Abstract
Background: Lung cancer is the leading cause of cancer death worldwide, but the additional economic burden regarding direct and indirect costs is largely unknown. This study provides information on the economic consequences of lung cancer on a national level.
Methods: From the Danish National Patient Registry (NPR) and the Danish Civil Registration System (CPR), 53,749 patients with lung cancer were identified and matched with 214,304 controls on age, gender, region of residence and marital status in the period 1998–2010. Direct and indirect costs, health care contacts and frequency, medication and social transfer payments were extracted from national databases.
Results: Direct health care cost were higher for lung cancer patients than controls both before and after being diagnosed with lung cancer. At the year of diagnosis, health care cost peaked with cost of €21,497 compared to €2,880 for controls. Average difference in income from employment was €+3,118 in years prior to diagnosis and €+748 after diagnosis in favor of controls. Average difference in total public transfer income was €+1,288 before and €+441 after diagnosis, with higher public transfer income for lung cancer patients.
Conclusion: For both genders, lung cancer was associated with significantly higher rates of health-related costs, medication costs, public transfer income, social transfer payments and significantly lower income from employment until retirement (age 65).
Introduction
World-wide, lung cancer is an important public health and economic burden with high mortality and morbidity [Citation1]. Lung cancer is the leading cause of cancer-related death and the incidence of lung cancer has rapidly increased since the beginning of the 20th century. Lung cancer accounts for 11.6% of the total cancer cases, but 18.4% of cancer deaths in 2018 in Europe [Citation1]. Lung cancer is currently the most frequent cancer type in men, and is second to breast cancer in women in Denmark [Citation2].
Cost-of-illness studies are key to informing cost-effectiveness evaluations, informing policy decisions for cancer control and improving public health. The burden of lung cancer on the health care system is substantial and studies have demonstrated high health care costs of lung cancer. Annual US direct costs of lung cancer were estimated at 4.9 USD billion in 1996 [Citation3], 3.35 USD billion in the European Union in 2011 [Citation4] and accounts for estimated 20% of all cancer cost [Citation5]. Previous studies have been based on smaller samples and extrapolated to national and international levels. Cost-of-illness studies measure the economic burden resulting from disease and illness across a defined population, and include direct and indirect costs. Direct costs include hospitalization, outpatient treatment and medication. Indirect costs represent the value of economic resources lost because of disease-related work disability or premature death. It is important to distinguish costs from monetary transfer payments such as disability and welfare payments. These payments represent a transfer of purchasing power to the recipients from the general taxpayers, but do not represent net increases in the use of resources and, therefore, are not included in the total cost estimate.
In Denmark, government-funded public health-care and individual-level linkage, have led to establishment of longitudinal population-based national registries [Citation6]. The extensive Danish registries provide unique possibility to calculate direct and indirect cost of all lung cancer patients. A study of total cancer costs across the European Union in 2009 found that the economic burden of lung cancer in Denmark, was similar to the average burden across the European Union [Citation7]. Thus, results from this study should be comparable to countries with similar health care systems.
We hypothesized, that a lung cancer diagnosis would result in a significant increase in health-related costs as well as significant changes in income from employment as well as from public transfer compared to matched controls. Our aim was to provide detailed population-based estimates of the health system costs for lung cancer care using linked patient-level data. Since the included lung cancer patients are compared to a control group, we estimated the incremental cost of lung cancer on a national level, which has not previously been reported.
Methods
The National Patient Registry (NPR) is a time-based national database that contains data from all in- and outpatient contacts. In the NPR, all hospital contacts in Denmark, including primary and secondary diagnoses are registered. The NPR includes administrative information, diagnoses, and diagnostic and treatment procedures using the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) [Citation8]. All contacts to the primary sector (general practice and specialist care) and the use of medications are recorded in the databases of the National Health Security and the Danish Health and Medicines Agency, respectively. We extracted the following first time primary or secondary diagnoses from the NPR in the time period 1998–2010: ‘C34 Malignant neoplasm of bronchus and lung’. Data on the disease stage were not available.
The Danish Civil Registration System (CPR) contains data on all Danish citizens including social factors, employment status, income, marital status etc. by linkage to the Danish Income Statistics [Citation9]. From the Danish Civil Registration System, each lung cancer patient was matched with four controls of the same gender, age and geographical area as the patient. The 14 Danish ‘amter’ were used as geographic units with an average of 388.000 persons. Neither the NPR nor any of the other national databases contains information about smoking status. Social compensation was performed by selecting control subjects residing in the same area of the country as the patients and with the same marital status. Municipal services such as care of the elderly (home care nursing and general home care) and municipal rehabilitation are not included as they are paid by the municipals. At present it is not possible to retrieve these data from any register. Patients and matched controls who could not be identified in the Income Statistics database were excluded.
Lung cancer patients and matched controls were followed from 1998 to 2010 or until death. If a patient or control was not present in the registry on 1st of January each year due to death, imprisonment or immigration, the corresponding controls or patient were not included in the dataset for that year. If diagnosis of lung cancer of any given individual was made in the first year (1998), we were able to follow that individual 11 years forward in time to see what happened after diagnosis. If a diagnosis of lung cancer of any given individual was made in the last year (2010), we were able to follow that individual 11 years backwards in time. If a diagnosis of lung cancer of any given individual was made between the first and the last year, we were able to follow that individual both backwards and forward in time. Controls were equally followed forwards and backwards in time from the matched lung cancer patient diagnosis and this method has previously been described [Citation10–12].
The economic burden of lung cancer was estimated by determining the annual costs per patient diagnosed with lung cancer, which was then compared to the average healthcare costs for the corresponding matched controls. The health cost was then divided into annual direct and indirect healthcare costs. Direct costs included the average national costs of hospitalization and outpatient treatment weighted by use, for separate diagnosis-related groups (DRG). These costs were all calculated from Danish Ministry of Health data using DRG as average case-mix costs of hospitals or outpatient costs updated on a yearly basis. The costs and use of drugs were obtained from the Danish Health and Medicines Agency consisting of the retail price of each drug (including dispensing costs) multiplied by the number of transactions. The costs and frequencies of consultations with general practitioners and other specialists were based on National Health Security data. Indirect costs per patient and for the corresponding matched controls included those related to reduced unemployment benefits and to social transfer payments. In Denmark, social transfer payments comprise income derived from government funds. These payments include pensions, social security, subsistence allowances, social assistance, publicly funded personal support for education, and others. Indirect costs were based on income data from Income Statistics. Costs were measured on a yearly basis and adjusted to 2010 prices using statistic Denmark’s general price index for all costs. All costs were measured in DKK and converted to Euros (€1:DKK 7.45).
Data were anonymized and neither ethical approval or individual consent were required. Statistical analysis was performed using SAS 9.1.3 (SAS, Inc., Cary, NC). Statistical significance of the cost estimates was assessed by nonparametric bootstrap analysis. A significance level of 0.05 was assumed for all tests.
Results
We identified 53,749 patients with lung cancer form the national databases (1998–2010). More than 99% of the observations in the two groups were successfully matched. Age distribution, marital status, survival and comorbidity of lung cancer patients and matched controls have previously been published [Citation13]. Lung cancer was associated with significantly higher rates of health care related costs, medication use and lower income rates compared to the matched control group before and increasingly so after being diagnosed with lung cancer (). For both genders, lung cancer was associated with significantly higher rates of public transfer income, social transfer payment and significantly lower income from employment until retirement age (65-years). Direct health cost of lung cancer patients before being diagnosed with lung cancer was €2,658 (€1,952 for controls), compared to €15,464 after diagnosis (€3,229 for controls).
Table 1. Health costs and income before and after diagnosis of lung cancer for cases and controls. Yearly average costs per person. N = summarized number of individuals × years observed. P-value from bootstrapped t -test. The values given are in euros (€)
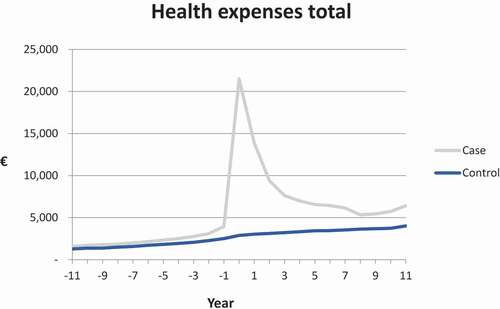
Total health expenses (costs related to outpatient clinics, hospital, primary health care and medication) before and after diagnosis of lung cancer compared with controls are shown in . The health-related costs were higher for lung cancer patients than for controls in the entire study period, including prior to diagnosis of lung cancer. For lung cancer patients, a peak in health-related costs was seen at the time of diagnosis (€21,497 compared to €2,880 for controls). After diagnosis the differences between lung cancer patients and controls reduced. Caution is mandatory when comparing one year with another in , as neighboring years are not identical. At year −11, only lung cancer patients diagnosed in 2010 are present, year −10 patients diagnosed in 2009 and 2010 and so on.
Figure 1. Total health expenses in euros (€) for lung cancer patients (cases – green) compared to controls (blue) before and after being diagnosed with lung cancer
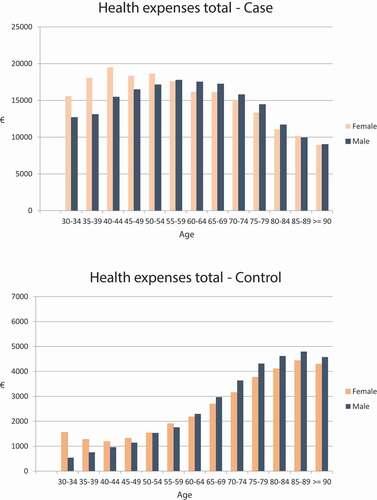
displays total health care costs for lung cancer patients and controls distributed by age and gender. In the control group, health expenses grew with age, whereas for lung cancer patients the costs declined with age after 50 years of age.
Figure 2. Health costs of lung cancer patients and controls in euros (€) distributed by age and gender
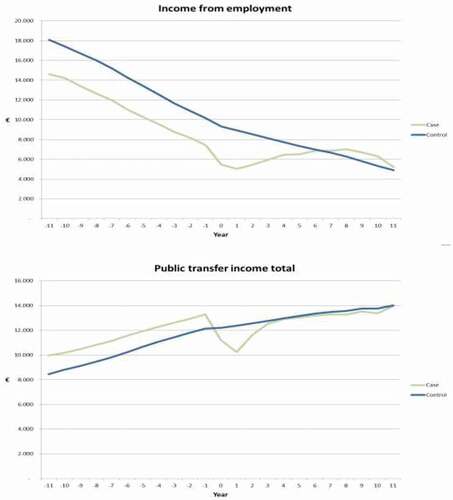
The average income from employment was significantly lower and the total public transfer income was significantly higher among lung cancer patients compared to controls – even 11 years before being diagnosed (). The difference in income from employment was stable until one year prior to diagnosis. Average difference in employment income between cases and controls were €3,118 in years prior to being diagnosed, and €748 after diagnosis with lung cancer, in favour of controls. Average difference in total public transfer income was €1,288 before and €441 after diagnosis, in favour of cases. Statistical calculations in supplementary data.
Discussion
The present study provides information on the incremental health care cost of lung cancer patients on average before and after being diagnosed with lung cancer. Average total health-related costs were higher for lung cancer patients both before and after being diagnosed with lung cancer with an expected peak around diagnosis and treatment. The total costs of diagnosing and treating a person with lung cancer was approximately €35,386 based on the excess costs in year 0 and 1 as we assume that these were by far attributable to lung cancer. Indirect costs were higher for lung cancer patients than for controls throughout the study period. For all ages and both genders, lung cancer was associated with significantly higher rates of health-related costs. Of greatest importance was inferior employment income prior to being diagnosed with lung cancer compared to the age- and gender matched, but not socioeconomic matched controls.
Lung cancer has been found to constitute 15% of all cancer costs in the European Union in 2008 in a large study from national databases [Citation7]. In-hospital treatment constitutes the main part of the total health cost before and after diagnosis. Direct costs have previously been evaluated in several studies including European studies. Migliorino et al. reported the direct cost of treating a lung cancer patient with chemotherapy in Italy over a 16-month period to be €25,859 (191 patients included) [Citation14]. Furthermore, Andreas et al. found the total direct cost to be €19,057 in France (and lower in Germany and the UK) over 26-months for stage IB-IIIA resected non-small cell lung cancer (NSCLC), however only 306 patients were included [Citation15]. A retrospective questionnaire survey from China report the average cost to be 42,540 USD per patient, looking at 195 surviving lung cancer patients [Citation16]. In our study, all lung cancer patients at all staged were included thus making it more comprehensive as well as true nationwide and population based. Furthermore, we estimate incremental health care costs over time before and after being diagnosed. The Danish Center for Health Economics has estimated the cost of cancer in a Danish report over the same period in time and found similar results; however, cost of medication not provided by hospitals were not included [Citation17]. A study by Luengo-Fernandez et al. reported an incremental cost of lung cancer of €8 per citizen in the European Union compared to 10€ per citizen in Denmark [Citation7]. Thus, the result of this study can be of value for other similar countries as Danish lung cancer expenses are comparable to other European countries. A few studies have described incremental costs of lung cancer by comparing to a matched control group. In Australia, the healthcare system includes government-funded universal coverage of many medical costs, however less comprehensive than the Danish, and incremental direct costs have been estimated at AU$51,944, excluding patients with previous cancer in their study [Citation18].
This study reveals that lung cancer patients had lower income from employment and higher public transfer income several years prior to being diagnosed with lung cancer. These differences might be partly explained by smoking (and the comorbidities that follow). This represents an important source of bias and ideally, we would have adjusted for smoking status. We found the average difference in employment income between cases and controls less substantial after diagnosis, where lung cancer patients had a higher average employment income. As the control group is getting older, a larger portion reached retirement age and the differences evens out due to public pension paid to all Danish citizens above 65 years. Correspondingly, we found a reduction in the difference in public transfer income in favour of the lung cancer patients, as a result of the control group receiving pension. Public funded sick pay was substantially higher for lung cancer patients compared to controls even before, but increasingly so after diagnosis. This corresponds to lung cancer patients higher burden of comorbidity [Citation13,Citation19,Citation20].
Few studies have included indirect costs in economic evaluations of lung cancer. A study from Greece including 128 patients with lung cancer, who were followed for 32 months, found a loss of productivity of 27,050 days for patients in total [Citation21]. In a study from Spain [Citation22], productivity losses summed €13.1 billion over a 10-year period. When evaluating the economic burden of lung cancer, The European Respiratory Society (ERS) reported a cost of 1,873,000 disability-adjusted life-years (DALYs) equivalent to over €100 billion in disability and premature mortality. A higher economic burden than in patients with COPD – accounting for approximately €93 billion a year [Citation4]. However, in Denmark, where health care is governmentally funded, the Health Authorities reports the overall costs of lung cancer as being negative. As lung cancer patients die early, future health care expenses and pensions are calculated as future savings to the government [Citation23].
Strengths and limitations
This study has several important strengths. We used data from large population-based registers for the whole nation and over a 12-year period and matched cases with four controls to give more robust results. However, this epidemiologic study is exclusively based on information from national databases leading to some limitations and potential bias. In Denmark, the ICD-10 classification is used only in the secondary health-care sector. However, the vast majority of lung cancer patients are diagnosed and primarily treated in the secondary sector and classified by ICD-10. In this study, all lung cancer patients were lumped together without paying attention to disease stage as this information was not included. Previous studies have found that direct medical costs per patients with NSCLC increases with disease stage [Citation24,Citation25] and with disease progression [Citation14]. The Danish Lung Cancer Registry (DLCR) holds information on staging, histology, performance-, and smoking status for most patients [Citation26,Citation27], and linking the present work with this registry, would have added valuable information. However, the present study contains data on lung cancer patients prior to the establishment of the DLCR. Marital status and income were available, but degree of educational level was not included in this study. Matching on education or income, would have excluded a significant number of cases and controls, due to missing information. Van der Heyden et al. described important socioeconomic inequalities to exist among patients with lung cancer; thus, it would be relevant to adjust for education [Citation28]. However, our epidemiological study on tuberculosis in a similar Danish setting found that adjusting for education did not change the results [Citation29].
Significant improvements in the medical management of lung cancer (especially NSCLC) have been observed over the last 10 years due to new treatment therapies and more comprehensive follow-up regiments [Citation30]. We expect the direct cost of lung cancer treatment to be even higher at present time and in the future, due to more treatment options since this study ended as well as longer average overall survival.
Conclusion
This study provides unique information on the incremental economic burden of lung cancer on a national level with both direct and indirect costs. We found higher rates of direct health care costs prior to and increasingly so after the diagnosis of lung cancer compared to matched controls. For both genders, lung cancer was associated with significantly higher rates of health-related costs, medication use, public transfer income, social transfer payment and significantly lower income from employment until retirement age as compared to matched controls.
This study confirms previously reported levels on the financial burden of lung cancer, with detailed evaluation of indirect cost not formerly evaluated.
Declarations
No consent or ethical approval was required for this study. All authors consent for the publication. All authors declare no conflict of interests or competing interest. All data are available upon request to corresponding author. No funding has been granted to this research project. All authors meet the ICMJE criteria for authorship. AG, AL, JR and OH contributed to the design of the study. NL and TR contributed to the interpretation of the results. RI performed the statistical analysis and prepared tables and figures. AG was responsible for drafting the manuscript, and all of the authors provided critical review of drafts and approved the final version submitted for publication.
Supplemental Material
Download MS Word (18.2 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed here
Additional information
Notes on contributors
Anja Gouliaev
Anja Gouliaev, MD, clinical doctor at the department of Respiratory Medicine and Allergy at Aarhus University Hospital, Denmark.
Jeyanthini Risikesan
Jeyanthini Risikesan, MD, PhD, clinical doctor at the department of Respiratory Medicine and Allergy at Aarhus University Hospital, Denmark.
Niels Lyhne Christensen
Niels Lyhne Christensen, MD, PhD, associated professor at the department of Respiratory Medicine and Allergy at Aarhus University Hospital, Denmark.
Torben Riis Rasmussen
Torben Riis Rasmussen, MD, PhD, associated professor at the department of Respiratory Medicine and Allergy at Aarhus University Hospital, Denmark.
Ole Hilberg
Ole Hilberg, MD, PhD, professor at the department of Medicine, Lillebaelt Hospital, Vejle, and Department of Regional Health Research, University og Southern Denmark, Odense, Denmark.
Rikke Ibsen
Rikke Ibsen, cand.scient, i2minds, Møllegade 32, 8000 Aarhus C, Denmark.
Anders Løkke
Anders Løkke, MD, associated professor at the department of Medicine, Lillebaelt Hospital, Vejle, and Department of Regional Health Research, University og Southern Denmark, Odense, Denmark.
References
- GLOBOCAN https://gco.iarc.fr/
- NORDCAN https://www-dep.iarc.fr/nordcan/dk/frame.asp
- Brown ML, Riley GF, Schussler N, et al. Estimating health care costs related to cancer treatment from SEER-medicare data. Med Care. 2002;40(8suppl):IV-104-IV-117.
- ERS. The economic burden of lung disease. In: Gibson GJ, Loddenkemper R, Sibille Y, et al., editors. European lung white book. UK: European Respiratory Society; 2013. p. 16–8.
- Goodwin PJ, Shepherd FA. Economic issues in lung cancer: a review. J Clin Oncol. 1998. Dec;16(12):3900–3912. Review.
- Olsen J, Brønnum-Hansen H, Gissler M, et al. High-throughput epidemiology: combining existing data from the Nordic countries in health-related collaborative research. Scand J Public Health. 2010;38(7):777–779.
- Luengo-Fernandez R, Leal J, Gray A, et al. Economic burden of cancer across the European union: a population-based cost analysis. Lancet Oncol. 2013 Nov;14(12):1165–1174.
- Schmidt M, Schmidt SAJ, Sandegaard JL, et al. The Danish national patient registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490.
- Pedersen CB. The Danish Civil Registration System. Scand J Pulic Health. 2011;32:183–190.
- Løkke A, Hilberg O, Tønnesen P, et al. Direct and indirect economic and health consequences of COPD in Denmark: a national register-based study: 1998-2010. BMJ Open. 2014 Jan 6;4(1):e004069.
- Rittig AH, Hilberg O, Ibsen R, et al. Incidence, comorbidity and survival rate of hypersensitivity pneumonitis: a national population-based study. ERJ Open Res. 2019 Oct 21;5(4):00259–2018.
- Gade Sikjær M, Hilberg O, Ibsen R, et al. Direct and indirect economic and health consequences related to sarcoidosis in Denmark: a national register-based study. Respir Med. 2019 Jun;152:7–13.
- Gouliaev A, Hilberg O, Christensen NL, et al. Comorbidity among Danish lung cancer patients before and after initial cancer diagnosis. Eur Clin Respir J. 2020;8(1):1861579.
- Migliorino MR, Santo A, Romano G, et al. Economic burden of patients affected by non-small cell lung cancer (NSCLC): the LIFE study. J Cancer Res Clin Oncol. 2017 May;143(5):783–791.
- Andreas S, Chouaid C, Danson S, et al. Economic burden of resected (stage IB-IIIA) non-small cell lung cancer in France, Germany and the UK: a retrospective observational study (LuCaBIS). Lung Cancer. 2018Oct;124:298–309.
- Zhang X, Liu S, Liu Y, et al. Economic burden for lung cancer survivors in Urban China. Int J Environ Res Public Health. 2017 Mar 15;14(3):E308.
- Kruse M, Hostenkamp G De samfundsøkonomiske omkostninger ved kræft, sep. 2016, COHERE. 258 s
- Goldsbury DE, Weber MF, Yap S, et al. Health services costs for lung cancer care in Australia: estimates from the 45 and up study. PLoS ONE. 2020;15(8):e0238018.
- Iachina M, Jakobsen E, Møller H, et al. The effect of different comorbidities on survival of non-small cells lung cancer patients. Lung. 2015 Apr;193(2):291–297.
- Islam KM, Jiang X, Anggondowati T, et al. Comorbidity and survival in lung cancer patients. Cancer Epidemiol Biomarkers Prev. 2015;24(7):1079–1085.
- Zarogoulidou V, Panagopoulou E, Papakosta D, et al. Estimating the direct and indirect costs of lung cancer: a prospective analysis in a Greek university pulmonary department. J Thorac Dis. 2015 Feb;7(Suppl 1):S12–9.
- Darbà J, Marsà A. The cost of lost productivity due to premature lung cancer-related mortality: results from Spain over a 10-year period. BMC Cancer. 2019;19(1):992.
- Falchs E, Eriksen L, Koch MB et al. Sygdomsbyrden i Danmark. Oct 2015. Sundheddstyrrelsen/Danish Health Authoroty. https://www.sst.dk/da/sygdom-og-behandling/~/media/00C6825B11BD46F9B064536C6E7DFBA0.ashx
- Fox KM, Brooks JM, Kim J. Metastatic non-small cell lung cancer: costs associated with disease progression. Am J Manag Care. 2008 Sep;14(9):565–571.
- Wood R, Taylor-Stokes G. Cost burden associated with advanced non-small cell lung cancer in Europe and influence of disease stage. BMC Cancer. 2019 Mar 8;19(1):214.
- Jakobsen E, Green A, Oesterlind K, et al. Nationwide quality improvement in lung cancer care: the role of the Danish Lung Cancer Group and Registry. J Thorac Oncol. 2013;8(10):1238–1247.
- Jakobsen E, Rasmussen TR. The Danish lung cancer registry. Clin Epidemiol. 2016;8:537–541.
- Van der Heyden JH, Schaap MM, Kunst AE, et al. Socioeconomic inequalities in lung cancer mortality in 16 European populations. Lung Cancer. 2009 Mar;63(3):322–330.
- Fløe A, Hilberg O, Weise C, et al. The economic burden of tuberculosis in Denmark 1998-2010. Cost analysis in patient and their spouses. Int J Infect Dic. 2015 Mar;32:183–190.
- Postmus PE, Kerr KM, Oudkerk M, et al. ESMO guidelines committee. Ann Oncol. 2017;28(suppl_4):iv1–iv21.