ABSTRACT
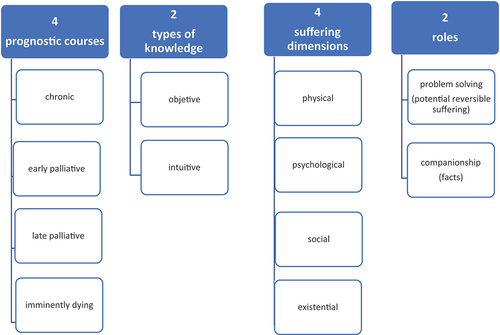
Palliative medicine has traditionally focused on people affected by cancer with rapidly advancing disease progression. However, as more people live longer time with serious illnesses, including lung diseases, the need of palliative care for these patients if also increasing. There is a lack of research and clinical knowledge about what palliative care is for people affected by chronic obstructive pulmonary disease and interstitial lung disease. The aim of this paper is to describe the development process of an easy to use and clinically relevant model for the palliative care approach in people affected by severe illnesses. The developed model consists of four components, which originated the title” 4,2,4,2 model”. Each number has a specific meaning: the first 4 = the four disease trajectories that patients may experience; 2 = the two forms of knowledge, objective, and intuitive that must be achieved by the health professionals to gain an understanding of the situation; 4 = the four dimensions of suffering physically, mentally, socially and existentially/spiritually; and 2 = the two roles that health-care professionals must be able to take in when treating patients with serious illnesses. The 4-2-4-2 model proposes an easy-to-use and clinically relevant model for palliative approach and integration of PC and pulmonary medicine. Another important purpose of this model is to provide HPs with different educational backgrounds and from different medical fields with a ‘golden standard approach’ to enhance the focus of the palliative approach in both the clinic and teaching. The effect and consequences of the use of the 4-2-4-2 model should be explored in future clinical trials. Furthermore, it should be investigated whether teaching the model creates a change in clinical approach to patients with serious illnesses as well as whether these changes are long-lasting.
Introduction
It has been estimated that 48 million people will die with serious health-related suffering due to severe illnesses in 2060, which means 47% of all deaths globally and represents an increase of 87% from 26 million in 2016 [Citation1].
International health-care associations, palliative care (PC) researchers, and engaged clinicians have promoted the concept that PC can be involved in any phase of the disease trajectory including the early phase, in both cancer diseases and other severe illnesses [Citation2–4]. Palliative care in its modern form started with St. Christopher’s hospice in 1967 [Citation5]. There was in the first international definition of palliative care WHO 1990 a clear cancer focus as it was described that the PC should start when curative treatment had been abandoned [Citation6]. Later in 2020, the WHO wrote that PC should be extended to patients with life-threatening illnesses [Citation7]. In 2020, the international association of hospice and palliative care (IAHPC) came up with their new definition where they use the term serious illness [Citation8]. This has origin on a from a definition published 2014, which describes serious illnesses within three main themes.
1. Diseases that carries a high risk of death over the course of a year, but cure may remain a possibility
2. reduced physical function and quality of life and
3. caregiver stress [Citation9].
Thus, in the definitions, there is a movement away from solely end-stage cancer focus and towards an early introduction of palliative care. Integrating palliative care with other health-care services has shown improved treatment of severe COPD patients [Citation10–12].
Due to the prognostic uncertainty, a timely integration of pulmonary medicine, primary care, rehabilitation services, and specialist palliative care (SPC) is widely recognized as a model to meet this challenge, but not yet reported as a practice solution [Citation3,Citation13,Citation14].
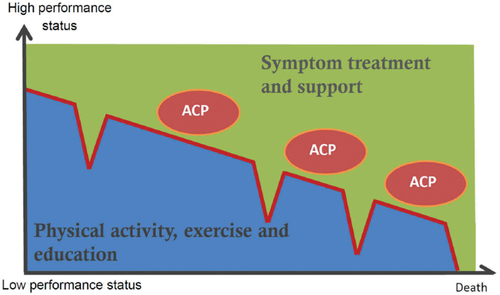
There is a great inequality in access to SPC in terms of diagnoses in Denmark. Almost 50% of patients with cancer diagnoses who died had had contact with a SPC team, while less than 2% of patients who died from chronic diseases from serious medical organ failure had contact [Citation15]. In 2020, the Danish Governmental Authority that audits the public accounts (Rigsrevisionen) criticized the inadequate availability and accessibility of SPC, particularly in patients with life-threatening organ failure. In addition, it was mentioned that referrals to SPC were too late and sometimes on a random basis [Citation16]. Resulting in suboptimal symptom management, increased suffering, and worse quality of life for patients and their families. The Danish Respiratory Society (DRS) published a Danish statement and an advance care planning (ACP) manual in 2015 [Citation17,Citation18] and a position paper in 2018 [Citation14]. In these documents, a treatment and care model for PC in patients with life-threatening lung diseases was proposed. The model was based on a modified version of Scott Murray’s description of illness trajectories [Citation19], adding coherent rehabilitation and palliation () [Citation14].
Figure 1. Personalized management and palliation includes symtom treatment, rehabilitation, patient education and support. Palliative support, including pyschological, social and existential support, may continue into care for the informal caregiver after the patient’s death. Routine and early Advance Care Planning (ACP) provide the ability to adjust treatment goals during the disease trajectory.
In 2020, the impact of the documents was examined in an electronic survey among members of DRS. Thus, 71% in this survey indicated knowledge of the documents, while less than 3% indicated using them regularly [Citation20]. Possibly several types of barriers to the integration of palliative care and pulmonary medicine exist, which highlight the need for new models of care simple to relate to and apply [Citation12,Citation21,Citation22].
Acknowledging this, we have developed a model for both clinical and educational use in a multidisciplinary setting. Hopefully, it will promote awareness four important clinical components on the healthcare approach of those in need of palliative care. In order to establish a palliative care service, a shared understanding of what such a service contains must be established and relevant teaching and training must be developed in order to be able to carry out this task [Citation23].
The AIM of this paper
The aim of this paper is to describe the development process of an user friendly and clinically relevant model for the palliative care approach in people affected by severe illnesses.
Method
Conceptualization
Through literature review of clinical work and teaching, four issues were identified
1. Prognostic uncertainty – and when to trigger PC and when to trigger rehabilitation.
2. Great emphasis on patient reported outcomes (PRO) questionnaires, biochemistry, lung function, and function test such as 6 minutes walking test and other objective measurements often without appropriate PC treatment and care in clinical practice.
3. Tendency to focus on physical and to some extend psychological symptoms rather than social and existential suffering.
4. Great insecurity towards patients and relatives, when medical treatment options were exhausted.
One challenge for specialized palliation is that it must be multidisciplinary. This means that professional development for a palliative approach should be able to embrace more disciplines. This involves day-to-day work and teaching.
In 2019, an employee manual of 24 pages was prepared, which describes in detail the PC approach. We tried to describe nuances, dilemmas, and different interpretations of existing evidence. This was initially introduced in Palliative Unit Herlev and Gentofte. The feedback was, for example, that it was an exciting review of research, difficult to understand and for some boring reading unrelated to their daily work. The feedback was given orally in connection with the implementation session and at later repeated evaluation discussions.
Based on the negative feedback, the guideline was abandoned and new a strategy for quality improvement work was developed. We wanted to create an over-arching, easily remembered, and clinically applicable model that could be used daily across different professional groups to both achieve a uniform clinical approach and for teaching purposes. We concluded that we needed a simple mnemonic model inspired by the ABCD model in emergency medicine [Citation24].
Model development
A method inspired by the Plan, Do, Study, Act (PDSA) model [Citation25] was chosen based on the strategy on several minor trials and adjustments. The model is based on small tests being followed by adjustments and then new tests.
Feedback during the development process was collected through three groups of informants. See .
Figure 2. The development of the model. There are 3 different types of feedback, from clinicians who take the model into clinical use, from teaching sessions and from experts.
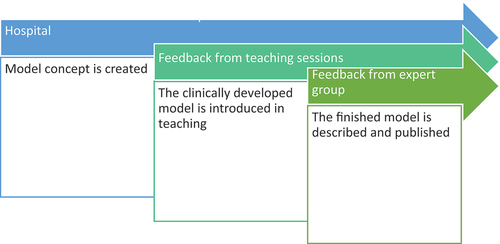
1. Nurses in the at specialized palliative care unit Herlev and Gentofte Hospital were presented with the model in weekly meetings with small discussion groups consisting of one nurse from the beds ward one from the outpatient clinic and two nurse specialists. Thus, this paper builds on feedback from around 50 meetings during the period 2019 to 2020.
2. Training of staff from other specialized palliative care services in both hospital and hospice settings.
3. Teaching other health professionals. There were more than 10 teaching sessions with doctor and nurse from general practice from 4 to 14 participants, as well as a teaching session for pulmonary physiotherapists, a pulmonary out-patient clinic, and staff from a pulmonary bed ward, a session for hematological specialists in training, and one for oncology specialists in training.
Feedback was continuously incorporated into the model and presentation. Following this evaluation process with clinical working HP 4 experts were invited to make the final version of the model. The experts were a hospital chaplain (LM), clinical psychologist with palliative expertise (SN) as well as a medical palliative professor (PS) and a nursing palliative professor (GK). This last workover to strengthen to description and theoretical basis of the model.
Feedback was continuously collected by JM and KM. In all three types of feedback from clinical use, teaching, and expert feedback were collected as comments and considerations and not quantitative feedback forms that were collected.
Results
The 4,2,4,2 model
Four prognostic trajectories: To establish an effective and relevant goal of care it is necessary to identify in which trajectory the patient is in. Severe illnesses have in our model 4 trajectories, and each trajectory has its own goals of care and means. In describing the four trajectories, we work systematically to integrate classical rehabilitation with palliative care both in goal of care and in intervention. This is described by many, but there is still a lack of scientific evidence [Citation26–29]
Chronic trajectory – the patient is in good physical condition and may have a substantial rehabilitation potential. The lifetime expectancy is unknown – maybe years. Goals in our model include typically improvement of function and health-enhancing behavior changes as known from rehabilitation [Citation30,Citation31]
Early progressive trajectory – the disease is progressive and will cause increasing frailty. Lifetime expectancy is of several months to a few years. The physical condition is affected to some degree, and the goals of care are to stabilize function and reduce further decline. Still part of the classical rehabilitation approach, but now with a larger focus on the immediate quality of life.
Late progressive trajectory – the patient is severely affected by general weakness and is resting most of the day. Lifetime expectancy is weeks to a few months. The goal of care is aiming at end-of-life care. It includes to prepare the patient and informal caregivers for imminent death. To reduce futile treatments and to ensure that there is appropriate support if the patient continues to live in their own home. No longer training based exercise, but rather movements to stimulate sensory bodily experiences.
Imminently dying trajectory – the patient is bedridden and may fall in and out of consciousness. Expected lifetime is from a few hours to a maximum of a few days. The goals of care are aiming at providing relief of suffering, dignified death, and preparing future bereavement support.
Two types of knowledge: Clinical judgments must be based on a combination of objective and the intuitive knowledges. Objective knowledge is what we can measure and what we can describe with numbers, such as vital signs (e.g. blood pressure, temperature, etc.). Alongside the objective knowledge is the intuitive knowledge [Citation32]. In our model intuitive knowledge is understood as interindividual relationship of interpreted feelings, perceptions, and compassion. Most HPs are trained to use the objective knowledge as it is feasible to pass on in documentation and easy to evaluate [Citation33]. However, intuitive knowledge is also important. In the intuitive knowledge is concrete, clinically worthy, as shown in a study where phlebotomists eyeball triages, that is, their intuitive assessment, were superior to standard triage models in predict short-term mortality in emergency departments patients [Citation34].
The dichotomy between objective evidence-based medicine and clinical intuition is possible inexistent [Citation35].
In the 4,2,4,2 model the two types of knowledge are equally important and should always be used in combination.
Four dimensions of suffering: It is based on Cicely Saunders’ concept of ‘total pain’, which described that pain has four dimensions of suffering: physical, psychological, existential/spiritual, and social [Citation5]. This nuanced understanding of suffering is the basis of the palliative approach since St. Christopher’s Hospice opened [Citation5].
It is integrated of the total pain model into the 4,2,4,2 model and use the term of ‘total suffering’ [Citation36]. The four dimensions are interrelated. This means that a physical experience of shortness of breath can influence and provoke feelings and emotional reactions, which in turn may be amplified by social patterns in the family. In this way, what starts as a physical experience of shortness of breath can quickly be amplified by the other dimensions. The same is true when well treated, relief in one dimension can also bring relief in other dimensions.
This is essential for the HP to remember that any symptom potentially involves more dimensions than first assumed and all dimensions of suffering should be assessed and addressed by the multidisciplinary team and reflected in the treatment. The total suffering calls for relief involving all four dimensions – the total relief.
Two essential roles: When the HP encounters the suffering of patients, they must distinguish between what is reversible and irreversible. In this model, symptoms/suffering that are reversible through meaningful intervention are called problems. When HP encounters a problem, a problem-solving role is assumed. It can be an acute exacerbation of dyspnea which requires corticosteroids and perhaps antibiotics, or treatment failure because the patient can no longer use his/her inhaler. The HP must fix the problem. It is this problem-solving role that HPs are most trained in through their health educations. Other kind of suffering appear to be facts of life, which may be of irreversible nature and therefore cannot be fixed. Such as grief following the loss of a loved one or the progressing of shortness of breath, which deprives them the capability of physical activity. Although, these facts of life cannot be fixed the HP can accompany the patient and thereby alleviate some of the suffering – also by providing support for the informal caregivers [Citation37–42]. Thus, the HP can take on a companionship role where the patient experiences continuity in care through an HP who follows the patient through the course of the disease in the different phase such as hospitalization, mild exacerbations treated at home, stable periods, and periods of biological disease activity and consequent vulnerability. This role is an active and professionally demanding role for the HP. The accompanying role is largely based on compassion [Citation43] and communication skills. For many HPs, it can be a very challenging role to be present and listen to a person’s history about suffering without being able to fix it but when it is done its meaningful for both patient and HP [Citation39,Citation40,Citation44]
When Cicely Saunders created modern palliative medicine, it was part of the basic idea that sometimes the best possible relief is to be present and compassionate [Citation5].
In most encounter with patients, both types of suffering (problem and facts) will be present. It is therefore the task of the HP to continuously assess whether it is a problem that needs to be solved or a fact that needs to be accompanied. A symptom like shortness of breath can also change type of suffering as diseases progress. In a patient in the chronic trajectory, shortness of breath is treated with inhalation medication and exercise in addition, but primarily the patient must learn to live the best possible despite shortness of breath. Whereas in a late palliative trajectory and in the imminent death one can try to relieve with opioids well aware of the potential side effects associated with this.
Discussion
We have presented a didactic framework for the PC approach. It is intended to be used as a clinical approach and in teaching to improve HP’s understanding of palliative care as well as increase the quality of daily clinical work. One of the strengths of the 4,2,4,2 model is that it provides a systematic approach that can be applied across educational background, different clinics, and in research - see . As such, it should support HPs to get a better assessment and knowledge of the patient’s holistic situation before they act. An important part of understanding PC is that it must be multidisciplinary as different HPs based on their education can identify different parts of the patient overall situation and symptom pattern [Citation33]. The goal of this model was therefore to develop a framework that could be used by any professional group within the multidisciplinary team as a shared starting point in the care and treatment of patients. No model can embrace all the nuances that the individual patient with serious health-related suffering presents. Nevertheless, 4,2,4,2 can support HPs in planning the best possible treatment and care.
Figure 3. The four elements in the 4,2,4,2 model which is a theoretical and systematic description of the palliative approach.
There are several studies that show the effect of a nurse who follow the patients over the disease trajectory. Through knowledge of the patient and a relationship build on trust and the possibility of following the patient over a longer period of time this can increased self management and lower health-care cost. In the Canadian studies, these nurses are called casemanager nurses and have shown their worth [Citation37,Citation45,Citation46]. In these studies, actions plan is a great part of the combined self-management intervention combined with the case managers.
Our model is intended as a foundation for training health-care professionals to follow the patient. Actions plans are not part of the model but can of course be used in those patients where it is considered to make sense.
Expanding an out-patient clinic with such an accompanying function, it will require organizational changes [Citation20,Citation47], and that it can create uncertainty in the nurse group when they are given new professional responsibility, this can in the worst case lead to stress and burn out [Citation40,Citation48]. However, we also know that through organization in palliative care, such as supervision and interdisciplinary collaboration, burn-out can be reduced [Citation44].
The use of a modified PDSA method is not without problems – especially, around loss transparency and process description [Citation25,Citation49], but it was still viewed as the best option under the circumstances. This iterative approach contrasts with classic RCT studies, which often require significantly more financial and time resources. The conditions where there were no funds allocated for this development work did not allow for a larger quantitative study of the model usability. We chose to use teaching sessions with different professions from many specialties and qualitatively collect their feedback. This became our ongoing evaluation and based on that we made ongoing adjustments.
A validation of a complex intervention, such as the 4,2,4,2 model will require that the HP in the validation process can understand and use the model and furthermore be able to deliver SPC. It requires according to MRC Population Health Science Research Network method several steps in the validation including a clear description of the intervention [Citation50]. We have certainly not validated 4,2,4,2 model, but we have tried to describe the development. Thus, the model can be:
- used by all regardless of educational background,
- easy to remember and applicable in daily clinical work, and
- easy to explain and to be used in teaching.
Conclusion
The 4-2-4-2 model proposes an easy-to-use and clinically relevant model for palliative approach and integration of PC and pulmonary medicine. Another important purpose of this model is to provide HPs with different educational backgrounds and from different medical fields with a ‘golden standard approach’ to enhance the focus of the palliative approach in both the clinic and teaching. The effect and consequences of the use of the 4-2-4-2 model should be explored in future clinical trials. Furthermore, it should be investigated whether teaching the model creates a change in clinical approach to patients with serious illnesses as well as whether these changes are long-lasting.
Further development
The effect and consequences of the use of the 4-2-4-2 model should be evaluated and tested in future clinical trials. Furthermore, it should be investigated whether teaching the model creates a change in clinical approach to patients with serious illnesses as well as whether these changes are long-lasting.
Acknowledgments
We would like to thank all the clinical staff who have contributed to the development of this model. We would also like to thank all the patients and informal caregivers whose lives we have been involved in at a very vulnerable time for them.
Disclosure statement
This research received no financial support from any funding agency, commercial or not-for-profit sectors. Kristoffer Marsaa has received honoraria from Astellas Pharma, GlaxoSmithKline, AstraZeneca, Novartis, Boehringer Ingelheim, Kyowa Kirin, and Norgine. Geana Kurita has received a grant from the Novo Nordisk Foundation and the Danish Cancer Society, not related to this work. The remaining authors have nothing to declare.
Additional information
Notes on contributors
Kristoffer Marsaa
Kristoffer Marsaa, MD, Senior consultant. Arresoedal Hospice, Denmark. Specialist in pulmonary medicine and certified specialist in palliative medicine with clinical and research focus in COPD, pulmonary fibrosis, Chronic care, rehabilitation and palliative care to persons with serious illness.
Janni Mendahl
Janni Mendahl, RN, Senior clinical nursing specialist, Palliative unite, Departmen of urology, Copenhagen University, Herlev and Gentofte hospital, Denmark. Research and teachings interest in chronic care and palliative care COPD and ILD, development of palliative care nursing skills.
Steen Nielsen
Steen P. Nielsen, Health psychologist, Sankt Lukas hospice, Denmark. Counsellor at the danish cancer association. Supervision and teaching of palliative staffs
Lotte Mørk
Lotte Mørk, Hospital Chaplain, Master of Theology Head of Church Section, Department of Oncology, Rigshospitalet - Copenhagen University Hospital, Denmark
Per Sjøgren
Per Sjøgren, MD, DMSci Department of Oncology, Rigshospitalet - Copenhagen University Hospital, Denmark Specialist in palliative medicine with research focus on pain and symptom management
Geana Paula Kurita
Geana P. Kurita holds a bachelor’s degree, master and PhD in nursing and serves as Professor at Rigshospitalet and the University of Copenhagen, Denmark. Her almost 15 years of research work in Denmark has contributed to developing the knowledge on chronic pain and palliative care in different populations.
References
- Sleeman KE, de Brito M, Etkind S, et al. The escalating global burden of serious health-related suffering: projections to 2060 by world regions, age groups, and health conditions. Lancet Glob Heal. 2019;7:e883–8.
- Kaasa S, Loge JH, Aapro M, et al. Integration of oncology and palliative care: a Lancet Oncology Commission. Lancet Oncol. 2018;19:588–653.
- Maddocks M, Lovell N, Booth S, et al. Palliative care and management of troublesome symptoms for people with chronic obstructive pulmonary disease. Lancet. 2017;390:988–1002.
- Lanken PN, Terry PB, Delisser HM, et al. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008;177:912–927.
- Saunders C. Watch with me. Mortal Press, 2003 http://endoflifestudies.academicblogs.co.uk/wp-content/uploads/sites/22/2014/04/Watch-with-Me-full-text-2005.pdf.
- Foley K, Macdonald N, McCaffery M, et al. Cancer pain relief and palliative care. Report of a WHO Expert Committee. World Heal Organ. 1990;804:1–75.
- Sepúlveda C, Marlin A, Yoshida T, et al. Palliative care: the world health organization’s global perspective. J Pain Symptom Manage. 2002;24:91–96.
- Radbruch L, De Lima L, Knaul F, et al. Redefining palliative care – a new consensus-based definition. J Pain Symptom Manage. 2020;60:754–764.
- Kelley AS. Defining ‘serious illness’. J Palliat Med. 2014;17:985.
- Payne S, Eastham R, Hughes S, et al. Enhancing integrated palliative care: what models are appropriate? A cross-case analysis. BMC Palliat Care. 2017;16:1–10.
- Boland J, Owen J, Ainscough R, et al. Developing a service for patients with very severe chronic obstructive pulmonary disease (COPD) within resources. BMJ Support Palliat Care. 2013;4:196–201.
- Smallwood N, Thompson M, Warrender-Sparkes M, et al. Integrated respiratory and palliative care may improve outcomes in advanced lung disease. ERS Monogr. 2018;4. DOI:10.1183/23120541.00102-2017.
- Ringbæk T, Wilcke T. Rehabilitering og palliation af patienter med svær KOL bør integreres. Ugeskr Laeger. 2013;175:1277–1280.
- Marsaa K, Gundestrup S, Jensen J-U, et al. Danish respiratory society position paper: palliative care in patients with chronic progressive non-malignant lung diseases. Eur Clin Respir J. 2018;5:1530029.
- Hansen MB, Adsersen M, and Grønvold M. Dansk Palliativ Database: Årsrapport 2020. København: DMCG-PAL og Regionernes Kliniske Kvalitetsprogram (RKKP). 2021 http://www.dmcgpal.dk/files/23_6_21_aarsrapport_dpd_2020_med_3_reglen.pdf.
- Statsrevisorene F, Rigsrevisionen F. Access to specialist palliative care - Extract from Rigsrevisionen’s report submitted to the Public Accounts Committee. BMJ. 2020. DOI:10.1136/bmj.308.6923.273d
- Marså K, Knudsen T, Gundestrup S, et al. Dansk Lungemedicinsk Selskab: klaringsrapport om palliation til voksne med kronisk fremadskridende non-malign lungesygdom. http://www.lungemedicin.dk/fagligt/klaringsrapporter/189-dls-klaringsrapport-om-palliation-2015/file.html.
- Marså K, Lavesen M, and Knudsen T, et al. Samtalen om Fælles Planlægning af Behandlingsmål. 2015:1–12.
- Murray SA, Kendall M, Boyd K, et al. Clinical review Illness trajectories and palliative care. Br Med J. 2005;330:1007–1011.
- Sørensen AR, Marsaa K, Prior TS, et al. Attitude and barriers in palliative care and advance care planning in nonmalignant chronic lung disease: results from a Danish National Survey. J Palliat Care. 2020;35:3–6.
- Brown CE, Jecker NS, Curtis JR. Inadequate palliative care in chronic lung disease an issue of health care inequality. Ann Am Thorac Soc. 2016;13:311–316.
- Mounsey L, Miriam F, Eastman P. Integrated respiratory and palliative care may improve outcomes in advanced lung disease. R Aust Coll Gen Pract. 2018;47. doi:10.1183/23120541.00102-2017.
- Fusi-Schmidhauser T, Riglietti A, Froggatt K, et al. Palliative care provision for patients with advanced chronic obstructive pulmonary disease: a systematic integrative literature review. COPD J Chronic Obstr Pulm Dis. 2018;15:600–611.
- Thim T, Krarup NHV, Grove EL, et al. Initial assessment and treatment with the Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach. Int J Gen Med. 2012;5:117–121.
- Taylor MJ, McNicholas C, Nicolay C, et al. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23:290–298.
- Eva G, Wee B. Rehabilitation in end-of-life management. Curr Opin Support Palliat Care. 2010;4:158–162.
- Spruit MA, Janssen DJA, Franssen FME, et al. Rehabilitation and palliative care in lung fibrosis. Respirology. 2009;14:781–787.
- Kaldjian LC, Curtis AE, Shinkunas LA, et al. Review article: goals of care toward the end of life: a structured literature review. Am J Hosp Palliat Med. 2009;25:501–511.
- Reticker AL, Nici L, ZuWallack R. Pulmonary rehabilitation and palliative care in COPD: two sides of the same coin? Chron Respir Dis. 2012;9:107–116.
- Spruit MA, Singh SJ, Garvey C, et al. An official American thoracic society/European respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:e13–e64.
- Garvey C, Bayles MP, Hamm LF, et al. Pulmonary rehabilitation exercise prescription in chronic obstructive pulmonary disease: review of selected guidelines: an official statement from the American association of cardiovascular and pulmonary rehabilitation. J Cardiopulm Rehabil Prev. 2016;36:75–83.
- Hall KH. Reviewing intuitive decision-making and uncertainty: the implications for medical education. Med Educ. 2002;36:216–224.
- Sandau C, Bove DG, Marsaa K, et al. Is the high intensity symptoms experienced by patients admitted with chronic obstructive pulmonary disease documented by health professionals? - a prospective survey with comparison of patient reported outcomes and medical records. Eur Clin Respir J. 2018;5:1506236.
- Iversen AKS, Kristensen M, Østervig RM, et al. A simple clinical assessment is superior to systematic triage in prediction of mortality in the emergency department. Emerg Med J. 2019;36:66–71.
- Greenhalgh T. Intuition and evidence-uneasy bedfellows? Stories of intuition. Br J Gen Pract. 2002;52:395.
- Arantzamendi M, Centeno C. Intangible values of palliative care. Eur J Palliat Care. 2017;24:72–74.
- Bourbeau J, Saad N, Joubert A, et al. Making collaborative self-management successful in COPD patients with high disease burden. Respir Med. 2013;107:1061–1065.
- Bischoff EWM, Hamd DH, Sedeno M, et al. Effects of written action plan adherence on COPD exacerbation recovery. Thorax. 2011;66:26–31.
- Bove DG, Jellington MO, Lavesen M, et al. Assigned nurses and a professional relationship: a qualitative study of COPD patients’ perspective on a new palliative outpatient structure named CAPTAIN. BMC Palliat Care. 2019;18:1–9.
- Bove DG, Lavesen M, Jellington MO, et al. First year experiences with a palliative out-patients structure for patients with COPD: a qualitative study of health professionals’ expectations and experiences. BMC Palliat Care. 2018;17:1–10.
- Overgaard D, Kaldan G, Marsaa K, et al. The lived experience with idiopathic pulmonary fibrosis: a qualitative study. Eur Respir J. 2016;47:1–9.
- den Herder-van der Eerden M, Hasselaar J, Payne S, et al. How continuity of care is experienced within the context of integrated palliative care: a qualitative study with patients and family caregivers in five European countries. Palliat Med. 2017;31:946–955.
- Sinclair S, Beamer K, Hack TF, et al. Sympathy, empathy, and compassion: a grounded theory study of palliative care patients’ understandings, experiences, and preferences. Palliat Med. 2017;31:437–447.
- Boegelund Kristensen T, Kelstrup Hallas M, Høgsted R, et al. Burnout in physicians: a survey of the Danish society for palliative medicine. BMJ Support Palliat Care. 2021. DOI:10.1136/bmjspcare-2021-003237
- Bourbeau J, Collet J-P, Schwartzman K, et al. Economic benefits of self-management education in COPD. Chest. 2006;130:1704–1711.
- Bourbeau J, Julien M, Maltais F, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease. Arch Intern Med. 2003;2003:163.
- Lavesen M, Marsa KBM, Bove DG. A new way of organising palliative care for patients with severe chronic obstructive pulmonary disease. Int J Palliat Nurs. 2018;24:64–68.
- Marsaa K, Mendahl J, Heilman H, et al. Pride and Uncertainty. J Hosp Palliat Nurs. 2021;23:140–144.
- Reed JE, Card AJ. The problem with plan-do-study-act cycles. BMJ Qual Saf. 2016;25:147–152.
- Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350:1–7.
