and was predicted to 7.7. This substantiates that affiliation with the CLT might decrease the number of COPD admissions as well as length of stay.
However, length of stay due to acute exacerbation in COPD varies with several factors such as age, severity of COPD, number and kind of comorbidities, carbon dioxide partial pressure and Body Mass Index [Citation24]. The length of stay generally varies from 4.5 to 13 days depending on exacerbation severity [Citation25–27]. If a patient was admitted to the Intensive Care Unit (ICU), the length of stay would increase further, as the average length of stay at the ICU is 4.48 days and the length of stay due to COPD exacerbation at the hospital is 11.63 days according to Brown et al [Citation28].
The study also showed that 40% of the admissions due to AECOPD happened without collaboration with the CLT. Although 76% of the patients at some point had contact to the CLT during the intervention some admissions might have been prevented if all the patients had contacted the CLT prior to an admission.
This pilot study, showed a numerical, but not statistically significant difference in CAT score from the time of inclusion (mean CAT score 21.96) to the end of the intervention (mean CAT score 20.86). The stratification into the four GOLD groups is based on the assessment of risk of exacerbation defined by a combination of the CAT score and exacerbation history. GOLD group D is defined by a CAT score equal to or exceeding 10 and at least 2 moderate exacerbations within the past year and/or at least one exacerbation leading to hospitalization. Although weak, the best predictor for future exacerbations is a history of previous events [Citation29].
The CAT was measured at the time of inclusion from September to February, during wintertime and again in August during late summer. This could introduce a bias in CAT scores, making comparison difficult as weather conditions might impact on symptoms. During winter, the number of symptoms and moderate exacerbations increases along with the number of COPD-related hospitalizations compared to summertime condition [Citation18,Citation19].
On the other hand, symptoms did not increase among patients while affiliated to the CLT. Indeed, total CAT score decreased numerically in all items, but were not statistically significant except for phlegm (from 2.86 to 2.47, p = 0.024). Because of the usual progressive nature, patients with COPD cannot expect any noticeable improvement in their symptoms as time advances – rather an increase [Citation29]. However, it cannot be ruled out that these findings merely represent seasonal changes – from winter to summertime. Furthermore, the Minimal Clinically Important Difference (MCID) in the CAT total score is estimated to two points [Citation30]. As CAT is comprised of eight items, you might divide the MCID of two points by eight. Hence, a MCID for each separate item might be 0.25. Based on this perspective the observed decrease in phlegm of 0.39 might be of clinical relevance. However, the MCID have not been estimated for the separate items in CAT.
The CLT integrates treatment at home and education, and it has been demonstrated in different studies that such interventions tend to reduce admissions. Studies showed that education concerning management of COPD reduces admissions [Citation10,Citation11]. However, Matsumura et al had only 11 men included in their study [Citation10], and Spiliopoulos et al.´s study relies on data from 1998 to 2006 and patients did not only receive education, but were also able to contact nurses by telephone if they had any symptoms resembling a COPD exacerbation [Citation11], Furthermore, a randomized controlled study including 177 patients indicated that two home visits regarding education about COPD and coping strategies concerning COPD, did not prevent readmission [Citation31]. This indicates that education alone might not be crucial for reducing admissions.
Another study investigating home visits from the local hospital every week and respiratory therapy and social service every 2 weeks reduced hospitalization and length of hospital stay [Citation32]. However, the study was based on 17 men only, and data were collected during 1985–1987 [Citation32]. Other studies showed that affiliating to a community special nursing team where patients received a personalized management plan and home visit or phone calls also decreased hospital admissions [Citation12–14], but one of these studies was based on a case study. Moreover, the contact between the nurses and the patient was often scheduled, whereas in our study contacts were conducted on the patient’s initiative. Hence, the findings in the above-mentioned studies adds to the likeliness that the observed effects in our study can be reproduced as the intervention is very comparable, although cross-sectorial and not mono-sectorial as most other interventions.
Strengths and limitations
The strength of this pilot study was that selection bias was low as only eight patients declined to be included in the study and all eligible patients were consecutively offered inclusion. the study, six patients declined the invitation for different reasons (e.g. the patients did not have surplus energy to be affiliated to the CLT, they did not find any need for affiliation to the CLT, or they preferred contacting their GP instead of the CLT). Nine died due to various causes as explained above. The 30-days mortality rate in Denmark is 10% and 25% 1 year after a COPD-related hospital admission [Citation16,Citation23]. In the present study, we observed a 6 months-mortality rate of 15%, which fit rather well with the national findings. It can be challenging to involve patients with COPD and encourage them to take action on their symptoms and contact the health professionals because patients with COPD often act late on their symptoms [Citation8]. Hence, our intervention might be suitable for patient with COPD as 76% contacted the CLT during intervention.
No diurnal or weekend variation pattern regarding hospitalization was revealed. This might be due to the fact, that individual patient action plans were made during daytime whenever needed. Additionally, patients had easy access to virtual and/or physical contact for advice and help 24/7.
A few limitations should also be acknowledged. Firstly, the patients were included consecutively from September 2015 to February 2016. This is a potential confounder as some patients had more time to adjust to the CLT than others. On the other hand, if a patient had no need to contact the CLT from the beginning, he or she might forget to use this possibility later on. Secondly, data on hospitalizations and length of stay were only compared with historical data from the same patients as no control group was included. As the sample size was small, it was not suitable for randomization. Therefore, we found it appropriate to compare the sample with its own historical data from the preceding years – thus making each patient their own control. Furthermore, due to the small sample size we decided to predict the number of admissions and length of stay using a Poisson regression model with repeated measures and compare the observed data with the predicted data. The use of historical data from the preceding 3 years will tend to equal out random deviations. Although the lack of a control group is a study limitation. Thirdly, the intervention lasted for 6 months only. The patients were observed during springtime and summertime. The observed rate of exacerbation might be lower than the rate of exacerbation in wintertime, as the number of exacerbations in Denmark, as in most Nordic countries, increase during wintertime compared to summertime [Citation18,Citation19]. Therefore, it makes sense that the observed period is the same for all the years included in the study.
Fourth, we did not perform any power calculation prior to the study, which might have been relevant for the analysis – especially in relation to CAT-score. However, this study was a pilot designed to investigated the feasibility and safety of patient affiliated to the CLT.
Conclusions
To our knowledge, this is the first study to evaluate the effects of a tailored CLT. The results demonstrate that affiliation to a CLT statistically significant reduced both the actual observed risk of being hospitalized due to COPD as well as the actual observed risk of a longer stay at the hospital when comparing with predicted values.
In addition, a numerical statistically non-significant difference in quality of life before and after intervention was observed.
Based on the results, establishing a CLT was feasible and seems to be safe for patients at risk of AECOPD.
However, a larger and longer randomized controlled study is needed to establish these findings.
Acknowledgments
The authors would like to acknowledge funding from the Municipality of Aarhus and Aarhus University Hospital.
The authors would also like to acknowledge the support and expertise provided by Michael Ibsen and Rikke Ibsen in the statistical analysis of the results.
Disclosure statement
The authors have no conflict of interest to declare.
Additional information
Funding
Notes on contributors
Birgit Refsgaard Iversen
Birgit Refsgaard Iversen RN, MLP, MScN is a PhD student and a Clinical Nurse Specialist in pulmonary diseases at the Department of Respiratory Diseases and Allergy at Aarhus University Hospital, Denmark.
Lotte Ørneborg Rodkjær
Lotte Ørneborg Rodkjær RN, MPH, PhD, associated professor at Faculty of Health, Aarhus University and Department of Infectious Diseases, Aarhus University Hospital. She is Deputy Head at Research Centre for Patient Involvement Aarhus University, Denmark.
Vibeke Bregnballe
Vibeke Bregnballe RN, MHH, PhD, part-time associate professor at Faculty of Health, Aarhus University, Denmark.
Anders Løkke
Anders Løkke MD and associate professor at Department of Regional Health Research, University of Southern Denmark. He is a consultant in pulmonary diseases and specialised in COPD at The Department of Medicine, Vejle, Hospital Little Belt, Denmark.
References
- Sundhedsstyrelsen. Anbefalinger for tværsektorielle forløb for mennesker med KOL. 2017 [cited 2020 May 15]. Available from: https://www.sst.dk/da/udgivelser/2017/~/media/8365DCEC9BB240A0BD6387A81CBDBB49.ashx
- Dansk Register for Kronisk Obstruktiv Lungesygdom. National årsrapport 2018. 2019 [cited 2019 Dec 21]. Available from: https://www.sundhed.dk/content/cms/90/4690_drkol-aarsrapport-2018_offentlig.pdf
- Dansk Register for Kronisk Obstruktiv Lungesygdom. Appendiks til National årsrapport 2018. 2019 [cited 2019 Dec 21]. Available from: https://www.sundhed.dk/content/cms/90/4690_appendix_drkol-aarsrapport-2018_05052019_offentlig.pdf
- Sundheds- og ældreministeriet. Kommunernes Landsforening, Danske Regioner, Nationale mål for Sundhedsvæsnet. 2016 [cited 2019 Dec 21]. Available from: https://www.sum.dk/Aktuelt/Publikationer/~/media/Filer%20-%20Publikationer_i_pdf/2016/Nationale-maal/SUM-Nationale-maal-L-april-2016.ashx
- Kompetencecenter for Patientoplevelser. Den Landsdækkende Undersøgelse af Patientoplevelser 2018. 2018 [cited 2019 Dec 21]. Available from: https://patientoplevelser.dk/files/lup_somatik_2018_national_rapport_1.pdf
- Witzel S, Nielsen PB, Jensen M. Patienternes perspektiv på kronisk sygdom – oplevelser på tværs af sundhedsvæsenet i Region Midtjylland. CFK - Folkesundhed og Kvalitetsudvikling; 2012. [cited 2020 May 21]. Available from: http://www.defactum.dk/publikationer/ShowPublication?id=421&pageId=309986
- Rasmussen L, Ølsgaard G. Forslag til kvalitetsforbedringer fra patienter og fagpersoner i indsatsen for kronisk syge - en opfølgning på rapporten ”Patientens perspektiv på kronisk sygdom”. CFK - Folkesundhed og Kvalitetsudvikling; 2014. [cited 2020 May 21]. Available from: http://www.defactum.dk/publikationer/ShowPublication?id=435&pageId=309986
- Martin HM, Borst L Sammenhæng i tværsektorielle KOL - forløb. En undersøgelse af patient er og pårørendes oplevelser. KORA - Det Nationale Institut for Kommuners og Regioners Analyse og Forskning; 2013. [cited 2020 May 21]. Available from: https://www.vive.dk/media/pure/9106/2043881
- Rea H, McAuley S, Stewart A, et al. A chronic disease management programme can reduce days in hospital for patients with chronic obstructive pulmonary disease. Intern Med J. 2004;34(11):608–10.
- Matsumura T, Takarada K, Oki Y, et al. Long-term effect of home nursing intervention on cost and healthcare utilization for patients with chronic obstructive pulmonary disease: a retrospective observational study. Rehabil Nurs. 2015;40(6):384–389.
- Spiliopoulos N, Donoghue J, Clark E, et al. Outcomes from a respiratory coordinated care program (RCCP) providing community-based interventions for COPD patients from 1998 to 2006. Contemp Nurse. 2008;31(1):2–8.
- Titova E, Steinshamn S, Indredavi B, et al. Long term effects of an integrated care intervention on hospital utilization in patients with severe COPD: a single centre controlled study. Respir Res. 2015;16:8–18.
- Lee G, Pickstone N, Facultad J, et al. The future of community nursing: hospital in the home. Br J Community Nurs. 2017;22(4):174–180.
- Ward S, Barnes H, Ward R. Evaluating a respiratory intermediate care team. Nurs Stand. 2005;20(5):46–50.
- Zwar NA, Hermiz O, Comino E, et al. Care of patients with a diagnosis of chronic obstructive pulmonary disease: a cluster randomised controlled trial. Med J Aust. 2012;197(7):394–398.
- Løkke A, Dahl R, Lange P, et al. Danske KOL-Guidelines. Dansk Lungemedicinsk Selskab; 2012.
- Global initiative for chronic obstructive lung diseas. Global strategy for diagnosis, management, and prevention of COPD – 2016; 2016.
- Jenkins CR, Celli B, Anderson JA, et al. Seasonality and determinants of moderate and severe COPD exacerbations in the TORCH study. Eur Respir J. 2012;39(1):38–45.
- Rabe KF, Fabbri LM, Vogelmeier C, et al. Seasonal distribution of COPD exacerbations in the prevention of exacerbations with tiotropium in COPD trial. Chest. 2013;143(3):711–719.
- GlaxoSmithKline. CAT COPD assesment test; 2009.
- Jones P, Jenkins C, Bauerle O. Healthcare professional user guide. CAT COPD Assesment Test; 2012.
- Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138.
- Dansk Register for Kronisk Obstruktiv Lungesygdom. Appendiks til National årsrapport 2016. 2017.
- Crisafulli E, Lelpo A, Barbeta E, et al. Clinical variables predicting the risk of a hospital stay for longer than 7 days in patients with severe acute exacerbations of chronic obstructive pulmonary disease: a prospective study. Respir Res. 2018;19(1):261–263.
- Tsimogianni AM, Papiris SA, Stathopoulos GT, et al. Predictors of outcome after exacerbation of chronic obstructive pulmonary disease. J Gen Intern Med. 2009;24(9):1043–1048.
- Parikh R, Shah TG, Tandon R. COPD exacerbation care bundle improves standard of care, length of stay, and readmission rates. Int J Chron Obstruct Pulmon Dis. 2016;11:577–583.
- De la Iglesia F, Valino P, Pita S, et al. Factors predicting a hospital stay of over 3 days in patients with acute exacerbation of chronic obstructive pulmonary disease. J Intern Med. 2002;251(6):500–507.
- Brown H, Dodic S, Goh SS, et al. Factors associated with hospital mortality in critically ill patients with exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:2361–2366.
- Global Initiative for Chronic Obstructive Lung, D. Global strategy for diagnosis, management, and prevention of COPD – 2019; 2019.
- Kon SS, Canavan JL, Jones SE, et al. Minimum clinically important difference for the COPD Assessment Test: a prospective analysis. Lancet Respir Med. 2014;2(3):195–203.
- Hermiz O, Comino E, Marks G, et al. Randomised controlled trial of home based care of patients with chronic obstructive pulmonary disease. BMJ (International Edition). 2002;325(7370):938–940.
- Haggerty MC, Stockdale-Woolley R, Nair S. Respi-Care: an innovative home care program for the patient with chronic obstructive pulmonary disease. Chest. 1991;100(3):607–612.