ABSTRACT
We herein report a rare case that describes and visualizes nocardiosis in a patient with diabetes. The patient presented with recurring fever, gout, leg pain, frailty and muscular pain through nine months, before a core needle biopsi, from an abscess in the abdominal musculature, revealed Nocardia Paucivorans. A PET-CT-scan showed multiple muscular FDG-positive sites. Furthermore, he experienced serious side effects to Sulfametoxazole and Trimethoprim, the antibiotic of choice for this type of infection. He was then switched to Moxifloxacin and Ampicillin. Nocardia often presents as opportunistic infections, typically in patients with severe immunodeficiencies, such as HIV, use of high-dose corticosteroids, hematologic malignancies or immunosuppression following organ transplantation. This case illustrates how a patient with only relative immunodeficiency gets rare nocardiosis. Our sparse knowledge on clinical presentation is based on case-reports and treatment is empirical. Hence, a better understanding of the clinical presentation and treatment is important. Especially given the prospect, that the health care system faces a greater load of patients with diabetes and other immunodeficiencies in the future.
Introduction
This case report describes and visualizes infection with Actinomyces Naeslundii (AN) and Nocardia Paucivorans (NP), causing lung infection and multiple muscular abscesses, respectively.
Case-report
A 78 year old male, with a medical history of hypertension, atrial fibrillation, arthritis urica, insulin-dependent type-2-diabetes complicated by diabetic nephropathy and former cancer prostate, for which he had undergone treatment, was initially admitted in September 2018. He presented a history, over the past six months, of recurring fever, gout, leg pain, frailty, alongside muscular pain from right humeral, and abdominal musculature.
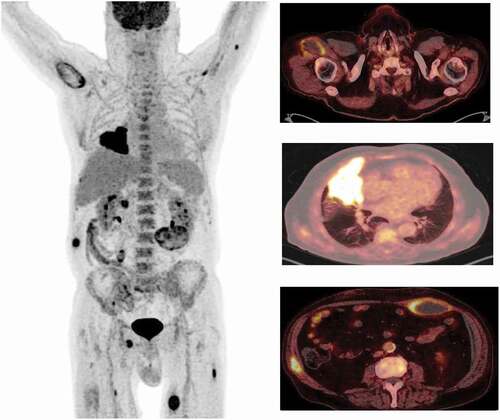
The initial diagnostic CT-imaging showed a pulmonary infiltrate. The patient responded clinically and biochemically on antibiotic treatment, however, a 6 week control scan showed progression of the infiltrate. Hence, the patient underwent additional diagnosing with PET-CT, bronchoscopy, and core needle biopsy (CNB). PET-CT showed multiple muscular abscesses (). AN was found in fluid from bronchoalveolar lavage and CNB from the lung did not confirm malignity. Only CNB from the abdominal musculature was positive for bacterial growth, namely NP. The patient was HIV negative and had normal levels of immunoglobulins.
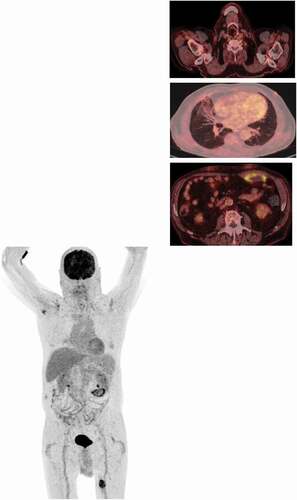
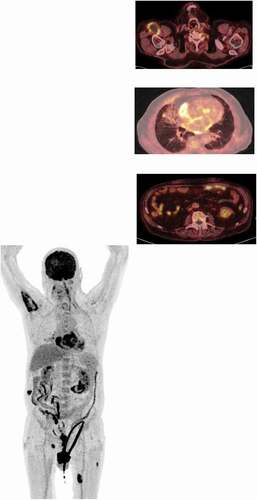
During medical examinations, the patient was treated with Piperacillin/Tazobactam and Metronidazole. After discovering NP, antibiotic treatment was adjusted to Sulfametoxazole and Trimethoprim (STM). However, three weeks later, the patient was submitted with bradycardia, acute kidney failure and myelosuppression, most likely side effects to STM. After normalization of bone marrow function, the antibiotic strategy was changed to Amoxicillin and Moxifloxacin. Regular PET-CT and blood sampling over additionally nine months showed sporadic and slowly regression of the abscesses. A year after first submitted the patient was without any muscular complaints. This lead to pause of antibiotics, which two months later, resulted in progression of the original lung foci. BAL was now positive for Actinomycis Odontolyticus (AO), which in writing, is treated with high doses of penicillin.
Discussion
This patient was infected with both AN and NP. Pulmonary infection with AN is likely due to aspiration of infected oral material, given this agent’s natural presence in the mucosal barrier of the oral cavity. It is likely that the AO infection of the lung was acquired through the first bronchoscopy. Conversely, Nocardia normally thrives in organic matter, and human infections are acquired by either inhalation or skin laceration [Citation1]. We suspect the latter to have been the way of contamination, since Nocardia was found in the abdominal rectus musculature, suggesting, that the patient has used a contaminated needle during insulin administration.
Both AN and NP are capable of hematogen spread and can present with abscesses and fever. The presence of NP could only be identified in the abdominal abscess, so whether we have to do with disseminated NP or AN infection in this case, is difficult to say. PET-CT scans show a relatively quick pulmonary response to antibiotic treatment, compared to a generally more vague response in the muscular foci (). These circumstances lead us to suspect disseminated NP infection. However, we cannot exclude that AN has been the cause of fever for this patient in some cases.
Figure 2. PET-CT, March 2019. Note the quick pulmonary response, against the more vague muscular response
Malignancy is a relevant differential diagnosis to infections with low pathogenic microorganism such as fungi, mycobacteria or, as in this case, actinomycetales. Clinically it can be hard to distinguish between them. The brief clinically and biochemically response to antibiotics in this case, together with PET-CT scans, supports the infection suspicion. If the physician suspects infection with the above-mentioned pathogens, the microbiological department must be notified, since these pathogens need either special media, circumstances (temperature, pH etc.) or longer time for growth.
Nocardia often presents as opportunistic infections, typically in patients with severe immunodeficiencies, such as HIV, use of high-dose corticosteroids, hematologic malignancies or immunosuppression following organ transplantation. But infections in immunocompetent patients and lung colonization in patients with COPD have been described [Citation2,Citation3]. The comorbidities of this patient are causing a relative immunodeficiency making him vulnerable to be infected with both AN and NP. Especially his diabetes must be considered a lead actor in this vulnerability, given that diabetes impairs the cellular immune system, which is vital for successful clearance of Nocardia infections [Citation4].
Regarding prognosis, a review from 2020 presents, that for pleuropulmonary Nocardia infection approximately 80% are cured and only 3% with disseminated nocardiosis are cured [Citation5].
This case illustrates how a patient with a common diagnosis such as diabetes gets infected with two opportunistic bacteria. Especially NP is rare. In addition, he did not tolerate first-line antibiotics for this type of infection. Our sparse knowledge on clinical presentation is based on case-reports and treatment is empirical. Hence, a better understanding of the clinical presentation is important, especially given the prospect, that the health care system faces a greater load of patients with diabetes and other immunodeficiencies in the future.
Disclosure statement
The authors report no conflict of interest.
Additional information
Notes on contributors
Cecilie Norup Thomsen
Cecilie Norup Thomsen, MD. Is a physician at the Department of Internal Medicine and Respiratory Diseases, at Holstebro Hospital, Hospital Unit West, Denmark.
Søren Sperling
Søren Sperling, MD. Is a physician, taking his rehsidency in Internal Medicine and Respiratory Diseases at Department of Internal Medicine, Holstebro Hospital, Hospital Unit West, Denmark and Department of Respiratory Diseases Aarhus University Hospital, Denmark.
Joan Fledelius
Joan Fedelius, MD, PhD. Is a senior doctor with specialty in Radiology, working at the Department of Nuclearmedicine, Herning, Hospital Unit West.
Pia Holland Gjørup
Pia Holland Gjørup, MD, PhD. Is a senior doctor with specialty in Internal Medicine and Respiratory Diseases, working at the Department of Internal Medicine, Holstebro, Hospital Unit West, Denmark
References
- Warren NG. Actinomycosis, nocardiosis and actinomycetoma. Dermatol Clin. 1996 Jan 1;14:85–95.
- Gray TJ, Serisier DJ. Nocardia paucivorans – a cause of disseminated Nocardiosis. J Infect. 2007 Feb 1;54(2):e95–5.
- Aliaga L, Fatoul G, Guirao E, et al. Nocardia paucivorans brain abscess. Clinical and microbiological characteristics. IDCases. 2018 Jul;4(13):e00422.
- Lin YJ, Yang KY, Ho JT. Nocardial brain abscess. J Clin Neurosci. 2010;17:250–253.
- Rathish B, Zito PM Nocardia. StatPearls Publishing; 2020 Sep 29.